Informal Caregiving in Amyotrophic Lateral Sclerosis (ALS): A High Caregiver Burden and Drastic Consequences on Caregivers’ Lives
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Recruitment
2.2. Data Collection and Assessment Instruments
2.2.1. Patients’ Functional Status
2.2.2. Disease Severity
2.2.3. Caregivers’ Burden and Duration of Care
2.2.4. Caregivers’ Anxiety and Depression
2.2.5. Caregivers’ Health-Related Quality of Life
2.2.6. Caregivers’ General Impairment in Daily Routine
2.2.7. Caregivers’ Work and Health Impairment, and Their Wishes and Needs
2.3. Statistical Analysis
3. Results
3.1. Study Population
3.1.1. Patients’ Characterization
3.1.2. Caregivers’ Characterization
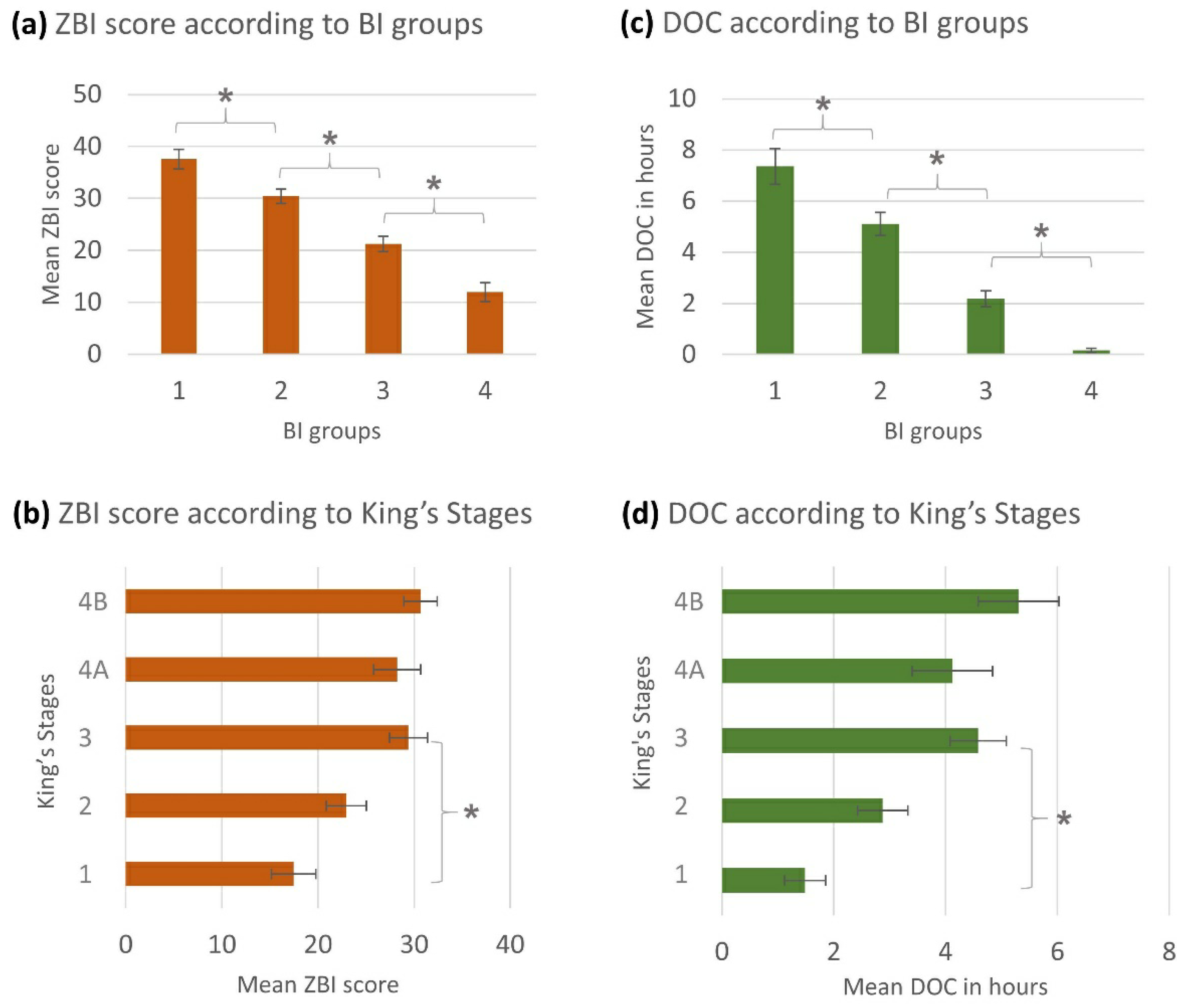
3.2. Caregivers’ General Burden in Relation to Patients’ Functional Status and Disease Severity
3.3. Influencing Factors on Caregiver Burden
3.4. Impact of Caregiving on the Caregivers
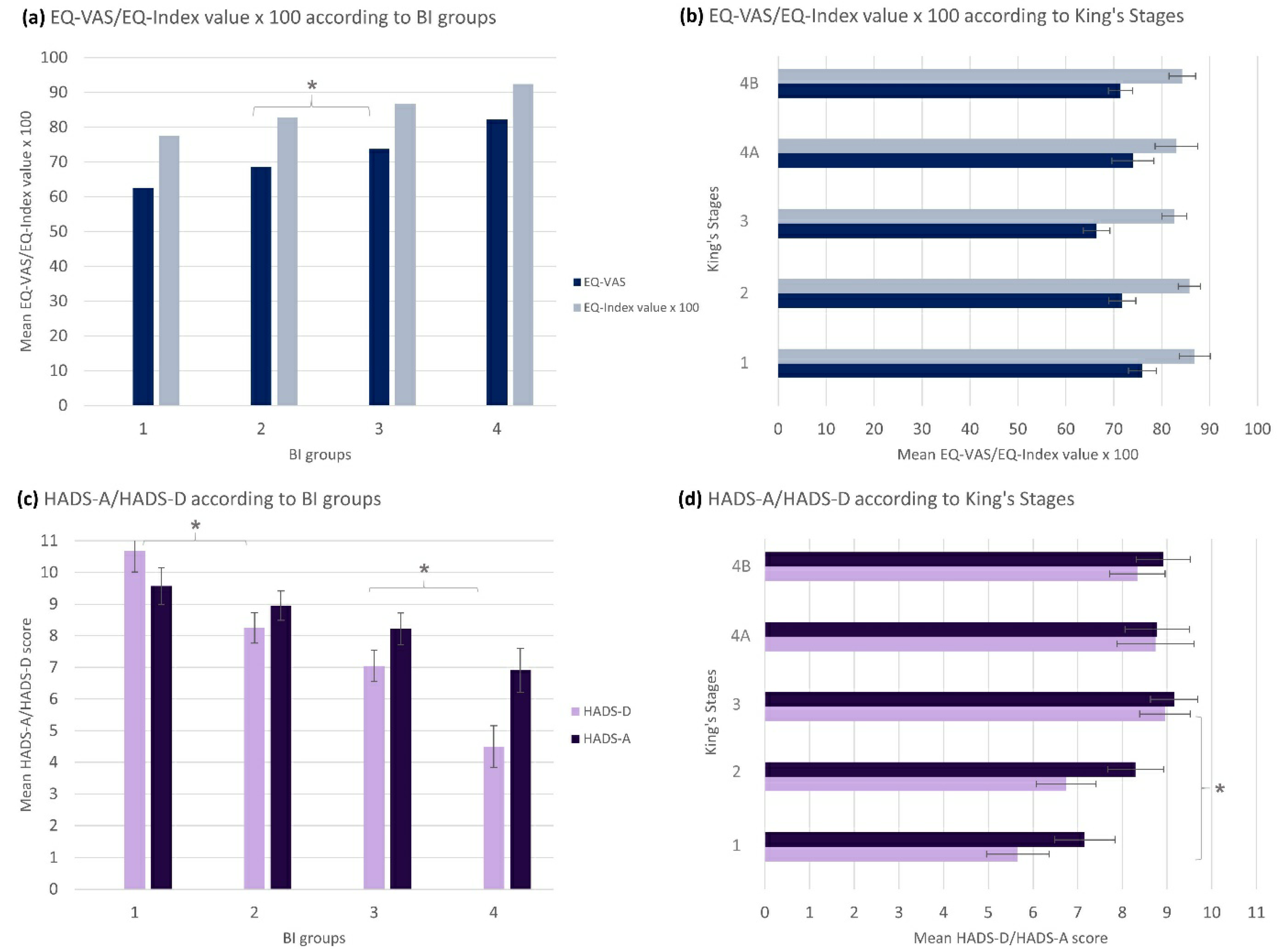
3.4.1. Caregivers’ Health-Related Quality of Life
3.4.2. Caregivers’ Anxiety and Depression
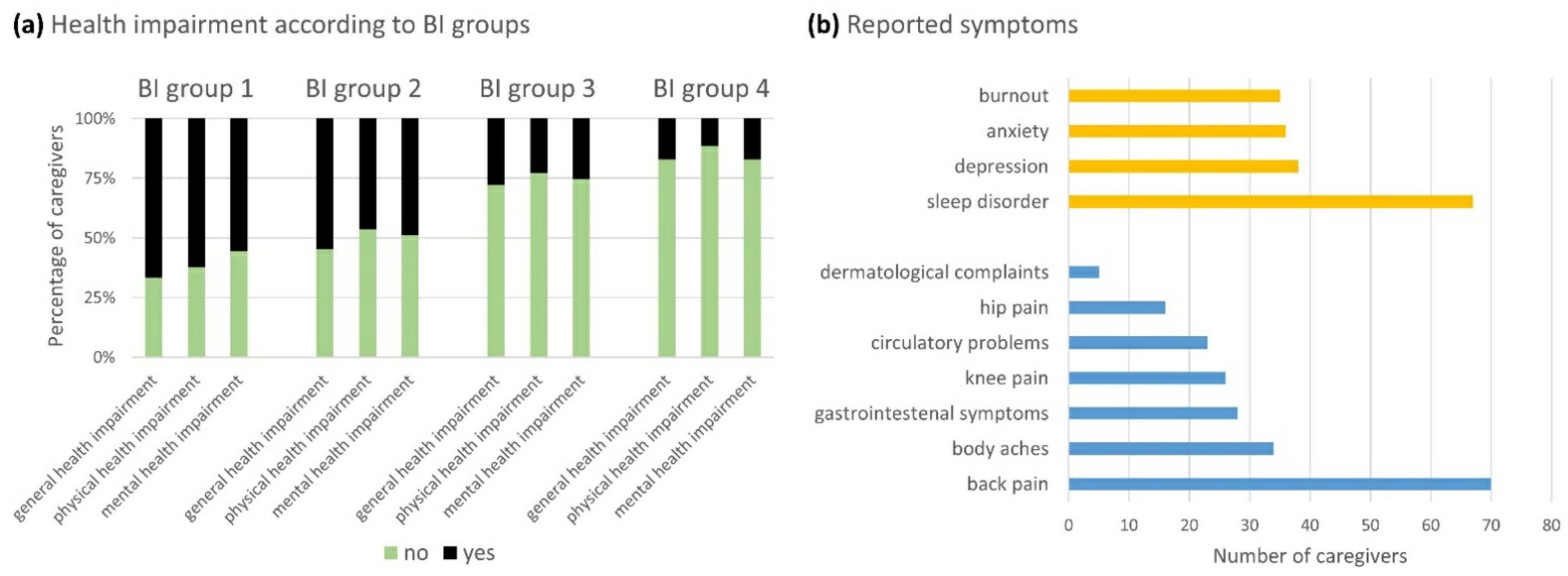
3.4.3. Caregivers’ Health Impairment
3.4.4. Caregivers’ Work Life Impairment
3.5. Effect Comparison between Highly and Lowly Burdened Caregivers
3.6. Gender-Specific Analysis
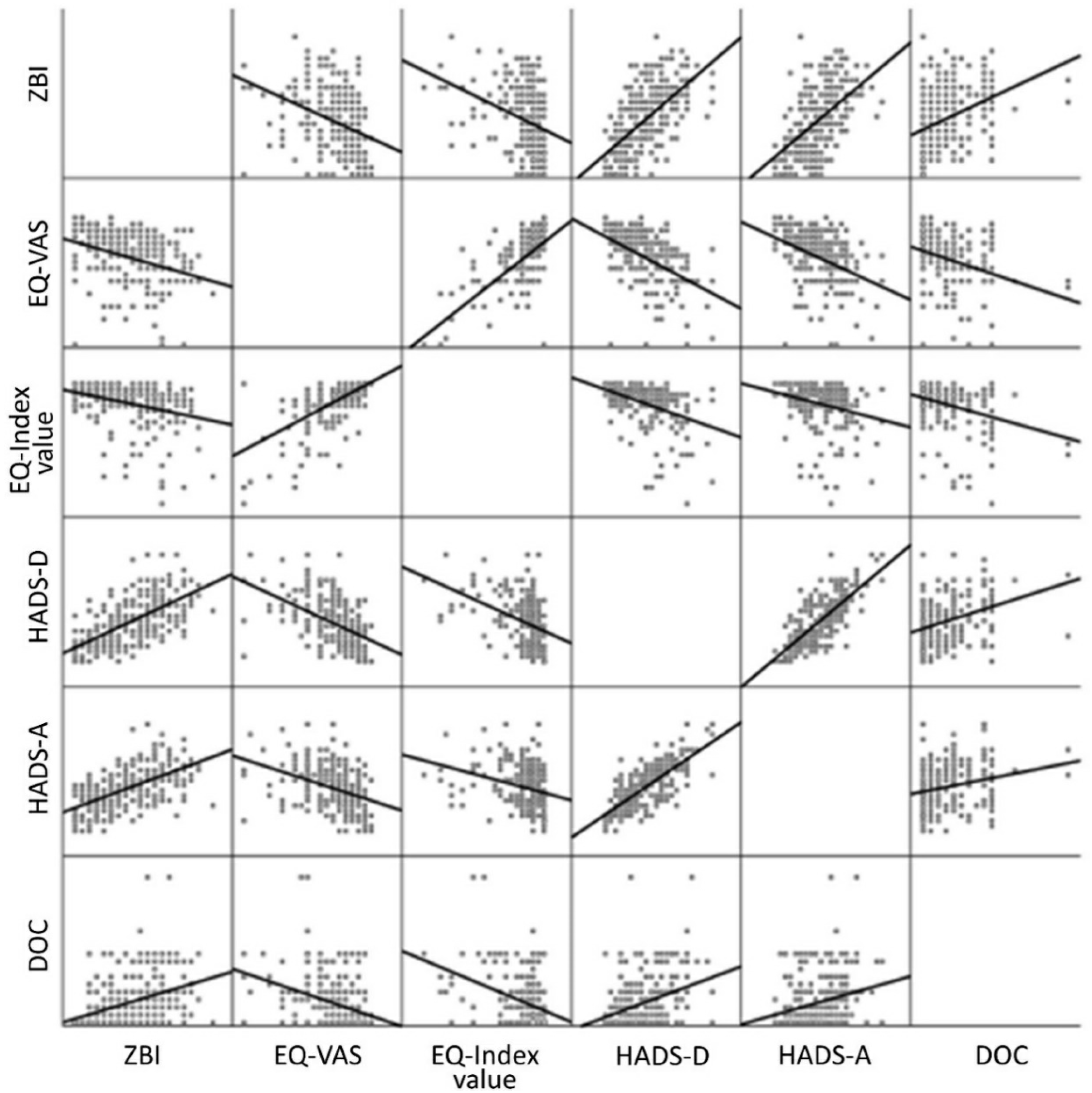
3.7. Correlation of Parameters
3.8. Caregivers’ Wishes and Treatment Satisfaction
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| State | n Included in Study (Percentage) | Total Population of the State, 2019 [in Thousands] (Percentage) [67] | Study Population’s Difference (Percentage Points) |
|---|---|---|---|
| Lower Saxony | 92 (36.9%) | 7994 (9.7%) | +27.2 |
| North Rhine-Westphalia | 62 (24.9%) | 17,947 (21.6%) | +3.3 |
| Bavaria | 46 (18.5%) | 13,125 (15.8%) | +2.7 |
| Saxony | 15 (6.0%) | 4072 (4.9%) | +1.1 |
| Baden-Wuerttemberg | 8 (3.2%) | 11,100 (13.3%) | −10.1 |
| Hesse | 6 (2.4%) | 6288 (7.6%) | −5.2 |
| Schleswig-Holstein | 6 (2.4%) | 2904 (3.5%) | −1.1 |
| Saxony-Anhalt | 5 (2.0%) | 2195 (2.6%) | −0.6 |
| Rhineland-Palatinate | 4 (1.6%) | 4094 (4.9%) | −3.3 |
| Bremen | 2 (0.8%) | 681 (0.8%) | 0 |
| Mecklenburg-Western Pomerania | 1 (0.4%) | 1608 (1.9%) | −1.5 |
| Brandenburg | 1 (0.4%) | 2522 (3.0%) | −2.6 |
| Thuringia | 1 (0.4%) | 2133 (2.6%) | −2.2 |
| Berlin | 0 (0.0%) | 3669 (4.4%) | −4.4 |
| Hamburg | 0 (0.0%) | 1847 (2.2%) | −2.2 |
| Saarland | 0 (0.0%) | 987 (1.2%) | −1.2 |
References
- Zarei, S.; Carr, K.; Reiley, L.; Diaz, K.; Guerra, O.; Altamirano, P.F.; Pagani, W.; Lodin, D.; Orozco, G.; Chinea, A. A comprehensive review of amyotrophic lateral sclerosis. Surg. Neurol. Int. 2015, 6, 171. [Google Scholar] [CrossRef]
- Foster, L.A.; Salajegheh, M.K. Motor Neuron Disease: Pathophysiology, Diagnosis, and Management. Am. J. Med. 2019, 132, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Abe, K.; Itoyama, Y.; Sobue, G.; Tsuji, S.; Aoki, M.; Doyu, M.; Hamada, C.; Kondo, K.; Yoneoka, T.; Akimoto, M.; et al. Confirmatory double-blind, parallel-group, placebo-controlled study of efficacy and safety of edaravone (MCI-186) in amyotrophic lateral sclerosis patients. Amyotroph. Lateral Scler. Front. Degener. 2014, 15, 610–617. [Google Scholar] [CrossRef]
