Signal Variability and Cognitive Function in Older Long-Term Survivors of Breast Cancer with Exposure to Chemotherapy: A Prospective Longitudinal Resting-State fMRI Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Rs-fMRI Acquisition and Analysis
2.3. Neurocognitive Testing
2.4. Statistical Analysis
3. Results
3.1. Study Participants
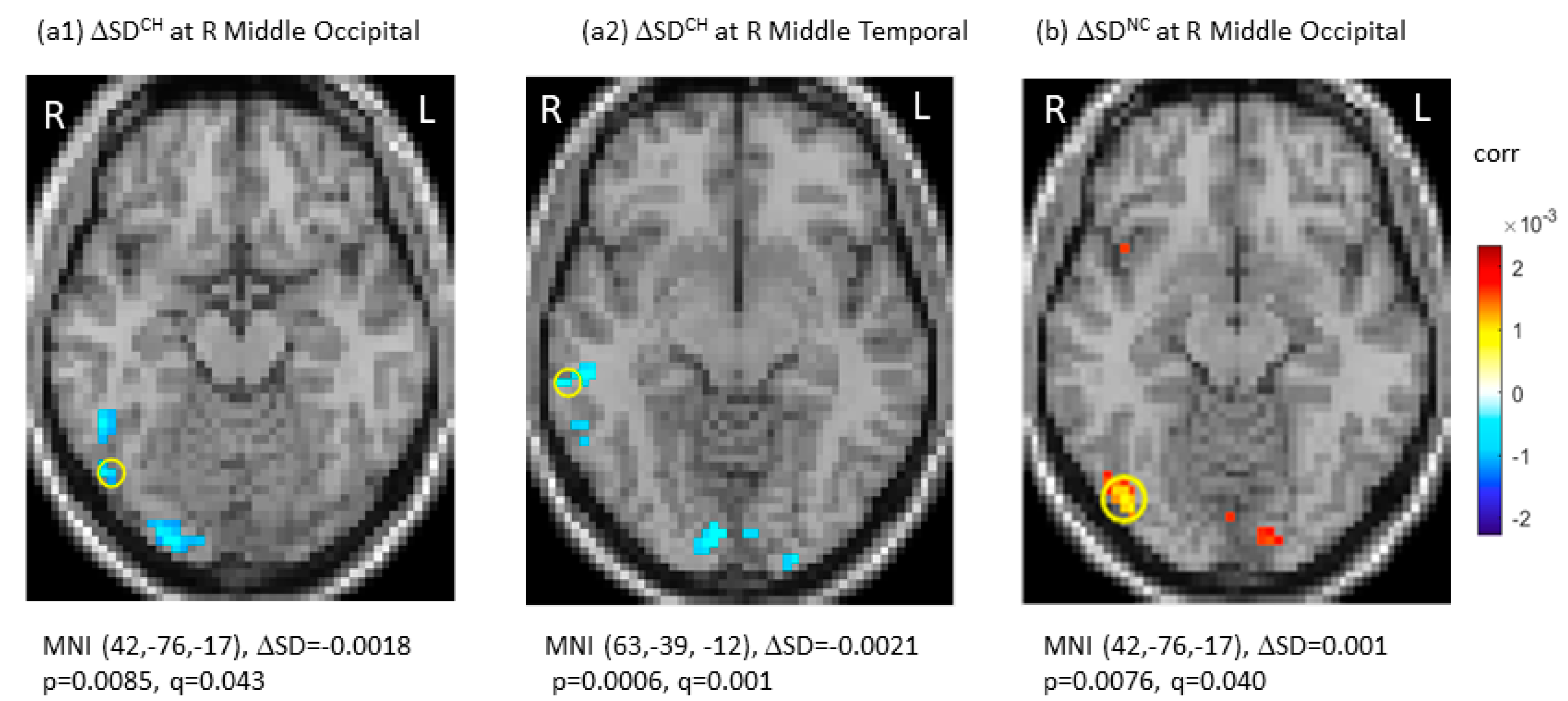
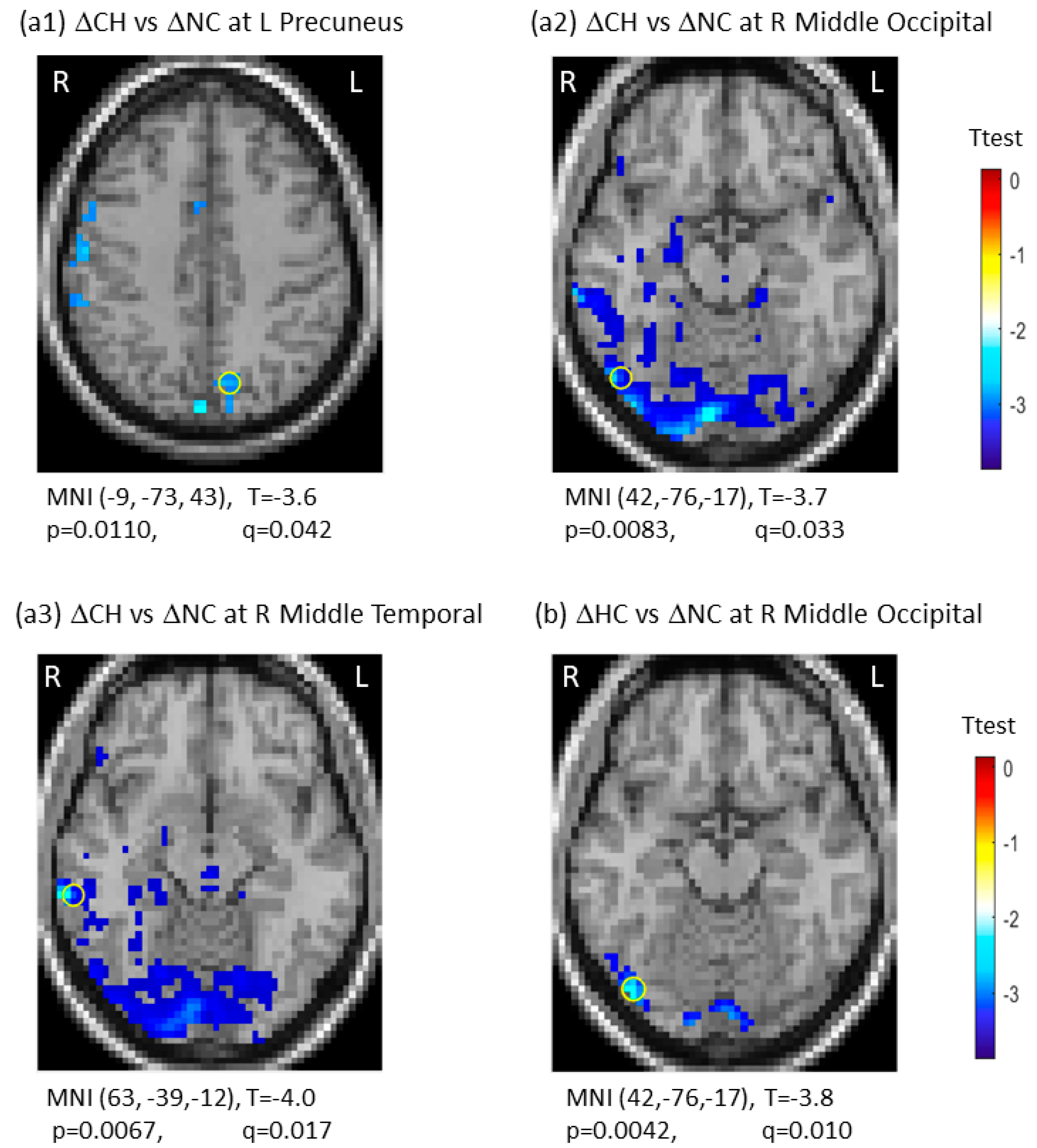
3.2. SDBOLD Data
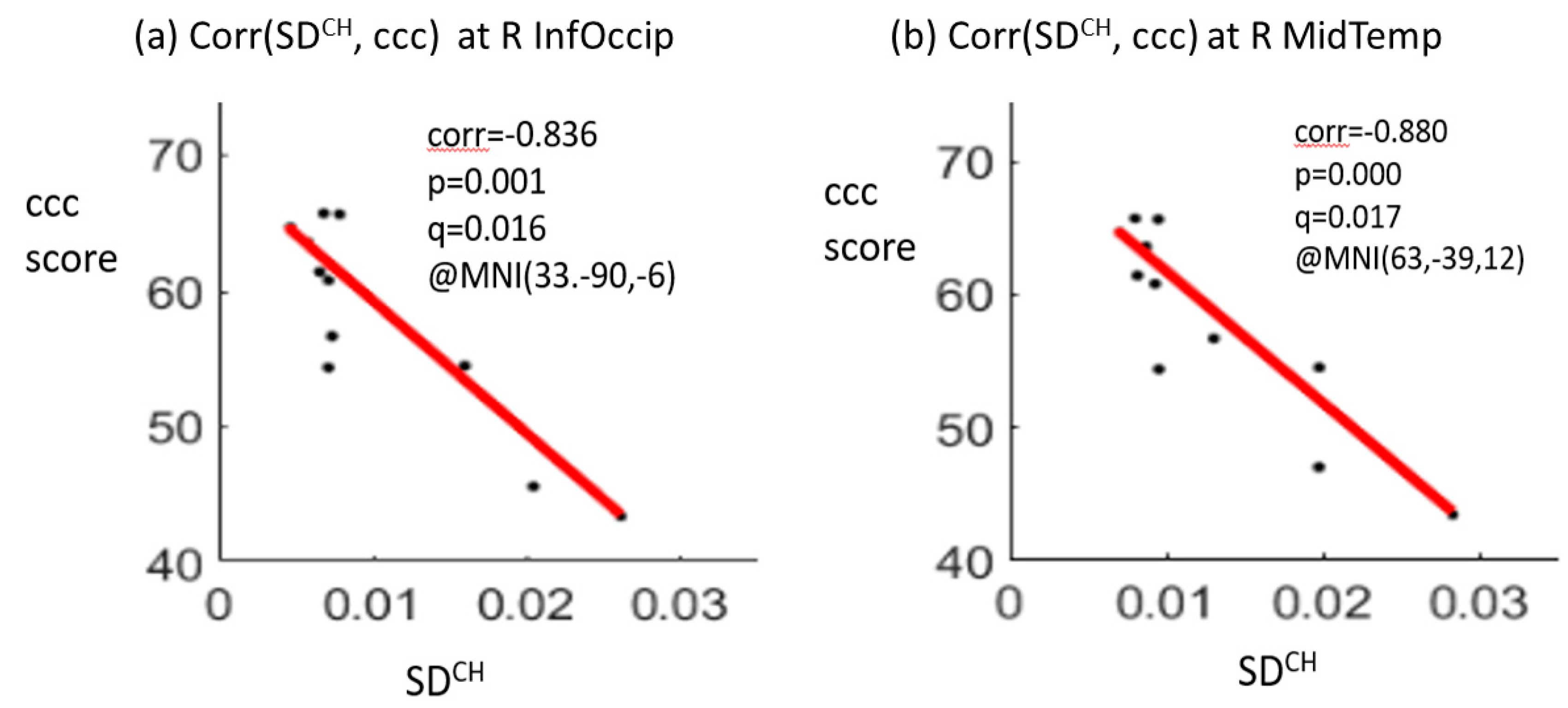
3.3. Correlation between SDBOLD and Neurocognitive Testing Scores
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nguyen, L.D.; Ehrlich, B.E. Cellular mechanisms and treatments for chemobrain: Insight from aging and neurodegenerative diseases. EMBO Mol. Med. 2020, 12, e12075. [Google Scholar] [CrossRef] [PubMed]
- Muss, H.B.; Berry, D.A.; Cirrincione, C.; Budman, D.R.; Henderson, I.C.; Citron, M.L.; Norton, L.; Winer, E.P.; Hudis, C.A. Toxicity of older and younger patients treated with adjuvant chemotherapy for node-positive breast cancer: The Cancer and Leukemia Group B Experience. J. Clin. Oncol. 2007, 25, 3699–3704. [Google Scholar] [CrossRef] [PubMed]
- Crivellari, D.; Bonetti, M.; Castiglione-Gertsch, M.; Gelber, R.D.; Rudenstam, C.M.; Thürlimann, B.; Price, K.N.; Coates, A.S.; Hürny, C.; Bernhard, J.; et al. Burdens and benefits of adjuvant cyclophosphamide, methotrexate, and fluorouracil and tamoxifen for elderly patients with breast cancer: The International Breast Cancer Study Group Trial VII. J. Clin. Oncol. 2000, 18, 1412–1422. [Google Scholar] [CrossRef]
- Pinder, M.C.; Duan, Z.; Goodwin, J.S.; Hortobagyi, G.N.; Giordano, S.H. Congestive heart failure in older women treated with adjuvant anthracycline chemotherapy for breast cancer. J. Clin. Oncol. 2007, 25, 3808–3815. [Google Scholar] [CrossRef] [PubMed]
