The Clinical Features of In-Hospital Recurrence in Acute Ischaemic Stroke Patients over Time: A Real-World Observation at a Single Center
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population and Variables of Interest
2.2. Outcome Measures
2.3. Assessment of Antiplatelet Therapy
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
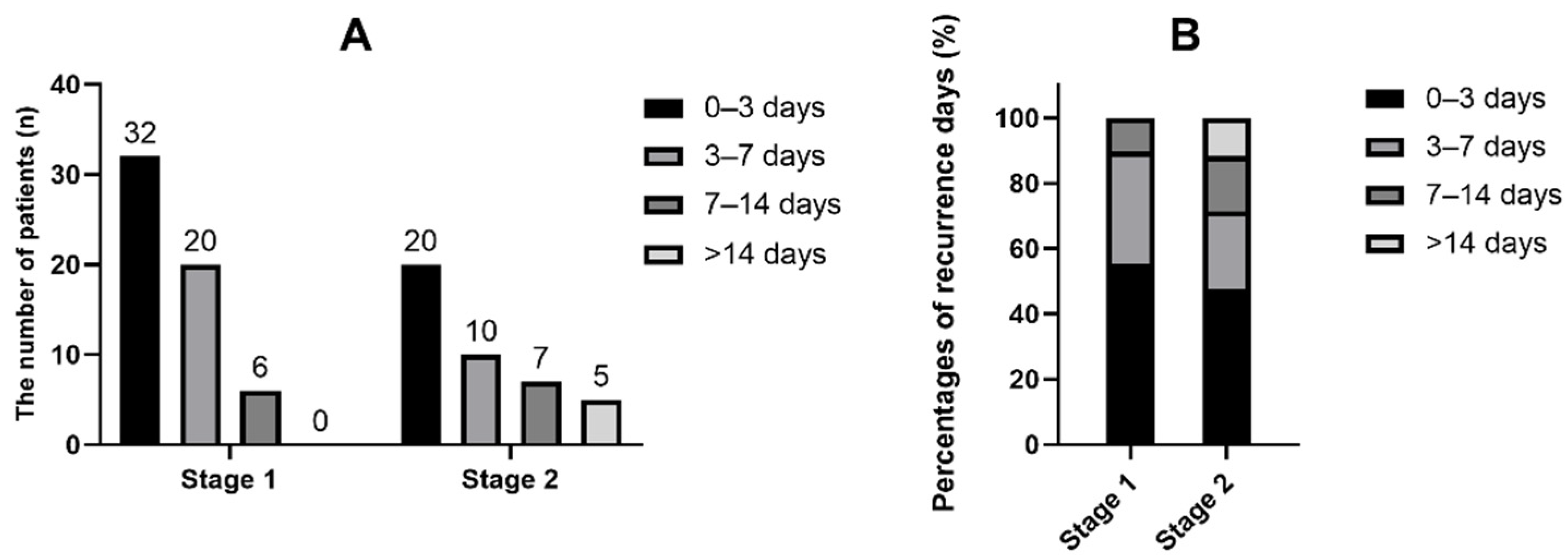
3.2. In-Hospital Ischaemic Recurrence in Different Stages
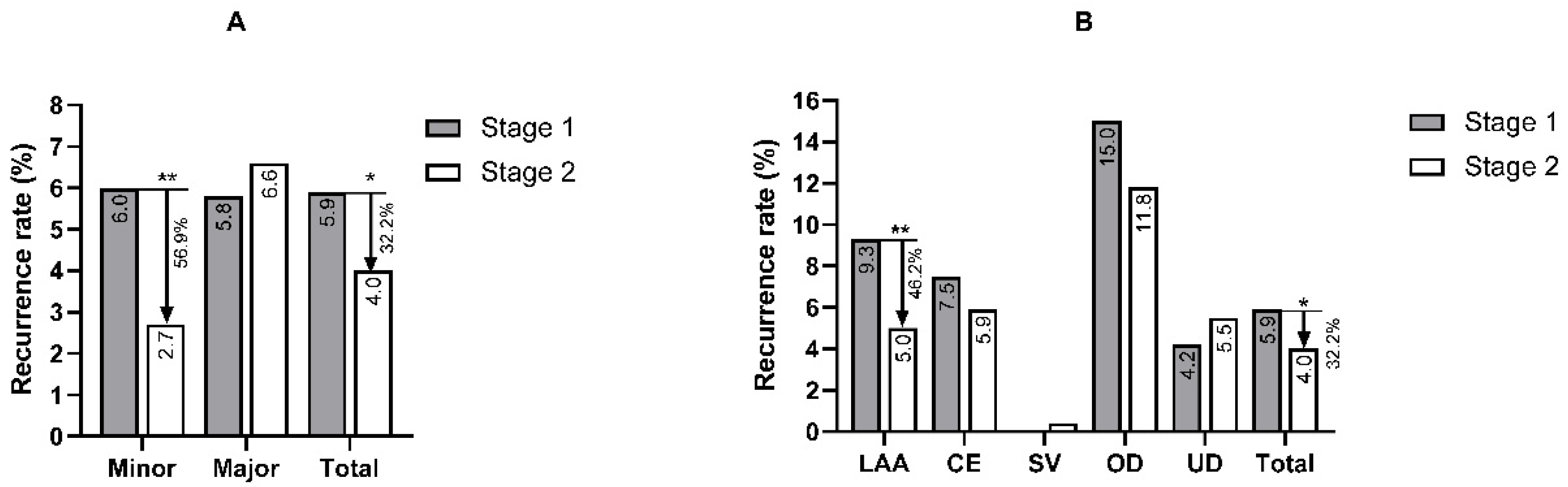
3.3. Clinical Characteristics of In-Hospital Recurrence in Different Subgroups
3.4. Factors Associated with Antiplatelet Therapy in Noncardiac Stroke Patients
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional review board statement
Informed consent statement
Data Availability Statement
Conflicts of Interest
References
- Hankey, G.J. Stroke. Lancet 2017, 389, 641–654. [Google Scholar] [CrossRef]
- Grau, A.J.; Weimar, C.; Buggle, F.; Heinrich, A.; Goertler, M.; Neumaier, S.; Glahn, J.; Brandt, T.; Hacke, W.; Diener, H.C. Risk factors, outcome, and treatment in subtypes of ischemic stroke: The German stroke data bank. Stroke 2001, 32, 2559–2566. [Google Scholar] [CrossRef]
- Callaly, E.; Ni Chroinin, D.; Hannon, N.; Marnane, M.; Akijian, L.; Sheehan, O.; Merwick, A.; Hayden, D.; Horgan, G.; Duggan, J.; et al. Rates, Predictors, and Outcomes of Early and Late Recurrence After Stroke: The North Dublin Population Stroke Study. Stroke 2016, 47, 244–246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maier, I.L.; Bauerle, M.; Kermer, P.; Helms, H.J.; Buettner, T. Risk prediction of very early recurrence, death and progression after acute ischaemic stroke. Eur. J. Neurol. 2013, 20, 599–604. [Google Scholar] [CrossRef]
- Lovett, J.K.; Coull, A.J.; Rothwell, P.M. Early risk of recurrence by subtype of ischemic stroke in population-based incidence studies. Neurology 2004, 62, 569–573. [Google Scholar] [CrossRef]
- Mohan, K.M.; Wolfe, C.D.; Rudd, A.G.; Heuschmann, P.U.; Kolominsky-Rabas, P.L.; Grieve, A.P. Risk and cumulative risk of stroke recurrence: A systematic review and meta-analysis. Stroke 2011, 42, 1489–1494. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amarenco, P.; Lavallee, P.C.; Labreuche, J.; Albers, G.W.; Bornstein, N.M.; Canhao, P.; Caplan, L.R.; Donnan, G.A.; Ferro, J.M.; Hennerici, M.G.; et al. One-Year Risk of Stroke after Transient Ischemic Attack or Minor Stroke. N. Engl. J. Med. 2016, 374, 1533–1542. [Google Scholar] [CrossRef] [PubMed]
