Quantitative Distribution of Cerebral Venous Oxygen Saturation and Its Prognostic Value in Patients with Acute Ischemic Stroke
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. MR Examinations
2.3. Quantitative Distribution of SvO2
2.3.1. Theory of Measuring SvO2
2.3.2. Reconstructed QSM
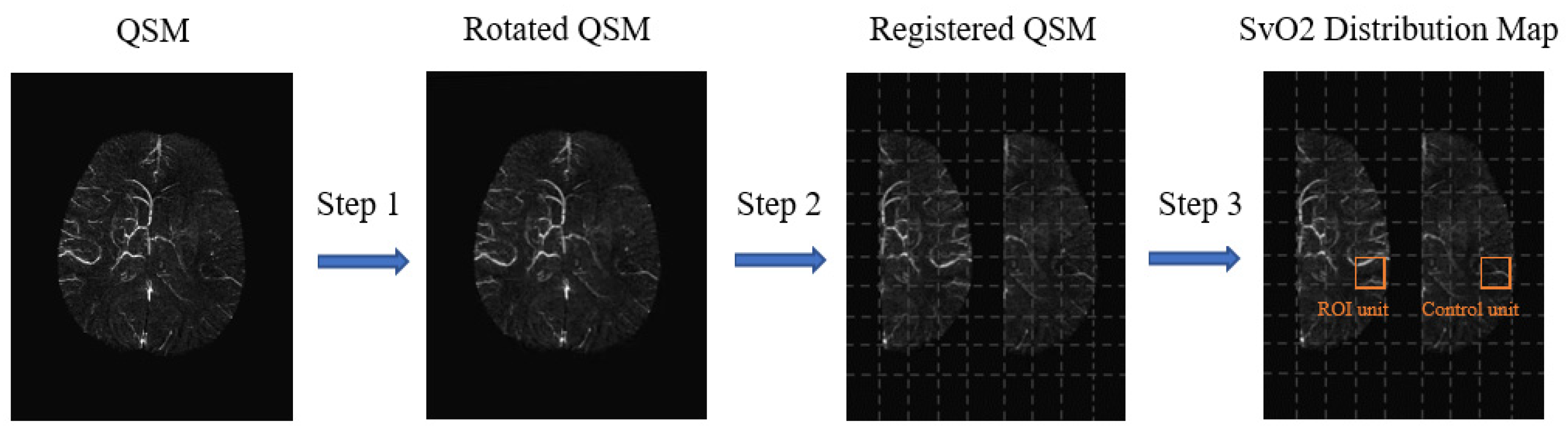
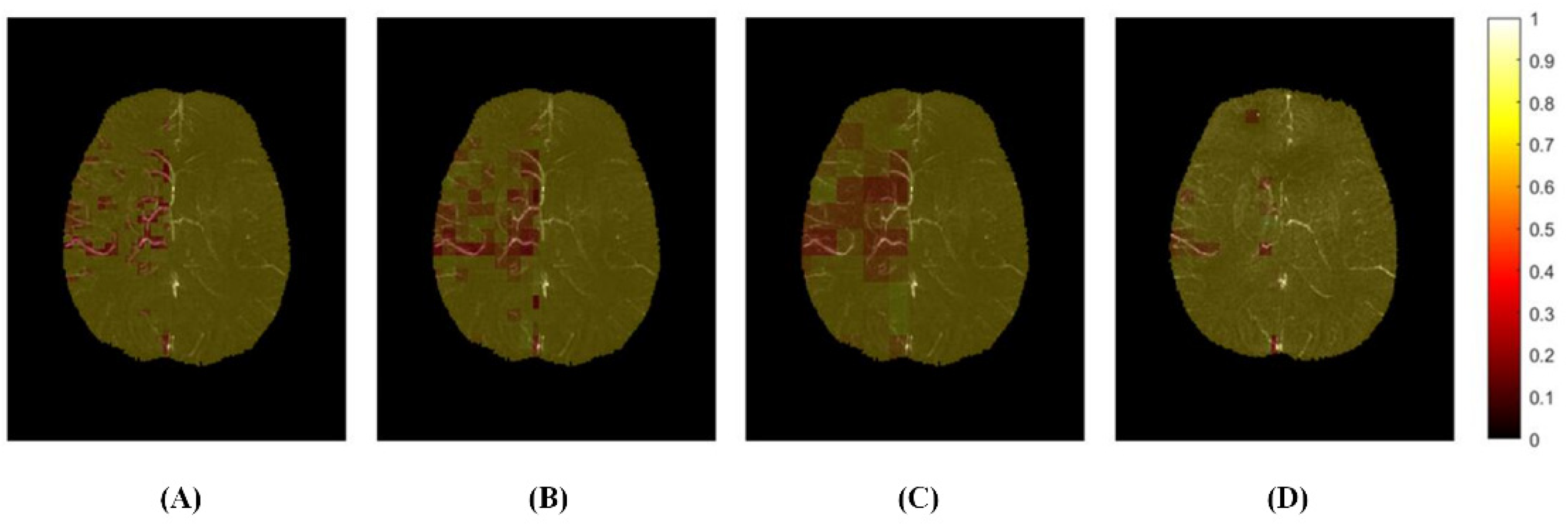
2.3.3. Generated Distribution Map
2.3.4. Parameters
2.4. Evaluated
2.4.1. Calculated Cerebral SvO2
2.4.2. Statistical Analysis
3. Results
3.1. Clinical Factors
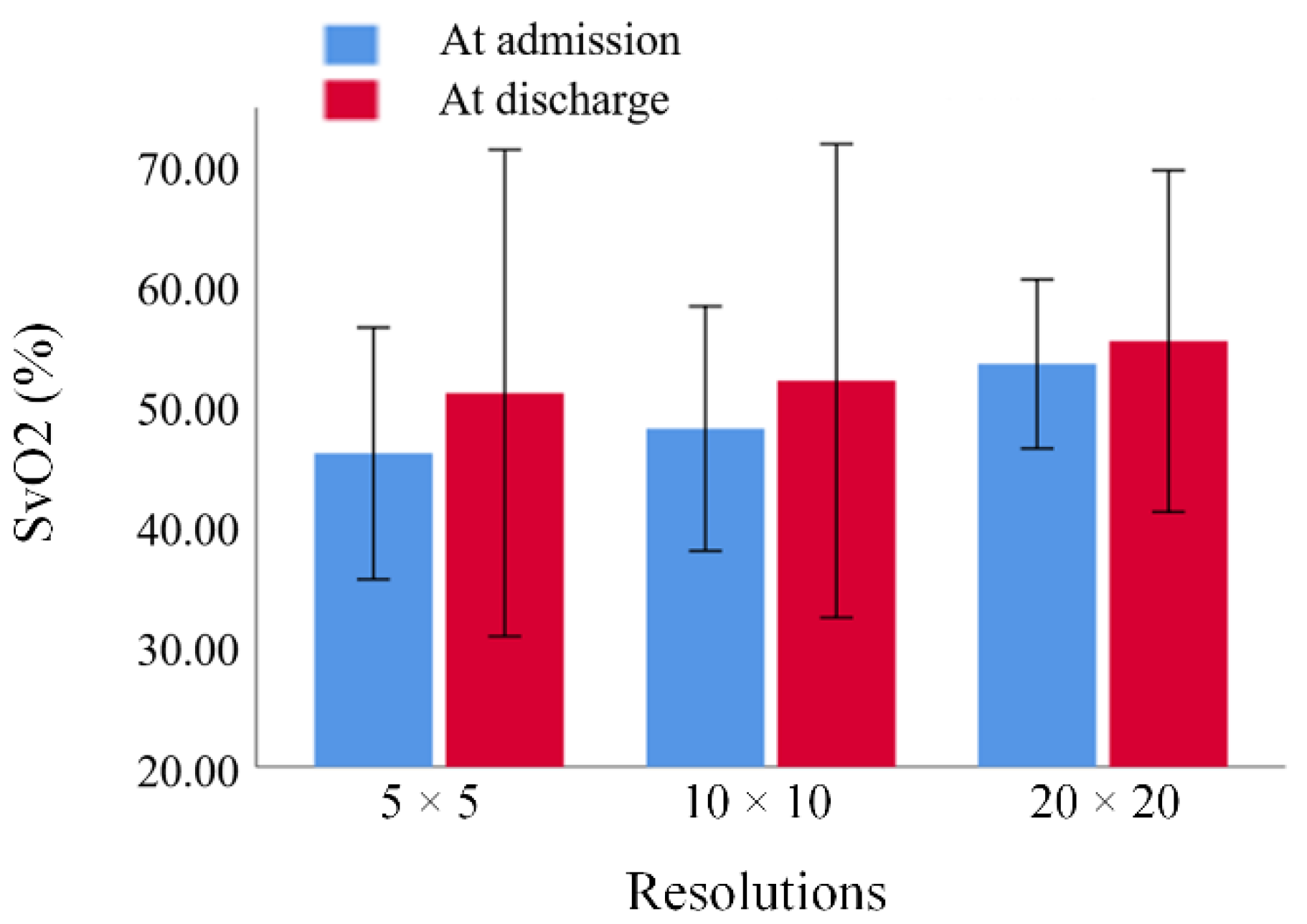
3.2. Comparison of SvO2 in Hypoxic Regions between Different Resolutions
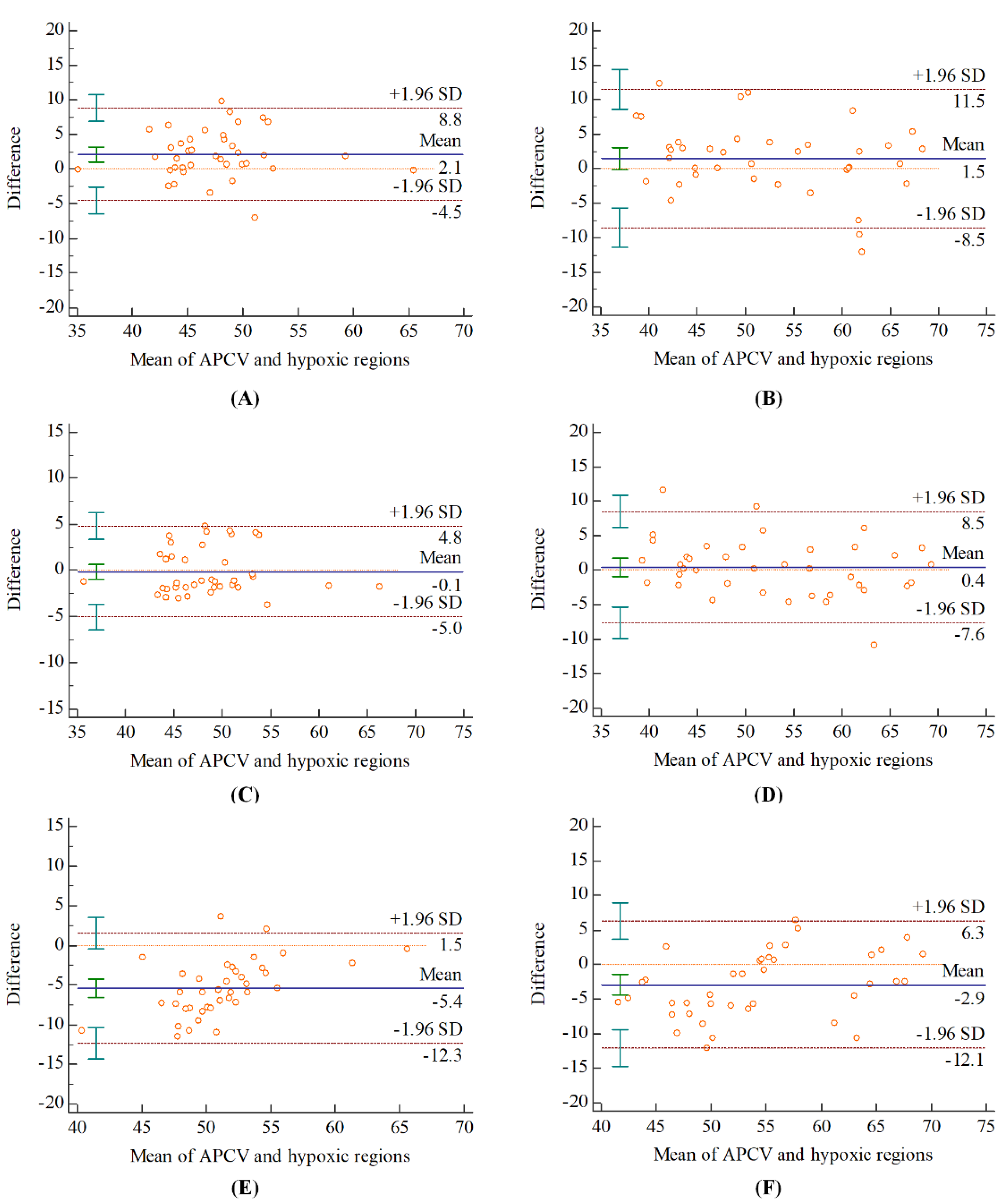
3.3. Agreement on SvO2 between Different Regions
3.4. Correlation between SvO2 and Clinical Scores
3.5. Association between SvO2 and Prognosis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wang, W.; Jiang, B.; Sun, H.; Ru, X.; Sun, D.; Wang, L.; Jiang, Y.; Li, Y.; Wang, Y.; Chen, Z.; et al. Prevalence, incidence, and mortality of stroke in China. Circulation 2017, 135, 759–771. [Google Scholar] [CrossRef] [PubMed]
- Vilela, P.; Rowley, H.A. Brain ischemia: CT and MRI techniques in acute ischemic stroke. Eur. J. Radiol. 2017, 96, 162–172. [Google Scholar] [CrossRef] [PubMed]
- Leigh, R.; Knutsson, L.; Zhou, J.; Zijil, P.C. Imaging the physiological evolution of the ischemic penumbra in acute ischemic stroke. J. Cereb. Blood Flow Metab. 2018, 38, 1500–1516. [Google Scholar] [CrossRef]
- An, H.; Ford, A.L.; Vo, K.D.; Liu, Q.; Chen, Y.; Lee, J.; Lin, W. Imaging oxygen metabolism in acute stroke using MRI. Curr. Radiol. Rep. 2014, 2, 39. [Google Scholar] [CrossRef]
- Iwata, T.; Mori, T.; Tanno, Y.; Kasakura, S.; Yoshioka, K. Measurement of oxygen extraction fraction by bloodsampling to estimate severe cerebral hemodynamic failure and anticipate cerebral hyperperfusion syndrome following carotid artery stenting. J. Neurointerv. Surg. 2018, 10, 1063–1066. [Google Scholar] [CrossRef] [PubMed]