- Koppelmans, V.; Breteler, M.M.; Boogerd, W.; Seynaeve, C.; Gundy, C.; Schagen, S.B. Neuropsychological performance in survivors of breast cancer more than 20 years after adjuvant chemotherapy. J. Clin. Oncol. 2012, 30, 1080–1086. [Google Scholar] [CrossRef]
- Merriman, J.D.; Sereika, S.M.; Brufsky, A.M.; McAuliffe, P.F.; McGuire, K.P.; Myers, J.S.; Phillips, M.L.; Ryan, C.M.; Gentry, A.L.; Jones, L.D.; et al. Trajectories of self-reported cognitive function in postmenopausal women during adjuvant systemic therapy for breast cancer. Psychooncology 2017, 26, 44–52. [Google Scholar] [CrossRef]
- De Ruiter, M.B.; Reneman, L.; Boogerd, W.; Veltman, D.J.; Van Dam, F.S.; Nederveen, A.J.; Boven, E.; Schagen, S.B. Cerebral hyporesponsiveness and cognitive impairment 10 years after chemotherapy for breast cancer. Hum. Brain Mapp. 2011, 32, 1206–1219. [Google Scholar] [CrossRef]
- Mandelblatt, J.S.; Hurria, A.; McDonald, B.C.; Saykin, A.J.; Stern, R.A.; VanMeter, J.W.; McGuckin, M.; Traina, T.; Denduluri, N.; Turner, S.; et al. Cognitive effects of cancer and its treatments at the intersection of aging: What do we know; what do we need to know? Semin. Oncol. 2013, 40, 709–725. [Google Scholar] [CrossRef]
- Holohan, K.N.; Von Ah, D.; McDonald, B.C.; Saykin, A.J. Neuroimaging, cancer, and cognition: State of the knowledge. Semin. Oncol. Nurs. 2013, 29, 280287. [Google Scholar] [CrossRef][Green Version]
- Miao, H.; Li, J.; Hu, S.; He, X.; Partridge, S.C.; Ren, J.; Bian, Y.; Yu, Y.; Qiu, B. Long-term cognitive impairment of breast cancer patients after chemotherapy: A functional MRI study. Eur. J. Radiol. 2016, 85, 1053–1057. [Google Scholar] [CrossRef]