- Ay, H.; Gungor, L.; Arsava, E.M.; Rosand, J.; Vangel, M.; Benner, T.; Schwamm, L.H.; Furie, K.L.; Koroshetz, W.J.; Sorensen, A.G. A score to predict early risk of recurrence after ischemic stroke. Neurology 2010, 74, 128–135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, F.; Liu, X.; Yang, Q.; Fu, Y.; Fan, D. In-hospital recurrence in a Chinese large cohort with acute ischemic stroke. Sci. Rep. 2019, 9, 14945. [Google Scholar] [CrossRef] [PubMed]
- Erdur, H.; Scheitz, J.F.; Ebinger, M.; Rocco, A.; Grittner, U.; Meisel, A.; Rothwell, P.M.; Endres, M.; Nolte, C.H. In-hospital stroke recurrence and stroke after transient ischemic attack: Frequency and risk factors. Stroke 2015, 46, 1031–1037. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yulin, W.; Yuming, X. Study of Prehospital Delay and in-Hospital Recurrence in Patients with TIA or Minor Stroke. Ph.D. Thesis, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, China, 2013. [Google Scholar]
- Wang, Y.; Wang, Y.; Zhao, X.; Liu, L.; Wang, D.; Wang, C.; Wang, C.; Li, H.; Meng, X.; Cui, L.; et al. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. N. Engl. J. Med. 2013, 369, 11–19. [Google Scholar] [CrossRef] [Green Version]
- Coull, A.J.; Rothwell, P.M. Underestimation of the early risk of recurrent stroke: Evidence of the need for a standard definition. Stroke 2004, 35, 1925–1929. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alvarez-Sabin, J.; Maisterra, O.; Santamarina, E.; Kase, C.S. Factors influencing haemorrhagic transformation in ischaemic stroke. Lancet Neurol. 2013, 12, 689–705. [Google Scholar] [CrossRef]
- Johnston, S.C.; Easton, J.D.; Farrant, M.; Barsan, W.; Conwit, R.A.; Elm, J.J.; Kim, A.S.; Lindblad, A.S.; Palesch, Y.Y.; Neurological Emergencies Treatment Trials Network; et al. Clopidogrel and Aspirin in Acute Ischemic Stroke and High-Risk TIA. N. Engl. J. Med. 2018, 379, 215–225. [Google Scholar] [CrossRef] [PubMed]
- Johnston, S.C.; Amarenco, P.; Denison, H.; Evans, S.R.; Himmelmann, A.; James, S.; Knutsson, M.; Ladenvall, P.; Molina, C.A.; Wang, Y.; et al. Ticagrelor and Aspirin or Aspirin Alone in Acute Ischemic Stroke or TIA. N. Engl. J. Med. 2020, 383, 207–217. [Google Scholar] [CrossRef]
