Efficacy and Safety of SPN-812 (Extended-Release Viloxazine) in Children and Adolescents with Attention-Deficit/Hyperactivity Disorder: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
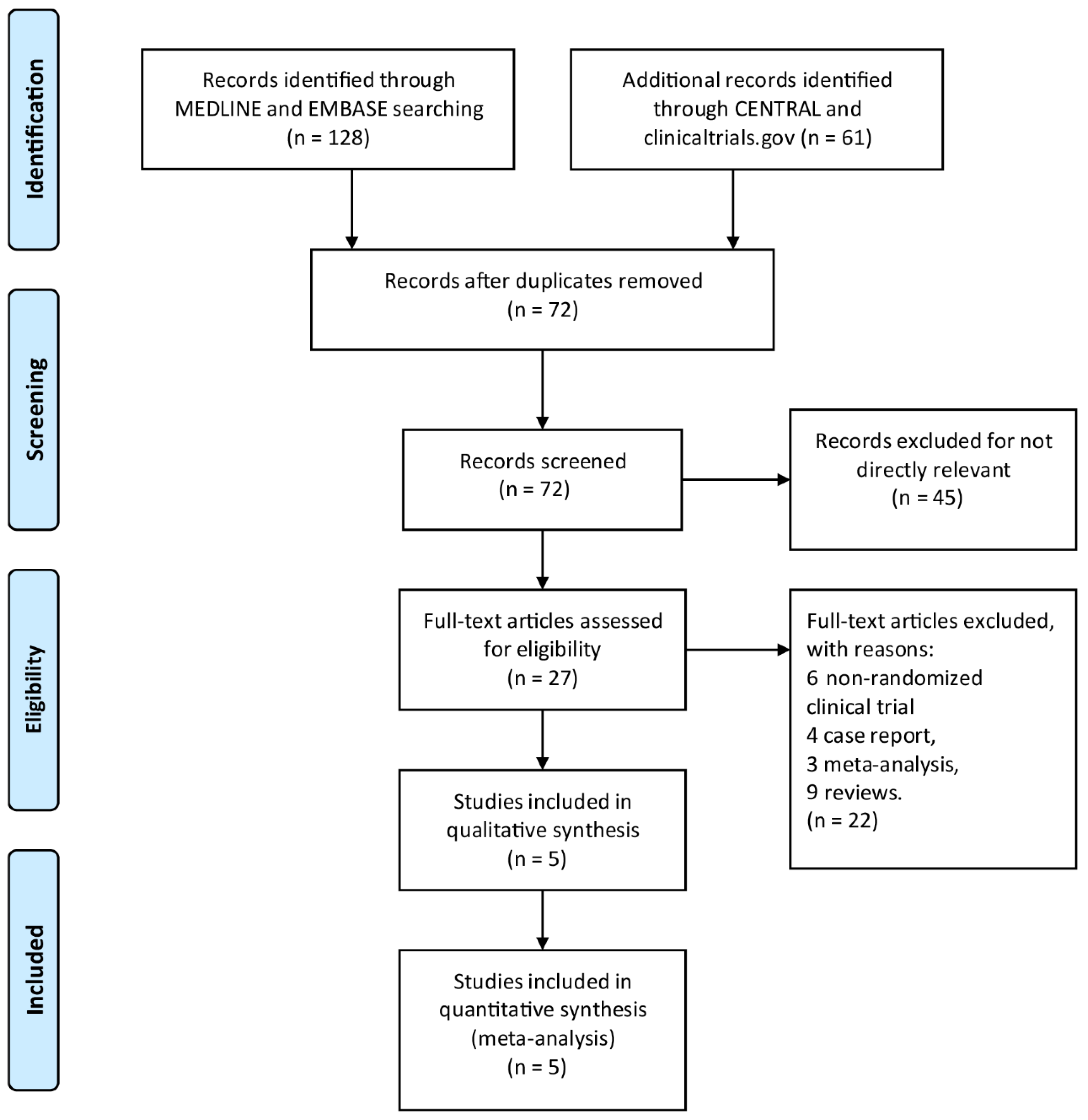
2. Methods
2.1. Study Protocol
2.2. Eligibility Criteria
2.3. Search Process
2.4. Study Selection and Data Collection
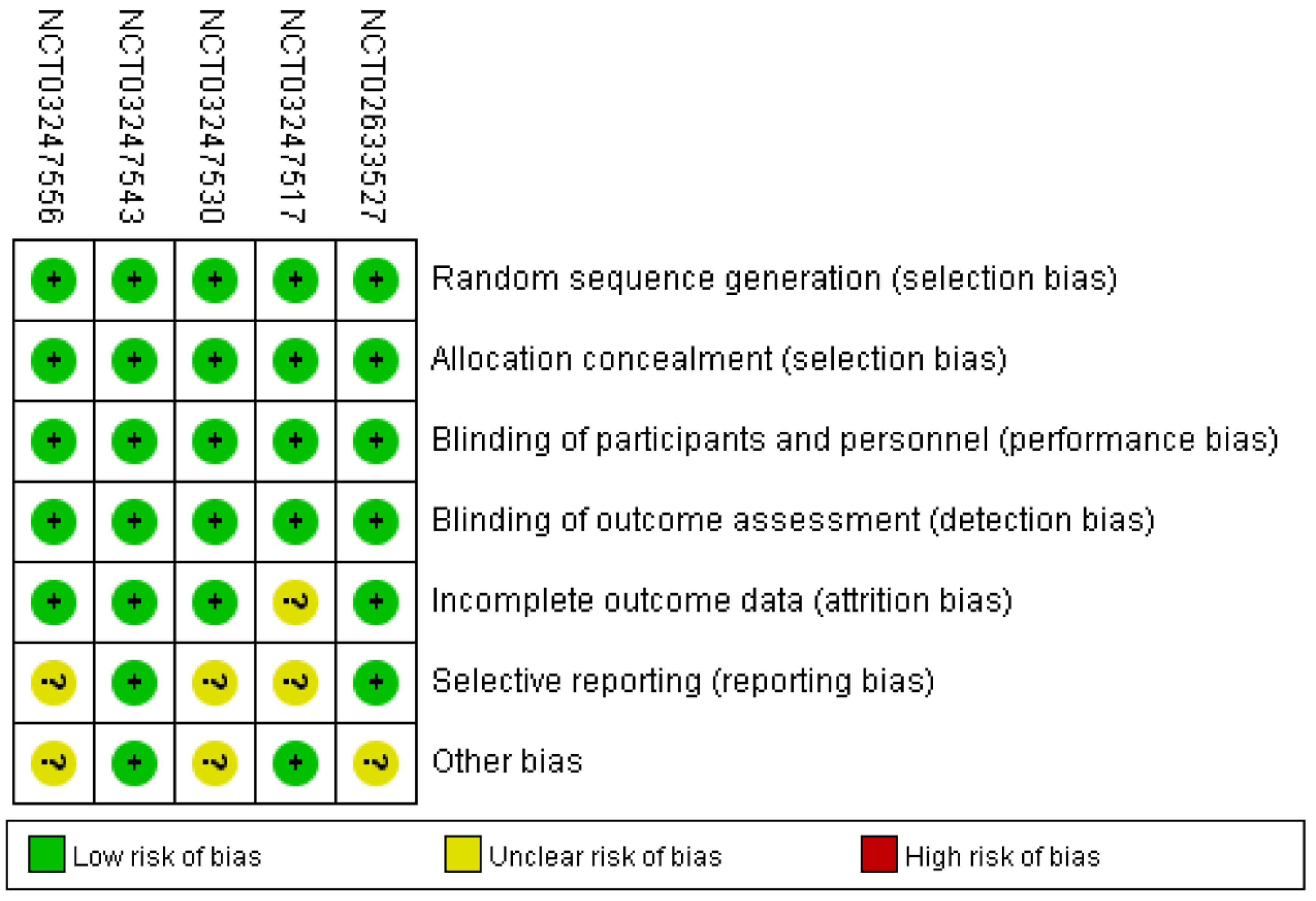
2.5. Analysis of Bias Risk
2.6. Summary Measures and Synthesis of Results
3. Results
3.1. Efficacy Outcomes Analysis
3.2. Safety Outcomes Analysis
3.3. Subgroup Analyses
3.4. Risk of Bias in Enrolled Studies
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cortese, S.; Adamo, N.; Del Giovane, C.; Mohr-Jensen, C.; Hayes, A.J.; Carucci, S.; Atkinson, L.Z.; Tessari, L.; Banaschewski, T.; Coghill, D.; et al. Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: A systematic review and network meta-analysis. Lancet Psychiatry 2018, 5, 727–738. [Google Scholar] [CrossRef] [PubMed]
- Simon, V.; Czobor, P.; Bálint, S.; Mészáros, Á.; Bitter, I. Prevalence and correlates of adult attention-deficit hyperactivity disorder: Meta-analysis. Br. J. Psychiatry J. Ment. Sci. 2009, 194, 204–211. [Google Scholar] [CrossRef]
- Luo, Y.; Weibman, D.; Halperin, J.M.; Li, X. A Review of Heterogeneity in Attention Deficit/Hyperactivity Disorder (ADHD). Front. Hum. Neurosci. 2019, 13, 42. [Google Scholar] [CrossRef]
- Barbaresi, W.J.; Colligan, R.C.; Weaver, A.L.; Voigt, R.G.; Killian, J.M.; Katusic, S.K.; Chawla, A.; Sprinz, P.G.; Welch, J.; Heeney, M.; et al. Mortality, ADHD, and Psychosocial Adversity in Adults with Childhood ADHD: A Prospective Study. PEDIATRICS 2013, 131, 637–644. [Google Scholar] [CrossRef] [PubMed]
- Barkley, R.A.; Fischer, M. Hyperactive Child Syndrome and Estimated Life Expectancy at Young Adult Follow-Up: The Role of ADHD Persistence and Other Potential Predictors. J. Atten. Disord. 2016, 23, 907–923. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Page, T.F.; Altszuler, A.R.; Pelham, W.E., III; Kipp, H.; Gnagy, E.M.; Coxe, S.; Schatz, N.K.; Merrill, B.M.; Macphee, F.L.; et al. Family Burden of Raising a Child with ADHD. J. Abnorm. Child Psychol. 2019, 47, 1327–1338. [Google Scholar] [CrossRef]