- Miller, R.G.; Mitchell, J.D.; Moore, D.H. Riluzole for amyotrophic lateral sclerosis (ALS)/motor neuron disease (MND). Cochrane Database Syst. Rev. 2012, 2012, CD001447. [Google Scholar] [CrossRef] [PubMed]
- Tramonti, F.; Bonfiglio, L.; Bongioanni, P.; Belviso, C.; Fanciullacci, C.; Rossi, B.; Chisari, C.; Carboncini, M.C. Caregiver burden and family functioning in different neurological diseases. Psychol. Heal. Med. 2018, 24, 27–34. [Google Scholar] [CrossRef]
- Bruletti, G.; Comini, L.; Scalvini, S.; Morini, R.; Luisa, A.; Paneroni, M.; Vitacca, M. A two-year longitudinal study on strain and needs in caregivers of advanced ALS patients. Amyotroph. Lateral Scler. Front. Degener. 2014, 16, 187–195. [Google Scholar] [CrossRef]
- Schönfelder, E.; Osmanovic, A.; Müschen, L.H.; Petri, S.; Schreiber-Katz, O. Costs of illness in amyotrophic lateral sclerosis (ALS): A cross-sectional survey in Germany. Orphanet J. Rare Dis. 2020, 15, 149. [Google Scholar] [CrossRef] [PubMed]
- Stone, N. Amyotrophic Lateral Sclerosis: A Challenge for Constant Adaptation. J. Neurosci. Nurs. 1987, 19, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Thompson, B. Amyotrophic lateral sclerosis: Integrating care for patients and their families. Am. J. Hosp. Palliat. Med. 1990, 7, 29–32. [Google Scholar] [CrossRef]
- Gelinas, D.F.; O’Connor, P.; Miller, R.G. Quality of life for ventilator-dependent ALS patients and their caregivers. J. Neurol. Sci. 1998, 160, S134–S136. [Google Scholar] [CrossRef]
- Krivickas, L.S.; Shockley, L.; Mitsumoto, H. Home care of patients with amyotrophic lateral sclerosis (ALS). J. Neurol. Sci. 1997, 152, s82–s89. [Google Scholar] [CrossRef]
- Moss, A.H.; Casey, P.; Stocking, C.B.; Roos, R.P.; Brooks, B.R.; Siegler, M. Home ventilation for amyotrophic lateral sclerosis patients: Outcomes, costs, and patient, family, and physician attitudes. Neurology 1993, 43, 438. [Google Scholar] [CrossRef]
- Chio, A.; Gauthier, A.; Calvo, A.; Ghiglione, P.; Mutani, R. Caregiver burden and patients’ perception of being a burden in ALS. Neurology 2005, 64, 1780–1782. [Google Scholar] [CrossRef]
- Gauthier, A.; Vignola, A.; Calvo, A.; Cavallo, E.; Moglia, C.; Sellitti, L.; Mutani, R.; Chio, A. A longitudinal study on quality of life and depression in ALS patient–caregiver couples. Neurology 2007, 68, 923–926. [Google Scholar] [CrossRef] [PubMed]
- Vignola, A.; Guzzo, A.; Calvo, A.; Moglia, C.; Pessia, A.; Cavallo, E.; Cammarosano, S.; Giacone, S.; Ghiglione, P.; Chiò, A. Anxiety undermines quality of life in ALS patients and caregivers. Eur. J. Neurol. 2008, 15, 1231–1236. [Google Scholar] [CrossRef]
- Pinho, A.C.; Gonçalves, E. Are Amyotrophic Lateral Sclerosis Caregivers at Higher Risk for Health Problems? Acta Médica Port. 2016, 29, 56–62. [Google Scholar] [CrossRef] [PubMed][Green Version]
- De Wit, J.; Bakker, L.A.; Van Groenestijn, A.C.; van den Berg, L.H.; Schröder, C.D.; Visser-Meily, J.M.; Beelen, A. Caregiver burden in amyotrophic lateral sclerosis: A systematic review. Palliat. Med. 2018, 32, 231–245. [Google Scholar] [CrossRef] [PubMed]
