A Diagnostic Dilemma of White Matter Lesions and Cerebral Oedema without Identifiable Cause—A Neurological Conundrum
Abstract
1. Introduction
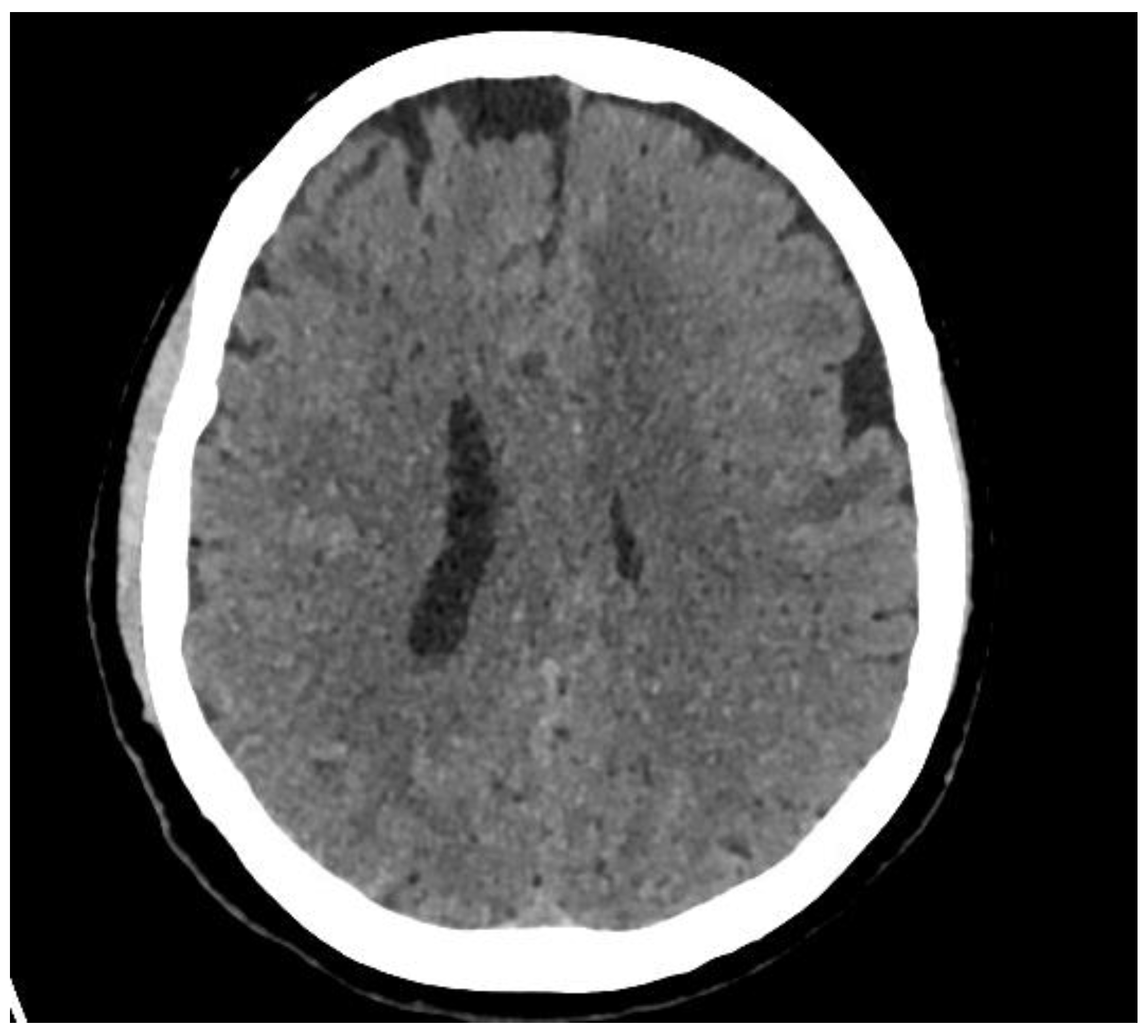
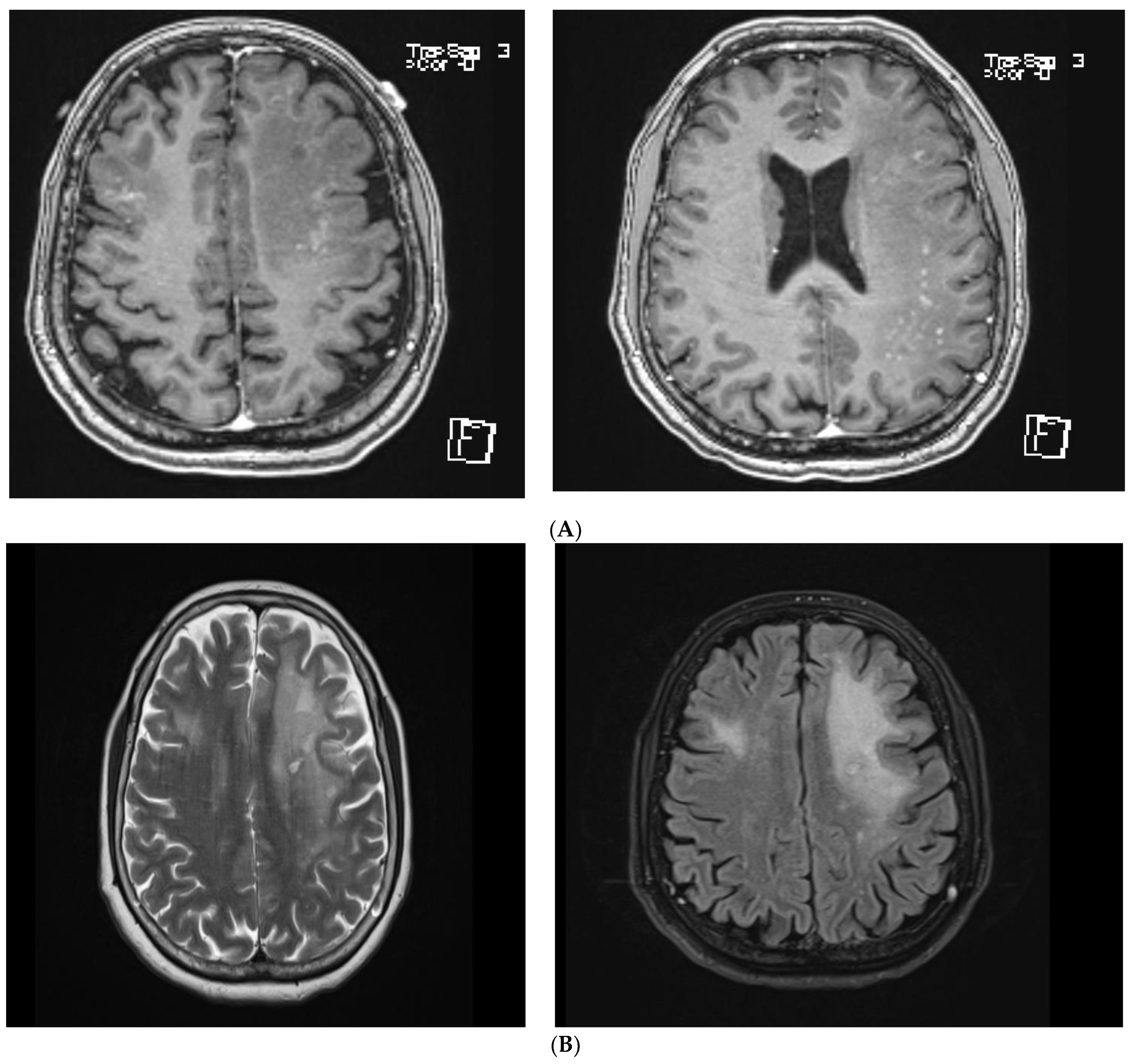
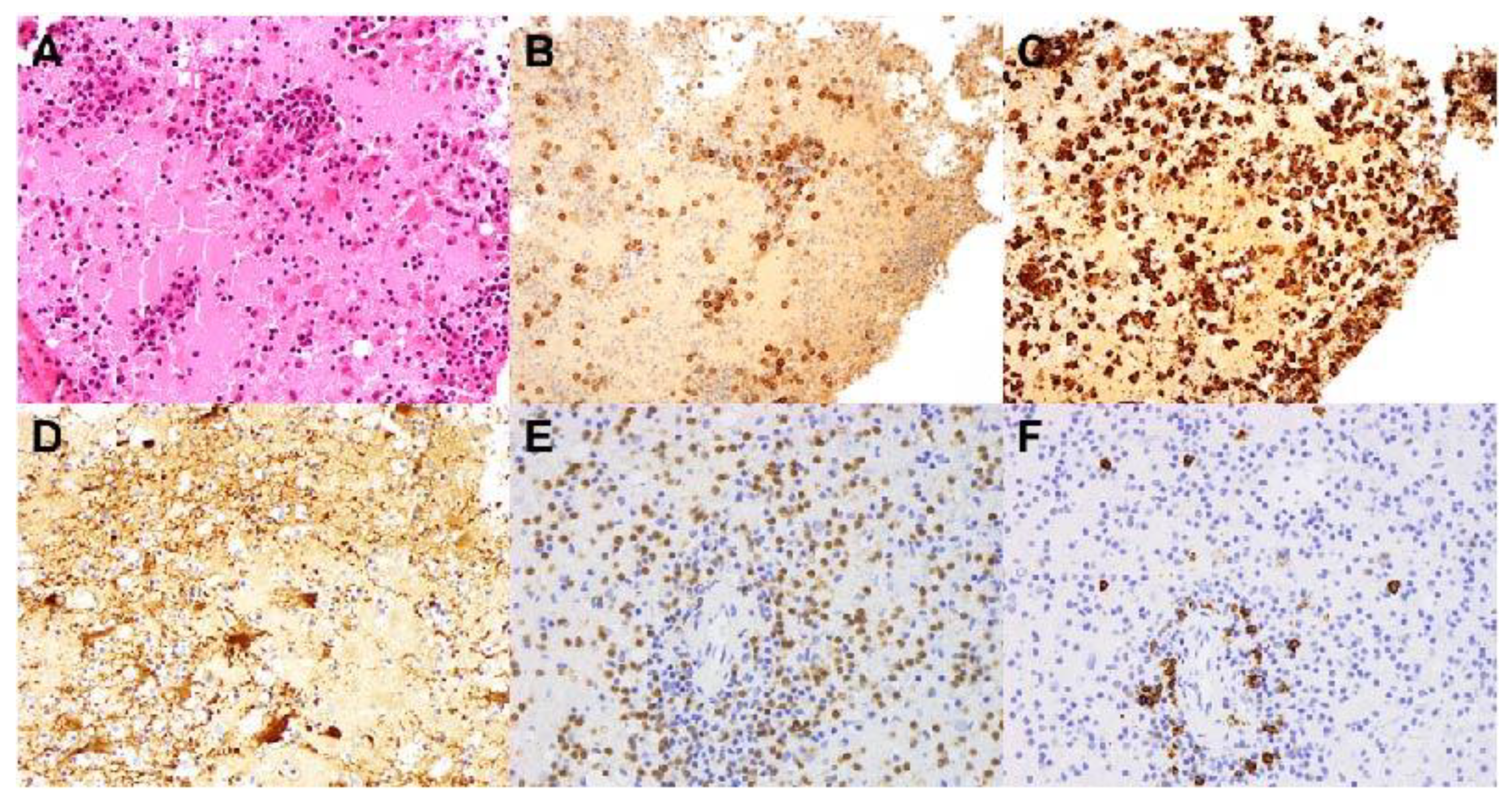
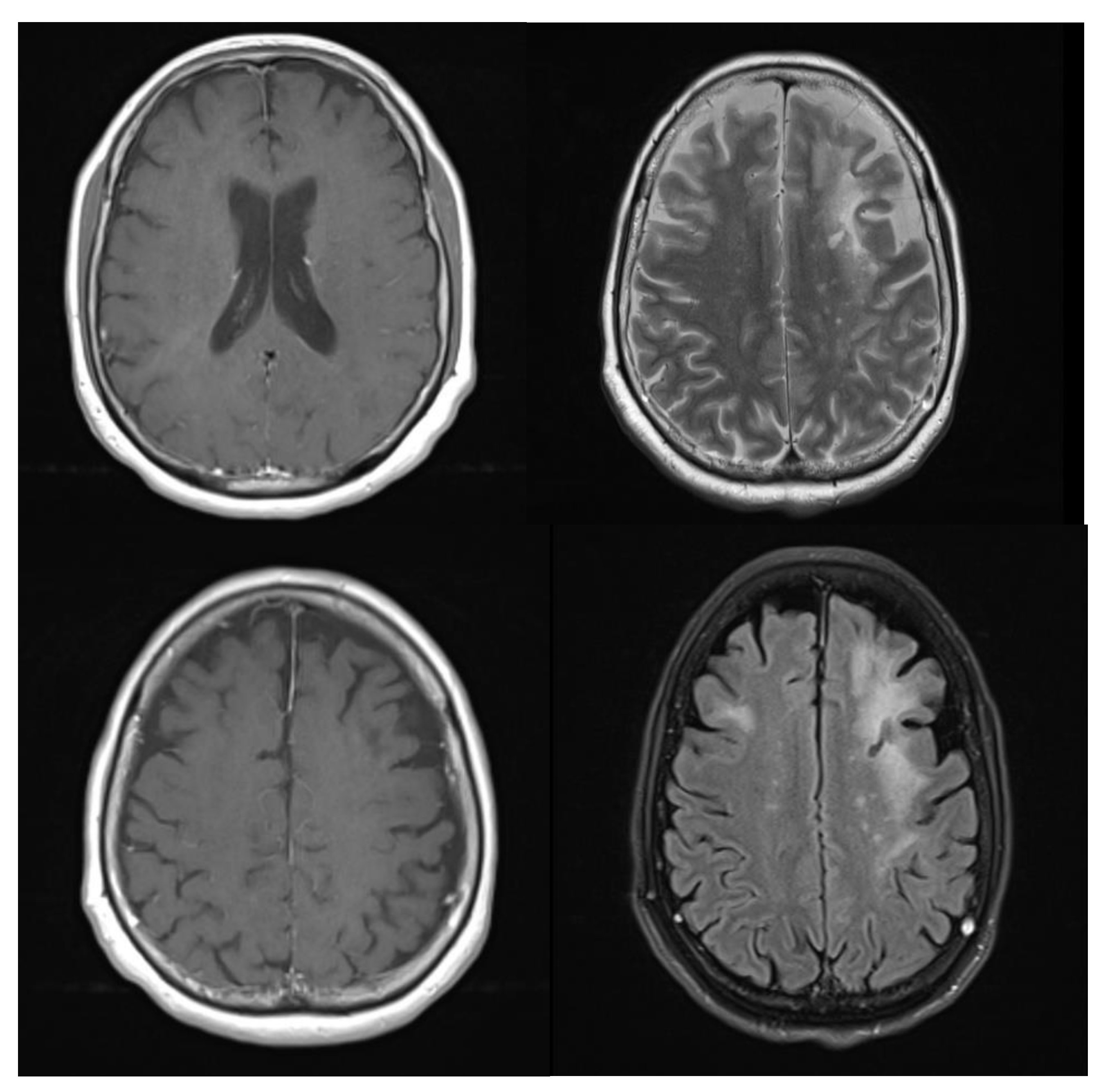
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Halstead, M.R.; Geocadin, R.G. The Medical Management of Cerebral Edema: Past, Present, and Future Therapies. Neurotherapeutics 2019, 16, 1133–1148. [Google Scholar] [CrossRef] [PubMed]
- Jha, R.M.; Kochanek, P.M.; Simard, J.M. Pathophysiology and treatment of cerebral edema in traumatic brain injury. Neuropharmacology 2019, 145, 230–246. [Google Scholar] [CrossRef] [PubMed]
- Nehring, S.M.; Tadi, P.; Tenny, S. Cerebral edema. In StatPearls. Treasure Island (FL); StatPearls Publishing: Pinellas, FL, USA, 2021. [Google Scholar]