- Vidal, R.; Castells, J.; Richarte, V.; Palomar, G.; García, M.; Nicolau, R.; Lazaro, L.; Casas, M.; Ramos-Quiroga, J.A. Group Therapy for Adolescents with Attention-Deficit/Hyperactivity Disorder: A Randomized Controlled Trial. J. Am. Acad. Child Adolesc. Psychiatry 2015, 54, 275–282. [Google Scholar] [CrossRef] [PubMed]
- Rahmani, M.; Mahvelati, A.; Farajinia, A.H.; Shahyad, S.; Khaksarian, M.; Nooripour, R.; Hassanvandi, S. Comparison of Vitamin D, Neurofeedback, and Neurofeedback Combined with Vitamin D Supplementation in Children with Attention-Deficit/Hyperactivity Disorder. Int. J. Infect. Dis. 2022, 25, 285–393. [Google Scholar] [CrossRef]
- Caye, A.; Swanson, J.M.; Coghill, D.; Rohde, L.A. Treatment strategies for ADHD: An evidence-based guide to select optimal treatment. Mol. Psychiatry 2018, 24, 390–408. [Google Scholar] [CrossRef]
- Cortese, S. Pharmacologic Treatment of Attention Deficit–Hyperactivity Disorder. New Engl. J. Med. 2020, 383, 1050–1056. [Google Scholar] [CrossRef]
- Rajeh, A.; Amanullah, S.; Shivakumar, K.; Cole, J. Interventions in ADHD: A comparative review of stimulant medications and behavioral therapies. Asian J. Psychiatry 2017, 25, 131–135. [Google Scholar] [CrossRef] [PubMed]
- Mechler, K.; Banaschewski, T.; Hohmann, S.; Häge, A. Evidence-based pharmacological treatment options for ADHD in children and adolescents. Pharmacol. Ther. 2021, 230, 107940. [Google Scholar] [CrossRef] [PubMed]
- Edinoff, A.N.; Akuly, H.A.; Wagner, J.H.; Boudreaux, M.A.; Kaplan, L.A.; Yusuf, S.; Neuchat, E.E.; Cornett, E.M.; Boyer, A.G.; Kaye, A.M.; et al. Viloxazine in the Treatment of Attention Deficit Hyperactivity Disorder. Front. Psychiatry 2021, 12, 789982. [Google Scholar] [CrossRef]
- Arnett, A.; Stein, M. Many patients discontinue treatment due to intolerable side effects of these drugs despite persistent symptoms. Lancet Psychiatry 2018, 5, 691–692. [Google Scholar] [CrossRef] [PubMed]
- Banaschewski, T.; Roessner, V.; Dittmann, R.W.; Santosh, P.J.; Rothenberger, A. Non-stimulant medications in the treatment of ADHD. Eur. Child Adolesc. Psychiatry 2004, 13, i102–i116. [Google Scholar] [CrossRef]