- Chen, B.T.; Chen, Z.; Patel, S.K.; Rockne, R.C.; Wong, C.W.; Root, J.C.; Saykin, A.J.; Ahles, T.A.; Holodny, A.I.; Sun, C.L.; et al. Effect of chemotherapy on default mode network connectivity in older women with breast cancer. Brain Imaging Behav. 2021, 16, 43–53. [Google Scholar] [CrossRef] [PubMed]
- McDonald, B.C.; Conroy, S.K.; Ahles, T.A.; West, J.D.; Saykin, A.J. Alterations in brain activation during working memory processing associated with breast cancer and treatment: A prospective functional magnetic resonance imaging study. J. Clin. Oncol. 2012, 30, 25002508. [Google Scholar] [CrossRef]
- Laumann, T.O.; Snyder, A.Z.; Mitra, A.; Gordon, E.M.; Gratton, C.; Adeyemo, B.; Gilmore, A.W.; Nelson, S.M.; Berg, J.J.; Greene, D.J.; et al. On the Stability of BOLD fMRI Correlations. Cereb. Cortex 2017, 27, 4719–4732. [Google Scholar] [CrossRef]
- Chen, Z.; Chen, Z.; Chen, B.T. Brain functional connectivity (FC) invariance and variability under timeseries editing (timeset operation). Comput. Biol. Med. 2022, 142, 105190. [Google Scholar] [CrossRef]
- Beim Graben, P.; Jimenez-Marin, A.; Diez, I.; Cortes, J.M.; Desroches, M.; Rodrigues, S. Metastable Resting State Brain Dynamics. Front. Comput. Neurosci. 2019, 13, 62. [Google Scholar] [CrossRef]
- Tognoli, E.; Kelso, J.A. The metastable brain. Neuron 2014, 81, 35–48. [Google Scholar] [CrossRef] [PubMed]
- Garrett, D.D.; Samanez-Larkin, G.R.; MacDonald, S.W.; Lindenberger, U.; McIntosh, A.R.; Grady, C.L. Moment-to-moment brain signal variability: A next frontier in human brain mapping? Neurosci. Biobehav. Rev. 2013, 37, 610–624. [Google Scholar] [CrossRef]
- Garrett, D.D.; Skowron, A.; Wiegert, S.; Adolf, J.; Dahle, C.L.; Lindenberger, U.; Raz, N. Lost Dynamics and the Dynamics of Loss: Longitudinal Compression of Brain Signal Variability is Coupled with Declines in Functional Integration and Cognitive Performance. Cereb. Cortex 2021, 31, 5239–5252. [Google Scholar] [CrossRef] [PubMed]
