Assessment of Contributing Factors and Treatment Practices for Therapeutic Efficacy and Drug-Related Problems in Suicidal Psychotic Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Sample Size
2.3. Inclusion and Exclusion Criteria
2.4. Methods for Assessment
2.5. Parametric Assessment
2.6. Suicidal Ideation and/or Attempt
2.7. Contributing Factors for Suicidal Behavior
2.8. Prevailing Treatment Practices
2.9. Drug-Related Problems
2.10. Drug Adherence and Patient’s Compliance
2.11. Socio-Demographics
2.12. Analysis
3. Results
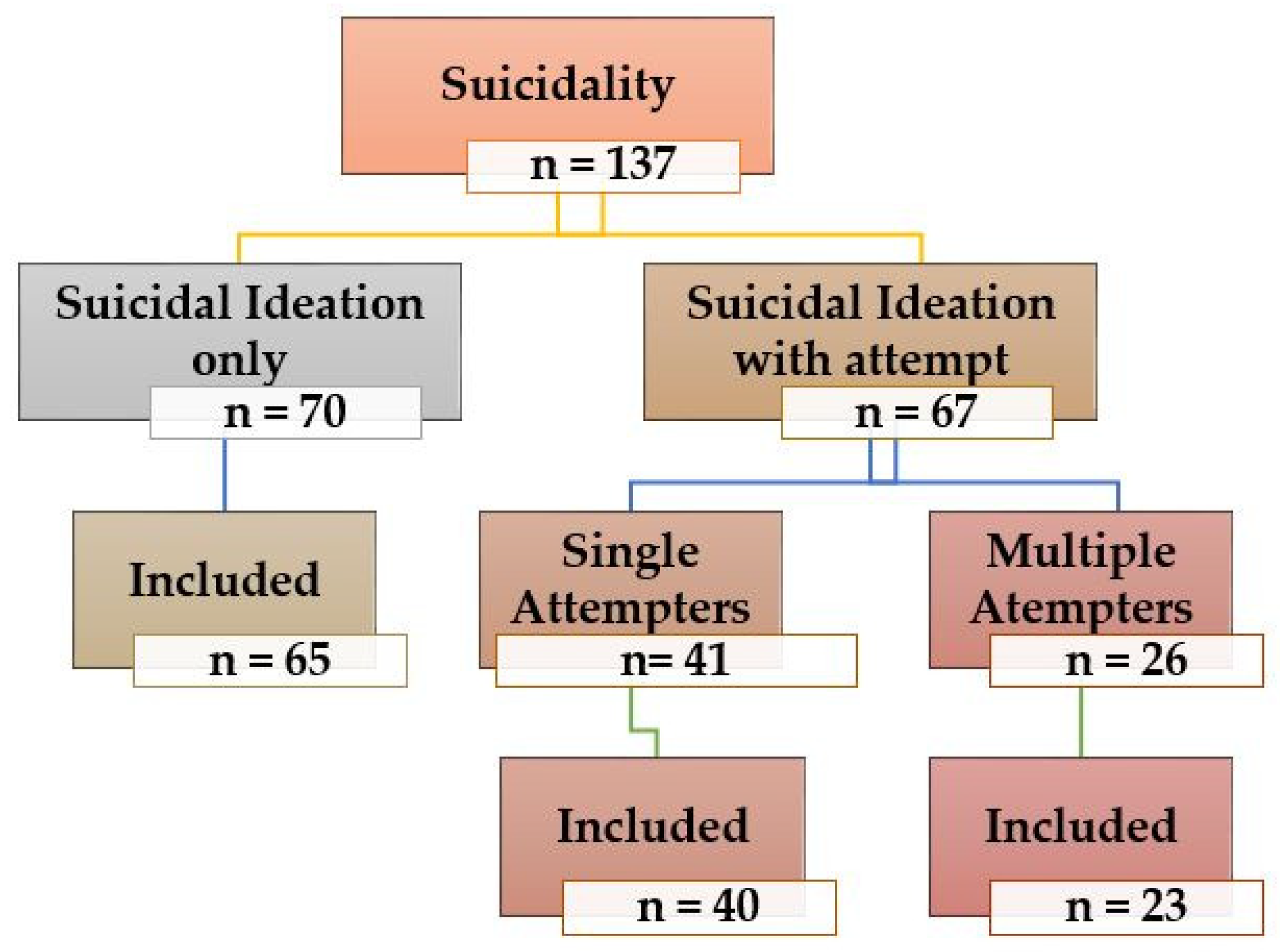
3.1. Study Sample Characteristics
3.2. Socio-Demographics
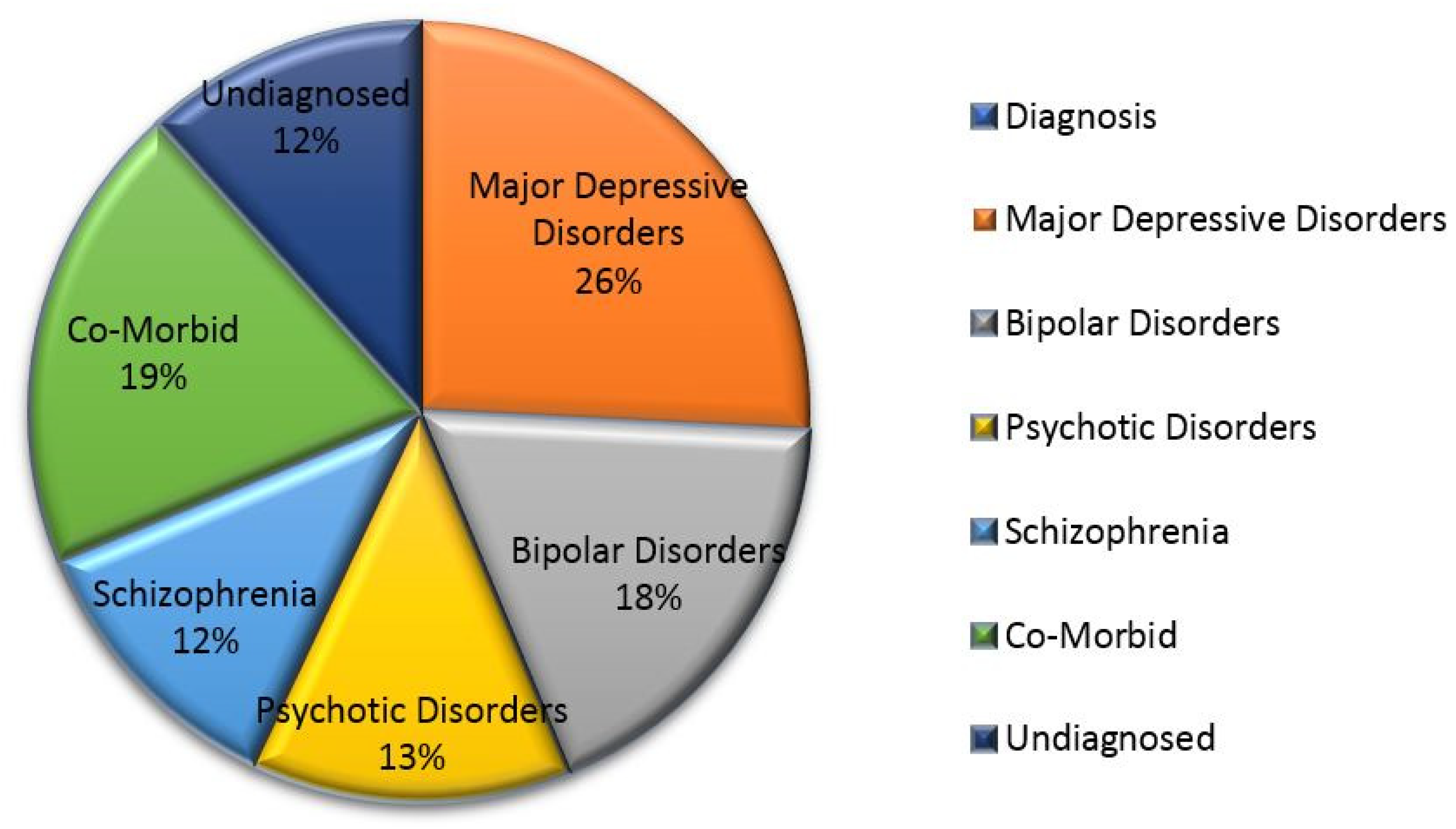
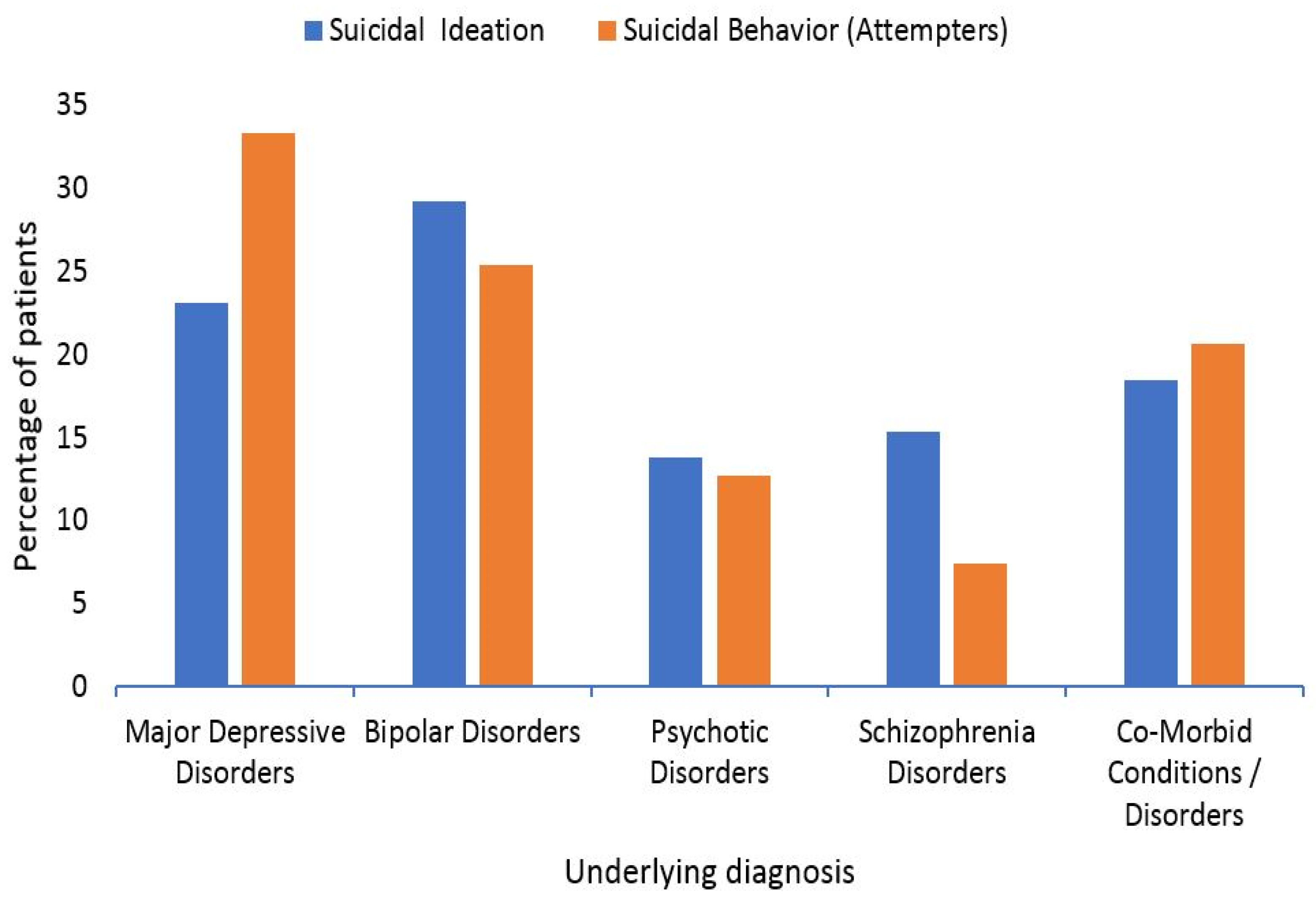
3.3. Underlying Psychotic Diseases
3.4. Treatment Groups
3.5. Drug-Related Problems (DRPs)
3.6. Treatment Adherence
4. Discussion
5. Practical Implications
6. Strengths and Limitations of the Study
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Persson, G.; Danielsson, M.; Rosén, M.; Alexanderson, K.; Lundberg, O.; Lundgren, B.; Stenbeck, M.; Wall, S. Health in Sweden, the National Public Health Report. Scand J. Public Health Suppl. 2006, 67, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Allgulander, C. Suicide and mortality patterns in anxiety neurosis and depressive neurosis. Arch. Gen. Psychiatry 1994, 51, 708–712. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Preventing Suicide: A Global Imperative; World Health Organization: Luxembourg, 2014; Available online: https://apps.who.int/iris/bitstream/handle/10665/131056/9789241564779_eng.pdf (accessed on 15 September 2019).
- Khan, M.M.; Ali Hyder, A. Suicides in the developing world: Case study from Pakistan. Suicide Life Threat. Behav. 2006, 36, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Definitions: Self-Directed Violence. Injury Prevention and Control: Division of Violence. 2015. Available online: http://www.cdc.gov/violenceprevention/suicide/definitions.html (accessed on 20 September 2019).
- Mann, J.J. Neurobiology of suicidal behaviour. Nat. Rev. Neurosci. 2003, 4, 819–828. [Google Scholar] [CrossRef] [PubMed]
- Crosby, A.; Gfroerer, J.; Han, B.; Ortega, L.; Parks, S.E. Suicidal Thoughts and Behaviors among Adults Aged_18 Years; United States, 2008–2009; Centers for Disease Control and Prevention, US Department of Health and Human Services: Atlanta, GA, USA, 2011.