- Kesavadas, C.; Santhosh, K.; Thomas, B. Susceptibility weighted imaging in cerebral hypoperfusion-can we predict increased oxygen extraction fraction? Neuroradiology 2010, 52, 1047–1054. [Google Scholar] [CrossRef] [PubMed]
- Jones, B.T. Oxygen metabolism, oxygen extraction and positron emission tomography: Historical perspective and impact on basic and clinical neuroscience. Neurolmage 2012, 61, 492–504. [Google Scholar] [CrossRef]
- Barhoum, S.; Rodgers, Z.B.; Langham, M.; Magland, J.F.; Li, C.; Wehrli, F.W. Comparison of MRI methods for measuring whole-brain venous oxygen saturation. Magn. Reason. Med. 2015, 73, 2122–2128. [Google Scholar] [CrossRef]
- Chiarelli, P.A.; Bulte, D.P.; Wise, R.; Gallichan, D.; Jezzard, P. A calibration method for quantitative BOLD fMRI based on hyperoxia. Neuroimage 2007, 37, 808–820. [Google Scholar] [CrossRef]
- Chen, J.J.; Pike, G.B. Global cerebral oxidative metabolism during hypercapnia and hypocapnia in humans: Implications for BOLD fMRI. J. Cereb. Blood Flow Metab. 2010, 30, 1094–1099. [Google Scholar] [CrossRef]
- Halani, S.; Kwinta, J.B.; Golestani, A.M.; Khatamian, Y.B.; Chen, J.J. Comparing cerebrovascular reactivity measured using BOLD and cerebral blood flow MRI: The effect of basal vascular tension on vasodilatory and vasoconstrictive reactivity. Neuroimage 2015, 110, 110–123. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Ge, Y. Quantitative evaluation of oxygenation in venous vessels using T2-Relaxation-Under-Spin-Tagging MRI. Magn. Reason. Med. 2008, 60, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Krishnamurthy, L.C.; Liu, P.; Ge, Y.; Lu, H. Vessel-specific measurement of blood oxygenation with T2-Relaxation-Under-Phase-Contrast (TRU-PC) MRI. Magn. Res. Med. 2014, 71, 978–989. [Google Scholar] [CrossRef] [PubMed]