- Biederman, J.; Spencer, T.J.; Newcorn, J.H.; Gao, H.; Milton, D.R.; Feldman, P.D.; Witte, M.M. Effect of comorbid symptoms of oppositional defiant disorder on responses to atomoxetine in children with ADHD: A meta-analysis of controlled clinical trial data. Psychopharmacology 2006, 190, 31–41. [Google Scholar] [CrossRef]
- Wolraich, M.L.; Hagan, J.F.; Allan, C.; Chan, E.; Davison, D.; Earls, M.; Evans, S.W.; Flinn, S.K.; Froehlich, T.; Frost, J.; et al. Clinical Practice Guideline for the Diagnosis, Evaluation, and Treatment of Attention-Deficit/Hyperactivity Disorder in Children and Adolescents. Pediatrics 2019, 144, e20192528. [Google Scholar] [CrossRef]
- Johnson, J.K.; Liranso, T.; Saylor, K.; Tulloch, G.; Adewole, T.; Schwabe, S.; Nasser, A.; Findling, R.L.; Newcorn, J.H. A Phase II Double-Blind, Placebo-Controlled, Efficacy and Safety Study of SPN-812 (Extended-Release Viloxazine) in Children With ADHD. J. Atten. Disord. 2019, 24, 348–358. [Google Scholar] [CrossRef]
- Yu, C.; Garcia-Olivares, J.; Candler, S.; Schwabe, S.; Maletic, V. New Insights into the Mechanism of Action of Viloxazine: Serotonin and Norepinephrine Modulating Properties. J. Exp. Pharmacol. 2020, 12, 285–300. [Google Scholar] [CrossRef]
- QELBREE™ (Viloxazine Extended-Release Capsules), for Oral Use Initial U.S. Approval: 2021. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/211964s000lbl.pdf (accessed on 20 August 2023).
- Singh, A.; Balasundaram, M.K.; Singh, A. Viloxazine for Attention-Deficit Hyperactivity Disorder: A Systematic Review and Meta-analysis of Randomized Clinical Trials. J. Cent. Nerv. Syst. Dis. 2022, 14, 11795735221092522. [Google Scholar] [CrossRef]
- Mather, K.; Condren, M. Extended-Release Viloxazine for Children and Adolescents with Attention Deficit Hyperactivity Disorder. J. Pediatr. Pharmacol. Ther. 2022, 27, 409–414. [Google Scholar] [CrossRef] [PubMed]
- Nasser, A.; Liranso, T.; Adewole, T.; Fry, N.; Hull, J.T.; Busse, G.D.; Chowdhry, F.; Cutler, A.J.; Jones, N.J.; Findling, R.L.; et al. A Phase 3, Placebo-Controlled Trial of Once-Daily Viloxazine Extended-Release Capsules in Adolescents with Attention-Deficit/Hyperactivity Disorder. J. Clin. Psychopharmacol. 2021, 41, 370–380. [Google Scholar] [CrossRef]
