One-Year Demographical and Clinical Indices of Patients with Chronic Disorders of Consciousness
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Assessment of the Level of Consciousness and Diagnostic Procedure
2.3. Follow-Up Data Collection
2.4. Statistical Data Analysis
2.5. Legal Issues
3. Results
3.1. Demographical and Clinical Data
3.2. Mortality within First Year after Brain Injury
3.3. Changes in the Level of Consciousness during the First Year after the Brain Injury
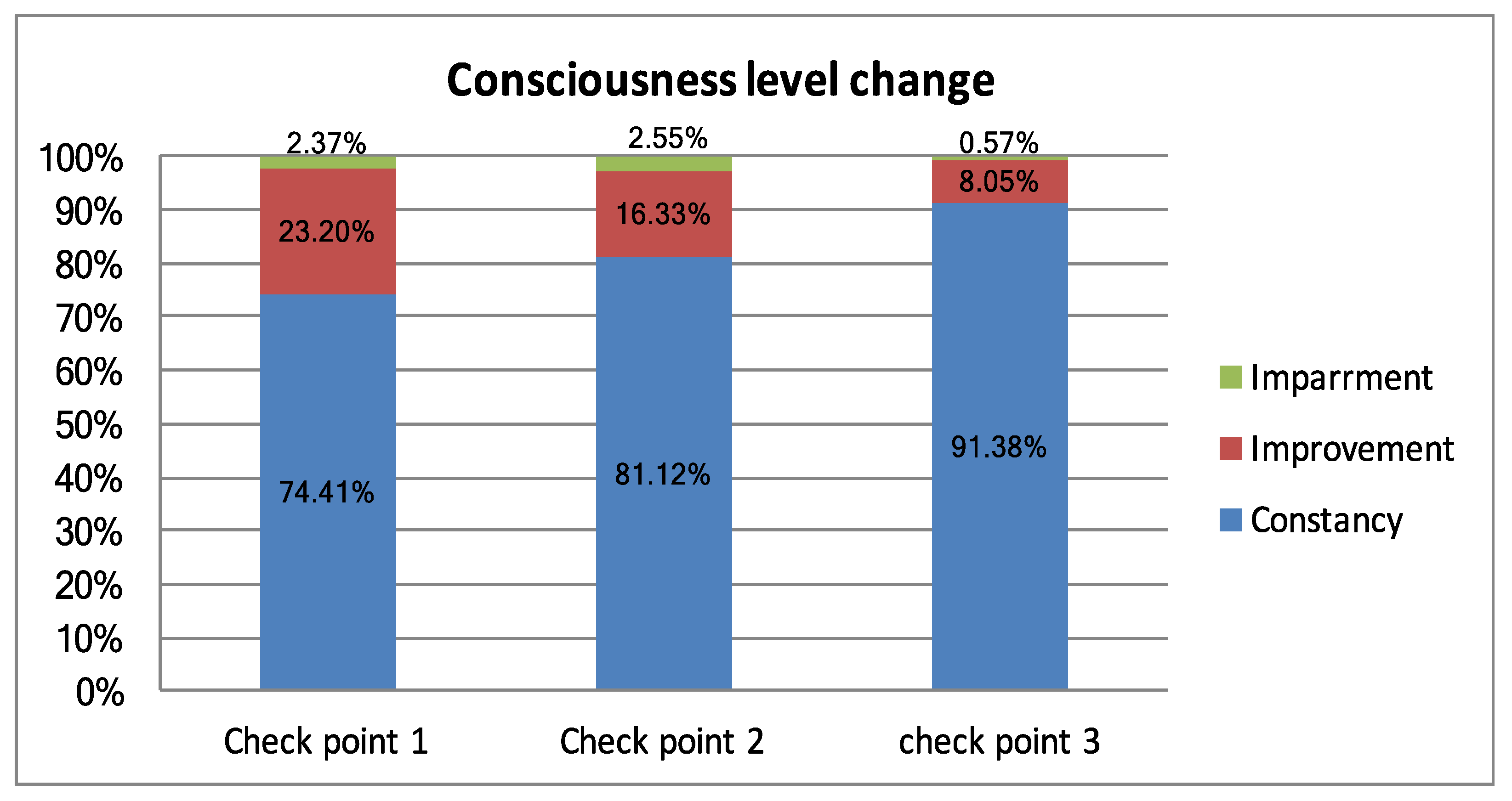
3.4. Predictors of Survival and Recovery of Consciousness in Patients with Chronic DOC
- The initial CRS-R score;
- Etiology;
- Gender and age of patients.
