From Shunt to Recovery: A Multidisciplinary Approach to Hydrocephalus Treatment in Severe Acquired Brain Injury Rehabilitation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Outcome Measures
2.3. Statistical Analysis
3. Results
3.1. Factors Associated with Length of Hospital Stay
3.2. Rehabilitation Outcomes and Associated Factors
3.3. Subgroup Analysis on Patients Undergoing VPS during Rehabilitation
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grabljevec, K.; Singh, R.; Denes, Z.; Angerova, Y.; Nunes, R.; Boldrini, P.; Delargy, M.; Laxe, S.; Kiekens, C.; Christodoulou, N. Evidence-based position paper on Physical and Rehabilitation Medicine professional practice for Adults with Acquired Brain Injury. The European PRM position (UEMS PRM Section). Eur. J. Phys. Rehabil. Med. 2018, 54, 971–979. [Google Scholar] [CrossRef]
- De Tanti, A.; Zampolini, M.; Pregno, S.; Group, C. Recommendations for clinical practice and research in severe brain injury in intensive rehabilitation: The Italian Consensus Conference. Eur. J. Phys. Rehabil. Med. 2015, 51, 89–103. [Google Scholar]
- Ganesh, S.; Guernon, A.; Chalcraft, L.; Harton, B.; Smith, B.; Louise-Bender Pape, T. Medical comorbidities in disorders of consciousness patients and their association with functional outcomes. Arch. Phys. Med. Rehabil. 2013, 94, 1899–1907. [Google Scholar] [CrossRef] [PubMed]
- Whyte, J.; Nordenbo, A.M.; Kalmar, K.; Merges, B.; Bagiella, E.; Chang, H.; Yablon, S.; Cho, S.; Hammond, F.; Khademi, A.; et al. Medical complications during inpatient rehabilitation among patients with traumatic disorders of consciousness. Arch. Phys. Med. Rehabil. 2013, 94, 1877–1883. [Google Scholar] [CrossRef]
- Weintraub, A.H.; Gerber, D.J.; Kowalski, R.G. Posttraumatic Hydrocephalus as a Confounding Influence on Brain Injury Rehabilitation: Incidence, Clinical Characteristics, and Outcomes. Arch. Phys. Med. Rehabil. 2017, 98, 312–319. [Google Scholar] [CrossRef]
- Mazzini, L.; Campini, R.; Angelino, E.; Rognone, F.; Pastore, I.; Oliveri, G. Posttraumatic hydrocephalus: A clinical, neuroradiologic, and neuropsychologic assessment of long-term outcome. Arch. Phys. Med. Rehabil. 2003, 84, 1637–1641. [Google Scholar] [CrossRef]
- Marmarou, A.; Foda, M.A.; Bandoh, K.; Yoshihara, M.; Yamamoto, T.; Tsuji, O.; Zasler, N.; Ward, J.D.; Young, H.F. Posttraumatic ventriculomegaly: Hydrocephalus or atrophy? A new approach for diagnosis using CSF dynamics. J. Neurosurg. 1996, 85, 1026–1035. [Google Scholar] [CrossRef]
