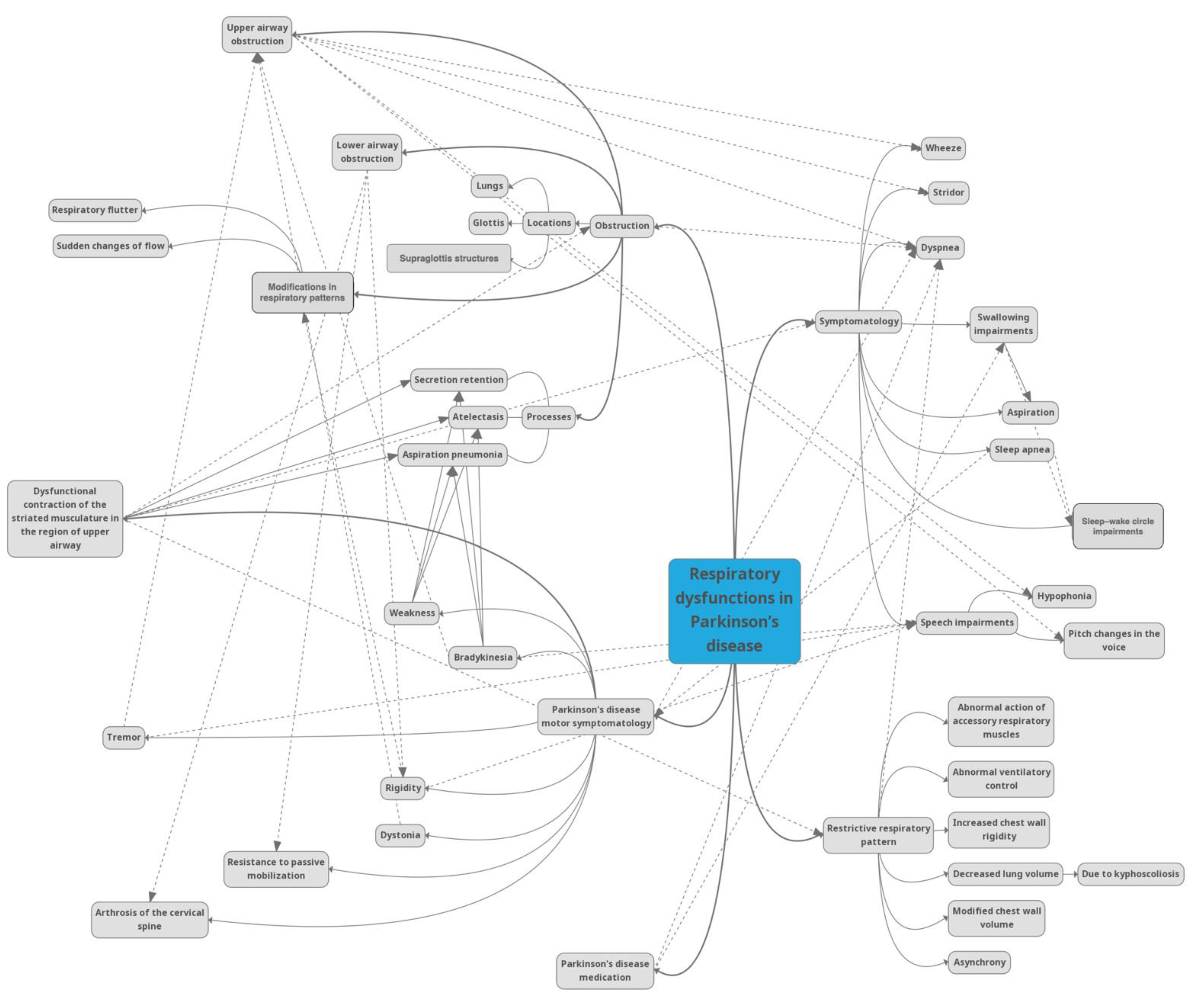
Respiratory Dysfunctions in Parkinson’s Disease Patients
Abstract
1. Introduction
2. Neuroanatomy and Pathophysiology of Respiratory Dysfunction in Parkinson’s Disease
3. Chest Wall Volume and Asynchrony
4. Obstruction
5. Dyspnea
6. Implications of Respiratory Characteristics in the Speech of Parkinson’s Disease Patients
7. Implications of Respiratory Characteristics in Swallowing and Aspiration of Parkinson’s Disease Patients
8. Sleep Disorder Breathing and Daytime Somnolence for Parkinson’s Disease Patients
9. The Effects of Treatment of Parkinson’s Disease on Respiratory Function
10. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Jankovic, J. Parkinson’s disease: Clinical features and diagnosis. J. Neurol. Neurosurg. Psychiatry 2008, 79, 368–376. [Google Scholar] [CrossRef]
- Monteiro, L.; Souza-Machado, A.; Pinho, P.; Sampaio, M.; Nobrega, A.C.; Melo, A. Swallowing impairment and pulmonary dysfunction in Parkinson’s disease: The silent threats. J. Neurol. Sci. 2014, 339, 149–152. [Google Scholar] [CrossRef] [PubMed]
- Braak, H.; Del Tredici, K.; Rüb, U.; de Vos, R.A.; Jansen Steur, E.N.; Braak, E. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol. Aging 2003, 24, 197–211. [Google Scholar] [CrossRef]
- Kazemi, H.; Johnson, D.C. Encyclopedia of the Human Brain; Ramachandran, V.S., Ed.; Academic Press: San Diego, CA, USA, 2002. [Google Scholar]
- Mehanna, R.; Jankovic, J. Respiratory problems in neurologic movement disorders. Parkinsonism Relat. Disord. 2010, 10, 628–638. [Google Scholar] [CrossRef]
- Weiner, P.; Inzelberg, R.; Davidovich, A.; Nisipeanu, P.; Magadle, R.; Berar-Yanay, N.; Carasso, R.L. Respiratory muscle performance and the Perception of dyspnea in Parkinson’s disease. Can. J. Neurol. Sci. 2002, 1, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Parkinson, J. An essay on the shaking palsy. 1817. J. Neuropsychiatry Clin. Neurosci. 2002, 2, 223–236. [Google Scholar] [CrossRef]
- Storch, A.; Schneider, C.B.; Wolz, M.; St¨urwald, Y.; Nebe, A.; Odin, P.; Mahler, A.; Fuchs, G.; Jost, W.H.; Chaudhuri, K.R.; et al. Nonmotor fluctuations in Parkinson disease: Severity and correlation with motor complications. Neurology 2013, 9, 800–809. [Google Scholar] [CrossRef]
- De Pandis, M.F.; Starace, A.; Stefanelli, F.; Marruzzo, P.; Meoli, I.; De Simone, G.; Prati, R.; Stocchi, F. Modification of respiratory function parameters in patients with severe Parkinson’s disease. Neurol. Sci. Suppl. 2002, 2, 69–70. [Google Scholar] [CrossRef]