- Grady, C.L.; Garrett, D.D. Understanding variability in the BOLD signal and why it matters for aging. Brain Imaging Behav. 2014, 8, 274283. [Google Scholar] [CrossRef]
- Nomi, J.S.; Bolt, T.S.; Ezie, C.E.C.; Uddin, L.Q.; Heller, A.S. Moment-to-Moment BOLD Signal Variability Reflects Regional Changes in Neural Flexibility across the Lifespan. J. Neurosci. 2017, 37, 5539–5548. [Google Scholar] [CrossRef]
- Weintraub, S.; Dikmen, S.S.; Heaton, R.K.; Tulsky, D.S.; Zelazo, P.D.; Bauer, P.J.; Carlozzi, N.E.; Slotkin, J.; Blitz, D.; Wallner-Allen, K.; et al. Cognition assessment using the NIH Toolbox. Neurology 2013, 80, S54–S64. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; Calhoun, V.; Chen, Z. Functional overestimation due to spatial smoothing of fMRI data. J. Neurosci. Methods 2017, 291, 1–12. [Google Scholar] [CrossRef] [PubMed]
- de Ruiter, M.B.; Reneman, L.; Boogerd, W.; Veltman, D.J.; Caan, M.; Douaud, G.; Lavini, C.; Linn, S.C.; Boven, E.; van Dam, F.S.; et al. Late effects of high-dose adjuvant chemotherapy on white and gray matter in breast cancer survivors: Converging results from multimodal magnetic resonance imaging. Hum. Brain Mapp. 2012, 33, 29712983. [Google Scholar] [CrossRef] [PubMed]
- Laird, N.M.; Ware, J.H. Random-effects models for longitudinal data. Biometrics 1982, 38, 963–974. [Google Scholar] [CrossRef]
- McDonald, B.C.; Conroy, S.K.; Ahles, T.A.; West, J.D.; Saykin, A.J. Gray matter reduction associated with systemic chemotherapy for breast cancer: A prospective MRI study. Breast Cancer Res. Treat. 2010, 123, 819–828. [Google Scholar] [CrossRef]