- Majmudar, S.; Wu, J.; Paganoni, S. Rehabilitation in amyotrophic lateral sclerosis: Why it matters. Muscle Nerve 2014, 50, 4–13. [Google Scholar] [CrossRef] [PubMed]
- Antoniadi, A.M.; Galvin, M.; Heverin, M.; Hardiman, O.; Mooney, C. Prediction of caregiver burden in amyotrophic lateral sclerosis: A machine learning approach using random forests applied to a cohort study. BMJ Open 2020, 10, e033109. [Google Scholar] [CrossRef]
- Galvin, M.; Carney, S.; Corr, B.; Mays, I.; Pender, N.; Hardiman, O. Needs of informal caregivers across the caregiving course in amyotrophic lateral sclerosis: A qualitative analysis. BMJ Open 2018, 8, e018721. [Google Scholar] [CrossRef]
- Reichert, M.; Hampel, S.; Reuter, V.; Reichert, M. Mobile Demenzberatung als niedrigschwelliges Hilfeangebot für pflegende Angehörige. Z. Für Gerontol. Und Geriatr. 2016, 49, 181–186. [Google Scholar] [CrossRef]
- Reckrey, J.M.; Boerner, K.; Franzosa, E.; Bollens-Lund, E.; Ornstein, K.A. Paid Caregivers in the Community-Based Dementia Care Team: Do Family Caregivers Benefit? Clin Ther. 2021. [Google Scholar] [CrossRef]
- De Wit, J.; Beelen, A.; Drossaert, C.H.C.; Kolijn, R.; Berg, L.H.V.D.; Schröder, C.D.; Visser-Meily, J.M.A. Blended psychosocial support for partners of patients with ALS and PMA: Results of a randomized controlled trial. Amyotroph. Lateral Scler. Front. Degener. 2020, 21, 344–354. [Google Scholar] [CrossRef]
- Navarta-Sánchez, M.V.; Ambrosio, L.; Portillo, M.C.; Ursúa, M.E.; Senosiain, J.M.; Riverol, M. Evaluation of a psychoeducational intervention compared with education in people with Parkinson’s disease and their informal caregivers: A quasi-experimental study. J. Adv. Nurs. 2020, 76, 2719–2732. [Google Scholar] [CrossRef]
- Sun, K.-T.; Hsieh, K.-L.; Syu, S.-R. Towards an Accessible Use of a Brain-Computer Interfaces-Based Home Care System through a Smartphone. Comput. Intell. Neurosci. 2020, 2020, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Galvin, M.; Corr, B.; Madden, C.; Mays, I.; McQuillan, R.; Timonen, V.; Staines, A.; Hardiman, O. Caregiving in ALS—A mixed methods approach to the study of Burden. BMC Palliat. Care 2016, 15, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Burke, T.; Hardiman, O.; Pinto-Grau, M.; Lonergan, K.; Heverin, M.; Tobin, K.; Staines, A.; Galvin, M.; Pender, N. Longitudinal predictors of caregiver burden in amyotrophic lateral sclerosis: A population-based cohort of patient–caregiver dyads. J. Neurol. 2018, 265, 793–808. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.-H.; Kim, M.S. Ventilator Use, Respiratory Problems, and Caregiver Well-Being in Korean Patients With Amyotrophic Lateral Sclerosis Receiving Home-Based Care. J. Neurosci. Nurs. 2014, 46, E25–E32. [Google Scholar] [CrossRef] [PubMed]
- Kaub-Wittemer, D.; Von Steinbüchel, N.; Wasner, M.; Laier-Groeneveld, G.; Borasio, G.D. Quality of life and psychosocial issues in ventilated patients with amyotrophic lateral sclerosis and their caregivers. J. Pain Symptom Manag. 2003, 26, 890–896. [Google Scholar] [CrossRef]
- Pagnini, F.; Phillips, D.; Bosma, C.M.; Reece, A.; Langer, E. Mindfulness as a Protective Factor for the Burden of Caregivers of Amyotrophic Lateral Sclerosis Patients. J. Clin. Psychol. 2015, 72, 101–111. [Google Scholar] [CrossRef]