3.4.1. The Initial CRS-R Score
3.4.2. Etiology: Mortality and Changes in Consciousness Level
3.4.3. Gender and Age
3.4.4. Logistic Regression Analysis
4. Discussion
- The remote method for determining the level of consciousness at the post-hospital stage, which does not exclude errors in the differential diagnosis of DOC. To minimize erroneous results, we abandoned the scale assessment, which can only be carried out with direct contact with the patient.
- The relatively short duration of the study. In the context of the tendencies towards the abolition of the term “permanent” in relation to DOC, it is more rational to assess the above indicators at a longer stage.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Owen, A.M. Detecting Consciousness: A Unique Role for Neuroimaging. Annu. Rev. Psychol. 2013, 64, 109–133. [Google Scholar] [CrossRef]
- Laureys, S.; Celesia, G.G.; Cohadon, F.; Lavrijsen, J.; León-Carrión, J.; Dolce, G. Unresponsive wakefulness syndrome: A new name for the vegetative state or apallic syndrome. BMC Med. 2010, 8. [Google Scholar] [CrossRef] [PubMed]
- Erp, V.S.W.; Aben, L.A.M.; Lavrijsen, M.J.C.; Vos, E.P.; Laureys, S.; Koopmans, M.R.T.C. Unexpected emergence from the vegetative state: Delayed discovery rather than late recovery of consciousness. J. Neurol. 2019. [Google Scholar] [CrossRef]
- Laureys, S.; Boly, M.; Maquet, P. Tracking the recovery of consciousness from coma. J. Clin. Invest. 2006, 116, 1823–1825. [Google Scholar] [CrossRef] [PubMed]
- Giacino, J.T.; Fins, J.J.; Laureys, S.; Schiff, N.D. Disorders of consciousness after acquired brain injury: The state of the science. Nat. Rev. Neurol. 2014, 10, 99–114. [Google Scholar] [CrossRef]
- Giacino, J.T.; Katz, D.I.; Schiff, N.D.; Whyte, J.; Ashman, E.J.; Ashwal, S.; Armstrong, M.J. Practice Guideline Update Recommendations Summary: Disorders of Consciousness. Arch. Phys. Med. Rehabil. 2018. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Luo, X.; Wan, M.; Li, J.; Wang, H.; Wei, D.; Feng, H. The effectiveness of non-invasive brain stimulation on arousal and alertness in patients in coma or persistent vegetative state after traumatic brain injury. Medicine 2018, 97, e12321. [Google Scholar] [CrossRef] [PubMed]
- Nakase-Richardson, R.; Whyte, J.; Giacino, J.T.; Pavawalla, S.; Barnett, S.D.; Yablon, S.A.; Walker, W.C. Longitudinal Outcome of Patients with Disordered Consciousness in the NIDRR TBI Model. Systems Programs. J. Neurotrauma 2012, 29, 59–65. [Google Scholar] [CrossRef]
- Higashi, K.; Sakata, Y.; Hatano, M.; Abiko, S.; Ihara, K.; Katayama, S.; Aoki, H. Epidemiological studies on patients with a persistent vegetative state. J. Neurol. Neurosurg. Psychiatry 1977, 40, 876–885. [Google Scholar] [CrossRef]