- Chen, B.T.; Jin, T.; Patel, S.K.; Ye, N.; Sun, C.L.; Ma, H.; Rockne, R.C.; Root, J.C.; Saykin, A.J.; Ahles, T.A.; et al. Gray matter density reduction associated with adjuvant chemotherapy in older women with breast cancer. Breast Cancer Res. Treat. 2018, 172, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Damoiseaux, J.S.; Rombouts, S.A.R.B.; Barkhof, F.; Scheltens, P.; Stam, C.J.; Smith, S.M.; Beckmann, C.F. Consistent resting-state networks across healthy subjects. Proc. Natl. Acad. Sci. USA 2006, 103, 13848–13853. [Google Scholar] [CrossRef]
- Raichle, M.E.; MacLeod, A.M.; Snyder, A.Z.; Powers, W.J.; Gusnard, D.A.; Shulman, G.L. A default mode of brain function. Proc. Natl. Acad. Sci. USA 2001, 98, 676–682. [Google Scholar] [CrossRef]
- Dumas, J.A.; Makarewicz, J.; Schaubhut, G.J.; Devins, R.; Albert, K.; Dittus, K.; Newhouse, P.A. Chemotherapy altered brain functional connectivity in women with breast cancer: A pilot study. Brain Imaging Behav. 2013, 7, 524–532. [Google Scholar] [CrossRef]
- Chen, B.T.; Jin, T.; Patel, S.K.; Ye, N.; Ma, H.; Wong, C.W.; Rockne, R.C.; Root, J.C.; Saykin, A.J.; Ahles, T.A.; et al. Intrinsic brain activity changes associated with adjuvant chemotherapy in older women with breast cancer: A pilot longitudinal study. Breast Cancer Res. Treat. 2019, 176, 181–189. [Google Scholar] [CrossRef]
- Ahles, T.A.; Saykin, A.J. Candidate mechanisms for chemotherapy-induced cognitive changes. Nat. Rev. Cancer 2007, 7, 192201. [Google Scholar] [CrossRef] [PubMed]
- Schroyen, G.; Blommaert, J.; Van Weehaeghe, D.; Sleurs, C.; Vandenbulcke, M.; Dedoncker, N.; Hatse, S.; Goris, A.; Koole, M.; Smeets, A.; et al. Neuroinflammation and Its Association with Cognition, Neuronal Markers and Peripheral Inflammation after Chemotherapy for Breast Cancer. Cancers 2021, 13, 4198. [Google Scholar] [CrossRef] [PubMed]
| All Participants | Participants Having Data for Both TP1 and TP2 | |||||||