- Goldman-Mellor, S.J.; Caspi, A.; Harrington, H.; Hogan, S.; Nada-Raja, S.; Poulton, R.; Moffitt, T.E. Suicide attempt in young people: A signal for long-term health care and social needs. JAMA Psychiatry 2014, 71, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Nock, M.K.; Borges, G.; Bromet, E.J.; Alonso, J.; Angermeyer, M.; Beautrais, A.; Bruffaerts, R.; Chiu, W.T.; de Girolamo, G.; Gluzman, S.; et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br. J. Psychiatry 2008, 192, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Ekramzadeh, S.; Javadpour, A.; Draper, B.; Mani, A.; Withall, A.; Sahraian, A. Prevalence and correlates of suicidal thought and self-destructive behavior among an elderly hospital population in Iran. Int. Psychogeriatr. 2012, 24, 1402–1408. [Google Scholar] [CrossRef]
- Kessler, R.C.; Borges, G.; Walters, E.E. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch. Gen. Psychiatry 1999, 56, 617–626. [Google Scholar] [CrossRef] [PubMed]
- Furlanetto, L.M.; Stefanello, B. Suicidal ideation in medical inpatients: Psychosocial and clinical correlates. Gen. Hosp. Psychiatry 2011, 33, 572–578. [Google Scholar] [CrossRef] [PubMed]
- Qin, P.; Agerbo, E.; Mortensen, P.B. Suicide risk in relation to socioeconomic, demographic, psychiatric, and familial factors: A national register-based study of all suicides in Denmark, 1981–1997. Am. J. Psychiatry 2003, 160, 765–772. [Google Scholar] [CrossRef]
- Luoma, J.B.; Martin, C.E.; Pearson, J.L. Contact with mental health and primary care providers before suicide: A review of the evidence. Am. J. Psychiatry 2002, 159, 909–916. [Google Scholar] [CrossRef]
- Smith, K.; Crawford, S. Suicidal behavior among “normal” high school students. Suicide Life Threat. Behav. 1986, 16, 313–325. [Google Scholar] [CrossRef] [PubMed]
- Granello, D.H. The process of suicide risk assessment: Twelve core principles. J. Couns. Dev. JCD 2010, 88, 363. [Google Scholar] [CrossRef]
- Maher, R.L.; Hanlon, J.; Hajjar, E.R. Clinical consequences of polypharmacy in elderly. Expert Opin. Drug Saf. 2014, 13, 57–65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ismail, M.; Iqbal, Z.; Khattak, M.B.; Javaid, A.; Khan, M.; Khan, T.; Asim, S.M. Potential Drug-Drug Interactions in Psychiatric Ward of a Tertiary Care Hospital: Prevalence, Levels and Association with Risk Factors. Trop. J. Pharm. Res. 2012, 11, 289–296. [Google Scholar] [CrossRef] [Green Version]