- Nasser, A.; Liranso, T.; Adewole, T.; Fry, N.; Hull, J.T.; Chowdhry, F.; Busse, G.D.; Cutler, A.J.; Jones, N.J.; Findling, R.L.; et al. A Phase III, Randomized, Placebo-controlled Trial to Assess the Efficacy and Safety of Once-daily SPN-812 (Viloxazine Extended-release) in the Treatment of Attention-deficit/Hyperactivity Disorder in School-age Children. Clin. Ther. 2020, 42, 1452–1466. [Google Scholar] [CrossRef] [PubMed]
- Nasser, A.; Liranso, T.; Adewole, T.; Fry, N.; Hull, J.T.; Chowdhry, F.; Busse, G.D.; Melyan, Z.; Cutler, A.J.; Findling, R.L.; et al. Once-Daily SPN-812 200 and 400 mg in the treatment of ADHD in School-aged Children: A Phase III Randomized, Controlled Trial. Clin. Ther. 2021, 43, 684–700. [Google Scholar] [CrossRef] [PubMed]
- Nasser, A.; Liranso, T.; Adewole, T.; Fry, N.; Hull, J.T.; Chowdhry, F.; Busse, G.D.; Melyan, Z.; Cutler, A.J.; Findling, R.L.; et al. A phase 3 placebo-controlled trial of once-daily 400-mg and 600-mg SPN-812 (viloxazine extended-release) in adolescents with ADHD. Psychopharmacol. Bull. 2021, 51, 43–64. [Google Scholar] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [PubMed]
- Nasser, A.; Hull, J.T.; Chaturvedi, S.A.; Liranso, T.; Odebo, O.; Kosheleff, A.R.; Fry, N.; Cutler, A.J.; Rubin, J.; Schwabe, S.; et al. A Phase III, Randomized, Double-Blind, Placebo-Controlled Trial Assessing the Efficacy and Safety of Viloxazine Extended-Release Capsules in Adults with Attention-Deficit/Hyperactivity Disorder. CNS Drugs 2022, 36, 897–915. [Google Scholar] [CrossRef]
- Goodman, D.; Faraone, S.V.; Adler, L.A.; Dirks, B.; Hamdani, M.; Weisler, R. Interpreting ADHD Rating Scale scores: Linking ADHD Rating Scale scores and CGI levels in two randomized controlled trials of lisdexamfetamine dimesylate in ADHD. Prim. Psychiatry 2010, 17, 44–52. [Google Scholar]
- Gajria, K.; Kosinski, M.; Sikirica, V.; Huss, M.; Livote, E.; Reilly, K.; Dittmann, R.W.; Erder, M.H. Psychometric validation of the Weiss Functional Impairment Rating Scale-Parent Report Form in children and adolescents with attention-deficit/hyperactivity disorder. Health Qual. Life Outcomes 2015, 13, 184. [Google Scholar] [CrossRef] [PubMed]
- Thompson, T.; Lloyd, A.; Joseph, A.; Weiss, M. The Weiss Functional Impairment Rating Scale-Parent Form for assessing ADHD: Evaluating diagnostic accuracy and determining optimal thresholds using ROC analysis. Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 2017, 26, 1879–1885. [Google Scholar] [CrossRef]