- Tramacere, I.; Boncoraglio, G.B.; Banzi, R.; Del Giovane, C.; Kwag, K.H.; Squizzato, A.; Moja, L. Comparison of statins for secondary prevention in patients with ischemic stroke or transient ischemic attack: A systematic review and network meta-analysis. BMC Med. 2019, 17, 67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hong, K.S.; Lee, J.S. Statins in Acute Ischemic Stroke: A Systematic Review. J. Stroke 2015, 17, 282–301. [Google Scholar] [CrossRef]
- Rothwell, P.M.; Giles, M.F.; Chandratheva, A.; Marquardt, L.; Geraghty, O.; Redgrave, J.N.; Lovelock, C.E.; Binney, L.E.; Bull, L.M.; Cuthbertson, F.C.; et al. Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): A prospective population-based sequential comparison. Lancet 2007, 370, 1432–1442. [Google Scholar] [CrossRef]
- Lim, S.; Oh, T.J.; Dawson, J.; Sattar, N. Diabetes drugs and stroke risk: Intensive versus conventional glucose-lowering strategies, and implications of recent cardiovascular outcome trials. Diabetes Obes. Metab. 2020, 22, 6–15. [Google Scholar] [CrossRef] [PubMed]
- Desta, Z.; Zhao, X.; Shin, J.G.; Flockhart, D.A. Clinical significance of the cytochrome P450 2C19 genetic polymorphism. Clin. Pharmacokinet. 2002, 41, 913–958. [Google Scholar] [CrossRef]
- Xu, J.; Yalkun, G.; Wang, M.; Wang, A.; Wangqin, R.; Zhang, X.; Chen, Z.; Mo, J.; Meng, X.; Li, H.; et al. Impact of Infection on the Risk of Recurrent Stroke among Patients with Acute Ischemic Stroke. Stroke 2020, 51, 2395–2403. [Google Scholar] [CrossRef] [PubMed]
- LP, D.A.; Schattner, M. Platelet toll-like receptors in thromboinflammation. Front. Biosci.-Landmark 2017, 22, 1867–1883. [Google Scholar] [CrossRef] [Green Version]
- Stoll, G.; Nieswandt, B. Thrombo-inflammation in acute ischaemic stroke—Implications for treatment. Nat. Rev. Neurol. 2019, 15, 473–481. [Google Scholar] [CrossRef]
- Vermeij, J.D.; Westendorp, W.F.; Dippel, D.W.; van de Beek, D.; Nederkoorn, P.J. Antibiotic therapy for preventing infections in people with acute stroke. Cochrane Database Syst. Rev. 2018, 1, CD008530. [Google Scholar] [CrossRef]
- Koupenova, M.; Clancy, L.; Corkrey, H.A.; Freedman, J.E. Circulating Platelets as Mediators of Immunity, Inflammation, and Thrombosis. Circ. Res. 2018, 122, 337–351. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Pan, Y.; Jing, J.; Zhao, X.; Liu, L.; Meng, X.; Wang, Y.; Wang, Y.; the CHANCE Investigators. Recurrent Stroke in Minor Ischemic Stroke or Transient Ischemic Attack With Metabolic Syndrome and/or Diabetes Mellitus. J. Am. Heart Assoc. 