- Leendertse, A.J.; Egberts, A.C.; Stoker, J. Frequency of and risk factors for preventable medication-related hospital admissions in the Netherlands. Arch. Intern. Med. 2008, 168, 1890–1896. [Google Scholar]
- Howard, R.L.; Avery, A.; Slavenburg, S.; Royal, S.; Pipe, G.; Lucassen, P.; Pirmohamed, M. Which drugs cause preventable admissions to hospital? A systematic review. Br. J. Clin. Pharmacol. 2007, 63, 136–147. [Google Scholar] [CrossRef] [Green Version]
- Blix, H.S.; Viktil, K.K.; Moger, T.A.; Reikvam, Å. Characteristics of drug-related problems discussed by hospital pharmacists in multidisciplinary teams. Pharm. World Sci. 2006, 28, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Bedouch, P.; Sylvoz, N.; Charpiat, B.; Juste, M.; Roubille, R.; Rose, F.-X.; Bosson, J.-L.; Conort, O.; Allenet, B. Trends in pharmacists’ medication order review in French hospitals from 2006 to 2009: Analysis of pharmacists’ interventions from the Act-IP© website observatory. J. Clin. Pharm. Ther. 2015, 40, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Guignard, B.; Bonnabry, P.; Perrier, A.; Dayer, P.; Desmeules, J.; Samer, C.F. Drug-related problems identification in general internal medicine: The impact and role of the clinical pharmacist and pharmacologist. Eur. J. Intern. Med. 2015, 26, 399–406. [Google Scholar] [CrossRef]
- Abunahlah, N.; Elawaisi, A.; Velibeyoglu, F.M.; Sancar, M. Drug related problems identified by clinical pharmacist at the Internal Medicine Ward in Turkey. Int. J. Clin. Pharm. 2018, 40, 360–367. [Google Scholar] [CrossRef] [PubMed]
- Charan, J.; Biswas, T. How to calculate sample size for different study designs in medical research. Indian J. Psychol. Med. 2013, 35, 121–126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gipson, P.Y.; Agarwala, P.; Opperman, K.J.; Horwitz, A.; King, C.A. Columbia-suicide severity rating scale: Predictive validity with adolescent psychiatric emergency patients. Pediatric Emerg. Care 2015, 31, 88–94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wani, R.T. Socioeconomic status scales-modified Kuppuswamy and UdaiPareekh’s scale updated for 2019. J. Fam. Med. Prim. Care 2019, 8, 1846–1849. [Google Scholar] [CrossRef] [PubMed]
- Arrindell, W.; Meeuwesen, L.; Huyse, F. The satisfaction with life scale (SWLS): Psychometric properties in a non-psychiatric medical outpatients’ sample. Personal. Individ. Differ. 1991, 12, 117–123. [Google Scholar] [CrossRef]