- Rink, L.; Adams, A.; Braun, C.; Bschor, T.; Kuhr, K.; Baethge, C. Dose-Response Relationship in Selective Serotonin and Norepinephrine Reuptake Inhibitors in the Treatment of Major Depressive Disorder: A Meta-Analysis and Network Meta-Analysis of Randomized Controlled Trials. Psychother. Psychosom. 2021, 91, 84–93. [Google Scholar] [CrossRef]
- Faison, S.L.; Fry, N.; Adewole, T.; Odebo, O.; Schwabe, S.; Wang, Z.; Maletic, V.; Nasser, A. Pharmacokinetics of Coadministered Viloxazine Extended-Release (SPN-812) and Methylphenidate in Healthy Adults. Clin. Drug Investig. 2020, 41, 149–159. [Google Scholar] [CrossRef]
- Wilens, T.E.; Gignac, M.; Swezey, A.; Monuteaux, M.C.; Biederman, J. Characteristics of Adolescents and Young Adults with ADHD Who Divert or Misuse Their Prescribed Medications. J. Am. Acad. Child Adolesc. Psychiatry 2006, 45, 408–414. [Google Scholar] [CrossRef] [PubMed]
- Kroutil, L.A.; Van Brunt, D.L.; Herman-Stahl, M.A.; Heller, D.C.; Bray, R.M.; Penne, M.A. Nonmedical use of prescription stimulants in the United States. Drug Alcohol Depend. 2006, 84, 135–143. [Google Scholar] [CrossRef]
- Moran, L.V.; Ongur, D.; Hsu, J.; Castro, V.M.; Perlis, R.H.; Schneeweiss, S. Psychosis with Methylphenidate or Amphetamine in Patients with ADHD. New Engl. J. Med. 2019, 380, 1128–1138. [Google Scholar] [CrossRef]
- Carlson, G.A.; Kelly, K.L. Stimulant rebound: How common is it and what does it mean? J. Child Adolesc. Psychopharmacol. 2003, 13, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.H.; Tsai, S.J. Treatment-resistant panic disorder: Clinical significance, concept and management. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2016, 70, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Mattingly, G.W.; Weisler, R.H.; Young, J.; Adeyi, B.; Dirks, B.; Babcock, T.; Lasser, R.; Scheckner, B.; Goodman, D.W. Clinical response and symptomatic remission in short- and long-term trials of lisdexamfetamine dimesylate in adults with attention-deficit/hyperactivity disorder. BMC Psychiatry 2013, 13, 39. [Google Scholar] [CrossRef]