- Haacke, E.M.; Tang, J.; Neelavalli, J.; Cheng, Y.C.N. Susceptibility mapping as a means to visualize veins and quantify oxygen saturation. J. Magn. Reason. Imaging 2010, 32, 663–676. [Google Scholar] [CrossRef]
- Langkammer, C.; Schweser, F.; Krebs, N.; Deistung, A.; Goessler, W.; Scheurer, E.; Sommer, K.; Reishofer, G.; Yen, K.; Fazekas, F.; et al. Quantitative susceptibility mapping (QSM) as a means to measure brain iron? A post mortem validation study. Neuroimage 2012, 62, 1593–1599. [Google Scholar] [CrossRef]
- Doshi, H.; Wiseman, N.; Liu, J.; Wang, W.; Welch, R.D.; O’Neil, B.J.; Zuk, C.; Wang, X.; Mika, V.; Szaflarski, J.P.; et al. Cerebral hemodynamic changes of mild traumatic brain injury at the acute stage. PLoS ONE 2015, 10, e0127487. [Google Scholar] [CrossRef]
- Buch, S.; Ye, Y.; Haacke, E.M. Quantifying the changes in oxygen extraction fraction and cerebral activity caused by caffeine and acetazolamide. J. Cereb. Blood Flow Metab. 2017, 37, 825–836. [Google Scholar] [CrossRef]
- Neelavalli, J.; Jella, P.K.; Krishnamurthy, U.; Buch, S.; Haacke, E.M.; Yeo, L.; Mody, S.; Katkuri, Y.; Bahado-Singh, R.; Hassan, S.S.; et al. Measuring venous blood oxygenation in fetal brain using susceptibility weighted imaging. J. Magn. Reson. Imaging 2014, 39, 998–1006. [Google Scholar] [CrossRef]
- Zuo, C.; Chai, C.; Xia, S. Preliminary study of cerebral venous oxygen saturation in healthy people using MR quantitative susceptibility mapping. Chin. J. Radiol. 2016, 50, 1005–1201. [Google Scholar] [CrossRef]
- Hsieh, M.C.; Tsai, C.Y.; Liao, M.C.; Yang, J.L.; Su, C.H.; Chen, J.H. Quantitative susceptibility mapping-based microscopy of magnetic resonance venography (QSM-mMRV) for in vivo morphologically and functionally assessing cerebromicrovasculature in rat stroke model. PLoS ONE 2016, 11, e0149602. [Google Scholar] [CrossRef]