2017, 6, e005446. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, J.T.; Kim, B.J.; Park, J.M.; Lee, S.J.; Cha, J.K.; Park, T.H.; Lee, K.B.; Lee, J.; Hong, K.S.; Lee, B.C.; et al. Risk of recurrent stroke and antiplatelet choice in breakthrough stroke while on aspirin. Sci. Rep. 2020, 10, 16723. [Google Scholar] [CrossRef] [PubMed]
- Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ 2002, 324, 71–86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pan, Y.; Jing, J.; Chen, W.; Meng, X.; Li, H.; Zhao, X.; Liu, L.; Wang, D.; Johnston, S.C.; Wang, Y.; et al. Risks and benefits of clopidogrel-aspirin in minor stroke or TIA: Time course analysis of CHANCE. Neurology 2017, 88, 1906–1911. [Google Scholar] [CrossRef] [PubMed]
- Seiffge, D.J.; Werring, D.J.; Paciaroni, M.; Dawson, J.; Warach, S.; Milling, T.J.; Engelter, S.T.; Fischer, U.; Norrving, B. Timing of anticoagulation after recent ischaemic stroke in patients with atrial fibrillation. Lancet Neurol. 2019, 18, 117–126. [Google Scholar] [CrossRef]
- Wankowicz, P.; Nowacki, P.; Golab-Janowska, M. Atrial fibrillation risk factors in patients with ischemic stroke. Arch. Med. Sci. 2021, 17, 19–24. [Google Scholar] [CrossRef]
- Suda, S.; Aoki, J.; Shimoyama, T.; Suzuki, K.; Sakamoto, Y.; Katano, T.; Okubo, S.; Nito, C.; Nishiyama, Y.; Mishina, M.; et al. Stroke-associated infection independently predicts 3-month poor functional outcome and mortality. J. Neurol. 2018, 265, 370–375. [Google Scholar] [CrossRef]
- Gwak, D.S.; Kwon, J.A.; Shim, D.H.; Kim, Y.W.; Hwang, Y.H. Perfusion and Diffusion Variables Predict Early Neurological Deterioration in Minor Stroke and Large Vessel Occlusion. J. Stroke 2021, 23, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Ng, F.C.; Coote, S.; Frost, T.; Bladin, C.; Choi, P.M. CT perfusion predicts tissue injury in TIA and minor stroke. J. Neurol. 2017, 264, 802–803. [Google Scholar] [CrossRef] [PubMed]

| Stage 1 (n = 978) | Stage 2 (n = 1047) | p-Value | |
|---|---|---|---|
| Age (years) | 64 (25–98) | 63 (20–93) | 0.954 |
| Gender (Male, %) | 722 (73.8) | 786 (75.1) | 0.520 |
| Medical history | |||
| Previous IS (%) | 232 (23.7) | 212 (20.2) | 0.059 |
| Previous TIA (%) | 64 (6.5) | 78 (7.4) | 0.425 |
| Atrial fibrillation (%) | 89 (9.1) | 96 (9.2) | 0.957 |
| Hypertension (%) | 668 (68.3) | 740 (70.7) | 0.246 |