- Newcorn, J.H.; Kratochvil, C.J.; Allen, A.J.; Casat, C.D.; Ruff, D.D.; Moore, R.J.; Michelson, D.; Atomoxetine/Methylphenidate Comparative Study Group. Atomoxetine and Osmotically Released Methylphenidate for the Treatment of Attention Deficit Hyperactivity Disorder: Acute Comparison and Differential Response. Am. J. Psychiatry 2008, 165, 721–730. [Google Scholar] [CrossRef]
- Faison, S.L.; Fry, N.M.; Adewole, T.; Odebo, O.; Wang, Z.; Maletic, V.; Nasser, A. Pharmacokinetics of Coadministered Viloxazine Extended-Release (SPN-812) and Lisdexamfetamine in Healthy Adults. J. Clin. Psychopharmacol. 2021, 41, 155–162. [Google Scholar] [CrossRef]
- Wang, Z.; Kosheleff, A.R.; Adeojo, L.W.; Odebo, O.; Adewole, T.; Qin, P.; Maletic, V.; Schwabe, S.; Nasser, A. Impact of Paroxetine, a Strong CYP2D6 Inhibitor, on SPN-812 (Viloxazine Extended-Release) Pharmacokinetics in Healthy Adults. Clin. Pharmacol. Drug Dev. 2021, 10, 1365–1374. [Google Scholar] [CrossRef] [PubMed]
- Cutler, A.J.; Mattingly, G.W. Beyond the pill: New medication delivery options for ADHD. CNS Spectr. 2017, 22, 463–474. [Google Scholar] [CrossRef] [PubMed]
| Study | Centers | Treatment Group (No. of Participants) | Male (%) | Mean Age ± SD (Year) | Study Period (Weeks) | Outcome Events |
|---|---|---|---|---|---|---|
| Nasser A et al., 2021 [26] (NCT03247556) | 27 | SPN-812 400 mg (99) vs. SPN-812 600 mg (97) vs. Placebo (96) | SPN-812 400 mg: 66.7 SPN-812 600 mg: 73.2 Placebo: 63.5 | SPN-812 400 mg: 14.0 ± 1.74 SPN-812 600 mg: 13.7 ± 1.52 Placebo: 13.8 ± 1.53 | 7 | a, b, c, d, e, f |
| Johnson et al., 2019 [18] (NCT02633527) | 32 | SPN-812 100 mg (45) vs. SPN-812 200 mg (46) vs. SPN-812 300 mg (47) vs. SPN-812 400 mg (44) vs. Placebo (24) | SPN-812 100 mg: 60.0 SPN-812 200 mg: 71.7 SPN-812 300 mg: 76.6 SPN-812 400 mg: 70.5 Placebo: 45.8 | SPN-812 100 mg: 8.2 ± 1.36 SPN-812 200 mg: 9.0 ± 1.36 SPN-812 300 mg: 9.0 ± 1.36 SPN-812 400 mg: 9.0 ± 1.36 Placebo: 8.9 ± 1.28 | 8 | a, e |
| Nasser A et al., 2021 [23] (NCT03247517) | 33 | SPN-812 200 mg (94) vs. SPN-812 400 mg (103) vs. Placebo (104) | SPN-812 200 mg: 70.2 SPN-812 400 mg: 65.0 Placebo: 55.8 | SPN-812 200 mg: 13.9 ± 1.48 SPN-812 400 mg: 14.0 ± 1.59 Placebo: 13.8 ± 1.60 | 6 | a, b, c, d, e, f |