- Luaute, J.; Maucort-Boulch, D.; Tell, L.; Quelard, F.; Sarraf, T.; Iwaz, J.; Fischer, C. Long-term outcomes of chronic minimally conscious and vegetative states. Neurology 2010, 75, 246–252. [Google Scholar] [CrossRef]
- Estraneo, A.; Moretta, P.; Loreto, V.; Lanzillo, B.; Santoro, L.; Trojano, L. Late recovery after traumatic, anoxic, or hemorrhagic long-lasting vegetative state. Neurology 2010, 75, 239–245. [Google Scholar] [CrossRef]
- Estraneo, A.; Moretta, P.; Loreto, V.; Lanzillo, B.; Cozzolino, A.; Saltalamacchia, A.; Trojano, L. Predictors of recovery of responsiveness in prolonged anoxic vegetative state. Neurology 2013, 80, 464–470. [Google Scholar] [CrossRef]
- Steppacher, I.; Kaps, M.; Kissler, J. Will time heal? A long-term follow-up of severe disorders of consciousness. Ann. Clin. Transl. Neurol. 2014, 1, 401–408. [Google Scholar] [CrossRef] [PubMed]
- Baricich, A. Recovery from vegetative state of patients with a severe brain injury: A 4-year real-practice with a severe brain injury: A 4-year real-practice prospective cohort study. Funct. Neurol. 2017, 37, 131. [Google Scholar] [CrossRef] [PubMed]
- Aidinoff, E.; Groswasser, Z.; Bierman, U.; Gelernter, I.; Catz, A.; Gur-Pollack, R. Vegetative state outcomes improved over the last two decades. Brain Inj. 2017, 32, 297–302. [Google Scholar] [CrossRef] [PubMed]
- Faugeras, F.; Rohaut, B.; Valente, M.; Sitt, J.; Demeret, S.; Bolgert, F.; Naccache, L. Survival and consciousness recovery are better in the minimally conscious state than in the vegetative state. Brain Inj. 2017, 32, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Yelden, K.; Duport, S.; James, L.M.; Kempny, A.; Farmer, S.F.; Leff, A.P.; Playford, E.D. Late recovery of awareness in prolonged disorders of consciousness –a cross-sectional cohort study. Disabil. Rehabil. 2017, 40, 2433–2438. [Google Scholar] [CrossRef]
- Pascarella, A. Multicentre registry of brain-injured patients with disorder of consciousness: Rationale and preliminary data. Funct. Neurol. 2018, 33, 19. [Google Scholar] [CrossRef] [PubMed]
- Estraneo, A.; De Bellis, F.; Masotta, O.; Loreto, V.; Fiorenza, S.; Lo Sapio, M.; Trojano, L. Demographical and clinical indices for long-term evolution of patients in vegetative or in minimally conscious state. Brain Inj. 2019, 1–7. [Google Scholar] [CrossRef]
- Chen, W.G.; Li, R.; Zhang, Y.; Jian-Hui, H.; Ju-Bao, D.; Ai-Song, G.; Wei-Qun, S. Recovery from prolonged disorders of consciousness: A dual-center prospective cohort study in China. World J. Clin. Cases. 2020, 8, 2520–2529. [Google Scholar] [CrossRef]
- Estraneo, A.; Fiorenza, S.; Magliacano, A.; Formisano, R.; Mattia, D.; Grippo, A.; Trojano, L. Multi-center prospective study on predictors of short-term outcome in disorders of consciousness. Neurology 2020. [Google Scholar] [CrossRef] [PubMed]