- Lillo, P.; Mioshi, E.; Hodges, J.R. Caregiver burden in amyotrophic lateral sclerosis is more dependent on patients’ behavioral changes than physical disability: A comparative study. BMC Neurol. 2012, 12, 156. [Google Scholar] [CrossRef]
- Creemers, H.; De Morée, S.; Veldink, J.H.; Nollet, F.; Berg, L.H.V.D.; Beelen, A. Factors related to caregiver strain in ALS: A longitudinal study. J. Neurol. Neurosurg. Psychiatry 2015, 87, 775–781. [Google Scholar] [CrossRef] [PubMed]
- Burke, T.; Galvin, M.; Pinto-Grau, M.; Lonergan, K.; Madden, C.; Mays, I.; Carney, S.; Hardiman, O.; Pender, N. Caregivers of patients with amyotrophic lateral sclerosis: Investigating quality of life, caregiver burden, service engagement, and patient survival. J. Neurol. 2017, 264, 898–904. [Google Scholar] [CrossRef] [PubMed]
- Sandstedt, P.; Littorin, S.; Widsell, G.C.; Johansson, S.; Gottberg, K.; Ytterberg, C.; Olsson, M.; Holmqvist, L.W.; Kierkegaard, M. Caregiver experience, health-related quality of life and life satisfaction among informal caregivers to patients with amyotrophic lateral sclerosis: A cross-sectional study. J. Clin. Nurs. 2018, 27, 4321–4330. [Google Scholar] [CrossRef]
- Burke, T.; Elamin, M.; Galvin, M.; Hardiman, O.; Pender, N. Caregiver burden in amyotrophic lateral sclerosis: A cross-sectional investigation of predictors. J. Neurol. 2015, 262, 1526–1532. [Google Scholar] [CrossRef] [PubMed]
- Tramonti, F.; Bongioanni, P.; Leotta, R.; Puppi, I.; Rossi, B. Age, gender, kinship and caregiver burden in amyotrophic lateral sclerosis. Psychol. Health Med. 2014, 20, 41–46. [Google Scholar] [CrossRef]
- Qutub, K.; Lacomis, D.; Albert, S.M.; Feingold, E. Life factors affecting depression and burden in amyotrophic lateral sclerosis caregivers. Amyotroph. Lateral Scler. Front. Degener. 2014, 15, 292–297. [Google Scholar] [CrossRef] [PubMed]
- Roach, A.R.; Averill, A.J.; Segerstrom, S.C.; Kasarskis, E.J. The Dynamics of Quality of Life in ALS Patients and Caregivers. Ann. Behav. Med. 2009, 37, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Peseschkian, T.; Cordts, I.; Günther, R.; Stolte, B.; Zeller, D.; Schröter, C.; Weyen, U.; Regensburger, M.; Wolf, J.; Schneider, I.; et al. A Nation-Wide, Multi-Center Study on the Quality of Life of ALS Patients in Germany. Brain Sci. 2021, 11, 372. [Google Scholar] [CrossRef]
- Ludolph, A.C.; Drory, V.E.; Hardiman, O.; Nakano, I.; Ravits, J.; Robberecht, W.; Shefner, J.M.; The WFN Research Group On ALS/MND. A revision of the El Escorial criteria. Amyotroph. Lateral Scler. Front. Degener. 2015, 16, 291–292. [Google Scholar] [CrossRef]
- Müller, K.; Brenner, D.; Weydt, P.; Meyer, T.; Grehl, T.; Petri, S.; Grosskreutz, J.; Schuster, J.; Volk, A.E.; Borck, G.; et al. Comprehensive analysis of the mutation spectrum in 301 German ALS families. J. Neurol. Neurosurg. Psychiatry 2018, 89, 817–827. [Google Scholar] [CrossRef]
- German Network for Motor Neuron Diseases (MND-NET). MND Net, German Network for Motor Neuron Diseases. Available online: http://www.mnd-als.de/html/home?set-language-to=en (accessed on 5 April 2021).