- Guyot, L.L.; Michael, D.B. Post-traumatic hydrocephalus. Neurol. Res. 2000, 22, 25–28. [Google Scholar] [CrossRef]
- Lalou, A.D.; Levrini, V.; Czosnyka, M.; Gergelé, L.; Garnett, M.; Kolias, A.; Hutchinson, P.J.; Czosnyka, Z. Cerebrospinal fluid dynamics in non-acute post-traumatic ventriculomegaly. Fluids Barriers CNS 2020, 17, 24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rasmussen, M.K.; Mestre, H.; Nedergaard, M. The glymphatic pathway in neurological disorders. Lancet Neurol. 2018, 17, 1016–1024. [Google Scholar] [CrossRef] [Green Version]
- Dehdashti, A.R.; Rilliet, B.; Rufenacht, D.A.; de Tribolet, N. Shunt-dependent hydrocephalus after rupture of intracranial aneurysms: A prospective study of the influence of treatment modality. J. Neurosurg. 2004, 101, 402–407. [Google Scholar] [CrossRef]
- Chen, K.H.; Lee, C.P.; Yang, Y.H.; Yang, Y.H.; Chen, C.M.; Lu, M.L.; Lee, Y.C.; Chen, V.C. Incidence of hydrocephalus in traumatic brain injury: A nationwide population-based cohort study. Medicine 2019, 98, e17568. [Google Scholar] [CrossRef]
- Kowalski, R.G.; Weintraub, A.H.; Rubin, B.A.; Gerber, D.J.; Olsen, A.J. Impact of timing of ventriculoperitoneal shunt placement on outcome in posttraumatic hydrocephalus. J. Neurosurg. 2018, 23, 1–12. [Google Scholar] [CrossRef]
- Timofeev, I.; Czosnyka, M.; Nortje, J.; Smielewski, P.; Kirkpatrick, P.; Gupta, A.; Hutchinson, P. Effect of decompressive craniectomy on intracranial pressure and cerebrospinal compensation following traumatic brain injury. J. Neurosurg. 2008, 108, 66–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vedantam, A.; Yamal, J.M.; Hwang, H.; Robertson, C.S.; Gopinath, S.P. Factors associated with shunt-dependent hydrocephalus after decompressive craniectomy for traumatic brain injury. J. Neurosurg. 2018, 128, 1547–1552. [Google Scholar] [CrossRef] [PubMed]
- Tribl, G.; Oder, W. Outcome after shunt implantation in severe head injury with post-traumatic hydrocephalus. Brain Inj. 2000, 14, 345–354. [Google Scholar]
- Qian, C.; Yu, X.; Chen, J.; Gu, C.; Wang, L.; Chen, G.; Dai, Y. Effect of the drainage of cerebrospinal fluid in patients with aneurismal subarachnoid hemorrhage: A meta-analysis. Medicine 2016, 95, e5140. [Google Scholar] [CrossRef]
- Wang, Y.; Wen, L.; You, W.; Zhu, Y.; Wang, H.; Sun, Y.; Bao, W.; Yang, X. Predicting the outcomes of shunt implantation in patients with post-traumatic hydrocephalus and severe conscious disturbance: A scoring system based on clinical characteristics. J. Integr. Neurosci. 2020, 19, 31–37. [Google Scholar] [PubMed]