- Bruno, M.-A.; Ledoux, D.; Vanhaudenhuyse, A.; Gosseries, O.; Thibaut, A.; Laureys, S. Prognosis of Patients with Altered State of Consciousness. Coma Disord. Conscious. 2012, 11–23. [Google Scholar] [CrossRef]
- Eilander, H.J.; Wijnen, V.J.; Scheirs, J.G.; de Kort, P.L.; Prevo, A.J. Children and young adults in a prolonged unconscious state due to severe brain injury: Outcome after an early intensive neurorehabilitation programme. Brain Inj. 2005, 19, 425–436. [Google Scholar] [CrossRef] [PubMed]
- Bruno, M.A.; Vanhaudenhuyse, A.; Schnakers, C.; Boly, M.; Gosseries, O.; Demertzi, A.; Majerus, S.; Moonen, G.; Hustinx, R.; Laureys, S. Visual fixation in the vegetative state: An observational case series PET study. BMC Neurol. 2010, 10, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Giacino, J. Disorders of Consciousness: Differential Diagnosis and Neuropathologic Features. Semin. Neurol. 1997, 17, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Gupte, R.; Brooks, W.M.; Vukas, R.R.; Pierce, J.D.; Harris, J.L. Sex differences in traumatic brain injury: What we know and what we should know. J. Neurotrauma 2018, 6171. [Google Scholar] [CrossRef]
- Bagnato, S.; Boccagni, C.; Sant’Angelo, A.; Fingelkurts, A.A.; Galardi, G. Longitudinal Assessment of Clinical Signs of Recovery in Patients with Unresponsive Wakefulness Syndrome after Traumatic or Nontraumatic Brain Injury. J. Neurotrauma 2016, 4418. [Google Scholar] [CrossRef]
- Lee, H.Y.; Park, J.H.; Kim, A.R.; Park, M.; Kim, T. Neurobehavioral recovery in patients who emerged from prolonged disorder of consciousness: A retrospective study. BMC Neurol. 2020, 20, 1–11. [Google Scholar] [CrossRef]
| No. | Study | Number of Patients According to the Level of Consciousness | Number of Patients according to the Etiology | Survival Rate, Level of Consciousness/Number of Patients/Years of Follow-Up | Improvement of Consciousness, Level of Consciousness/Number of Patients/Years of Follow-Up |
|---|---|---|---|---|---|
| 1 | Nakase-Richardson et al., 1977 [8] | VS/UWS + MCS—396 | TBI—396 | VS/UWS + MCS/368/2 | VS/UWS + MCS/28/3 |
| 2 | Higashi et al., 1977 [9] | VS/UWS—10, MCS—0 | TBI—about 1/3, VL—about 1/5 | VS/UWS/65/1 VS/UWS/39/3 | VS/UWS/9/1 |
| 3 | Luaute et al., 2010 [10] | VS/UWS—12, MCS—39 | TBI—18, ABI—16, Other—17 | VS/UWS/3/5 MCS/25/5 | VS/UWS/0/5 MCS/13/5 |
| 4 | Estraneo et al., 2010 [11] | VS/UWS—50, MCS—0 | TBI—18, ABI—18, VL—14 | VS/UWS/29/1 | VS/UWS/6/1 |
| 5 | Estraneo et al., 2013 [12] | VS/UWS—43, MCS—0 | ABI—43 | VS/UWS/19/2 | VS/UWS/9/2 |
| 6 | Steppacher et al., 2014 [13] | VS/UWS—59, MCS—43 | Not specified | VS/UWS + MCS/29/2 | VS/UWS + MCS/12/2 |
| 7 | Baricich et al., 2017 [14] | VS/UWS—49, MCS—0 | ABI—24, TBI—12, VL—11 | VS/UWS/20/4 | VS/UWS/6/4 |
| 8 | Aidinoff et al., 2017 [15] | VS/UWS—206, MCS—0 | TBI—154, ABI—14, VL—30, Other—8 | VS/UWS/139/1 VS/UWS/107/2 VS/UWS/105/3 | VS/UWS/111/3 |