| Diabetes (%) | 336 (34.4) | 405 (38.7) | 0.043 |
| Hyperlipidaemia (%) | 210 (21.5) | 229 (21.9) | 0.819 |
| TOAST | |||
| AA (%) | 429 (43.9) | 517 (49.4) | 0.013 # |
| CE (%) | 80 (8.2) | 85 (8.1) | 0.960 |
| SV (%) | 233 (23.8) | 282 (26.9) | 0.108 |
| OD (%) | 20 (2.0) | 17 (1.6) | 0.479 |
| UD (%) | 213 (21.8) | 146 (13.9) | <0.001 * |
| NIHSS score | 2 (0–27) | 2 (0–36) | 0.140 |
| Stage 1 (n = 978) | Stage 2 (n = 1047) | |||||
|---|---|---|---|---|---|---|
| Nonrecurrence (n = 920) | Recurrence (n = 58) | p-Value | Nonrecurrence (n = 1005) | Recurrence (n = 42) | p-Value | |
| Age (years) | 63 (25–98) | 68 (29–85) | 0.106 | 63 (20–93) | 63.5 (27–92) | 0.418 |
| Gender (male, %) | 676 (73.5) | 46 (79.3) | 0.306 | 754 (75.0) | 32 (78.2) | 0.864 |
| Medical history | ||||||
| Previous IS (%) | 221 (24.0) | 11 (19.0) | 0.380 | 201 (20.0) | 11 (26.2) | 0.328 |
| Previous TIA (%) | 56 (6.1) | 8 (13.8) | 0.047 * | 74 (7.4) | 4 (9.5) | 0.547 |
| Atrial fibrillation (%) | 82 (8.9) | 7 (12.1) | 0.418 | 88 (8.8) | 8 (19.0) | 0.048 * |
| Hypertension (%) | 627 (68.2) | 41 (70.7) | 0.687 | 709 (70.5) | 31 (73.8) | 0.649 |
| Diabetes (%) | 309 (33.6) | 27 (46.6) | 0.044 * | 381 (37.9) | 24 (57.1) | 0.012 * |
| Hyperlipidaemia (%) | 192 (20.9) | 18 (31.0) | 0.067 | 219 (21.8) | 10 (23.8) | 0.759 |
| Presentation | ||||||
| Paresis/ataxia (%) | 643 (69.9) | 43 (74.1) | 0.556 | 875 (87.1) | 38 (90.5) | 0.657 |
| Aphasia (%) | 332 (36.1) | 12 (20.7) | 0.017 * | 137 (13.6) | 10 (23.8) | 0.063 |
| Coma (%) | 28 (3.0) | 0 (0.0) | 0.404 | 52 (5.2) | 8 (19.0) | 0.002 * |
| NIHSS score | 2 (0–27) | 3 (0–12) | 0.767 | 2 (0–36) | 4.5 (0–28) | <0.001 * |
| TOAST | ||||||
| AA (%) | 389 (42.3) | 40 (60.9) | <0.001 * | 491 (48.9) | 26 (61.9) | 0.097 |
| CE (%) | 74 (8.0) | 6 (10.3) | 0.464 | 80 (8.0) | 5 (11.9) | 0.359 |
| SV (%) | 233 (25.3) | 0 (0.0) | <0.001 * | 281 (28.0) | 1 (2.4) | <0.001 * |
| OD (%) | 17 (1.8) | 3 (5.2) | 0.110 | 15 (1.5) | 2 (4.8) | 0.146 |
| UD (%) | 204 (22.2) | 9 (15.5) | 0.324 | 138 (13.7) | 8 (19.0) | 0.330 |
| Indicators | ||||||
| HCY (µmol/L) | 15.21 (0.2–130.9) | 14.97 (8.61–121.6) | 0.877 | 12.21 (4.97–109.52) | 11.34 (5.68–36.54) | 0.111 |
| hsCRP (mg/L) | 2.05 (0.01–209.88) | 2.01 (0.46–82.23) | 0.370 | 1.40 (0.01–120.86) | 3.73 (0.12–78.37) | <0.001 * |
| CHL (mmol/L) | 4.19 (1.41–11.25) | 3.71 (2.53–7.36) | 0.256 | 3.95 (1.99–7.68) | 3.94 (2.25–8.94) | 0.152 |