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Prev. Med. 2007, 45, 247–251. [Google Scholar] [CrossRef]
- Klug, C.; Schreiber-Katz, O.; Thiele, S.; Schorling, E.; Zowe, J.; Reilich, P.; Walter, M.C.; Nagels, K.H. Disease burden of spinal muscular atrophy in Germany. Orphanet J. Rare Dis. 2016, 11, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Schreiber-Katz, O.; Klug, C.; Thiele, S.; Schorling, E.; Zowe, J.; Reilich, P.; Nagels, K.H.; Walter, M.C. Comparative cost of illness analysis and assessment of health care burden of Duchenne and Becker muscular dystrophies in Germany. Orphanet J. Rare Dis. 2014, 9, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, F.I.; Barthel, D.W. Functional Evaluation: The Barthel Index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar] [PubMed]
- Collin, C.; Wade, D.T.; Davies, S.; Horne, V. The Barthel ADL Index: A reliability study. Int. Disabil. Stud. 1988, 10, 61–63. [Google Scholar] [CrossRef] [PubMed]
- De Groot, I.J.M.; Post, M.W.M.; Van Heuveln, T.; Berg, L.H.V.D.; Lindeman, E. Measurement of decline of functioning in persons with amyotrophic lateral sclerosis: Responsiveness and possible applications of the Functional Independence Measure, Barthel Index, Rehabilitation Activities Profile and Frenchay Activities Index. Amyotroph. Lateral Scler. 2006, 7, 167–172. [Google Scholar] [CrossRef]
- Ishida, N.; Hongo, S.; Kumano, A.; Hatta, H.; Zakoji, N.; Hirutani, M.; Yamamoto, Y.; Aono, H.; Tuigi, M.; Suzuki, R.; et al. Relationship between Pain and Functional Status in Patients with Amyotrophic Lateral Sclerosis: A Multicenter Cross-Sectional Study. J. Palliat. Med. 2018, 21, 588–591. [Google Scholar] [CrossRef]
- Shah, S.; Vanclay, F.; Cooper, B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J. Clin. Epidemiol. 1989, 42, 703–709. [Google Scholar] [CrossRef]
- Leigh, P.N.; Swash, M.; Iwasaki, Y.; Ludolph, A.; Meininger, V.; Miller, R.G.; Mitsumoto, H.; Shaw, P.; Tashiro, K.; Berg, L.V.D. Amyotrophic lateral sclerosis: A consensus viewpoint on designing and implementing a clinical trial. Amyotroph. Lateral Scler. 2004, 5, 84–98. [Google Scholar] [CrossRef]
- Balendra, R.; Jones, A.; Jivraj, N.; Knights, C.; Ellis, C.M.; Burman, R.; Turner, M.; Leigh, P.N.; Shaw, C.; Al-Chalabi, A. Estimating clinical stage of amyotrophic lateral sclerosis from the ALS Functional Rating Scale. Amyotroph. Lateral Scler. Front. Degener. 2014, 15, 279–284. [Google Scholar] [CrossRef] [PubMed]
- Cedarbaum, J.M.; Stambler, N.; Malta, E.; Fuller, C.; Hilt, D.; Thurmond, B.; Nakanishi, A. The ALSFRS-R: A revised ALS functional rating scale that incorporates assessments of respiratory function. J. Neurol. Sci. 1999, 169, 13–21. [Google Scholar] [CrossRef]
- Roche, J.C.; Rojas-Garcia, R.; Scott, K.M.; Scotton, W.; Ellis, C.E.; Burman, R.; Wijesekera, L.; Turner, M.; Leigh, P.N.; Shaw, C.; et al. A proposed staging system for amyotrophic lateral sclerosis. Brain 2012, 135, 847–852. [Google Scholar] [CrossRef] [PubMed]
- Zarit, S.H.; Reever, M.K.E.; Bach-Peterson, M.J. Relatives of the Impaired Elderly: Correlates of Feelings of Burden. Gerontologist 1980, 20, 649–655. [Google Scholar] [CrossRef]
- Macchi, Z.A.; Koljack, C.E.; Miyasaki, J.M.; Katz, M.; Galifianakis, N.; Prizer, L.P.; Sillau, S.H.; Kluger, B.M. Patient and caregiver characteristics associated with caregiver burden in Parkinson’s disease: A palliative care approach. Ann. Palliat. Med. 2020, 9, S24–S33. [Google Scholar] [CrossRef]
- Braun, M.; Scholz, U.; Hornung, R.; Martin, M. Die subjektive Belastung pflegender Ehepartner von Demenzkranken. Z. Für Gerontol. Und Geriatr. 2010, 43, 111–119. [Google Scholar] [CrossRef]
- Andrieu, S.; Grand, A.; Henrard, J.C. Beyond the global score of the Zarit Burden Interview: Useful dimensions for clinicians. Int. J. Geriatr. Psychiatry 2005, 20, 254–260. [Google Scholar] [CrossRef]
- Schreiner, A.S.; Morimoto, T.; Arai, Y.; Zarit, S. Assessing family caregiver’s mental health using a statistically derived cut-off score for the Zarit Burden Interview. Aging Ment. Heal. 2006, 10, 107–111. [Google Scholar] [CrossRef]
- Bjelland, I.; Dahl, A.A.; Haug, T.T.; Neckelmann, D. The validity of the Hospital Anxiety and Depression Scale. J. Psychosom. Res. 2002, 52, 69–77. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef]
- Nolte, S.; Rose, M. Die Erfassung gesundheitsbezogener Lebensqualität bei Erwachsenen. Das Gesundh. 2013, 75, 166–175. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.-S.; Kohlmann, T.; Janssen, M.F.; Buchholz, I. Psychometric properties of the EQ-5D-5L: A systematic review of the literature. Qual. Life Res. 2021, 30, 647–673. [Google Scholar] [CrossRef] [PubMed]
- Van Hout, B.; Janssen, M.; Feng, Y.-S.; Kohlmann, T.; Busschbach, J.; Golicki, D.; Lloyd, A.; Scalone, L.; Kind, P.; Pickard, A.S. Interim Scoring for the EQ-5D-5L: Mapping the EQ-5D-5L to EQ-5D-3L Value Sets. Value Heal. 2012, 15, 708–715. [Google Scholar] [CrossRef]
- Rosenbohm, A.; The ALS Registry Study Group; Peter, R.S.; Erhardt, S.; Lulé, D.; Rothenbacher, D.; Ludolph, A.C.; Nagel, G. Epidemiology of amyotrophic lateral sclerosis in Southern Germany. J. Neurol. 2017, 264, 749–757. [Google Scholar] [CrossRef]
- Statista. Population in Germany as of December 2019, by Federal State. Available online: https://www.statista.com/statistics/1127686/population-by-federal-state-germany/ (accessed on 24 May 2021).