- Cardoso, S.R.X.; Pereira, J.S. Analysis of breathing function in Parkinson’s disease. Arq. Neuropsiquiatr. 2002, 1, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.A.; Prentice, W.M.; Hildreth, A.J.; Walker, R.W. Measuring symptom load in idiopathic Parkinson’s disease. Parkinsonism Relat. Disord. 2007, 13, 284–289. [Google Scholar] [CrossRef]
- Diederich, N.J.; McIntyre, D.J. Sleep disorders in Parkinson’s disease: Many causes, few therapeutic options. J. Neurol. Sci. 2012, 314, 12.e9. [Google Scholar] [CrossRef]
- Troche, M.S.; Huebner, I.; Rosenbek, J.C.; Okun, M.S.; Sapienza, C.M. Respiratory-swallowing coordination and swallowing safety in patients with Parkinson’s disease. Dysphagia 2011, 26, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Hammer, M.J.; Murphy, C.A.; Abrams, T.M. Airway somatosensory deficits and dysphagia in Parkinson’s disease. J. Parkinsons Dis. 2013, 3, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Tuppy, M.; Barna, B.F.; Alves-Dos-Santos, L.; Britto, L.R.; Chiavegatto, S.; Moreira, T.S.; Takakura, A.C. Respiratory deficits in a rat model of Parkinson’s disease. Neuroscience 2015, 297, 194–204. [Google Scholar] [CrossRef]
- Zhang, L.Y.; Liu, W.Y.; Kang, W.Y.; Yang, Q.; Wang, X.Y.; Ding, J.Q.; Chen, S.D.; Liu, J. Association of rapid eye movement sleep behavior disorder with sleep-disordered breathing in Parkinson’s disease. Sleep Med. 2016, 20, 110–115. [Google Scholar] [CrossRef]
- Fernandes-Junior, S.A.; Carvalho, K.S.; Moreira, T.S.; Takakura, A.C. Correlation between neuroanatomical and functional respiratory changes observed in an experimental model of Parkinson’s disease. Exp. Physiol. 2018, 103, 1377–1389. [Google Scholar] [CrossRef] [PubMed]
- Gourine, A.V.; Kasymov, V.; Marina, N.; Tang, F.; Figueiredo, M.F.; Lane, S.; Teschemacher, A.G.; Spyer, K.M.; Deisseroth, K.; Kasparov, S. Astrocytes control breathing through pH-dependent release of ATP. Science 2010, 329, 571–575. [Google Scholar] [CrossRef] [PubMed]
- Wenker, I.C.; Kréneisz, O.; Nishiyama, A.; Mulkey, D.K. Astrocytes in the retrotrapezoid nucleus sense H+ by inhibition of a Kir4. 1–Kir5. 1-like current and may contribute to chemoreception by a purinergic mechanism. J. Neurophysiol. 2010, 104, 3042–3052. [Google Scholar] [CrossRef][Green Version]
- Onodera, H.; Okabe, S.; Kikuchi, Y.; Tsuda, T.; Itoyama, Y. Impaired chemosensitivity and perception of dyspnoea in Parkinson’s disease. Lancet 2000, 356, 739–740. [Google Scholar] [CrossRef]