- Xia, S.; Utriainen, D.; Tang, J.; Kou, Z.; Zheng, G.; Wang, X.; Shen, W.; Haacke, E.M.; Lu, G. Decreased oxygen saturation in asymmetrically prominent cortical veins in patients with cerebral ischemic stroke. Magn. Reson. Imaging 2014, 32, 1272–1276. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Gong, Z.; Zhou, Y.; Chang, B.; Chai, C.; Liu, T.; Han, Y.; Wang, M.; Qian, T.; Haacke, E.M.; et al. Increased susceptibility of asymmetrically prominent cortical veins correlates with misery perfusion in patients with occlusion of the middle cerebral artery. Eur. Radiol. 2017, 27, 2381–2390. [Google Scholar] [CrossRef] [PubMed]
- Haacke, E.M.; Song, L.; Reichenbach, J.R.; Kuppusamy, K.; Hoogenraad, F.G.; Takeichi, H.; Lin, W. In vivo measurement of blood oxygen saturation using magnetic resonance imaging: A direct validation of the blood oxygen level-dependent concept in functional brain imaging. Hum. Brain Mapp. 1997, 5, 341–346. [Google Scholar] [CrossRef]
- Jain, V.; Langham, M.C.; Wehrli, F.W. MRI estimation of global brain oxygen consumption rate. J. Cereb. Blood Flow Metab. 2010, 30, 1598–1607. [Google Scholar] [CrossRef] [PubMed]
- Yamauchi, H.; Okazawa, H.; Kishibe, Y.; Sugimoto, K.; Takahashi, M. The effect of acetazolamide on the changes of cerebral blood flow and oxygen metabolism during visual stimulation. Neuroimage 2003, 20, 543–549. [Google Scholar] [CrossRef]
- Fernández-Seara, M.A.; Techawiboonwong, A.; Detre, J.A.; Wehrli, F.W. MR susceptometry for measuring global brain oxygen extraction. Magn. Reason. Med. 2010, 55, 967–973. [Google Scholar] [CrossRef] [PubMed]