- Manjaly, Z.R.; Scott, K.M.; Abhinav, K.; Wijesekera, L.; Ganesalingam, J.; Goldstein, L.; Janssen, A.; Dougherty, A.; Willey, E.; Stanton, B.R.; et al. The sex ratio in amyotrophic lateral sclerosis: A population based study. Amyotroph. Lateral Scler. 2010, 11, 439–442. [Google Scholar] [CrossRef] [PubMed]
- Sandstedt, P.; Johansson, S.; Ytterberg, C.; Ingre, C.; Holmqvist, L.W.; Kierkegaard, M. Predictors of health-related quality of life in people with amyotrophic lateral sclerosis. J. Neurol. Sci. 2016, 370, 269–273. [Google Scholar] [CrossRef] [PubMed]
- Wijesekera, L.L.; Leigh, P.N. Amyotrophic lateral sclerosis. Orphanet J. Rare Dis. 2009, 4, 3–22. [Google Scholar] [CrossRef]
- Ludwig, K.; Von Der Schulenburg, J.-M.G.; Greiner, W. German Value Set for the EQ-5D-5L. PharmacoEconomics 2018, 36, 663–674. [Google Scholar] [CrossRef]
- Grochtdreis, T.; Dams, J.; König, H.-H.; Konnopka, A. Health-related quality of life measured with the EQ-5D-5L: Estimation of normative index values based on a representative German population sample and value set. Eur. J. Health Econ. 2019, 20, 933–944. [Google Scholar] [CrossRef]
- Landfeldt, E.; Lindgren, P.; Bell, C.F.; Guglieri, M.; Straub, V.; Lochmüller, H.; Bushby, K. Quantifying the burden of caregiving in Duchenne muscular dystrophy. J. Neurol. 2016, 263, 906–915. [Google Scholar] [CrossRef]
- Aranda-Reneo, I.; Peña-Longobardo, L.M.; Oliva-Moreno, J.; Litzkendorf, S.; Durand-Zaleski, I.; Tizzano, E.F.; López-Bastida, J. The Burden of Spinal Muscular Atrophy on Informal Caregivers. Int. J. Environ. Res. Public Health 2020, 17, 8989. [Google Scholar] [CrossRef]
- Pagnini, F.; Rossi, G.; Lunetta, C.; Banfi, P.; Castelnuovo, G.; Corbo, M.; Molinari, E. Burden, depression, and anxiety in caregivers of people with amyotrophic lateral sclerosis. Psychol. Health Med. 2010, 15, 685–693. [Google Scholar] [CrossRef] [PubMed]
- Chiò, A.; Vignola, A.; Mastro, E.; Giudici, A.D.; Iazzolino, B.; Calvo, A.; Moglia, C.; Montuschi, A. Neurobehavioral symptoms in ALS are negatively related to caregivers’ burden and quality of life. Eur. J. Neurol. 2010, 17, 1298–1303. [Google Scholar] [CrossRef] [PubMed]
- Caga, J.; Hsieh, S.; Highton-Williamson, E.; Zoing, M.C.; Ramsey, E.; Devenney, E.; Ahmed, R.M.; Hogden, A.; Kiernan, M.C. The burden of apathy for caregivers of patients with amyotrophic lateral sclerosis. Amyotroph. Lateral Scler. Front. Degener. 2018, 19, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Pagnini, F.; Lunetta, C.; Rossi, G.; Banfi, P.; Gorni, K.; Cellotto, N.; Castelnuovo, G.; Molinari, E.; Corbo, M. Existential well-being and spirituality of individuals with amyotrophic lateral sclerosis is related to psychological well-being of their caregivers. Amyotroph. Lateral Scler. 2010, 12, 105–108. [Google Scholar] [CrossRef] [PubMed]
- Klietz, M.; Drexel, S.C.C.; Schnur, T.; Lange, F.; Groh, A.; Paracka, L.; Greten, S.; Dressler, D.; Höglinger, G.U.U.; Wegner, F. Mindfulness and Psychological Flexibility are Inversely Associated with Caregiver Burden in Parkinson’s Disease. Brain Sci. 2020, 10, 111. [Google Scholar] [CrossRef]
- Roth, D.L.; Fredman, L.; Haley, W.E. Informal Caregiving and Its Impact on Health: A Reappraisal From Population-Based Studies. Gerontologist 2015, 55, 309–319. [Google Scholar] [CrossRef] [PubMed]
- Bartolomei, L.; Pastore, A.; Meligrana, L.; Sanson, E.; Bonetto, N.; Minicuci, G.M.; Marsala, S.Z.; Mesiano, T.; Bragagnolo, L.; Antonini, A. Relevance of sleep quality on caregiver burden in Parkinson’s disease. Neurol. Sci. 2018, 39, 835–839. [Google Scholar] [CrossRef]
- Whynes, D.K. Correspondence between EQ-5D health state classifications and EQ VAS scores. Health Qual. Life Outcomes 2008, 6, 94. [Google Scholar] [CrossRef]
- Lulé, D.; Kübler, A.; Ludolph, A.C. Ethical Principles in Patient-Centered Medical Care to Support Quality of Life in Amyotrophic Lateral Sclerosis. Front. Neurol. 2019, 10, 259. [Google Scholar] [CrossRef]
- Zesiewicz, T.A. Parkinson Disease. Contin. Lifelong Learn. Neurol. 2019, 25, 896–918. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.; Guo, X.; Zheng, Z.; Wei, Q.; Song, W.; Cao, B.; Huang, R.; Yang, R.; Shang, H. Depression and anxiety in amyotrophic lateral sclerosis: Correlations between the distress of patients and caregivers. Muscle Nerve 2015, 51, 353–357. [Google Scholar] [CrossRef]
- Sebring, K.; Shattuck, J.; Berk, J.; Boersma, I.; Sillau, S.; Kluger, B.M. Assessing the validity of proxy caregiver reporting for potential palliative care outcome measures in Parkinson’s disease. Palliat. Med. 2018, 32, 1522–1528. [Google Scholar] [CrossRef]
- Linse, K.; Rüger, W.; Joos, M.; Schmitz-Peiffer, H.; Storch, A.; Hermann, A. Eye-tracking-based assessment suggests preserved well-being in locked-in patients. Ann. Neurol. 2017, 81, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Hack, T.F.; McClement, S.E.; Chochinov, H.M.; Dufault, B.; Johnston, W.; Enns, M.W.; Thompson, G.N.; Harlos, M.; Damant, R.W.; Ramsey, C.D.; et al. Assessing Symptoms, Concerns, and Quality of Life in Noncancer Patients at End of Life: How Concordant Are Patients and Family Proxy Members? J. Pain Symptom Manag. 2018, 56, 760–766. [Google Scholar] [CrossRef]
- Lazzari, C. Ecological Momentary Assessments and Interventions in Alzheimer’s Caregiving. Curr. Alzheimer Res. 2018, 15, 1027–1031. [Google Scholar] [CrossRef]
