Inattention, Impulsivity, and Hyperactivity among Individuals with Self-Reported Impaired Wound Healing
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hamza, C.A.; Willoughby, T.; Heffer, T. Impulsivity and nonsuicidal self-injury: A review and meta-analysis. Clin. Psychol. Rev. 2015, 38, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Lalloo, R.; Sheiham, A. Risk factors for childhood major and minor head and other injuries in a nationally representative sample. Injury 2003, 34, 261–266. [Google Scholar] [CrossRef]
- Lalloo, R.; Sheiham, A.; Nazroo, J. Behavioural characteristics and accidents: Findings from the Health Survey for England, 1997. Accid. Anal. Prev. 2002, 35, 661–667. [Google Scholar] [CrossRef]
- Glania, T.; Lialiaris, T.; Tripsianis, G.; Papadakis, N.; Constandinidis, T.C. Is psychopathology related to children’s unintentional injury? Int. J. Adolesc. Med. Health 2010, 22, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Gayton, W.F.; Bailey, C.; Wagner, A.; Hardesty, V.A. Relationship between Childhood Hyperactivity and Accident Proneness. Percept. Mot. Ski. 1986, 63, 801–802. [Google Scholar] [CrossRef] [PubMed]
- Thompson, A.L.; Molina, B.S.; Pelham, W., Jr.; Gnagy, E.M. Risky driving in adolescents and young adults with childhood ADHD. J. Pediat. Psychol. 2007, 32, 745–759. [Google Scholar] [CrossRef] [Green Version]
- Pless, I.B.; Taylor, H.G.; Arsenault, L. The Relationship Between Vigilance Deficits and Traffic Injuries Involving Children. Pediatrics 1995, 95, 219–224. [Google Scholar] [CrossRef]
- Connolly, A.; Fielding, J.; Papadopoulos, N.; McGinley, J.; Murphy, A.; Rinehart, N.J. Factors associated with accidental injuries in children with ADHD–combined type: More than a motor problem? J. Atten. Disord. 2019, 23, 1320–1330. [Google Scholar] [CrossRef]
- Verster, J.C.; Bekker, E.M.; De Roos, M.; Minova, A.; Eijken, E.J.E.; Kooij, J.J.S.; Buitelaar, J.K.; Kenemans, J.L.; Verbaten, M.N.; Olivier, B.; et al. Methylphenidate significantly improves driving ability of adults with attention-deficit hyperactivity disorder: A randomized crossover trial. J. Psychopharmacol. 2008, 22, 230–239. [Google Scholar] [CrossRef] [Green Version]
- Fischer, M.; Barkley, R.A.; Smallish, L.; Fletcher, K. Hyperactive children as young adults: Driving abilities, safe driving behavior, and adverse driving outcomes. Accid. Anal. Prev. 2007, 39, 94–105. [Google Scholar] [CrossRef]
- Barkley, R.A.; Murphy, K.R.; Kwasnik, D. Motor Vehicle Driving Competencies and Risks in Teens and Young Adults with Attention Deficit Hyperactivity Disorder. Pediatrics 1996, 98, 1089–1095. [Google Scholar] [CrossRef] [PubMed]