- Abdul-Rahman, H.S.; Gdeisat, M.A.; Burton, D.R.; Lalor, M.J.; Lilley, F.; Moore, C.J. Fast and robust three-dimensional best path phase unwrapping algorithm. Appl. Opt. 2007, 46, 6623–6635. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Wilman, A.H. Background field removal using spherical mean value filtering and Tikhonov regularization. Magn. Reason. Med. 2014, 71, 1151–1157. [Google Scholar] [CrossRef]
- Shmueli, K.; Zwart, J.; Gelderen, P.V.; Li, T.Q.; Dodd, S.J.; Duyn, J.H. Magnetic susceptibility mapping of brain tissue in vivo using MRI phase data. Magn. Reason. Med. 2009. [Google Scholar] [CrossRef]
- Haacke, E.M.; Xu, Y.; Cheng, Y.C.N.; Reichenbach, J.R. Susceptibility weighted imaging (SWI). Magn. Reason. Med. 2004, 52, 612–618. [Google Scholar] [CrossRef]
- Bilgic, B.; Pfefferbaum, A.; Rohlfing, T.; Sullivan, E.V.; Adalsteinsson, E. MRI estimates of brain iron concentration in normal aging using quantitative susceptibility mapping. Neuroimage 2012, 59, 2625–2635. [Google Scholar] [CrossRef] [PubMed]
- Kimura, K.; Sakamoto, Y.; Aoki, J. The extension of time window until 4.5 h and development of MRI in t-PA patients. Rinsho. Shinkeigaku 2011, 51, 1174–1176. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Luo, Y.; Fawaz, M.; Zhu, C.; Chai, C.; Wu, G.; Wang, H.; Liu, J.; Zou, Y.; Gong, Y.; et al. Dynamic changes of asymmetric cortical veins relate to neurologic prognosis in acute ischemic stroke. Radiology 2021, 28, 672–681. [Google Scholar] [CrossRef] [PubMed]
- Kao, H.W.; Tsai, F.Y.; Hasso, A.N. Predicting stroke evolution: Comparison of susceptibility-weighted MR imaging with MR perfusion. Eur. Radiol. 2012, 22, 1397–1403. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Jing, L.; Zhao, M. Baseline cerebral ischemic core quantified by different automatic software and its predictive value for clinical outcome. Front. Neurosci. 2021, 15. [Google Scholar] [CrossRef]