- Licata, C.; Cristofori, L.; Gambin, R.; Vivenza, C.; Turazzi, S. Post-traumatic hydrocephalus. J. Neurosurg. Sci. 2001, 45, 141–149. [Google Scholar] [PubMed]
- Hiler, M.; Czosnyka, M.; Hutchinson, P.; Balestreri, M.; Smielewski, P.; Matta, B.; Pickard, J.D. Predictive value of initial computerized tomography scan, intracranial pressure, and state of autoregulation in patients with traumatic brain injury. J. Neurosurg. 2006, 104, 731–737. [Google Scholar] [CrossRef]
- Chen, H.; Yuan, F.; Chen, S.W.; Guo, Y.; Wang, G.; Deng, Z.F.; Tian, H.L. Predicting posttraumatic hydrocephalus: Derivation and validation of a risk scoring system based on clinical characteristics. Metab. Brain Dis. 2017, 32, 1427–1435. [Google Scholar] [CrossRef] [PubMed]
- Formisano, R.; Azicnuda, E.; Sefid, M.K.; Zampolini, M.; Scarponi, F.; Avesani, R. Early rehabilitation: Benefits in patients with severe acquired brain injury. Neurol. Sci. 2017, 38, 181–184. [Google Scholar] [CrossRef]
- Bendel, P.; Koivisto, T.; Äikiä, M.; Niskanen, E.; Könönen, M.; Hänninen, T.; Vanninen, R. Atrophic enlargement of CSF volume after subarachnoid hemorrhage: Correlation with neuropsychological outcome. Am. J. Neuroradiol. 2010, 31, 370–376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flannery, J.; Land, K. Teaching acute care nurses cognitive assessment using LOCFAS: What’s the best method? J. Neurosci. Nurs. 2001, 33, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Rappaport, M.; Hall, K.M.; Hopkins, K.; Belleza, T.; Cope, D.N. Disability rating scale for severe head trauma: Coma to community. Arch. Phys. Med. Rehabil. 1982, 63, 118–123. [Google Scholar] [PubMed]
- Galeoto, G.; Turriziani, S.; Berardi, A.; Sansoni, J.; Santilli, V.; Mascio, M.; Paoloni, M. Levels of Cognitive Functioning Assessment Scale: Italian cross-cultural adaptation and validation. Ann Ig 2020, 32, 16–26. [Google Scholar] [PubMed]
- Sherer, M.; Yablon, S.A.; Nakase-Richardson, R.; Nick, T.G. Effect of Severity of Post-Traumatic Confusion and Its Constituent Symptoms on Outcome After Traumatic Brain Injury. Arch. Phys. Med. Rehabil. 2008, 89, 42–47. [Google Scholar] [CrossRef]
- Williams, M.W.; Smith, E.L. Clinical utility and psychometric properties of the Disability Rating Scale with individuals with traumatic brain injury. Rehabil. Psychol. 2017, 62, 407–408. [Google Scholar] [CrossRef]
- Kammersgaard, L.P.; Linnemann, M.; Tibæk, M. Hydrocephalus following severe traumatic brain injury in adults. Incidence, timing, and clinical predictors during rehabilitation. NeuroRehabilitation 2013, 33, 473–480. [Google Scholar] [CrossRef] [PubMed]