- Sidorkiewicz, S.; Tran, V.-T.; Cousyn, C.; Perrodeau, E.; Ravaud, P. Development and validation of an instrument to assess treatment adherence for each individual drug taken by a patient. BMJ Open 2016, 6, e010510. [Google Scholar] [CrossRef] [PubMed]
- Seematter-Bagnoud, L.; Karmaniola, A.; Santos-Eggimann, B. Adverse life events among community-dwelling persons aged 65–70 years: Gender differences in occurrence and perceived psychological consequences. Soc. Psychiatry Psychiatr. Epidemiol. 2010, 45, 9–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murphy, G.E. Why women are less likely than men to commit suicide. Compr. Psychiatry 1998, 39, 165–175. [Google Scholar] [CrossRef]
- Charbonneau, A.M.; Mezulis, A.H.; Hyde, J.S. Stress and emotional reactivity as explanations for gender differences in adolescents’ depressive symptoms. J. Youth Adolesc 2009, 38, 1050–1058. [Google Scholar] [CrossRef]
- Galdas, P.M.; Cheater, F.; Marshall, P. Men and health help-seeking behaviour: Literature review. J. Adv. Nurs 2005, 49, 616–623. [Google Scholar] [CrossRef] [PubMed]
- Verma, R.; Balhara, Y.P.S.; Gupta, C.S. Gender differences in stress response: Role of developmental and biological determinants. Ind. Psychiatry J. 2011, 20, 4. [Google Scholar] [PubMed]
- Naghavi, F.; Redzuan, M. The relationship between gender and emotional intelligence. World ApplSci. J. 2011, 15, 555–561. [Google Scholar]
- Beautrais, A.L. Suicide and serious suicide attempts in youth: A multiple-group comparison study. Am. J. Psychiatry 2003, 160, 1093–1099. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, A.E.; Lu, H.; Skinner, R. Time trends in medically serious suicide-related behaviours in boys and girls. Can. J. Psychiatry 2014, 59, 556–560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gould, M.S.; Velting, D.; Kleinman, M.; Lucas, C.; Thomas, J.G.; Chung, M. Teenagers’ attitudes about coping strategies and help-seeking behavior for suicidality. J. Am. Acad. Child. Adolesc. Psychiatry 2004, 43, 1124–1133. [Google Scholar] [CrossRef] [PubMed]
- Canetto, S.S.; Sakinofsky, I. The gender paradox in suicide. Suicide Life-Threat. Behav. 1998, 28, 1–23. [Google Scholar]
- Stone, D.M.; Holland, K.M.; Bartholow, B.; Crosby, A.E.; Davis, S.; Wilkins, N. Preventing Suicide: A Technical Package of Policies, Programs, and Practices. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. Suicide Prevention: Youth Suicide. 2014. Available online: http://www.cdc.gov/violenceprevention/pub/youth_suicide.html (accessed on 22 September 2019).