- Seccombe, L.M.; Giddings, H.L.; Rogers, P.G.; Corbett, A.J.; Hayes, M.W.; Peters, M.J.; Veitch, E.M. Abnormal ventilatory control in Parkinson’s disease—Further evidence for non-motor dysfunction. Respir. Physiol. Neurobiol. 2011, 179, 300–304. [Google Scholar] [CrossRef]
- Izquierdo-Alonso, J.L.; Jimenez-Jimenez, F.J.; Cabrera-Valdivia, F.; Mansilla-Lesmes, M. Airway dysfunction in patients with Parkinson’s disease. Lung 1994, 172, 47–55. [Google Scholar] [CrossRef]
- Sabaté, M.; González, I.; Ruperez, F.; Rodriguez, M. Obstructive and restrictive pulmonary dysfunctions in Parkinson’s disease. J. Neurol. Sci. 1996, 138, 114–119. [Google Scholar] [CrossRef]
- Sathyaprabha, T.N.; Kapavarapu, P.K.; Pal, P.K.; Thennarasu, K.; Raju, T.R. Pulmonary functions in Parkinson’s disease. Indian J. Chest Dis. Allied Sci. 2005, 47, 251–257. [Google Scholar] [PubMed]
- Pal, P.K.; Sathyaprabha, T.N.; Tuhina, P.; Thennarasu, K. Pattern of subclinical pulmonary dysfunctions in Parkinson’s disease and the effect of levodopa. Mov. Disord. 2007, 3, 420–424. [Google Scholar] [CrossRef] [PubMed]
- Florêncio, R.B.; da Nobrega, A.J.S.; Lima I´, N.D.F.; Gualdi, L.P.; Cabral, E.E.; Fagundes, M.L.L.C.; Aliverti, A.; Resqueti, V.R.; de Fregonezi, G.A. Chest wall volume and asynchrony in stroke and Parkinson’s disease subjects: A case-control study. PLoS ONE 2019, 14, e0216641. [Google Scholar] [CrossRef] [PubMed]
- Hoehn, M.M.; Yahr, M.D. Parkinsonism: Onset, progression and mortality. Neurology 1967, 17, 427–442. [Google Scholar] [CrossRef]
- McMahon, L.; Blake, C.; Lennon, O. Nonpharmacological interventions for respiratory health in Parkinson’s disease: A systematic review and meta-analysis. Eur. J. Neurol. 2021, 28, 1022–1040. [Google Scholar] [CrossRef]
- Rodríguez, M.Á.; Crespo, I.; Del Valle, M.; Olmedillas, H. Should respiratory muscle training be part of the treatment of Parkinson’s disease? A systematic review of randomized controlled trials. Clin. Rehabil. 2020, 34, 429–437. [Google Scholar] [CrossRef]
- Vincken, W.G.; Gauthier, S.G.; Dolfuss, R.E.; Hanson, R.E.; Darauay, C.M.; Cosio, M.G. Involvement of upper airway muscles in extrapyramidal disorders: A cause of airflow limitation. N. Engl. J. Med. 1984, 311, 438–442. [Google Scholar] [CrossRef] [PubMed]
- Herer, B.; Arnulf, I.; Housset, B. Effects of levodopa on pulmonary function in Parkinson’s disease. Chest 2001, 119, 387–393. [Google Scholar] [CrossRef]
- Vincken, W.G.; Darauay, C.M.; Cosio, M.G. Reversibility of upper airway obstruction after levodopa therapy in Parkinson’s disease. Chest 1989, 96, 210–212. [Google Scholar] [CrossRef]