- Hotter, B.; Padberg, I.; Liebenau, A.; Knispel, P.; Heel, S.; Steube, D.; Wissel, J.; Wellwood, I.; Meisel, A. Identifying unmet needs in long-term stroke care using in-depth assessment and the Post-Stroke Checklist—The Managing Aftercare for Stroke (MAS-I) study. Eur. Stroke J. 2018, 3, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Elmståhl, S.; Dahlrup, B.; Ekström, H.; Nordell, E. The association between medical diagnosis and caregiver burden: A cross-sectional study of recipients of informal support and caregivers from the general population study ‘Good Aging in Skåne’, Sweden. Aging Clin. Exp. Res. 2018, 30, 1023–1032. [Google Scholar] [CrossRef] [PubMed]


| Patients’ Characterization (n = All, n = Men, n = Women); Score’s Range | All Absolute Number, Percent or Median (IQR)/Mean (SD) | Men Absolute Number, Percent or Median (IQR)/Mean (SD) | Women Absolute Number, Percent or Median (IQR)/Mean (SD) |
|---|---|---|---|
| Number * | 249, 100 | 157, 64.1 | 88, 35.9 |
| Age, years (n = 245, n = 157, n = 88) | 65 (16)/64.19 (11.67) | 64 (16)/63.59 (12.25) | 65.5 (15.25)/65.27 (10.53) |
| Marital status (n = 243, n = 156, n = 87) | |||
| • Single | 9, 3.7 | 5, 3.2 | 4, 4.6 |
| • Living in a partnership | 15, 6.2 | 9, 5.8 | 6, 6.9 |
| • Married | 202, 83.1 | 139, 89.1 | 63, 72.4 |
| • Divorced | 11, 4.5 | 3, 1.9 | 8, 9.2 |
| • Widowed | 6, 2.5 | 0, 0.0 | 6, 6.9 |
| Housing situation (n = 233, n = 151, n = 82) | |||
| • With the family/partner | 212, 91.0 | 142, 94.0 | 70, 85.4 |
| • Alone | 16, 6.9 | 5, 3.3 | 11, 13.4 |
| • Assisted living | 2, 0.9 | 2, 1.3 | 0, 0.0 |
| • Nursing home | 3, 1.3 | 2, 1.3 | 1, 1.2 |
| Employment (n = 222, n = 143, n = 79) | |||
| • Working | 31, 14.0 | 34, 23.8 | 26, 32.9 |
| • Employment no longer possible due to ALS | 60, 27.0 | 25, 17.5 | 6, 7.6 |
| • Retired due to age, unemployed, homemaker | 131, 59.0 | 84, 58.7 | 47, 59.5 |
| Use of wheelchair (n = 249, n = 157, n = 88) | 120, 48.2 | 69, 43.9 | 49, 55.7 |
| Use of home ventilator support (n = 249, n = 157, n = 88) | 53, 21.3 | 37, 23.6 | 16, 18.2 |
| Use of PEG (n = 249, n = 157, n = 88) | 38, 15.3 | 19, 12.1 | 18, 20.5 |
| Permanent supervision necessary (n = 221, n = 143, n = 78) | 92, 41.6 | 46, 32.2 | 46, 59.0 |
| BI score (n = 249, n = 157, n = 88); 0–100 | 60 (60)/58.63 (31.23) | 65 (60)/62.58 (30.79) | 45 (58.75)/50.97 (31.26) |
| BI groups (n = 249, n = 157, n = 88) | |||
| • 1 (0–20) | 45, 18.1 | 23, 14.6 | 22, 25.0 |
| • 2 (21–60) | 86, 34.5 | 51, 32.5 | 34, 38.6 |
| • 3 (61–99) | 83, 33.3 | 55, 35.0 | 25, 28.4 |
| • 4 (100) | 35, 14.1 | 28, 17.8 | 7, 8.0 |
| ALSFRS-R score (n = 244, n = 157, n = 87); 0–48 | 32.5 (13.75)/31.39 (9.52) | 34 (16)/32.38 (9.50) | 30 (13)/29.61 (9.33) |
| King’s Stages (n = 244, n = 157, n = 87) | |||
| • 1 | 39, 16.0 | 31, 19.7 | 8, 9.2 |
| • 2 | 53, 21.7 | 35, 22.3 | 18, 20.7 |
| • 3 | 66, 27.0 | 36, 22.9 | 30, 34.5 |
| • 4A | 29, 11.9 | 15, 9.6 | 14, 16.1 |
| • 4B | 57, 23.4 | 40, 25.5 | 17, 19.5 |
| Caregivers’ Characterization (n = All, n = Men/Male CGs, n = Women/Female CGs); Score’s Range | All Absolute Number, Percent or Median (IQR)/Mean (SD) | Male CGs Absolute Number, Percent or Median (IQR)/Mean (SD) | Female CGs Absolute Number, Percent or Median (IQR)/Mean (SD) |
|---|---|---|---|
| Number * | 249, 100.0 | 75, 30.1 | 174, 69.9 |
| Age, years (n = 248, n = 75, n = 173) | 61(16.75)/59.84 (13.77) | 65 (16)/64.23 (13.47) | 60 (16)/57.94 (13.52) |
| Marital status (n = 249, n = 75, n = 174) | |||
| • Single | 9, 3.6 | 5, 6.7 | 4, 2.3 |
| • Living in a partnership | 23, 9.2 | 10, 13.3 | 13, 7.5 |
| • Married | 214, 86.0 | 60, 80.0 | 154, 88.5 |
| • Divorced | 2, 0.8 | 0, 0.0 | 2, 1.1 |
| • Widowed | 1, 0.4 | 0, 0.0 | 1, 0.6 |
| Relation to the patient (n = 249, n = 75, n = 174) | |||
| • Spouse | 207, 83.1 | 67, 89.3 | 140, 80.5 |
| • Parent | 17, 6.8 | 5, 6.7 | 12, 6.9 |
| • Sibling | 8, 3.2 | 0, 0.0 | 8, 4.6 |
| • Child | 15, 6.0 | 3, 4.0 | 12, 6.9 |
| • Friend | 2, 0.8 | 0, 0.0 | 2, 1.1 |
| Employment (n = 249, n = 75, n = 174) | |||
| • Working | 110, 44.2 | 25, 33.3 | 85, 48.9 |
| • Employment no longer possible due to patient’s ALS | 20, 8.0 | 7, 9.3 | 13, 7.5 |
| • Retired, unemployed, homemaker | 119, 47.8 | 43, 57.3 | 76, 43.7 |
| Health impairment due to caregiving (n = 249, n = 75, n = 174) | 106, 42.6 | 32, 42.7 | 74, 42.5 |
| • Only physical impairment | 12, 11.3 | 4, 12.5 | 8, 10.8 |
| • Only mental impairment | 15, 14.2 | 5, 15.6 | 10, 13.5 |
| • Physical and mental impairment | 79, 74.5 | 23, 71.9 | 56, 75.7 |
| DOC, hours per day (n = 249, n = 75, n = 174) | 3 (6)/3.85 (4.25) | 3 (6)/4.31 (4.03) | 2.5 (5)/3.65 (4.34) |
| ZBI score (n = 242, n = 74, n = 168); 0–88 | 26 (25)/26.28 (14.97) | 25 (26.25)/27.60 (15.25) | 26 (25)/25.68 (14.86) |
| EQ-VAS score (n = 243, n = 73, n = 170); 0–100 | 75 (28)/71.16 (20.47) | 75 (20)/69.27 (19.29) | 75 (30)/71.97 (20.96) |
| EQ-5D-5L index value (n = 244, n = 73, n = 171); −0.205–1.0 | 0.909 (0.193)/0.845 (0.196) | 0.909 (0.102)/0.849 (0.164) | 0.909 (0.193)/0.844 (0.209) |
| HADS-D score (n = 240, n = 71, n = 169); 0–21 | 8 (7)/7.80 (4.68) | 8 (7)/7.93 (4.47) | 7 (7)/7.75 (4.77) |
| HADS-A score (n = 240, n = 71, n = 169); 0–21 | 9 (6)/8.55 (4.28) | 7 (6)/7.69 (3.92) | 9 (6.5)/8.91 (4.38) |
| Variable | Change in ZBI | 95% CI | p-Value | |
|---|---|---|---|---|
| Mental health impairment of the caregiver | 11.36 | 6.84 | 15.87 | <0.001 |
| Use of wheelchair | 9.30 | 5.94 | 12.66 | <0.001 |
| Patient’s age | −0.24 | −0.37 | −0.11 | <0.001 |
| Permanent supervision necessary | 5.01 | 1.63 | 8.38 | 0.004 |
| Use of PEG | 3.80 | −0.25 | 7.86 | 0.066 |
| Use of home ventilator support | 2.77 | −0.97 | 6.51 | 0.146 |
| Physical health impairment of caregiver | 1.96 | −2.64 | 6.55 | 0.402 |
| Variable | Change in DOC | 95% CI | p-Value | |