- Kposowa, A.J. Marital status and suicide in the National Longitudinal Mortality Study. J. Epidemiol. Commun. Health 2000, 54, 254–261. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agerbo, E. High income, employment, postgraduate education, and marriage: A suicidal cocktail among psychotic patients. Arch. Gen. Psychiatry 2007, 64, 1377–1384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pompili, M.; Vichi, M.; Qin, P.; Innamorati, M.; De Leo, D.; Girardi, P. Does the level of education influence completed suicide? A nationwide register study. J. Affect. Disord. 2013, 147, 437–440. [Google Scholar] [CrossRef]
- Gibb, S.; Beautrais, A. Epidemiology of attempted suicide in Canterbury province, New Zealand (1993–2002). N. Z. Med. J. 2004, 117, 1–9. [Google Scholar]
- Cullberg, J.; Wasserman, D.; Stefansson, C.G. Who commits suicide after a suicide attempt? An 8 to 10 year follow up in a suburban catchment area. ActaPsychiatr Scand. 1988, 77, 598–603. [Google Scholar] [CrossRef] [PubMed]
- Pompili, M.; Innamorati, M.; Szanto, K.; Di Vittorio, C.; Conwell, Y.; Lester, D.; Tatarelli, R.; Girardi, P.; Amore, M. Life events as precipitants of suicide attempts among first-time suicide attempters, repeaters, and non-attempters. Psychiatry Res. 2011, 186, 300–305. [Google Scholar] [CrossRef] [PubMed]
- Beautrais, A.; Joyce, P.; Mulder, R.; Fergusson, D.M.; Deavoll, B.J.; Nightingale, S.K. Prevalence and comorbidity of mental disorders in persons making serious suicide attempts: A case-control study. Am. J. Psychiatry 1996, 153, 1009–1014. [Google Scholar]
- Beautrais, A.L. Suicides and serious suicide attempts: Two populations or one? Psychol. Med. 2001, 31, 837–845. [Google Scholar] [CrossRef] [PubMed]
- Jackson, C.A.; Henderson, M.; Frank, J.W.; Haw, S.J. An overview of prevention of multiple risk behaviour in adolescence and young adulthood. J. Public Health 2012, 34 (Suppl. S1), i31–i40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berardelli, I.; Serafini, G.; Cortese, N.; Fiaschè, F.; O’Connor, R.C.; Pompili, M. The Involvement of Hypothalamus-Pituitary-Adrenal (HPA) Axis in Suicide Risk. Brain Sci. 2020, 10, 653. [Google Scholar] [CrossRef] [PubMed]
- Lester, D. The concentration of neurotransmitter metabolites in the cerebrospinal fluid of suicidal individuals: A meta-analysis. Pharmacopsychiatry 1995, 28, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Rao, M.L.; Hawellek, B.; Papassotiropoulos, A.; Deister, A.; Frahnert, C. Upregulation of the platelet Serotonin2A receptor and low blood serotonin in suicidal psychotic patients. Neuropsychobiology 1998, 38, 84–89. [Google Scholar] [CrossRef] [Green Version]
- Pandey, G.N.; Pandey, S.C.; Dwivedi, Y.; Sharma, R.P.; Janicak, P.G.; Davis, J.M. Platelet serotonin-2A receptors: A potential biological marker for suicidal behavior. Am. J. Psychiatry 1995, 152, 850–855. [Google Scholar]
- Pandey, G.N.; Dwivedi, Y. What can post-mortem studies tell us about the patho-etiology of suicide? Future Neurol. 2010, 5, 701–720. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meltzer, H.Y.; Perline, R.; Tricou, B.J.; Lowy, M.; Robertson, A. Effect of 5-hydroxytryptophan on serum cortisol levels in major affective disorders. II. Relation to suicide, psychosis, and depressive symptoms. Arch. Gen. Psychiatry 1984, 41, 379–387. [Google Scholar] [CrossRef]
- Banki, C.M.; Arato, M.; Papp, Z.; Kurcz, M. Biochemical markers in suicidal patients. Investigations with cerebrospinal fluid amine metabolites and neuroendocrine tests. J. Affect. Disord. 1984, 6, 341–350. [Google Scholar] [CrossRef]
- Reul, J.M.; de Kloet, E.R. Two receptor systems for corticosterone in rat brain: Microdistribution and differential occupation. Endocrinology 1985, 117, 2505–2511. [Google Scholar] [CrossRef] [PubMed]
- Yerevanian, B.I.; Feusner, J.D.; Koek, R.J.; Mintz, J. The dexamethasone suppression test as a predictor of suicidal behavior in unipolar depression. J. Affect. Disord. 2004, 83, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Coryell, W.; Schlesser, M.A. Suicide and the dexamethasone suppression test in unipolar depression. Am. J. Psychiatry 1981, 138, 1120–1121. [Google Scholar] [PubMed]