| Nasser A et al., 2020 [24] (NCT03247530) | 34 | SPN-812 100 mg (147) vs. SPN-812 200 mg (158) vs. Placebo (155) | SPN-812 100 mg: 63.9 SPN-812 200 mg: 62.7 Placebo: 62.6 | SPN-812 100 mg: 8.5 ± 1.7 SPN-812 200 mg: 8.5 ± 1.7 Placebo: 8.5 ± 1.7 | 6 | a, b, c, d, e, f |
| Nasser A et al., 2021 [25] (NCT03247543) | 28 | SPN-812 200 mg (107) vs. SPN-812 400 mg (97) vs. Placebo (97) | SPN-812 200 mg: 69.2 SPN-812 400 mg: 60.8 Placebo: 62.9 | SPN-812 200 mg: 8.5 ± 1.7 SPN-812 400 mg: 8.4 ± 1.7 Placebo: 8.5 ± 1.7 | 8 | a, b, c, d, e, f |
| Outcomes | No. of Trials Contributing to the Meta-Analysis | No. of Participants Contributing to the Meta-Analysis | MD (95% CI)/RR [95% CI] | p Value | I2 (%) |
|---|---|---|---|---|---|
| 1. ADHD-RS-5 | |||||
| SPN-812 100 mg | 2 | 371 | −5.79 (−8.68, −2.90) | <0.0001 | 0 |
| SPN-812 200 mg | 4 | 785 | −6.10 (−8.10, −4.09) | <0.00001 | 0 |
| SPN-812 300 mg | 1 | 71 | −8.10 (−14.93, −1.27) | 0.02 | N/A |
| SPN-812 400 mg | 4 | 664 | −5.61 (−7.76, −3.46) | <0.00001 | 0 |
| SPN-812 600 mg | 1 | 193 | −3.50 (−7.34, 0.34) | 0.07 | N/A |
| 2. Number of patients with increased CGI-I score | |||||
| SPN-812 100 mg | 1 | 302 | 1.51 [1.12, 2.04] | 0.007 | N/A |
| SPN-812 200 mg | 3 | 715 | 1.57 [1.30, 1.88] | <0.00001 | 0 |
| SPN-812 400 mg | 3 | 596 | 1.58 [1.30, 1.91] | <0.00001 | 0 |
| SPN-812 600 mg | 1 | 193 | 1.38 [0.98, 1.95] | 0.07 | N/A |
| 3. Conners 3-PS | |||||
| SPN-812 100 mg | 1 | 302 | −4.30(−6.58, −2.02) | 0.0002 | N/A |
| SPN-812 200 mg | 3 | 715 | −3.13(−5.27, −1.00) | 0.004 | 49 |
| SPN-812 400 mg | 3 | 596 | −2.37(−3.93, −0.80) | 0.003 | 0 |
| SPN-812 600 mg | 1 | 193 | −1.30(−3.75, 1.15) | 0.30 | N/A |
| 4. WFIRS-P | |||||
| SPN-812 100 mg | 1 | 302 | −0.14 (−0.23, −0.05) | 0.002 | N/A |
| SPN-812 200 mg | 3 | 715 | −0.13 (−0.19, −0.07) | <0.0001 | 0 |
| SPN-812 400 mg | 3 | 596 | −0.10 (−0.16, −0.04) | 0.0008 | 0 |
| SPN-812 600 mg | 1 | 193 | 0.00 (−0.08, 0.08) | 1.00 | N/A |
| 5. AEs | |||||
| SPN-812 100 mg | 2 | 385 | 1.60 [1.25, 2.05] | 0.0002 | 0 |
| SPN-812 200 mg | 4 | 805 | 1.31 [1.11, 1.56] | 0.002 | 8 |
| SPN-812 300 mg | 1 | 72 | 1.50 [0.93, 2.41] | 0.09 | N/A |
| SPN-812 400 mg | 4 | 682 | 1.61 [1.21, 2.13] | 0.001 | 70 |
| SPN-812 600 mg | 1 | 196 | 1.81 [1.39, 2.36] | <0.00001 | N/A |
| 6. SAEs | |||||