- Aduen, P.A.; Kofler, M.J.; Sarver, D.E.; Wells, E.; Soto, E.F.; Cox, D.J. ADHD, depression, and motor vehicle crashes: A prospective cohort study of continuously-monitored, real-world driving. J. Psychiatr. Res. 2018, 101, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Kaya, A.; Taner, Y.; Guclu, B.; Taner, E.; Kaya, Y.; Bahcivan, H.G.; Benli, I.T. Trauma and Adult Attention Deficit Hyperactivity Disorder. J. Int. Med. Res. 2008, 36, 9–16. [Google Scholar] [CrossRef] [PubMed]
- El Farouki, K.; Lagarde, E.; Orriols, L.; Bouvard, M.-P.; Contrand, B.; Galera, C. The Increased Risk of Road Crashes in Attention Deficit Hyperactivity Disorder (ADHD) Adult Drivers: Driven by Distraction? Results from a Responsibility Case-Control Study. PLoS ONE 2014, 9, e115002. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Narad, M.; Garner, A.A.; Brassell, A.A.; Saxby, D.; Antonini, T.N.; O’Brien, K.M.; Tamm, L.; Matthews, G.; Epstein, J.N. Impact of Distraction on the Driving Performance of Adolescents with and without Attention-Deficit/Hyperactivity Disorder. JAMA Pediatr. 2013, 167, 933–938. [Google Scholar] [CrossRef]
- Kittel-Schneider, S.; Wolff, S.; Queiser, K.; Wessendorf, L.; Meier, A.M.; Verdenhalven, M.; Brunkhorst-Kanaan, N.; Grimm, O.; McNeill, R.; Grabow, S.; et al. Prevalence of ADHD in Accident Victims: Results of the PRADA Study. J. Clin. Med. 2019, 8, 1643. [Google Scholar] [CrossRef] [Green Version]
- Bartoli, F.; Callovini, T.; Cavaleri, D.; Cioni, R.M.; Bachi, B.; Calabrese, A.; Moretti, F.; Canestro, A.; Morreale, M.; Nasti, C.; et al. Clinical correlates of comorbid attention deficit hyperactivity disorder in adults suffering from bipolar disorder: A meta-analysis. Aust. N. Z. J. Psychiatry, 2022; in press. [Google Scholar] [CrossRef]
- Pan, P.-Y.; Bölte, S. The association between ADHD and physical health: A co-twin control study. Sci. Rep. 2020, 10, 22388. [Google Scholar] [CrossRef]
- van der Schans, J.; Çiçek, R.; de Vries, T.W.; Hak, E.; Hoekstra, P.J. Association of atopic diseases and attention-deficit/hyperactivity disorder: A systematic review and meta-analyses. Neurosci. Biobehav. Rev. 2017, 74, 139–148. [Google Scholar] [CrossRef]
- Cortese, S.; Sun, S.; Zhang, J.; Sharma, E.; Chang, Z.; Kuja-Halkola, R.; Almqvist, C.; Larsson, H.; Faraone, S.V. Association between attention deficit hyperactivity disorder and asthma: A systematic review and meta-analysis and a Swedish population-based study. Lancet Psychiatry 2018, 5, 717–726. [Google Scholar] [CrossRef]
- Prehn-Kristensen, A.; Zimmermann, A.; Tittmann, L.; Lieb, W.; Schreiber, S.; Baving, L.; Fischer, A. Reduced microbiome alpha diversity in young patients with ADHD. PLoS ONE 2018, 13, e0200728. [Google Scholar] [CrossRef] [PubMed]