- Lester, D. The dexamethasone suppression test as an indicator of suicide: A meta-analysis. Pharmacopsychiatry 1992, 25, 265–270. [Google Scholar] [CrossRef]
- Norman, W.H.; Brown, W.A.; Miller, I.W.; Keitner, G.I.; Overholser, J.C. The dexamethasone suppression test and completed suicide. ActaPsychiatrScand 1990, 81, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Yerevanian, B.I.; Olafsdottir, H.; Milanese, E.; Russotto, J.; Mallon, P.; Baciewicz, G.; Sagi, E. Normalization of the dexamethasone suppression test at discharge from hospital. Its prognostic value. J. Affect. Disord. 1983, 5, 191–197. [Google Scholar] [CrossRef]
- Nemeroff, C.B.; Owens, M.J.; Bissette, G.; Andorn, A.C.; Stanley, M. Reduced corticotropin releasing factor binding sites in the frontal cortex of suicide victims. Arch. Gen. Psychiatry 1988, 45, 577–579. [Google Scholar] [CrossRef] [PubMed]
- Filaković, P.; Erić, A.P. Pharmacotherapy of suicidal behaviour in major depression, schizophrenia and bipolar disorder. Coll. Antropol. 2013, 37, 1039–1044. [Google Scholar] [PubMed]
- Kobeissi, J.; Aloysi, A.; Tobias, K.; Popeo, D.; Kellner, C.H. Resolution of severe suicidality with a single electroconvulsive therapy. J. ECT 2011, 27, 86–88. [Google Scholar] [CrossRef] [PubMed]
- Schechter, M.; Ronningstam, E.; Herbstman, B.; Goldblatt, M.J. Psychotherapy with Suicidal Patients: The Integrative Psychodynamic Approach of the Boston Suicide Study Group. Medicina 2019, 55, 303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sackeim, H.A. Modern electroconvulsive therapy: Vastly improved yet greatly underused. JAMA Psychiatry 2017, 4, 779–780. [Google Scholar] [CrossRef] [PubMed]
- Dierckx, B.; Heijnen, W.T.; van den Broek, W.W.; Birkenhäger, T.K. Efficacy of electroconvulsive therapy in bipolar versus unipolar major depression: A meta-analysis. Bipolar Disord. 2012, 14, 146–150. [Google Scholar] [CrossRef] [PubMed]
- Husain, M.M.; Rush, A.J.; Fink, M.; Knapp, R.; Petrides, G.; Rummans, T.; Biggs, M.M.; O’Connor, K.; Rasmussen, K.; Litle, M.; et al. Speed of response and remission in major depressive disorder with acute electroconvulsive therapy (ECT): A Consortium for Research in ECT (CORE) report. J. Clin. Psychiatry 2004, 65, 485–491. [Google Scholar] [CrossRef] [PubMed]
- Higashi, K.; Medic, G.; Littlewood, K.J.; Diez, T.; Granström, O.; De Hert, M. Medication adherence in schizophrenia: Factors influencing adherence and consequences of nonadherence, a systematic literature review. Ther. Adv. Psychopharmacol. 2013, 3, 200–218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cerovecki, A.; Musil, R.; Klimke, A.; Seemüller, F.; Haen, E.; Schennach, R.; Kühn, K.U.; Volz, H.P.; Riedel, M. Withdrawal symptoms and rebound syndromes associated with switching and discontinuing atypical antipsychotics: Theoretical background and practical recommendations. CNS Drugs 2013, 27, 545–572. [Google Scholar] [CrossRef]
- Chan, L.F.; Shamsul, A.S.; Maniam, T. Are predictors of future suicide attempts and the transition from suicidal ideation to suicide attempts shared or distinct: A 12-month prospective study among patients with depressive disorders. Psychiatry Res. 2014, 220, 867–873. [Google Scholar] [CrossRef] [PubMed]
- Rush, A.J.; Trivedi, M.H.; Wisniewski, S.R.; Nierenberg, A.A.; Stewart, J.W.; Warden, D.; Niederehe, G.; Thase, M.E.; Lavori, P.W.; Lebowitz, B.; et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: A STAR*D report. Am. J. Psychiatry 2006, 163, 1905–1917. [Google Scholar] [CrossRef]
- Irigoyen, M.; Porras-Segovia, A.; Galván, L.; Puigdevall, M.; Giner, L.; De Leon, S.; Baca-García, E. Predictors of re-attempt in a cohort of suicide attempters: A survival analysis. J. Affect. Disord. 2019, 247, 20–28. [Google Scholar] [CrossRef]
- Callor, W.B.; Petersen, E.; Gray, D.; Grey, T.; Lamoreaux, T.; Bennett, P.J. Preliminary findings of noncompliance with psychotropic medication and prevalence of methamphetamine intoxication associated with suicide completion. Crisis 2005, 26, 78–84. [Google Scholar] [CrossRef] [PubMed]