| SPN-812 100 mg | 1 | 313 | 5.16 [0.25, 106.64] | 0.29 | N/A |
| SPN-812 200 mg | 3 | 733 | 3.61 [0.59, 22.00] | 0.16 | 0 |
| SPN-812 400 mg | 2 | 400 | 5.00 [0.59, 42.40] | 0.14 | 0 |
| Children (6–11 Years) | Adolescents (12–17 Years) | |||
|---|---|---|---|---|
| MD (95% CI)/RR [95% CI] | p Value | MD (95% CI)/RR [95% CI] | p Value | |
| Efficacy outcomes | ||||
| ADHD-RS-5 | −6.33 (−8.37, −4.30) | <0.00001 | −4.60 (−6.94, −2.25) | 0.0001 |
| Number of patients with increased CGI-I score | 1.50 [1.22, 1.83] | <0.0001 | 1.59 [1.28, 1.98] | <0.0001 |
| Conners 3-PS | −3.92 (−5.43, −2.40) | <0.00001 | −1.72 (−3.35, −0.09) | 0.04 |
| WFIRS-P | −0.14 (−0.20, −0.08) | <0.00001 | −0.07 (−0.13, −0.01) | 0.02 |
| Safety outcomes | ||||
| AEs | 1.40 [1.15, 1.71] | 0.0008 | 1.52 [1.24, 1.85] | <0.0001 |
| SAEs | 3.52 [0.44, 28.47] | 0.24 | 5.05 [0.59, 42.82] | 0.14 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tan, X.; Xu, Y.; Wang, S.; Li, J.; Hu, C.; Chen, Z.; Cheng, Q.; Wang, Z. Efficacy and Safety of SPN-812 (Extended-Release Viloxazine) in Children and Adolescents with Attention-Deficit/Hyperactivity Disorder: A Systematic Review and Meta-Analysis. Brain Sci. 2023, 13, 1627. https://doi.org/10.3390/brainsci13121627
Tan X, Xu Y, Wang S, Li J, Hu C, Chen Z, Cheng Q, Wang Z. Efficacy and Safety of SPN-812 (Extended-Release Viloxazine) in Children and Adolescents with Attention-Deficit/Hyperactivity Disorder: A Systematic Review and Meta-Analysis. Brain Sciences. 2023; 13(12):1627. https://doi.org/10.3390/brainsci13121627
Chicago/Turabian StyleTan, Xin, Yuejuan Xu, Shixin Wang, Jiaxuan Li, Chunxia Hu, Zhouqing Chen, Qingzhang Cheng, and Zhong Wang. 2023. "Efficacy and Safety of SPN-812 (Extended-Release Viloxazine) in Children and Adolescents with Attention-Deficit/Hyperactivity Disorder: A Systematic Review and Meta-Analysis" Brain Sciences 13, no. 12: 1627. https://doi.org/10.3390/brainsci13121627
APA StyleTan, X., Xu, Y., Wang, S., Li, J., Hu, C., Chen, Z., Cheng, Q., & Wang, Z. (2023). Efficacy and Safety of SPN-812 (Extended-Release Viloxazine) in Children and Adolescents with Attention-Deficit/Hyperactivity Disorder: A Systematic Review and Meta-Analysis. Brain Sciences, 13(12), 1627. https://doi.org/10.3390/brainsci13121627