- Herpertz-Dahlmann, B.; Seitz, J.; Baines, J. Food matters: How the microbiome and gut–brain interaction might impact the development and course of anorexia nervosa. Eur. Child Adolesc. Psychiatry 2017, 26, 1031–1041. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rieder, R.; Wisniewski, P.J.; Alderman, B.L.; Campbell, S.C. Microbes and mental health: A review. Brain Behav. Immun. 2017, 66, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Santocchi, E.; Guiducci, L.; Fulceri, F.; Billeci, L.; Buzzigoli, E.; Apicella, F.; Calderoni, S.; Grossi, E.; Morales, M.A.; Muratori, F. Gut to brain interaction in Autism Spectrum Disorders: A randomized controlled trial on the role of probiotics on clinical, biochemical and neurophysiological parameters. BMC Psychiatry 2016, 16, 183. [Google Scholar] [CrossRef] [Green Version]
- Sfera, A.; Osorio, C.; Inderias, L.A.; Parker, V.; Price, A.I.; Cummings, M. The Obesity–Impulsivity Axis: Potential Metabolic Interventions in Chronic Psychiatric Patients. Front. Psychiatry 2017, 8, 20. [Google Scholar] [CrossRef] [Green Version]
- Wallace, C.J.K.; Milev, R. The effects of probiotics on depressive symptoms in humans: A systematic review. Ann. Gen. Psychiatry 2017, 16, 14. [Google Scholar] [CrossRef] [Green Version]
- Balikji, J.; Hoogbergen, M.M.; Garssen, J.; Verster, J.C. The Association of Irritable Bowel Complaints and Perceived Immune Fitness among Individuals That Report Impaired Wound Healing: Supportive Evidence for the Gut–Brain–Skin Axis. Gastroenterol. Insights 2021, 12, 423–432. [Google Scholar] [CrossRef]
- Salem, I.; Ramser, A.; Isham, N.; Ghannoum, M.A. The Gut Microbiome as a Major Regulator of the Gut-Skin Axis. Front. Microbiol. 2018, 9, 1459. [Google Scholar] [CrossRef] [Green Version]
- Balikji, J.; Hoogbergen, M.M.; Garssen, J.; Verster, J.C. Self-Reported Impaired Wound Healing in Young Adults and Their Susceptibility to Experiencing Immune-Related Complaints. J. Clin. Med. 2022, 11, 980. [Google Scholar] [CrossRef]
- Cortese, S.; Moreira-Maia, C.R.; Fleur, D.S.; Morcillo-Peñalver, C.; Rohde, L.A.; Faraone, S.V. Association Between ADHD and Obesity: A Systematic Review and Meta-Analysis. Am. J. Psychiatry 2016, 173, 34–43. [Google Scholar] [CrossRef]
- Sen, C.K.; Gordillo, G.M.; Roy, S.; Kirsner, R.; Lambert, L.; Hunt, T.K.; Gottrup, F.; Gurtner, G.C.; Longaker, M.T. Human skin wounds: A major and snowballing threat to public health and the economy. Wound Repair Regen. 2009, 17, 763–771. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Erfurt-Berge, C.; Ronicke, M.; Richter-Schmidinger, T.; Walther, F.; Renner, R. Quality of life assessment in family members of patients with chronic wounds. Eur. J. Dermatol. 2019, 29, 484–489. [Google Scholar] [CrossRef] [PubMed]