- Granboulan, V.; Roudot-Thoraval, F.; Lemerle, S.; Alvin, P. Predictive factors of post-discharge follow-up care among adolescent suicide attempters. ActaPsychiatr Scand. 2001, 104, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Costantini, L.; Pasquarella, C.; Odone, A.; Colucci, M.E.; Costanza, A.; Serafini, G.; Aguglia, A.; Murri, M.B.; Brakoulias, V.; Amore, M.; et al. Screening for depression in primary care with Patient Health Questionnaire-9 (PHQ-9): A systematic review. J. Affect. Disord. 2021, 279, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Steer, R.A. Manual for Beck Scale for Suicide Ideation; Psychological Corporation: San Antonio, TX, USA, 1991. [Google Scholar]
- Posner, K.; Brown, G.K.; Stanley, B.; Brent, D.A.; Yershova, K.V.; Oquendo, M.A.; Currier, G.W.; Melvin, G.A.; Greenhill, L.; Shen, S.; et al. The Columbia-Suicide Severity Rating Scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am. J. Psychiatry 2011, 168, 1266–1277. [Google Scholar] [CrossRef] [Green Version]
| Category | Suicidal Ideation Only | Suicidal Behavior (Attempts) | Total | χ2 | df | Asymp. Sig. (2-Sided) p-Value | B-H Value (FDR) | Odds Ratio (OR) | ||
|---|---|---|---|---|---|---|---|---|---|---|
| N = 65 | N = 63 | N = 128 | ||||||||
| Family History of Suicide | Yes | 14 (31.1) | 31 (68.9) | 45 (35.15) | 10.74 | 1 | 0.001 * | 0.01 | 3.529 | |
| No | 51 (61.4) | 32 (38.6) | 83 (64.84) | |||||||
| Gender | Males | 24 (36.4) | 42 (63.6) | 66 (51.56) | 11.33 | 1 | 0.001 * | 0.01 | 1.892 | |
| Females | 41 (66.1) | 21 (33.9) | 62 (48.43) | |||||||
| Age (years) | 13–23 | 20 (30.8) | 17 (27) | 37 (28.90) | 1.64 | 3 | 0.65 | 0.05 | 1.049 | 1.281 |
| 24–34 | 37 (56.9) | 33 (58.7) | 70 (54.68) | 1.961 | ||||||
| 35–45 | 6 (9.2) | 10 (15.8) | 16 (12.5) | 1.765 | ||||||
| ≥46 | 2 (3.1) | 3 (4.7) | 5 (3.90) | 0.850 | ||||||
| Socioeconomic Class | Upper Class | 10 (15.4) | 3 (4.8) | 13 (10.15) | 5.86 | 2 | 0.05 * | 0.03 | 3.972 | 1.271 |
| Middle Class | 47 (72.3) | 56 (88.9) | 103 (80.4) | 1.667 | ||||||
| Poor | 8 (12.3) | 4 (6.3) | 12 (9.38) | 0.300 | ||||||
| Occupation | Unemployed | 17 (26.2) | 19 (30.2) | 36 (28.12) | 4.48 | 5 | 0.483 | 0.04 | 1.432 | 0.953 |
| Employed 1 | 5 (7.7) | 8 (12.7) | 13 (10.15) | 1.789 | ||||||
| Farmer | 1 (1.5) | 2 (3.2) | 3 (2.34) | 0.569 | ||||||
| Student | 11 (16.9) | 7 (11.1) | 18 (14.06) | 0.503 | ||||||
| House wife | 16 (24.6) | 9 (14.3) | 25 (19.53) | 1.150 | ||||||
| Others 2 | 14 (21.5) | 18 (28.6) | 32 (25) | 1.118 | ||||||
| Educational Level | Illiterate | 12 (18.5) | 12 (19) | 24 (18.75) | 17.19 | 5 | 0.004 * | 0.03 δ | 3.600 | 0.769 |
| Primary school (1–5) | 5 (7.7) | 18 (28.6) | 23 (17.96) | 1.400 | ||||||
| Middle school (6–8) | 5 (7.7) | 7 (11.1) | 12 (9.37) | 2.00 | ||||||
| Secondary/High school (9–10) | 4 (6.2) | 8 (12.7) | 12 (9.37) | 0.353 | ||||||
| Higher secondary school (10–12) | 17 (26.2) | 6 (9.5) | 23 (17.96) | 0.545 | ||||||
| Tertiary (12+) | 22 (33.8) | 12 (19) | 34 (26.56) | 1.000 | ||||||
| Life Satisfaction level | Dissatisfied | 14 (21.5) | 26 (41.3) | 40 (31.25) | 15.75 | 4 | 0.003 | 0.02 | 0.769 | 0.679 |
| Slightly Dissatisfied | 14 (21.5) | 20 (31.7) | 34 (26.56) | 0.049 | ||||||
| Neutral | 11 (16.9) | 1 (1.6) | 12 (9.37) | 0.380 | ||||||
| Slightly satisfied | 17 (26.1) | 12 (19) | 29 (22.65) | 0.239 | ||||||
| Satisfied | 9 (13.84) | 4 (6.3) | 13 (10.15) | 1.857 | ||||||
| Marital Status | Single | 15 (23.1) | 20 (31.7) | 35 (27.34) | 15.32 | 3 | 0.002 * | 0.02 | 0.938 | 0.557 |
| Married | 28 (43.1) | 35 (55.6) | 63 (49.21) | 1.875 | ||||||
| Engaged | 2 (3.1) | 5 (7.9) | 8 (6.25) | 0.113 | ||||||
| Widowed | 20 (30.8) | 3 (4.8) | 23 (17.96) | 1.333 | ||||||
| History | No Suicidal Ideations | 32 (49.2) | 0 (0) | 32 (25) | 29.63 | 3 | 0.000002 * | 0.005 | 0.000 | 0.390 |
| Previous Suicide Attempt | ---- | 13 (20.6) | 13 (10.15) | 323 | ||||||
| Self-injurious behavior | 11 (16.9) | 25 (39.7) | 36 (28.125) | 4.54 | ||||||
| Interrupted/Aborted attempts | ---- | 14 (22.2) | 14 (10.93) | 323 | ||||||