- Denes, Z.; Barsi, P.; Szel, I.; Boros, E.; Fazekas, G. Complication during postacute rehabilitation: Patients with posttraumatic hydrocephalus. Int. J. Rehabil. Res. 2011, 34, 222–226. [Google Scholar] [CrossRef]
- Gouvier, W.D.; Blanton, P.D.; LaPorte, K.K.; Nepomuceno, C. Reliability and validity of the Disability Rating Scale and the Levels of Cognitive Functioning Scale in monitoring recovery from severe head injury. Arch. Phys. Med. Rehabil. 1987, 68, 94–97. [Google Scholar] [CrossRef]
- Rossato, E.; Verzini, E.; Scandola, M.; Ferrari, F.; Bonadiman, S. Role of LCF scale as an outcome prognostic index in patients with traumatic brain injury. Neurol. Sci. 2021, 42, 2747–2752. [Google Scholar] [CrossRef]
- De Bonis, P.; Mangiola, A.; Pompucci, A.; Formisano, R.; Mattogno, P.; Anile, C. CSF dynamics analysis in patients with post-traumatic ventriculomegaly. Clin. Neurol. Neurosurg. 2013, 115, 49–53. [Google Scholar] [CrossRef]
- Xin, H.; Yun, S.; Jun, X.; Liang, W.; Cao, Y.-L.; Yang, X.-F. Long-term outcomes after shunt implantation in patients with posttraumatic hydrocephalus and severe conscious disturbance. J. Craniofac. Surg. 2014, 25, 1280–1283. [Google Scholar] [CrossRef]
- Wen, L.; Wan, S.; Zhan, R.Y.; Li, G.; Gong, J.B.; Liu, W.G.; Yang, X.F. Shunt implantation in a special sub-group of post-traumatic hydrocephalus--patients have normal intracranial pressure without clinical representations of hydrocephalus. Brain Inj. 2009, 23, 61–64. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S.; Lee, S.U.; Cha, J.H.; Heo, W.; Song, J.S.; Kim, S.J. Clinical Analysis of Results of Shunt Operation for Hydrocephalus Following Traumatic Brain Injury. Korean J. Neurotrauma 2015, 11, 58–62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sheffler, L.R.; Ito, V.Y.; Philip, P.A.; Sahgal, V. Shunting in chronic post-traumatic hydrocephalus: Demonstration of neurophysiologic improvement. Arch. Phys. Med. Rehabil. 1994, 75, 338–341. [Google Scholar] [CrossRef]
- Honeybul, S.; Ho, K.M. Incidence and risk factors for post-traumatic hydrocephalus following decompressive craniectomy for intractable intracranial hypertension and evacuation of mass lesions. J. Neurotrauma 2012, 29, 1872–1878. [Google Scholar] [CrossRef] [PubMed]
- Dijkers, M.; Brandstater, M.; Horn, S.; Ryser, D.; Barrett, R. Inpatient rehabilitation for traumatic brain injury: The influence of age on treatments and outcomes. NeuroRehabilitation 2013, 32, 233–252. [Google Scholar] [CrossRef]