- Hovestadt, A.; Bogaard, J.M.; Meerwaldt, J.D.; van der Meche, F.G.A. Pulmonary function in Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 1989, 52, 329–333. [Google Scholar] [CrossRef] [PubMed]
- Guindi, G.M.; Bannister, R.; Gibson, W.P.; Payne, J.K. Laryngeal electromyography in multiple system atrophy with autonomic failure. J. Neurol. Neurosurg. Psychiatry 1981, 44, 49–53. [Google Scholar] [CrossRef] [PubMed]
- Estenne, M.; Hubert, M.; De Troyer, A. Respiratory-muscle involvement in Parkinson’s disease. N. Engl. J. Med. 1984, 311, 1516–1517. [Google Scholar] [PubMed]
- Neu, H.C.; Connolly JJJr Schwertley, F.W.; Ladwig, H.A.; Brody, A.W. Obstructive respiratory dysfunction in parkinsonian patients. Am. Rev. Respir. Dis. 1967, 95, 33–47. [Google Scholar]
- Parshall, M.B.; Schwartzstein, R.M.; Adams, L.; Banzett, R.B.; Manning, H.L.; Bourbeau, J.; Calverley, P.M.; Gift, A.G.; Harver, A.; Lareau, S.C.; et al. An official American Thoracic Society statement: Update on the mechanisms, assessment, and management of dyspnea. Am. J. Respir. Crit. Care Med. 2012, 185, 435–452. [Google Scholar] [CrossRef]
- Shill, H.; Stacy, M. Respiratory complications of Parkinson’s disease. Semin. Respir. Crit. Care Med. 2002, 23, 261–266. [Google Scholar] [CrossRef]
- Baille, G.; Chenivesse, C.; Perez, T.; Machuron, F.; Dujardin, K.; Devos, D.; Defebvre, L.; Moreau, C. Dyspnea: An underestimated symptom in Parkinson’s disease. Parkinsonism Relat. Disord. 2019, 60, 162–166. [Google Scholar] [CrossRef]
- Witjas, T.; Kaphan, E.; Azulay, J.P.; Blin, O.; Ceccaldi, M.; Pouget, J.; Poncet, M.; Chérif, A.A. Nonmotor fluctuations in Parkinson’s disease: Frequent and disabling. Neurology 2002, 59, 408–413. [Google Scholar] [CrossRef]
- Barone, P.; Antonini, A.; Colosimo, C.; Marconi, R.; Morgante, L.; Avarello, T.P.; Bottacchi, E.; Cannas, A.; Ceravolo, G.; Ceravolo, R.; et al. The PRIAMO study: A multicenter assessment of nonmotor symptoms and their impact on quality of life in Parkinson’s disease. Mov. Disord. 2009, 24, 1641–1649. [Google Scholar] [CrossRef]
- Huber, J.E.; Darling, M. Effect of Parkinson’s disease on the production of structured and unstructured speaking tasks: Respiratory physiologic and linguistic considerations. J. Speech Lang. Hear. Res. 2011, 54, 33–46. [Google Scholar] [CrossRef]
- Bunton, K. Patterns of lung volume use during an extemporaneous speech task in persons with Parkinson’s disease. J. Commun. Disord. 2005, 38, 331–348. [Google Scholar] [CrossRef] [PubMed]
- Stegemöller, E.L.; Radig, H.; Hibbing, P.; Wingate, J.; Sapienza, C. Effects of singing on voice, respiratory control and quality of life in persons with Parkinson’s disease. Disabil. Rehabil. 2017, 39, 594–600. [Google Scholar] [CrossRef] [PubMed]