- Itaya, S.; Ueda, Y.; Kobayashi, Z.; Tomimitsu, H.; Kobayashi, D.; Shintani, S. Bilateral Frontal Lobe Vasogenic Edema Resulting from Hypertrophic Pachymeningitis due to Granulomatosis with Polyangiitis. Intern. Med. 2017, 56, 3353–3355. [Google Scholar] [CrossRef] [PubMed]
- Nuninga, J.O.; Mandl, R.C.; Froeling, M.; Siero, J.C.; Somers, M.; Boks, M.P.; Nieuwdorp, W.; Heringa, S.; Sommer, I.E. Vasogenic edema versus neuroplasticity as neural correlates of hippocampal volume increase following electroconvulsive therapy. Brain Stimul. 2020, 13, 1080–1086. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, E.P.; Hinson, S.R.; Lennon, V.A.; Fang, B.; Aksamit, A.J.; Morris, P.P.; Basal, E.; Honorat, J.A.; Alfugham, N.B.; Linnoila, J.J.; et al. Glial fibrillary acidic protein immunoglobulin G as biomarker of autoimmune astrocytopathy: Analysis of 102 patients. Ann. Neurol. 2017, 81, 298–309. [Google Scholar] [CrossRef] [PubMed]
- Fang, B.; McKeon, A.; Hinson, S.R.; Kryzer, T.J.; Pittock, S.J.; Aksamit, A.J.; Lennon, V.A. Autoimmune glial fibrillary acidic protein astrocytopathy: A novel meningoencepha-lomyelitis. JAMA Neurol. 2016, 73, 1297–1307. [Google Scholar] [CrossRef] [PubMed]
- Kimura, A.; Takekoshi, A.; Yoshikura, N.; Hayashi, Y.; Shimohata, T. Clinical characteristics of autoimmune GFAP astrocytopathy. J. Neuroimmunol. 2019, 332, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Shan, F.; Long, Y.; Qiu, W. Autoimmune glial fibrillary acidic protein astrocytopathy: A review of the literature. Front. Immunol. 2018, 9, 2802. [Google Scholar] [CrossRef] [PubMed]
- Kunchok, A.; Zekeridou, A.; McKeon, A. Autoimmune glial fibrillary acidic protein astrocytopathy. Curr. Opin. Neurol. 