- Knigsberg, A.; Demarco, A.T.; Mayer, C.; Wouters, A.; Cheng, B. Influence of stroke infarct location on quality of life assessed in a multivariate lesion-symptom mapping study. Sci. Rep. 2021, 11, 13490. [Google Scholar] [CrossRef]
- Buschmann, I.; Schaper, W. The pathophysiology of the collateral circulation (arteriogenesis). J. Pathol. 2015, 190, 338–342. [Google Scholar] [CrossRef]

| Factors | ALL (n = 39) | Favorable (n = 27) | Unfavorable (n = 12) | p |
|---|---|---|---|---|
| Age(years) | 70.0 ± 10.5 | 68.9 ± 11.0 | 72.7 ± 9.1 | 0.299 |
| Sex(male) | 27 (69.2%) | 20 (74.1%) | 7 (58.3%) | 0.326 |
| Hypertension | 30 (76.9%) | 22 (81.5%) | 8 (66.7%) | 0.311 |
| Diabetes | 15 (38.5%) | 7 (25.9%) | 8 (66.7%) | 0.016 |
| Atrial fibrillation | 11 (28.2%) | 9 (33.3%) | 2 (16.7%) | 0.286 |
| NIHSS 1 | 6.2 ± 5.7 | 5.8 ± 5.9 | 7.2 ± 5.5 | 0.492 |
| Resolution (mm3) | At Admission | At Discharge |
|---|---|---|
| 3.59 × 3.59 × 1.6 | 0.741, 95% CI 1: 0.435–0.875 | 0.852, 95% CI: 0.733–0.920 |
| 7.18 × 7.18 × 1.6 | 0.879, 95% CI: 0.782–0.935 | 0.906, 95% CI: 0.828–0.949 |
| 14.36 × 14.36 × 1.6 | 0.412, 95% CI: −0.103–0.740 | 0.784, 95% CI:0.509–0.898 |
| Clinical Scores | At Admission | At Discharge | Changes | |||
|---|---|---|---|---|---|---|
| Spearman | 1-β 4 | Spearman | 1-β | Spearman | 1-β | |
| NIHSS (1) 1 | −0.452 ** | 0.842 | 0.140 | 0.136 | 0.335 | 0.562 |
| NIHSS (2) | −0.246 | 0.330 | −0.507 ** | 0.924 | −0.353 * | 0.611 |
| ΔNIHSS 2 | 0.384 | 0.691 | −0.531 ** | 0.945 | −0.661 ** | 0.997 |
| 90-day mRS 3 | −0.177 | 0.190 | −0.619 ** | 0.992 | −0.463 ** | 0.862 |
| Parameter | Spearman | 1-β 3 | |
|---|---|---|---|
| 90-day mRS | NIHSS (1) 1 | 0.217 | 0.266 |
| NIHSS (2) | 0.770 ** | 0.999 | |
| ΔNIHSS 2 | −0.379 * | 0.679 | |
| MRI measurement | |||
| Infarct volume (1) | 0.149 | 0.148 | |
| Infarct volume (2) | 0.547 ** | 0.962 | |
| Δ Infarct volume | −0.525 ** | 0.943 | |
| Hypoperfusion volume (1) | −0.108 | 0.100 | |