|---|---|---|---|---|---|---|---|---|
| Parameters | CH N = 20 | NC N = 20 | HC N = 20 | p | CH N = 12 | NC N = 12 | HC N = 15 | p |
| Age (years) | ||||||||
| Mean (SD) | 73.5 (5.06) | 76.85 (4.63) | 74.00 (6.09) | 0.106 | 73.75 (5.41) | 76.50 (4.28) | 74.53 (6.73) | 0.477 |
| Median (Range) | 73.5 (66–84) | 77.5 (69–86) | 72.5 (66–88) | 71.50 (68–84) | 75.5 (71–86) | 73.00 (66–88) | ||
| Race (N, %) | ||||||||
| White or Caucasian | 15 (75) | 18 (90) | 18 (90) | 0.100 | 10 (83) | 11 (92) | 14 (93) | 0.765 |
| Black | 1 (5) | 2 (10) | 1 (8) | 1 (8) | ||||
| Asian/Native Hawaiian | 4 (20) | 1 (5) | 1 (8) | 1 (7) | ||||
| Other | 1 (5) | |||||||
| Ethnicity (N, %) | ||||||||
| Not Hispanic | 18 (90) | 20 (100) | 17 (85) | 0.352 | 10 (83) | 12 (100) | 13 (87) | 0.527 |
| Hispanic | 2 (10) | 3 (15) | 2 (17) | 2 (13) | ||||
| Marital Status (N, %) | ||||||||
| Married/Partner | 11 (55) | 12 (60) | 12 (60) | 0.988 | 6 (50) | 8 (67) | 9 (60) | 0.915 |
| Not married | 8 (40) | 8 (40) | 8 (40) | 5 (42) | 4 (33) | 6 (40) | ||
| Unknown | 1 (5) | 1 (8) | ||||||
| Highest grade (N, %) | ||||||||
| High school or less | 4 (20) | 5 (25) | 6 (30) | 0.327 | 3 (25) | 4 (33) | 4 (27) | 0.279 |
| Some college | 9 (45) | 7 (35) | 3 (15) | 6 (50) | 5 (42) | 2 (13) | ||
| Bachelor’s degree | 5 (25) | 7 (35) | 6 (30) | 2 (17) | 3 (25) | 5 (33) | ||
| Advanced degree | 2 (10) | 1 (5) | 5 (25) | 1 (8) | 4 (27) | |||
| Smoking (N, %) *1 | ||||||||
| No | 13 (65) | 13 (65) | 14 (70) | 0.928 | 7 (58) | 8 (67) | 11 (73) | 0.775 |
| Yes | 7 (35) | 7 (35) | 6 (30) | 5 (42) | 4 (33) | 4 (27) | ||
| BMI (kg/m2) | ||||||||
| Mean (SD) | 30.78 (6.03) | 27.11 (5.08) | 24.83 (5.08) | 0.004 | 29.89 (3.84) | 27.01 (4.90) | 23.63 (4.08) | 0.002 |