2019, 32, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Long, Y.; Liang, J.; Xu, H.; Huang, Q.; Yang, J.; Gao, C.; Qiu, W.; Lin, S.; Chen, X. Autoimmune glial fibrillary acidic protein astrocytopathy in Chinese patients: A retrospective study. Eur. J. Neurol. 2018, 25, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Di, H.; Yin, Y.; Chen, R.; Zhang, Y.; Ni, J.; Zeng, X. Uncommon manifestations of a rare disease: A case of autoimmune GFAP astrocytopathy. BMC Neurol. 2021, 21, 37. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Chin, J.H.; Fang, B.-Y.; Chen, X.; Zhao, A.-L.; Ren, H.-T.; Guan, H.-Z. Autoimmune glial fibrillary acidic protein astrocytopathy manifesting as subacute meningoencephalitis with descending myelitis: A case report. BMC Neurol. 2020, 20, 443. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goire, N.; Buckland, M.; Cuganesan, R.; Saleem, S.; Lea, V.; Beran, R.G. A Diagnostic Dilemma of White Matter Lesions and Cerebral Oedema without Identifiable Cause—A Neurological Conundrum. Brain Sci. 2021, 11, 1238. https://doi.org/10.3390/brainsci11091238
Goire N, Buckland M, Cuganesan R, Saleem S, Lea V, Beran RG. A Diagnostic Dilemma of White Matter Lesions and Cerebral Oedema without Identifiable Cause—A Neurological Conundrum. Brain Sciences. 2021; 11(9):1238. https://doi.org/10.3390/brainsci11091238
Chicago/Turabian StyleGoire, Namraj, Michael Buckland, Ramesh Cuganesan, Sameer Saleem, Vivienne Lea, and Roy G Beran. 2021. "A Diagnostic Dilemma of White Matter Lesions and Cerebral Oedema without Identifiable Cause—A Neurological Conundrum" Brain Sciences 11, no. 9: 1238. https://doi.org/10.3390/brainsci11091238
APA StyleGoire, N., Buckland, M., Cuganesan, R., Saleem, S., Lea, V., & Beran, R. G. (2021). A Diagnostic Dilemma of White Matter Lesions and Cerebral Oedema without Identifiable Cause—A Neurological Conundrum. Brain Sciences, 11(9), 1238. https://doi.org/10.3390/brainsci11091238