| 9 | Faugeras et al., 2017 [16] | VS/UWS—33, MCS—34 | TBI—13, ABI—19, Other—35 | VS/UWS/5/0.5–3 MCS/20/0.5–3 | No data available |
| 10 | Yelden et al., 2017 [17] | VS/UWS—27, MCS—7 | ABI—15, TBI—6, VL—13 | No data available | VS/UWS + MCS/11/2 - 16 |
| 11 | Pascarella et al., 2018 [18] | VS/UWS—37, MCS—16 | TBI—12, ABI—11, VL—30 | VS/UWS + MCS/37/6 | VS/UWS + MCS/17/6 |
| 12 | Estraneo et al., 2019 [19] | VS/UWS—159, MCS—57 | VL—96, ABI—71, TBI—49 | VS/UWS/131/1 VS/UWS/105/2 VS/UWS/92/3 MCS/41/1 MCS/34/2 MCS/32/3 | VS/UWS/35/1 VS/UWS/8/2 VS/UWS/0/3 MCS/26/1 MCS/1/2 MCS/1/3 |
| 13 | Chen et al., 2020 [20] | VS/UWS—52, MCS—31 | ABI—10, TBI—35, VL—48 | VS/UWS + MCS/7/1 | VS/UWS + MCS/33/3 |
| 14 | Estraneo et al., 2020 [21] | VS/UWS—71 MCS—76 | ABI—36, TBI—55, VL—56 | VS/UWS/60/0.5 MCS/72/0.5 | VS/UWS + MCS/72/0.5 |
| Mean (Median) Age | 44.99 ± 15.69 (43 (32, 59) | |||
|---|---|---|---|---|
| Sex (Male/Female) | 122/89 | |||
| Etiology | Total (Male/Female) | VS/UWS | MCS− | MCS+ |
| Anoxia | 53 (26/27) | 40 | 12 | 1 |
| TBI | 93 (65/28) | 44 | 25 | 24 |
| Vascular lesions | 59 (28/31) | 35 | 16 | 8 |
| Other | 6 (3/3) | 4 | 2 | 0 |
| Total level of consciousness | 123 | 55 | 33 | |
| Mean CRS-R score | 7.34 ± 3.67 | 5.081 ± 1.22 | 8.22 ± 2.2 | 14.33 ± 1.83 |
| Level of Consciousness | At 3 Months | At 6 Months | At 12 Months |
|---|---|---|---|
| Total: 74 | 15 | 22 | 37 |
| VS/UWS | 13 | 8 | 20 |
| MCS− | 1 | 6 | 11 |
| MCS+ | 1 | 4 | 6 |
| Coma | 3 | ||
| Conscious | 1 |
| Level of Consciousness | Improvement (the Level of Consciousness Achieved) (out of Them Died) | Impairment (the Level of Consciousness Achieved) (out of Them Died) | No Change (out of Them Died) |
|---|---|---|---|
| Total: 211 | 49 (20 in MCS−; 21 in MCS+; 8 conscious) (1) | 5 (2 in coma; 3 in MCS−) (1) | 157 (13) |
| VS/UWS | 27 (20 in MCS−; 5 in MCS+; 2 conscious) | 0 | 96 (12) |
| MCS− | 17 (16 in MCS+; 1 conscious) (1) | 1 (1 in coma) | 37 (1) |
| MCS+ | 5 (5 conscious) | 4 (1 in coma; 3 in MCS−) (1) | 24 |
| Level of Consciousness | Improvement (the Level of Consciousness Achieved) (out of Them Died) | Impairment (the Level of Consciousness Achieved) (out of Them Died) | No Change (out of Them Died) |
|---|---|---|---|
| Total: 196 | 32 (15 in MCS−; 12 in MCS+; 5 conscious) (3) | 5 (2 in coma; 2 in MCS−; 1 in VS/UWS) (2) | 159 (17) |
| VS/UWS | 18 (15 in MCS−; 3 in MCS+) (1) | 1 (1 in coma) (1) | 65 (8) |
| MCS− | 10 (9 in MCS+, 1 conscious) (2) | 1 (1 in VS/UWS) | 48 (5) |
| MCS+ | 4 (4 conscious) | 3 (1 in coma, 2 in MCS−) (1) | 37 (3) |
| Coma | 1 (1) | ||
| Conscious | 8 |
| Level of Consciousness | Improvement (the Level of Consciousness Achieved) (out of Them Died) | Impairment (the Level of Consciousness Achieved) (out of Them Died) | No Change (out of Them Died) |
|---|---|---|---|