- Balikji, J.; Hoogbergen, M.M.; Garssen, J.; Verster, J.C. Mental Resilience, Mood, and Quality of Life in Young Adults with Self-Reported Impaired Wound Healing. Int. J. Environ. Res. Public Health 2022, 19, 2542. [Google Scholar] [CrossRef] [PubMed]
- Green, J.; Jester, R. Health-related quality of life and chronic venous leg ulceration: Part 1. Br. J. Community Nurs. 2009, 14, S12–S17. [Google Scholar] [CrossRef]
- Nogueira, G.S.; Zanin, C.R.; Miyazaki, M.C.O.S.; De Godoy, J.M.P. Venous Leg Ulcers and Emotional Consequences. Int. J. Low. Extremity Wounds 2009, 8, 194–196. [Google Scholar] [CrossRef]
- Wiechman, S.; Kalpakjian, C.Z.; Johnson, K.L. Measuring depression in adults with burn injury: A systematic review. J. Burn Care Res. 2016, 37, e415–e426. [Google Scholar] [CrossRef] [Green Version]
- Zhou, K.; Jia, P. Depressive symptoms in patients with wounds: A cross-sectional study. Wound Repair Regen. 2016, 24, 1059–1065. [Google Scholar] [CrossRef]
- Herber, O.R.; Schnepp, W.; Rieger, M.A. A systematic review on the impact of leg ulceration on patients’ quality of life. Health Qual. Life Outcomes 2007, 5, 44. [Google Scholar] [CrossRef] [Green Version]
- Poerio, G.L.; Totterdell, P.; Miles, E. Mind-wandering and negative mood: Does one thing really lead to another? Conscious. Cogn. 2013, 22, 1412–1421. [Google Scholar] [CrossRef] [Green Version]
- Otten, L.; De Kruijff, D.; Mackus, M.; Garssen, J.; Verster, J. Attention deficit hyperactivity disorder (ADHD) and the dietary intake of fiber and fat. Eur. Neuropsychopharmacol. 2016, 26, S726. [Google Scholar] [CrossRef]
- Kooij, J.S.; Boonstra, A.M.; Swinkels, S.; Bekker, E.M.; de Noord, I.; Buitelaar, J.K. Reliability, Validity, and Utility of Instruments for Self-Report and Informant Report Concerning Symptoms of ADHD in Adult Patients. J. Atten. Disord. 2008, 11, 445–458. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar] [CrossRef]
- Lantman, M.V.S.; Mackus, M.; Otten, L.S.; de Kruijff, D.; van de Loo, A.J.; Kraneveld, A.D.; Garssen, J.; Verster, J.C. Mental resilience, perceived immune functioning, and health. J. Multidiscip. Healthc. 2017, 10, 107–112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilod Versprille, L.J.F.; van de Loo, A.J.A.E.; Mackus, M.; Arnoldy, L.; Sulzer, T.A.L.; Vermeulen, S.A.; Abdulahad, S.; Huls, H.; Baars, T.; Scholey, A.; et al. Development and Validation of the Immune Status Questionnaire (ISQ). Int. J. Environ. Res. Public Health 2019, 16, 4743. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brunkhorst-Kanaan, N.; Libutzki, B.; Reif, A.; Larsson, H.; McNeill, R.V.; Kittel-Schneider, S. ADHD and accidents over the life span—A systematic review. Neurosci. Biobehav. Rev. 2021, 125, 582–591. [Google Scholar] [CrossRef]