- Bonow, R.H.; Oron, A.P.; Hanak, B.W.; Browd, S.R.; Chesnut, R.M.; Ellenbogen, R.G.; Vavilala, M.S.; Rivara, F.P. Post-Traumatic Hydrocephalus in Children: A Retrospective Study in 42 Pediatric Hospitals Using the Pediatric Health Information System. Neurosurgery 2018, 83, 732–739. [Google Scholar] [CrossRef]
- Czosnyka, M.; Czosnyka, Z.H.; Whitfield, P.C.; Donovan, T.; Pickard, J.D. Age dependence of cerebrospinal pressure-volume compensation in patients with hydrocephalus. J. Neurosurg. 2001, 94, 482–486. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Black, P.M.; Hakim, R.; Bailey, N.O. The use of the Codman-Medos Programmable Hakim valve in the management of patients with hydrocephalus: Illustrative cases. Neurosurgery 1994, 34, 1110–1113. [Google Scholar] [CrossRef] [PubMed]
- Miyake, H.; Ohta, T.; Kajimoto, Y.; Nagao, K. New concept for the pressure setting of a programmable pressure valve and measurement of in vivo shunt flow performed using a microflow meter. J. Neurosurg. 2000, 92, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Missori, P.; Miscusi, M.; Formisano, R.; Peschillo, S.; Polli, F.M.; Melone, A.; Martini, S.; Paolini, S.; Delfini, R. Magnetic resonance imaging flow void changes after cerebrospinal fluid shunt in post-traumatic hydrocephalus: Clinical correlations and outcome. Neurosurg. Rev. 2006, 29, 224–228. [Google Scholar] [CrossRef]
- Li, G.; Wen, L.; Zhan, R.Y.; Shen, F.; Yang, X.F.; Fu, W.M. Cranioplasty for patients developing large cranial defects combined with post-traumatic hydrocephalus after head trauma. Brain Inj. 2008, 22, 333–337. [Google Scholar] [CrossRef] [PubMed]
| Total Sample | VPS Placement before Admission | VPS Placement during Rehabilitation | p-Value | |
|---|---|---|---|---|
| N = 82 | N = 23 | N = 59 | ||
| Age, mean ± SD | 49.7 ± 17.8 | 48.2 ± 18.9 | 50.3 ± 17.5 | 0.691 |
| Male, n (%) | 40 (49%) | 10 (43%) | 30 (51%) | 0.549 |
| Etiology, n (%) | 0.475 | |||
| Non-Traumatic Hemorrhagic | 45 (55%) | 14 (61%) | 31 (53%) | |
| Traumatic | 29 (35%) | 6 (26%) | 23 (39%) | |
| Other | 8 (10%) | 3 (13%) | 5 (8%) | |
| Time to hospitalization (days) †, median (IQ range) | 48 (29–91) | 87 (71–130) | 36 (26–61) | <0.001 |
| Time to surgery (days) §, median (IQ range) | 119 (64–186) | 56 (35–86) | 151 (89–207) | <0.001 |
| Valve type, n (%) | 0.852 | |||
| Fixed | 37 (45%) | 10 (43%) | 27 (46%) | |
| Programmable | 45 (55%) | 13 (57%) | 32 (54%) | |
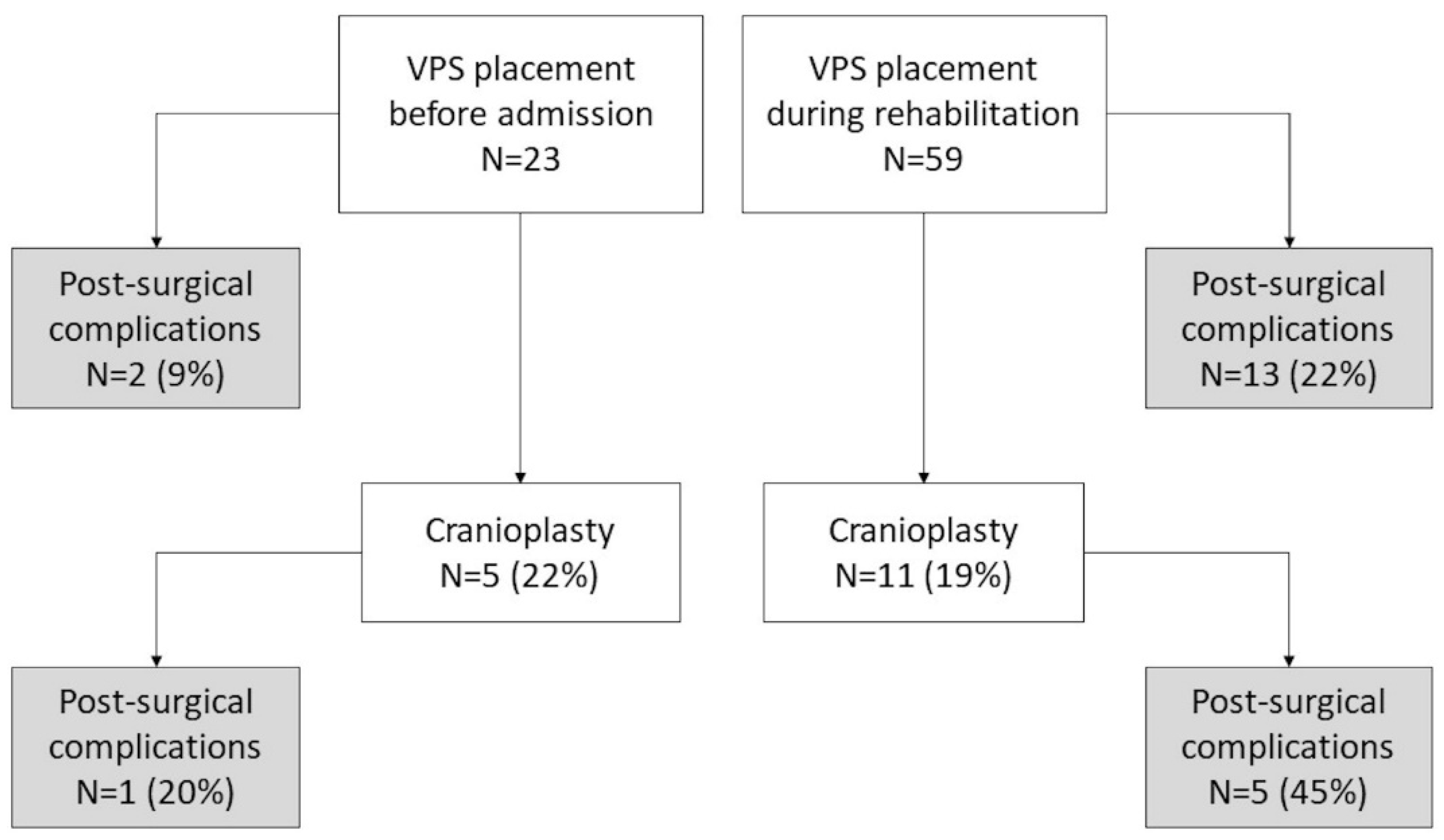
| VPS Complications, n (%) | 15 (18%) | 2 (9%) | 13 (22%) | 0.213 |
| Cranioplasty, n (%) | 16 (20%) | 5 (22%) | 11 (19%) | 0.762 |