| TG (mmol/L) | 1.38 (0.39–13.65) | 1.38 (0.61–4.16) | 0.905 | 1.37 (0.35–14.52) | 1.32 (0.47–15.61) | 0.382 |
| LDL (mmol/L) | 2.48 (0.43–5.50) | 2.19 (1.07–5.96) | 0.286 | 2.41 (0.73–5.41) | 2.33 (1.14–4.93) | 0.152 |
| HDL (mmol/L) | 0.96 (0.41–3.74) | 0.97 (0.62–1.73) | 0.703 | 0.95 (0.47–3.22) | 0.89 (0.58–1.52) | 0.304 |
| FBG (mmol/L) | 5.10 (2.30–21.23) | 5.45 (4.0–12.00) | 0.019 * | 5.6 (3.2–20.2) | 6.1 (3.2–15.6) | 0.066 |
| HbA1C (%) | 5.8 (4.2–15.6) | 6.05 (4.7–13.5) | 0.012 * | 6.1 (4.6–14.2) | 6.5 (5.0–12.0) | 0.136 |
| Glucose abnormality (%) | 67 (7.3) | 14 (24.1) | <0.001 * | 101 (10.2) | 7 (16.7) | 0.192 |
| Average BP (mmHg) | 138.0 (94.0–190.8) | 143.0 (113.0–170.8) | 0.011 * | 142.0 (99.3–201.2) | 140.7 (109.6–177.5) | 0.764 |
| BPSD | 9.57 (0–57.44) | 11.2 (1.9–23.2) | 0.019 * | 10.5 (0.96–59.4) | 11.5 (4.03–27.1) | 0.162 |
| Treatment | ||||||
| IVT (%) | 83 (9.0) | 4 (6.9) | 0.580 | 50 (5.0) | 2 (4.8) | 0.956 |
| AntiPlt (%) | 884 (96.1) | 55 (94.8) | 0.499 | 961 (95.6) | 40 (95.2) | 0.707 |
| DAPT (%) | 360 (39.1) | 28 (48.3) | 0.167 | 684 (68.1) | 27 (64.3) | 0.608 |
| Anticoagulant (%) | 31 (3.4) | 4 (6.9) | 0.148 | 83 (8.3) | 9 (21.4) | 0.008 * |
| AntiHTN (%) | 447 (48.6) | 27 (46.6) | 0.764 | 641 (63.8) | 25 (59.5) | 0.574 |
| AntiDM (%) | 255 (27.7) | 21 (36.2) | 0.164 | 353 (35.1) | 20 (47.6) | 0.098 |
| Statin (%) | 835 (90.8) | 55 (94.8) | 0.474 | 988 (98.3) | 41 (97.6) | 0.524 |
| EVT in 24 h (%) | 5 (0.5) | 2 (3.4) | 0.060 | 12 (1.2) | 0 (0.0) | 1.000 |
| Examination | ||||||
| Holter (%) | 75 (8.2) | 4 (6.9) | 1.000 | 517 (51.4) | 26 (61.9) | 0.408 |
| UCG (%) | 855 (92.9) | 54 (93.1) | 1.000 | 954 (94.9) | 41 (97.6) | 0.521 |
| CTA/MRA/DSA (%) | 818 (88.9) | 50 (86.2) | 0.527 | 957 (95.2) | 41 (97.6) | 0.717 |
| CVUS (%) | 839 (91.2) | 56 (96.6) | 0.222 | 936 (93.1) | 40 (95.2) | 0.859 |
| Outcome | ||||||
| LOS (days) | 14 (1–94) | 18 (3–40) | <0.001 * | 14 (2–90) | 20.5 (4–89) | <0.001 * |
| Mortality (%) | 10 (1.1) | 3 (5.2) | 0.037 * | 13 (1.3) | 3 (7.1) | 0.024 * |
| Pulmonary or urinary infection (%) | 68 (7.4) | 10 (17.2) | 0.020 * | 77 (7.7) | 19 (45.2) | <0.001 * |
| Haemorrhage (%) | 13 (1.4) | 1 (1.7) | 0.578 | 23 (2.3) | 5 (11.9) | 0.004 * |
| mRS (0–2, %) | 823 (89.5) | 41 (74.5) | <0.001 * | 877 (88.3) | 14 (36.8) | <0.001 * |
| Multivariate Analysis | ||||
|---|---|---|---|---|
| OR | 95% CI | p-Value | ||