- Firouzabadi, F.D.; Ramezanpour, S.; Firouzabadi, M.D.; Yousem, I.J.; Puts, N.A.J.; Yousem, D.M. Neuroimaging in Attention-Deficit/Hyperactivity Disorder: Recent Advances. Am. J. Roentgenol. 2022, 218, 321–332. [Google Scholar] [CrossRef]
| Control Group (N = 575) | IWH Group (N = 198) | p-Value | |
|---|---|---|---|
| Sex (m/f) (%) | 40.7/59.3 | 29.7/70.3 | 0.008 * |
| Age | 21.6 (2.7) | 21.0 (2.4) | 0.008 * |
| BMI (kg/m2) | 22.2 (2.9) | 22.2 (2.6) | 0.897 |
| Alcohol consumption (% yes) | 81.6% | 82.2% | 0.693 |
| Number of drinks per week 1 | 7.3 (8.7) | 8.7 (12.4) | 0.079 |
| Smoking (% yes) | 12.6% | 12.6% | 0.233 |
| Perceived immune fitness | 7.8 (1.2) | 7.5 (1.2) | <0.001 * |
| Reduced immune fitness (%) | 21.9% | 34.9% | 0.002 * |
| Diagnosed ADHD (%) | 3.0% | 4.5% | 0.359 |
| Control Group | IWH Group | p-Value | |
|---|---|---|---|
| ADHD Rating Scale overall score | 14.2 (6.8) | 16.8 (7.4) | <0.001 * |
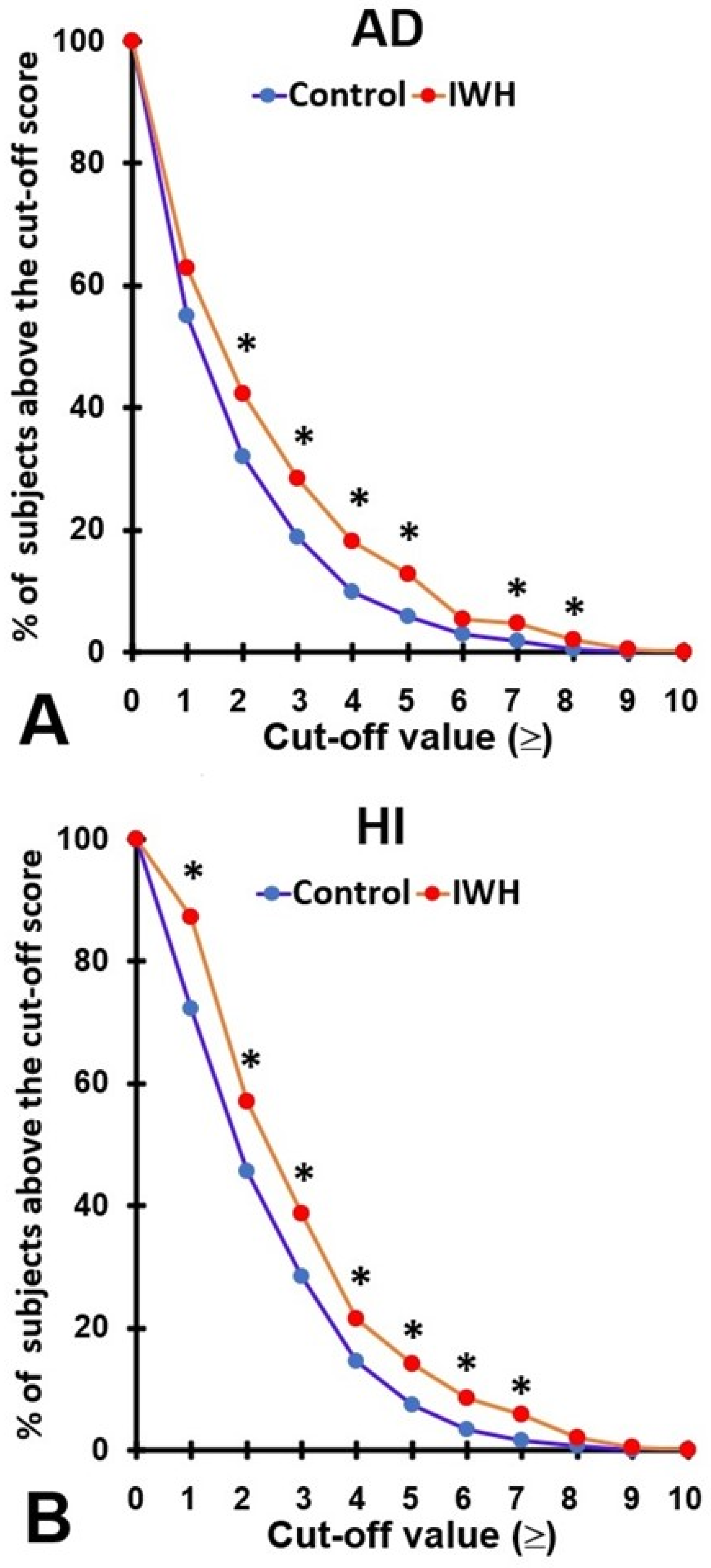
| Attention deficit subscale | 1.3 (1.6) | 1.8 (2.1) | 0.001 * |
| AD% ≥ 4, Kooij et al. [41] | 9.9% | 18.2% | 0.003 * |
| AD% ≥ 5, DSM-5 [42] | 5.8% | 12.8% | 0.002 * |
| Hyperactivity, impulsivity subscale | 1.7 (1.7) | 2.4 (2.0) | <0.001 * |
| HI% ≥ 4, Kooij et al. [41] | 14.6% | 21.5% | 0.028 * |
| HI% ≥ 5, DSM-5 [42] | 7.4% | 14.0% | 0.007 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Balikji, J.; Hoogbergen, M.M.; Garssen, J.; Verster, J.C. Inattention, Impulsivity, and Hyperactivity among Individuals with Self-Reported Impaired Wound Healing. Brain Sci. 2022, 12, 961. https://doi.org/10.3390/brainsci12080961
Balikji J, Hoogbergen MM, Garssen J, Verster JC. Inattention, Impulsivity, and Hyperactivity among Individuals with Self-Reported Impaired Wound Healing. Brain Sciences. 2022; 12(8):961. https://doi.org/10.3390/brainsci12080961
Chicago/Turabian StyleBalikji, Jessica, Maarten M. Hoogbergen, Johan Garssen, and Joris C. Verster. 2022. "Inattention, Impulsivity, and Hyperactivity among Individuals with Self-Reported Impaired Wound Healing" Brain Sciences 12, no. 8: 961. https://doi.org/10.3390/brainsci12080961
APA StyleBalikji, J., Hoogbergen, M. M., Garssen, J., & Verster, J. C. (2022). Inattention, Impulsivity, and Hyperactivity among Individuals with Self-Reported Impaired Wound Healing. Brain Sciences, 12(8), 961. https://doi.org/10.3390/brainsci12080961