| Cranioplasty Complications * | 6 (38%) | 1 (20%) | 5 (45%) | |
| LCF, mean ±SD | ||||
| Upon admission | 3.0 ± 1.3 | 3.3 ± 1.4 | 2.8 ± 1.3 | 0.178 |
| At discharge | 4.8 ± 1.7 | 5.0 ± 1.7 | 4.7 ± 1.8 | 0.478 |
| DRS, mean ± SD | ||||
| Upon admission | 21.2 ± 4.8 | 19.8 ± 4.7 | 21.7 ± 4.8 | 0.069 |
| At discharge | 14.5 ± 6.0 | 13.7 ± 5.8 | 14.8 ± 6.0 | 0.445 |
| Length of hospital stay (days), median (IQ range) | 221 (160–317) | 189 (125–317) | 227 (165–325) | 0.297 |
| Discharge, n (%) | 0.263 | |||
| At home | 46 (56%) | 17 (74%) | 29 (49%) | |
| Hospital | 20 (24%) | 3 (13%) | 17 (29%) | |
| Long-term Care Facility | 14 (17%) | 3 (13%) | 11 (19%) | |
| Deceased | 2 (2%) | 0 (0%) | 2 (3%) |
| Univariate Regressions | Multiple Regression | |||
|---|---|---|---|---|
| OR (95%CI) | p-Value | OR (95%CI) | p-Value | |
| Age | 0.97 (0.94–1.00) | 0.099 | 0.94 (0.90–0.99) | 0.008 |
| Male | 3.6 (1.0–12.5) | 0.043 | ||
| Etiology | 0.754 | |||
| Non-Traumatic Hemorrhagic (ref. cat.) | 1.0 | |||
| Traumatic | 1.4 (0.4–4.7) | |||
| Other | 1.8 (0.3–10.9) | |||
| Time to hospitalization (weeks) † | 1.06 (1.00–1.13) | 0.039 | ||
| Time to surgery (weeks) § | 1.02 (0.97–1.07) | 0.450 | ||
| VPS during rehabilitation | 3.0 (0.6–14.3) | 0.176 | ||
| Fixed-type valve | 6.7 (1.7–26.1) | 0.006 | 16.1 (3.1–84.4) | 0.002 |
| Univariate Regressions | Multiple Regression | |||
|---|---|---|---|---|
| b (95%CI) | p-Value | b (95%CI) | p-Value | |
| Age | −0.27 (−0.45–−0.09) | 0.004 | −0.29 (−0.46–−0.12) | 0.002 |
| Male | 5.39 (−1.13–11.91) | 0.104 | ||
| Etiology | 0.007 | |||
| Non-Traumatic Hemorrhagic (ref. cat.) | 1.00 | |||
| Traumatic | 10.37 (3.59–17.15) | |||
| Other | 10.30 (−0.51–21.11) | |||
| Time to hospitalization (weeks) † | 0.32 (−0.06–0.70) | 0.101 | ||
| Time to surgery (weeks) § | 0.40 (0.12–0.68) | 0.006 | 0.38 (0.11–0.64) | 0.006 |
| VPS during rehabilitation | 2.96 (−4.36–10.29) | 0.423 | ||
| Valve type fixed | −7.09 (−13.58–−0.61) | 0.032 | ||
| VPS Complications | 2.94 (−5.80–11.69) | 0.505 | ||
| Cranioplasty | −0.93 (−9.46–7.61) | 0.829 | ||
| Univariate Regressions | Multiple Regression | |||
|---|---|---|---|---|
| b (95%CI) | p-Value | b (95%CI) | p-Value | |
| Age | 0.02 (0.00–0.04) | 0.032 | ||
| Male | −0.46 (−1.22–0.31) | 0.239 | ||
| Etiology | 0.164 | |||
| Non-Traumatic Hemorrhagic (ref. cat.) | 1.00 | |||
| Traumatic | −0.75 (−1.56–0.07) | |||
| Other | −0.73 (2.12–0.66) | |||
| Time to hospitalization (weeks) † | −0.01 (−0.06–0.04) | 0.697 | ||
| Time to surgery (weeks) § | −0.02 (−0.05–0.02) | 0.340 | ||