| Total: 174 | 14 (2 in MCS−; 6 in MCS+; 6 conscious) (4) | 1 (1 in VS/UWS) (1) | 159 (32) |
| VS/UWS | 5 (2 in MCS−; 2 in MCS+; 1 conscious) (2) | 53 (19) | |
| MCS− | 6 (4 in MCS+; 2 conscious) (2) | 53 (11) | |
| MCS+ | 3 (3 conscious) | 1 (in VS/UWS) (1) | 41 (2) |
| Coma | |||
| Conscious | 12 |
| Etiology | C, init | N, init | C, 3 m | N, 3 m | D, 3 m | C, 6 m | N, 6 m | D, 6 m | C, 12 m | N, 12 m | D, 12 m |
|---|---|---|---|---|---|---|---|---|---|---|---|
| ABI | 1 | 52 | 3 (+2) | 43 (−9) | 7 | 5 (+2) | 36 (−7) | 12 (+5) | 5 | 24 (−12) | 24 (+12) |
| TBI | 24 | 69 | 31 (+7) | 61 (−8) | 1 | 33 (+2) | 55 (−6) | 5 (+4) | 37 (+4) | 34 (−21) | 22 (+17) |
| VL | 8 | 51 | 18 (+10) | 36 (−15) | 5 | 18 | 24 (−12) | 17 (+12) | 17 (+2) | 18 (−6) | 24 (+7) |
| Other | 0 | 6 | 0 | 4 (−2) | 2 | 1 (+1) | 2 (−2) | 3 (+1) | 4 (+3) | 2 | 4 (+1) |
| Factor | Reference | β | p | OR (95% CI) |
|---|---|---|---|---|
| Age | –0.05 | <0.001 | 0.94 (0.92–0.97) | |
| Gender (M) | F | –0.17 | 0.61 | 0.84 (0.43–1.63) |
| Etiology (Traumatic) | Non-Traumatic | –0.12 | 0.74 | 0.88 (0.42–1.84) |
| Status (Non-Communicating) | Communicating | –0.65 | 0.47 | 0.52 (0.08–3.2) |
| CRS-R | 0.25 | <0.001 | 1.29 (1.08–1.53) |
| Factor | Reference | β | p | OR (95% CI) |
|---|---|---|---|---|
| Age | 0.01 | 0.26 | 1.02 (0.99–1.04) | |
| Gender (M) | F | 0.12 | 0.77 | 1.13 (0.49–2.63) |
| Etiology (Traumatic) | Non-Traumatic | –0.47 | 0.29 | 0.62 (0.25–1.51) |
| CRS-R | –0.13 | 0.05 | 0.88 (0.77–1.00) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nekrasova, J.; Kanarskii, M.; Borisov, I.; Pradhan, P.; Shunenkov, D.; Vorobiev, A.; Smirnova, M.; Pasko, V.; Petrova, M.V.; Luginina, E.; et al. One-Year Demographical and Clinical Indices of Patients with Chronic Disorders of Consciousness. Brain Sci. 2021, 11, 651. https://doi.org/10.3390/brainsci11050651
Nekrasova J, Kanarskii M, Borisov I, Pradhan P, Shunenkov D, Vorobiev A, Smirnova M, Pasko V, Petrova MV, Luginina E, et al. One-Year Demographical and Clinical Indices of Patients with Chronic Disorders of Consciousness. Brain Sciences. 2021; 11(5):651. https://doi.org/10.3390/brainsci11050651
Chicago/Turabian StyleNekrasova, Julia, Mikhail Kanarskii, Ilya Borisov, Pranil Pradhan, Denis Shunenkov, Alexey Vorobiev, Maria Smirnova, Vera Pasko, Marina V. Petrova, Elena Luginina, and et al. 2021. "One-Year Demographical and Clinical Indices of Patients with Chronic Disorders of Consciousness" Brain Sciences 11, no. 5: 651. https://doi.org/10.3390/brainsci11050651
APA StyleNekrasova, J., Kanarskii, M., Borisov, I., Pradhan, P., Shunenkov, D., Vorobiev, A., Smirnova, M., Pasko, V., Petrova, M. V., Luginina, E., & Pryanikov, I. (2021). One-Year Demographical and Clinical Indices of Patients with Chronic Disorders of Consciousness. Brain Sciences, 11(5), 651. https://doi.org/10.3390/brainsci11050651