|---|---|---|---|---|
| Use of wheelchair | 2.29 | 1.22 | 3.36 | <0.001 |
| Permanent supervision necessary | 1.86 | 0.78 | 2.93 | 0.001 |
| Physical health impairment of the caregiver | 1.62 | 0.15 | 3.09 | 0.031 |
| Use of home ventilator support | 1.32 | 0.12 | 2.52 | 0.031 |
| Patient’s age | 0.03 | −0.02 | 0.07 | 0.214 |
| Mental health impairment of the caregiver | 0.85 | −0.59 | 2.30 | 0.246 |
| Low Burden Group (ZBI Score < 24), n = 107 | High Burden Group (ZBI Score ≥ 24), n = 135 | Low vs. High Burden Group | ||
|---|---|---|---|---|
| EQ-VAS, range 0–100 | Mean (SD) Mann–Whitney test | 78.85 (18.25), n = 103 | 64.93 (20.45), n = 134 | U = 3750.50; Z = −6.05; p < 0.001; n = 237 |
| EQ-5D-5L index value, range 0–1 | Mean (SD) Mann–Whitney test | 0.905 (0.128), n = 104 | 0.796 (0.230), n = 134 | U = 4306.50; Z = −5.01; p < 0.001; n = 238 |
| HADS-D score, range 0–21 | Mean (SD) Mann–Whitney test | 4.78 (3.47), n = 101 | 10.05 (4.24), n = 133 | U = 2285.00; Z = −8.66; p < 0.001; n = 234 |
| HADS-A score, range 0–21 | Mean (SD) Mann–Whitney test | 6.02 (3.42), n = 101 | 10.52 (3.77), n = 133 | U = 2580.00; Z = −8.09; p < 0.001; n = 234 |
| Physical health impairment | Relative frequency χ2-test; Cramér’s V | 11.2%, n = 107 | 57.8%, n = 135 | χ2 = 55.40; φc = 0.478, p < 0.001; n = 242 |
| Mental health impairment | Relative frequency χ2-test; Cramér’s V | 11.2%, n = 107 | 60.0%, n = 135 | χ2 = 60.04; φc = 0.498, p < 0.001; n = 242 |
| General work life impairment | Relative frequency χ2-test; Cramér’s V | 25.0%, n = 44 | 78.0%, n = 59 | χ2 = 28.61; φc = 0.527, p < 0.001; n = 103 |
| Career restrictions | Relative frequency χ2-test; Cramér’s V | 13.6%, n = 44 | 51.7%, n = 58 | χ2 = 15.89; φc = 0.395, p < 0.001; n = 102 |
| Reduction of working hours | Relative frequency χ2-test; Cramér’s V | 11.6%, n = 43 | 60.0%, n = 55 | χ2 = 9.73; φc = 0.315, p = 0.001; n = 98 |
| Drop in salary | Relative frequency χ2-test; Cramér’s V | 12.5%, n = 40 | 30.2%, n = 53 | χ2 = 4.01; φc = 0.209, p = 0.043; n = 93 |
| Effect Comparison between the Female and Male CG Cohort | ||||
|---|---|---|---|---|
| Male CGs, n = 75 | Female CGs, n = 174 | Male vs. female CGs | ||
| ZBI, range 0–88 | Mean (SD) Mann–Whitney test | 27.60 (15.25), n = 74 | 25.68 (14.86), n = 168 | U = 5825.50; Z = −0.78; p = 0.436; n = 242 |
| DOC | Mean (SD) Mann–Whitney test | 4.31 (4.03), n = 75 | 3.65 (4.34), n = 174 | U = 5692.00; Z = −1.62; p = 0.105; n = 249 |
| EQ-VAS, range 0–100 | Mean (SD) Mann–Whitney test | 69.27 (19.29), n = 73 | 71.97 (20.96), n = 170 | U = 5463.50; Z = −1.48; p = 0.138; n = 243 |
| EQ-5D-5L index value, range 0–1 | Mean (SD) Mann–Whitney test | 0.849 (0.164), n = 73 | 0.844 (0.209), n = 171 | U = 5686.50; Z = −0.75; p = 0.457; n = 244 |
| HADS-D score, range 0–21 | Mean (SD) Mann–Whitney test | 7.93 (4.47), n = 71 | 7.75 (4.77), n = 169 | U = 5744,50; Z = −0.52; p = 0.603; n = 240 |
| HADS-A score, range 0–21 | Mean (SD) Mann–Whitney test | 7.69 (3.92), n = 71 | 8.91 (4.38), n = 169 | U = 5059.00; Z = −1.92; p = 0.055; n = 240 |
| Physical health impairment | Relative frequency χ2-test; Cramér’s V | 34.7%, n = 75 | 37.4%, n = 174 | χ2 = 0.16; φc = 0.026, p = 0.686; n = 249 |
| Mental health impairment | Relative frequency χ2-test; Cramér’s V | 36.0%, n = 75 | 38.5%, n = 174 | χ2 = 0.14; φc = 0.024, p = 0.708; n = 249 |
| General work life impairment | Relative frequency χ2-test; Cramér’s V | 45.8%, n = 24 | 56.8%, n = 81 | χ2 = 0.90; φc = 0.092, p = 0.344; n = 105 |
| Career restrictions | Relative frequency χ2-test; Cramér’s V | 24.0%, n = 25 | 40.0%, n = 80 | χ2 = 2.11; φc = 0.142, p = 0.146; n = 105 |
| Reduction of working hours | Relative frequency χ2-test; Cramér’s V | 33.3%, n = 24 | 24.7%, n = 77 | χ2 = 0.70; φc = 0.083, p = 0.403; n = 101 |
| Drop in salary | Relative frequency χ2-test; Cramér’s V | 19.0%, n = 21 | 22.7%, n = 75 | χ2 = 0.126; φc = 0.036, p = 0.723; n = 96 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schischlevskij, P.; Cordts, I.; Günther, R.; Stolte, B.; Zeller, D.; Schröter, C.; Weyen, U.; Regensburger, M.; Wolf, J.; Schneider, I.; et al. Informal Caregiving in Amyotrophic Lateral Sclerosis (ALS): A High Caregiver Burden and Drastic Consequences on Caregivers’ Lives. Brain Sci. 2021, 11, 748. https://doi.org/10.3390/brainsci11060748
Schischlevskij P, Cordts I, Günther R, Stolte B, Zeller D, Schröter C, Weyen U, Regensburger M, Wolf J, Schneider I, et al. Informal Caregiving in Amyotrophic Lateral Sclerosis (ALS): A High Caregiver Burden and Drastic Consequences on Caregivers’ Lives. Brain Sciences. 2021; 11(6):748. https://doi.org/10.3390/brainsci11060748
Chicago/Turabian StyleSchischlevskij, Pavel, Isabell Cordts, René Günther, Benjamin Stolte, Daniel Zeller, Carsten Schröter, Ute Weyen, Martin Regensburger, Joachim Wolf, Ilka Schneider, and et al. 2021. "Informal Caregiving in Amyotrophic Lateral Sclerosis (ALS): A High Caregiver Burden and Drastic Consequences on Caregivers’ Lives" Brain Sciences 11, no. 6: 748. https://doi.org/10.3390/brainsci11060748
APA StyleSchischlevskij, P., Cordts, I., Günther, R., Stolte, B., Zeller, D., Schröter, C., Weyen, U., Regensburger, M., Wolf, J., Schneider, I., Hermann, A., Metelmann, M., Kohl, Z., Linker, R. A., Koch, J. C., Stendel, C., Müschen, L. H., Osmanovic, A., Binz, C., ... Schreiber-Katz, O. (2021). Informal Caregiving in Amyotrophic Lateral Sclerosis (ALS): A High Caregiver Burden and Drastic Consequences on Caregivers’ Lives. Brain Sciences, 11(6), 748. https://doi.org/10.3390/brainsci11060748