| VPS during rehabilitation | −0.31 (−1.16–0.55) | 0.478 | ||
| Valve type fixed | 0.06 (−0.73–0.84) | 0.885 | ||
| VPS Complications | −0.91 (−1.91–0.09) | 0.073 | ||
| Cranioplasty | −1.03 (−1.97–−0.09) | 0.032 | −0.85 (−1.55–−0.14) | 0.019 |
| Length of hospital stay (weeks) * | −0.04 (−0.07–−0.02) | 0.001 | ||
| Score on admission | 0.90 (0.69–1.12) | <0.001 | 0.89 (0.68–1.10) | <0.001 |
| Univariate Linear Regressions | Multiple Regression | |||
|---|---|---|---|---|
| b (95%CI) | p-Value | b (95%CI) | p-Value | |
| Age | −0.08 (−0.15–−0.01) | 0.029 | ||
| Male | 1.50 (−1.16–4.16) | 0.265 | ||
| Etiology | 0.610 | |||
| Non-Traumatic Hemorrhagic (ref. cat.) | 1.00 | |||
| Traumatic | 1.41 (−1.45–4.28) | |||
| Other | 0.99 (−3.88–5.87) | |||
| Time to hospitalization (weeks) † | 0.04 (−0.12–0.20) | 0.636 | ||
| Time to surgery (weeks) § | 0.06 (−0.06–0.19) | 0.301 | ||
| VPS during rehabilitation | 1.14 (−1.81–4.09) | 0.445 | ||
| Valve type fixed | −1.89 (−4.56–0.78) | 0.162 | ||
| VPS Complications | 2.12 (−1.37–5.62) | 0.230 | ||
| Cranioplasty | 3.02 (−0.26–6.30) | 0.071 | 2.66 (0.33–4.99) | 0.026 |
| Length of hospital stay (weeks) * | 0.15 (0.07–0.24) | 0.001 | 0.08 (0.01–0.14) | 0.026 |
| Score on admission | 0.87 (0.67–1.07) | <0.001 | 0.79 (0.59–0.99) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castellani, G.B.; Miccoli, G.; Cava, F.C.; Salucci, P.; Colombo, V.; Maietti, E.; Palandri, G. From Shunt to Recovery: A Multidisciplinary Approach to Hydrocephalus Treatment in Severe Acquired Brain Injury Rehabilitation. Brain Sci. 2022, 12, 3. https://doi.org/10.3390/brainsci12010003
Castellani GB, Miccoli G, Cava FC, Salucci P, Colombo V, Maietti E, Palandri G. From Shunt to Recovery: A Multidisciplinary Approach to Hydrocephalus Treatment in Severe Acquired Brain Injury Rehabilitation. Brain Sciences. 2022; 12(1):3. https://doi.org/10.3390/brainsci12010003
Chicago/Turabian StyleCastellani, Giovanna B., Giovanni Miccoli, Francesca C. Cava, Pamela Salucci, Valentina Colombo, Elisa Maietti, and Giorgio Palandri. 2022. "From Shunt to Recovery: A Multidisciplinary Approach to Hydrocephalus Treatment in Severe Acquired Brain Injury Rehabilitation" Brain Sciences 12, no. 1: 3. https://doi.org/10.3390/brainsci12010003
APA StyleCastellani, G. B., Miccoli, G., Cava, F. C., Salucci, P., Colombo, V., Maietti, E., & Palandri, G. (2022). From Shunt to Recovery: A Multidisciplinary Approach to Hydrocephalus Treatment in Severe Acquired Brain Injury Rehabilitation. Brain Sciences, 12(1), 3. https://doi.org/10.3390/brainsci12010003