| Median (Range) | 29.9 (22.4–43.8) | 26.95 (18.7–35.9) | 24.05 (16.6–37.5) | 29.9 (23–37) | 26.00 (21–36) | 23.60 (17–31) | ||
| BOMC Score | ||||||||
| Mean (SD) | 2.90 (2.86) | 3.05 (2.89) | 2.89 (2.92) | 0.982 | 3.33 (2.74) | 1.83 (2.48) | 2.71 (2.67) | 0.385 |
| Median (Range) | 2 (0–8) | 2 (0–10) | 2 (0–10) | 2 (0–8) | 1(0–8) | 2(0–8) | ||
| Stage (N, %) | ||||||||
| DCIS | 1 (5) | 9 (45) | 1 (8) | 6 (50) | ||||
| I | 4 (20) | 8 (40) | 1 (8) | 4 (33) | ||||
| II | 14 (70) | 3 (15) | 10 (84) | 2 (17) | ||||
| III | 1 (5) | |||||||
| Regimen Non-Trastuzumab Regimen (N, %) | ||||||||
| AC-T | 2 (10) | |||||||
| TC | 9 (45) | 6 (50) | ||||||
| AC | 1 (5) | 1 (8) | ||||||
| CMF | 1 (5) | 1 (8) | ||||||
| TAC | 2 (10) | 1 (8) | ||||||
| Other *2 | 1 (5) | |||||||
| Trastuzumab Regimen (N, %) | ||||||||
| AC T + H | 1 (5) | 1 (8) | ||||||
| TCH | 1 (5) | 1 (8) | ||||||
| Other *3 | 2 (10) | 1 (8) | ||||||
| 1.SDBOLD difference at timepoint 1 (TP1) (thresholding by q < 0.05) CH vs. HC: None CH vs. NC: None HC vs. NC: None | ||||||
| 2.Longitudinal SDBOLD changes (ΔSDBOLD): CH: | ||||||
| ΔSDBOLD | t(t-test) | MNI | Region | p-value | q-value | |
| −0.0018 | −4.0 | (42, −76, 17) | Mid Occipital R | 0.0085 | 0.043 | |
| −0.0021 | −4.6 | (63, −39, −12) | Mid Temporal R | 0.0006 | 0.001 | |
| NC: | ||||||
| ΔSDBOLD | t(t-test) | MNI | Region | p-value | q-value | |
| 0.0010 | 3.9 | (42, −76, −17) | Mid Occipital R | 0.0076 | 0.040 | |
| HC: None | ||||||
| 3.Group-by-time interaction: ΔSDBOLD | ||||||
| CH vs. HC: None CH vs. NC: | ||||||
| ΔSDBOLD(CH) | ΔSDBOLD(NC) | t(t-test) | MNI | Region | p-value | q-value |
| −0.0025 | 0.0010 | −3.5 | (−9, −73, 43) | Precuneus L | 0.0110 | 0.042 |
| −0.0019 | 0.0023 | −3.7 | (42, −76, −17) | Mid Occipital R | 0.0083 | 0.033 |
| −0.0013 | 0.0006 | −4.0 | (63, −39, −12) | Mid Temporal R | 0.0067 | 0.017 |