| Hypoperfusion volume (2) | 0.284 | 0.425 | |
| Δ Hypoperfusion volume | −0.012 | 0.051 | |
| Hypoxia volume (1) | 0.121 | 0.113 | |
| Hypoxia volume (2) | 0.125 | 0.118 | |
| Δ Hypoxia volume | −0.023 | 0.052 |
| Indicators | Univariate Logistic Regression | Multivariate Logistic Regression | ||||
|---|---|---|---|---|---|---|
| OR 3 | 95% CI 4 | p | OR | 95% CI | p | |
| SvO2 (1) 1 | 0.951 | 0.822–1.101 | 0.500 | 0.950 | 0.818–1.104 | 0.504 |
| SvO2 (2) 1 | 0.849 | 0.757–0.952 | 0.005 | 0.812 | 0.701–0.941 | 0.006 |
| ΔSvO2 2 | 0.902 | 0.831–0.980 | 0.015 | 0.886 | 0.804–0.975 | 0.013 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cao, F.; Wang, M.; Han, S.; Fan, S.; Guo, Y.; Yang, Y.; Luo, Y.; Guo, J.; Kang, Y. Quantitative Distribution of Cerebral Venous Oxygen Saturation and Its Prognostic Value in Patients with Acute Ischemic Stroke. Brain Sci. 2022, 12, 1109. https://doi.org/10.3390/brainsci12081109
Cao F, Wang M, Han S, Fan S, Guo Y, Yang Y, Luo Y, Guo J, Kang Y. Quantitative Distribution of Cerebral Venous Oxygen Saturation and Its Prognostic Value in Patients with Acute Ischemic Stroke. Brain Sciences. 2022; 12(8):1109. https://doi.org/10.3390/brainsci12081109
Chicago/Turabian StyleCao, Fengqiu, Mingming Wang, Shanhua Han, Shengyu Fan, Yingwei Guo, Yingjian Yang, Yu Luo, Jia Guo, and Yan Kang. 2022. "Quantitative Distribution of Cerebral Venous Oxygen Saturation and Its Prognostic Value in Patients with Acute Ischemic Stroke" Brain Sciences 12, no. 8: 1109. https://doi.org/10.3390/brainsci12081109
APA StyleCao, F., Wang, M., Han, S., Fan, S., Guo, Y., Yang, Y., Luo, Y., Guo, J., & Kang, Y. (2022). Quantitative Distribution of Cerebral Venous Oxygen Saturation and Its Prognostic Value in Patients with Acute Ischemic Stroke. Brain Sciences, 12(8), 1109. https://doi.org/10.3390/brainsci12081109