| Suicidal ideations only | 22 (33.8) | 11 (17.5) | 33 (25.78) | 0.500 | ||||||
| Treatment Group | Suicidality | C-SSRS | Correlation | Paired t-Test | |||
|---|---|---|---|---|---|---|---|
| Mean | MD | R | Sig. | t | Sig. | ||
| Psychotherapy | Baseline | 5.54 | 1.09 | 0.23 | 0.29 | 1.37 | 0.183 |
| Follow-up | 4.45 | ||||||
| Pharmacotherapy | Baseline | 5.96 | 1.57 | 0.24 | 0.16 | 2.93 | 0.006 |
| Follow-up | 4.39 | ||||||
| Electroconvulsive therapy | Baseline | 5.64 | 2.32 | 0.39 | 0.04 | 3.98 | 0.001 |
| Follow-up | 3.32 | ||||||
| Combination therapy | Baseline | 5.8 | 2.14 | −0.22 | 0.17 | 3.52 | 0.001 |
| Follow-up | 3.65 | ||||||
| Treatment Group | Suicidal Ideation | Suicidal Behavior | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean C-SSRS | Correlation | Paired t-Test | Mean C-SSRS | Correlation | Paired t-Test | |||||||
| B | F | r | p | t | p | B | F | r | p | t | p | |
| Psychotherapy | 2.44 | 2.55 | 0.59 | 0.09 | −0.21 | 0.84 | 7.69 | 5.77 | 0.78 | 0.00 | 6.22 | 0.00 |
| Pharmacotherapy | 3.28 | 3.00 | 0.08 | 0.80 | 0.43 | 0.68 | 7.95 | 5.42 | −0.13 | 0.58 | 9.04 | 0.00 |
| Electroconvulsive therapy | 3.09 | 2.00 | 0.71 | 0.01 | 3.46 | 0.01 | 7.64 | 4.36 | 0.74 | 0.00 | 13.45 | 0.00 |
| Combination therapy | 4.22 | 2.27 | −0.13 | 0.60 | 4.51 | 0.00 | 7.47 | 5.12 | 0.63 | 0.01 | 6.14 | 0.00 |
| N (%) | N (%) | ||
|---|---|---|---|
| Drug Selection | 39 (17.88) | ||
| Duplication | 7 (3.21) | ||
| Wrong drug | 5 (2.29) | ||
| Preferred/better choice of drug not given | 9 (4.12) | ||
| Drug should have been ceased | 18 (8.25) | ||
| Dosage-related problems | 45 (20.64) | ||
| Inappropriate frequency | 9 (4.12) | ||
| Inappropriate duration | 11 (5.04) | ||
| Wrong dose/Dose changed too quickly | 8 (3.66) | ||
| Incorrect or unclear dosing instructions | 14 (6.42) | ||
| Dosage form inappropriateness | 3 (1.37) | ||
| Potential Drug–drug interactions | 53 (24.31) | ||
| Contraindications apparent | 2 (0.91) | ||
| Minor | 6 (2.75) | ||
| Moderate | 31 (14.22) | ||
| Major | 14 (6.42) | ||
| Adverse Drug Reactions | 25 (11.46) | ||
| Symptom of an undesirable effect | 19 (8.71) | ||
| Toxicity or allergic events | 6 (2.75) | ||
| Other Problems | 56 (25.68) | ||
| Incorrect Spelling of trade name | 9 (4.12) | ||
| Inadequate education or counseling | 47 (21.55) | ||
| Treatment Adherence Status | Suicidal Ideation | Suicidal Behavior | Total (N) | χ2 | df | Asymp. Sig. (2-Sided) |
|---|---|---|---|---|---|---|
| High Adherence | 9 | 3 | 12 | 9.29 | 2 | 0.01 |
| Intermediate Adherence | 53 | 11 | 64 | |||
| Low Adherence | 21 | 18 | 39 | |||
| Total (N) | 83 | 32 | 115 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shahzad, S.; Ullah, S.; Nazar, Z.; Riaz, M.; Khuda, F.; Khalil, A.A.K.; Almutairi, M.H.; Sayed, A.A.; Büyüker, S.M.; Khan, N. Assessment of Contributing Factors and Treatment Practices for Therapeutic Efficacy and Drug-Related Problems in Suicidal Psychotic Patients. Brain Sci. 2022, 12, 543. https://doi.org/10.3390/brainsci12050543
Shahzad S, Ullah S, Nazar Z, Riaz M, Khuda F, Khalil AAK, Almutairi MH, Sayed AA, Büyüker SM, Khan N. Assessment of Contributing Factors and Treatment Practices for Therapeutic Efficacy and Drug-Related Problems in Suicidal Psychotic Patients. Brain Sciences. 2022; 12(5):543. https://doi.org/10.3390/brainsci12050543
Chicago/Turabian StyleShahzad, Saimon, Sami Ullah, Zahid Nazar, Muhammad Riaz, Fazli Khuda, Atif Ali Khan Khalil, Mikhlid H. Almutairi, Amany A. Sayed, Sultan Mehtap Büyüker, and Nazimuddin Khan. 2022. "Assessment of Contributing Factors and Treatment Practices for Therapeutic Efficacy and Drug-Related Problems in Suicidal Psychotic Patients" Brain Sciences 12, no. 5: 543. https://doi.org/10.3390/brainsci12050543
APA StyleShahzad, S., Ullah, S., Nazar, Z., Riaz, M., Khuda, F., Khalil, A. A. K., Almutairi, M. H., Sayed, A. A., Büyüker, S. M., & Khan, N. (2022). Assessment of Contributing Factors and Treatment Practices for Therapeutic Efficacy and Drug-Related Problems in Suicidal Psychotic Patients. Brain Sciences, 12(5), 543. https://doi.org/10.3390/brainsci12050543