| HC vs. NC: | ||||||
| ΔSDBOLD(HC) | ΔSDBOLD(NC) | t(t-test) | MNI | Region | p-value | q-value |
| −0.0012 | 0.0023 | −3.8 | (42, −76, −17) | Mid Occipital R | 0.0042 | 0.010 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, B.T.; Chen, Z.; Deng, F.; Patel, S.K.; Sedrak, M.S.; Root, J.C.; Ahles, T.A.; Razavi, M.; Kim, H.; Sun, C.-L.; et al. Signal Variability and Cognitive Function in Older Long-Term Survivors of Breast Cancer with Exposure to Chemotherapy: A Prospective Longitudinal Resting-State fMRI Study. Brain Sci. 2022, 12, 1283. https://doi.org/10.3390/brainsci12101283
Chen BT, Chen Z, Deng F, Patel SK, Sedrak MS, Root JC, Ahles TA, Razavi M, Kim H, Sun C-L, et al. Signal Variability and Cognitive Function in Older Long-Term Survivors of Breast Cancer with Exposure to Chemotherapy: A Prospective Longitudinal Resting-State fMRI Study. Brain Sciences. 2022; 12(10):1283. https://doi.org/10.3390/brainsci12101283
Chicago/Turabian StyleChen, Bihong T., Zikuan Chen, Frank Deng, Sunita K. Patel, Mina S. Sedrak, James C. Root, Tim A. Ahles, Marianne Razavi, Heeyoung Kim, Can-Lan Sun, and et al. 2022. "Signal Variability and Cognitive Function in Older Long-Term Survivors of Breast Cancer with Exposure to Chemotherapy: A Prospective Longitudinal Resting-State fMRI Study" Brain Sciences 12, no. 10: 1283. https://doi.org/10.3390/brainsci12101283
APA StyleChen, B. T., Chen, Z., Deng, F., Patel, S. K., Sedrak, M. S., Root, J. C., Ahles, T. A., Razavi, M., Kim, H., Sun, C.-L., & Dale, W. (2022). Signal Variability and Cognitive Function in Older Long-Term Survivors of Breast Cancer with Exposure to Chemotherapy: A Prospective Longitudinal Resting-State fMRI Study. Brain Sciences, 12(10), 1283. https://doi.org/10.3390/brainsci12101283