| Stage 1 | ||||
| Aphasia | 0.394 | 0.200 | 0.775 | 0.007 |
| Infection | 2.566 | 1.155 | 5.702 | 0.021 |
| Glucose abnormality | 3.055 | 1.542 | 6.055 | 0.001 |
| TOAST | ||||
| UD | 1.000 | |||
| AA | 2.254 | 1.062 | 4.786 | 0.034 |
| Stage 2 | ||||
| Diabetes | 1.998 | 1.032 | 3.868 | 0.040 |
| Pulmonary or urinary infection | 9.856 | 4.918 | 19.750 | <0.001 |
| TOAST | ||||
| UD | 1.000 | |||
| SV | 0.059 | 0.007 | 0.492 | 0.009 |
| Combined | ||||
| Pulmonary or urinary infection | 4.658 | 2.843 | 7.631 | <0.001 |
| Glucose abnormality | 2.572 | 1.514 | 4.371 | <0.001 |
| TOAST | ||||
| UD | 1.000 | |||
| SV | 0.043 | 0.006 | 0.327 | 0.002 |
| Large-Artery Atherosclerosis | Minor Stroke | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | ||||
| Stage 1 | Stage 1 | ||||||||
| Pulmonary or urinary infection | 4.967 | 2.622 | 9.410 | <0.001 | Aphasia | 0.351 | 0.130 | 0.947 | 0.039 |
| Glucose abnormality | 3.300 | 1.789 | 6.085 | <0.001 | Glucose abnormality | 2.505 | 1.047 | 5.989 | 0.039 |
| Stage 2 | Average BP | 1.029 | 1.005 | 1.054 | 0.019 | ||||
| Diabetes | 3.050 | 1.265 | 7.352 | 0.013 | Stage 2 | ||||
| NIHSS score | 1.114 | 1.016 | 1.222 | 0.022 | Pulmonary or urinary infection | 12.078 | 3.378 | 43.191 | <0.001 |
| Pulmonary or urinary infection | 5.605 | 2.044 | 15.367 | 0.001 | Anticoagulants | 6.419 | 2.237 | 18.419 | 0.001 |
| Combined | Combined | ||||||||
| Pulmonary or urinary infection | 4.967 | 2.622 | 9.410 | <0.001 | Previous TIA | 2.622 | 1.254 | 5.483 | 0.010 |
| Glucose abnormality | 3.300 | 1.789 | 6.085 | <0.001 | Pulmonary or urinary infection | 4.161 | 1.791 | 9.667 | 0.001 |
| Anticoagulant | 4.252 | 1.895 | 9.541 | <0.001 | |||||
| Glucose abnormality | 3.002 | 1.495 | 6.026 | 0.002 | |||||
| AverageBP | 1.020 | 1.001 | 1.039 | 0.041 | |||||
| Combined (n = 1860) | Stage 1 (n = 898) | Stage 2 (n = 862) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Treatment Trends | OR | 95% CI | p-Value | OR | 95% CI | p-Value | OR | 95% CI | p-Value | |||
| Conserved | 1.000 | 1.000 | 1.000 | |||||||||
| Neutral | 1.211 | 0.714 | 2.056 | 0.477 | 1.499 | 0.803 | 2.798 | 0.204 | 1.412 | 0.472 | 4.227 | 0.538 |
| Positive | 1.871 | 1.019 | 3.437 | 0.043 # | 1.369 | 0.576 | 3.252 | 0.477 | 3.511 | 1.143 | 10.780 | 0.028 # |
| Conserved | Positive | |||||||
|---|---|---|---|---|---|---|---|---|
| Factor | OR | 95% CI | p-Value | OR | 95% CI | p-Value | ||