- Di Benedetto, P.; Cavazzon, M.; Mondolo, F.; Peratoner, A.; Biasutti, E. Voice and choral singing treatment: A new approach for speech and voice disorders in Parkinson’s disease. Eur J. Phys. Rehabil. Med. 2009, 45, 13–19. [Google Scholar]
- Sadagopan, N.; Huber, J.E. Effects of loudness cues on respiration in individuals with Parkinson’s disease. Mov. Disord. 2007, 22, 651–659. [Google Scholar] [CrossRef] [PubMed]
- Pitts, T.; Bolser, D.; Rosenbek, J.; Troche, M.; Okun, M.S.; Sapienza, C. Impact of expiratory muscle strength training on voluntary cough and swallow function in Parkinson disease. Chest 2009, 135, 1301–1308. [Google Scholar] [CrossRef] [PubMed]
- Troche, M.S.; Okun, M.S.; Rosenbek, J.C.; Musson, N.; Fernandez, H.H.; Rodriguez, R.; Romrell, J.; Pitts, T.; Wheeler-Hegland, K.M.; Sapienza, C.M. Aspiration and swallowing in Parkinson disease and rehabilitation with EMST: A randomized trial. Am. Acad. Neurol. 2010, 75, 1912–1919. [Google Scholar] [CrossRef]
- Suttrup, I.; Warnecke, T. Dysphagia in Parkinson’s Disease. Dysphagia 2015, 31, 24–32. [Google Scholar] [CrossRef]
- Motolese, F.; Gupta, D.; Marano, M. Excessive daytime sleepiness and dysphagia in Parkinson’s disease, from the assessment of a risk to a pathophysiological landscape. J. Neurol. Sci. 2020, 413, 116882. [Google Scholar] [CrossRef]
- Marano, M.; Gupta, D.; Motolese, F.; Rossi, M.; Luccarelli, V.; Altamura, C.; Di Lazzaro, V. Excessive daytime sleepiness is associated to the development of swallowing impairment in a cohort of early stage drug naïve Parkinson’s disease patients. J. Neurol. Sci. 2020, 410, 116626. [Google Scholar] [CrossRef]
- Nóbrega, A.C.; Rodrigues, B.; Melo, A. Silent aspiration in Parkinson’s disease patients with diurnal sialorrhea. Clin. Neurol Neurosurg. 2008, 110, 117–119. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, B.; Nóbrega, A.C.; Sampaio, M.; Argolo, N.; Melo, A. Silent saliva aspiration in Parkinson’s disease. Mov. Disord. 2011, 26, 138–141. [Google Scholar] [CrossRef] [PubMed]
- Müller, J.; Wenning, G.K.; Verny, M.; McKee, A.; Chaudhuri, K.R.; Jellinger, K.; Poewe, W.; Litvan, I. Progression of dysarthria and dysphagia in postmortem-confirmed Parkinsonian disorders. Arch. Neurol. 2001, 58, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Kalf, J.G.; Munneke, M.; van den Engel-Hoek, L.; de Swart, B.J.; Borm, G.F.; Bloem, B.R.; Zwarts, M.J. Pathophysiology of diurnal drooling in Parkinson’s disesase. Mov. Disord. 2011, 26, 1670–1676. [Google Scholar] [CrossRef] [PubMed]