| Age (≥75 years) | 1.613 | 1.264 | 2.058 | <0.001 * | 0.886 | 0.642 | 1.223 | 0.462 |
| Previous IS | 1.013 | 0.783 | 1.310 | 0.922 | 1.357 | 1.016 | 1.813 | 0.038 # |
| Previous TIA | 1.013 | 0.683 | 1.502 | 0.948 | 0.742 | 0.441 | 1.249 | 0.262 |
| Hypertension | 0.865 | 0.692 | 1.083 | 0.206 | 1.137 | 0.862 | 1.500 | 0.365 |
| Diabetes | 0.701 | 0.562 | 0.874 | 0.002 * | 1.106 | 0.859 | 1.425 | 0.433 |
| History of hyperlipaemia | 0.940 | 0.729 | 1.211 | 0.940 | 0.995 | 0.738 | 1.342 | 0.995 |
| Paresis/ataxia | 0.547 | 0.431 | 0.696 | <0.001 * | 3.151 | 2.021 | 4.914 | <0.001 * |
| Aphasia | 0.826 | 0.637 | 1.070 | 0.148 | 1.466 | 1.109 | 1.938 | 0.007 * |
| Coma | 0.301 | 0.116 | 0.782 | 0.014 * | 2.668 | 1.539 | 4.624 | <0.001 * |
| AA | 0.632 | 0.512 | 0.781 | <0.001 * | 1.348 | 1.047 | 1.737 | 0.021 * |
| SV | 1.452 | 1.158 | 1.820 | 0.001 * | 0.686 | 0.506 | 0.930 | 0.015 * |
| IVT | 1.007 | 0.660 | 1.537 | 0.973 | 0.975 | 0.586 | 1.623 | 0.922 |
| AntiHTN | 0.874 | 0.709 | 1.079 | 0.211 | 1.110 | 0.862 | 1.430 | 0.419 |
| AntiDM | 0.646 | 0.512 | 0.816 | <0.001 * | 1.215 | 0.940 | 1.571 | 0.137 |
| Statin | 0.180 | 0.107 | 0.303 | <0.001 * | 1.364 | 0.508 | 3.663 | 0.538 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, G.; Yang, Q.; Zhang, H.; Huang, X.; Fu, Y.; Fan, D. The Clinical Features of In-Hospital Recurrence in Acute Ischaemic Stroke Patients over Time: A Real-World Observation at a Single Center. Brain Sci. 2022, 12, 123. https://doi.org/10.3390/brainsci12020123
Zhang G, Yang Q, Zhang H, Huang X, Fu Y, Fan D. The Clinical Features of In-Hospital Recurrence in Acute Ischaemic Stroke Patients over Time: A Real-World Observation at a Single Center. Brain Sciences. 2022; 12(2):123. https://doi.org/10.3390/brainsci12020123
Chicago/Turabian StyleZhang, Gaoqi, Qiong Yang, Huagang Zhang, Xiao Huang, Yu Fu, and Dongsheng Fan. 2022. "The Clinical Features of In-Hospital Recurrence in Acute Ischaemic Stroke Patients over Time: A Real-World Observation at a Single Center" Brain Sciences 12, no. 2: 123. https://doi.org/10.3390/brainsci12020123
APA StyleZhang, G., Yang, Q., Zhang, H., Huang, X., Fu, Y., & Fan, D. (2022). The Clinical Features of In-Hospital Recurrence in Acute Ischaemic Stroke Patients over Time: A Real-World Observation at a Single Center. Brain Sciences, 12(2), 123. https://doi.org/10.3390/brainsci12020123