- Gaeckle, M.; Domahs, F.; Kartmann, A.; Tomandl, B.; Frank, U. Predictors of Penetration-Aspiration in Parkinson’s Disease Patients with Dysphagia: A Retrospective Analysis. Ann. Otol. Rhinol. Laryngol. 2019, 128, 728–735. [Google Scholar] [CrossRef]
- Gros, P.; Mery, V.P.; Lafontaine, A.L.; Robinson, A.; Benedetti, A.; Kimoff, R.J.; Kaminska, M. Obstructive sleep apnea in Parkinson’s disease patients: Effect of Sinemet CR taken at bedtime. Sleep Breath. 2016, 20, 205–212. [Google Scholar] [CrossRef]
- Taylor, J.M.; Main, B.S.; Crack, P.J. Neuroinflammation and oxidative stress: Co- conspirators in pathology of Parkinson’s disease. Neurochem. Int. 2013, 62, 803–819. [Google Scholar] [CrossRef]
- Olanow, C.W. The pathogenesis of cell death in Parkinson’s disease. Mov. Disord. 2007, 22, S335.e42. [Google Scholar] [CrossRef]
- Davies, C.R.; Harrington, J.J. Impact of obstructive sleep apnea on neurocognitive function and impact of continuous positive air pressure. Sleep Med. Clin. 2016, 11, 287–298. [Google Scholar] [CrossRef]
- Jones, B.E. Paradoxical sleep and its chemical/structural substrates in the brain. Neuroscience 1991, 40, 637–656. [Google Scholar] [CrossRef]
- Ferini-Strambi, L.; Baietto, C.; Di Gioia, M.R.; Castaldi, P.; Castronovo, C.; Zucconi, M.; Cappa, S.F. Cognitive dysfunction in patients with obstructive sleep apnea (OSA): Partial reversibility after continuous positive airway pressure (CPAP). Brain Res. Bull. 2003, 61, 87–92. [Google Scholar] [CrossRef]
- Mery, V.P.; Gros, P.; Lafontaine, A.L.; Robinson, A.; Benedetti, A.; Kimoff, R.J.; Kaminska, M. Reduced cognitive function in patients with Parkinson disease and obstructive sleep apnea. Neurology 2017, 88, 1120–1128. [Google Scholar] [CrossRef]
- Kaminska, M.; Mery, V.P.; Lafontaine, A.L.; Robinson, A.; Benedetti, A.; Gros, P.; Kimoff, R.J. Change in cognition and other non-motor symptoms with obstructive sleep apnea treatment in Parkinson disease. J. Clin. Sleep Med. 2018, 14, 819–828. [Google Scholar] [CrossRef]
- Tambasco, N.; Murgia, N.; Nigro, P.; Paoletti, F.P.; Romoli, M.; Brahimi, E.; Filidei, M.; Simoni, S.; Muzi, G.; Calabresi, P. Levodopa-responsive breathing discomfort in Parkinson’s disease patients. J. Neural Transm 2018, 125, 1033–1036. [Google Scholar] [CrossRef] [PubMed]
- Baille, G.; Perez, T.; Devos, D.; Deken, V.; Defebvre, L.; Moreau, C. Early occurrence of inspiratory muscle weakness in Parkinson’s disease. PLoS ONE 2018, 13, e0190400. [Google Scholar] [CrossRef]
- Bhatt, M.H.; Keenan, S.P.; Fleetham, J.A.; Calne, D.B. Pleuropulmonary disease associated with dopamine agonist therapy. Ann. Neurol. 1991, 30, 613–616. [Google Scholar] [CrossRef] [PubMed]
- Weiner, W.J.; Goetz, C.G.; Nausieda, P.A.; Klawans, H.L. Respiratory dyskinesias: Extrapyramidal dysfunction and dyspnea. Ann. Intern. Med. 1978, 88, 327–331. [Google Scholar] [CrossRef]
- Ko, P.W.; Kang, K.; Lee, H.W. Levodopa-induced respiratory dysfunction confirmed by levodopa challenge test: A case report. Medicine 2018, 97, e12488. [Google Scholar] [CrossRef]
- Lim, A.; Leow, L.; Huckabee, M.L.; Frampton, C.; Anderson, T. A pilot study of respiration and swallowing integration in Parkinson’s disease: “on” and “off” levodopa. Dysphagia 2008, 23, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Fink, M.; Klebanoff, L.; Lennihan, L.; Fahn, S. Acute respiratory failure during drug manipulation in patients with Parkinson disease. Neurology 1989, 39, 578. [Google Scholar]
- Riley, D.E.; Grossman, G.; Martin, L. Acute respiratory failure from dopamine agonist withdrawal. Neurology 1992, 42, 1843–1844. [Google Scholar] [CrossRef] [PubMed]
- de Bruin, P.F.; de Bruin, V.M.; Lees, A.J.; Pride, N.B. Effects of treatment on airway dynamics and respiratory muscle strength in Parkinson’s disease. Am. Rev. Respir. Dis. 1993, 148, 1576–1580. [Google Scholar] [CrossRef] [PubMed]
- Wei, L.; Chen, Y. Neuroleptic malignant-like syndrome with a slight elevation of creatine-kinase levels and respiratory failure in a patient with Parkinson’s disease. Patient Prefer. Adherence 2014, 8, 271–273. [Google Scholar] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Docu Axelerad, A.; Stroe, A.Z.; Arghir, O.C.; Docu Axelerad, D.; Gogu, A.E. Respiratory Dysfunctions in Parkinson’s Disease Patients. Brain Sci. 2021, 11, 595. https://doi.org/10.3390/brainsci11050595
Docu Axelerad A, Stroe AZ, Arghir OC, Docu Axelerad D, Gogu AE. Respiratory Dysfunctions in Parkinson’s Disease Patients. Brain Sciences. 2021; 11(5):595. https://doi.org/10.3390/brainsci11050595
Chicago/Turabian StyleDocu Axelerad, Any, Alina Zorina Stroe, Oana Cristina Arghir, Daniel Docu Axelerad, and Anca Elena Gogu. 2021. "Respiratory Dysfunctions in Parkinson’s Disease Patients" Brain Sciences 11, no. 5: 595. https://doi.org/10.3390/brainsci11050595
APA StyleDocu Axelerad, A., Stroe, A. Z., Arghir, O. C., Docu Axelerad, D., & Gogu, A. E. (2021). Respiratory Dysfunctions in Parkinson’s Disease Patients. Brain Sciences, 11(5), 595. https://doi.org/10.3390/brainsci11050595







