Synaptic Vesicle Protein 2A Expression in Glutamatergic Terminals Is Associated with the Response to Levetiracetam Treatment
Abstract
1. Introduction
2. Methods
2.1. Animals
2.2. Groups
2.3. Induction of SE and Post-SE Care
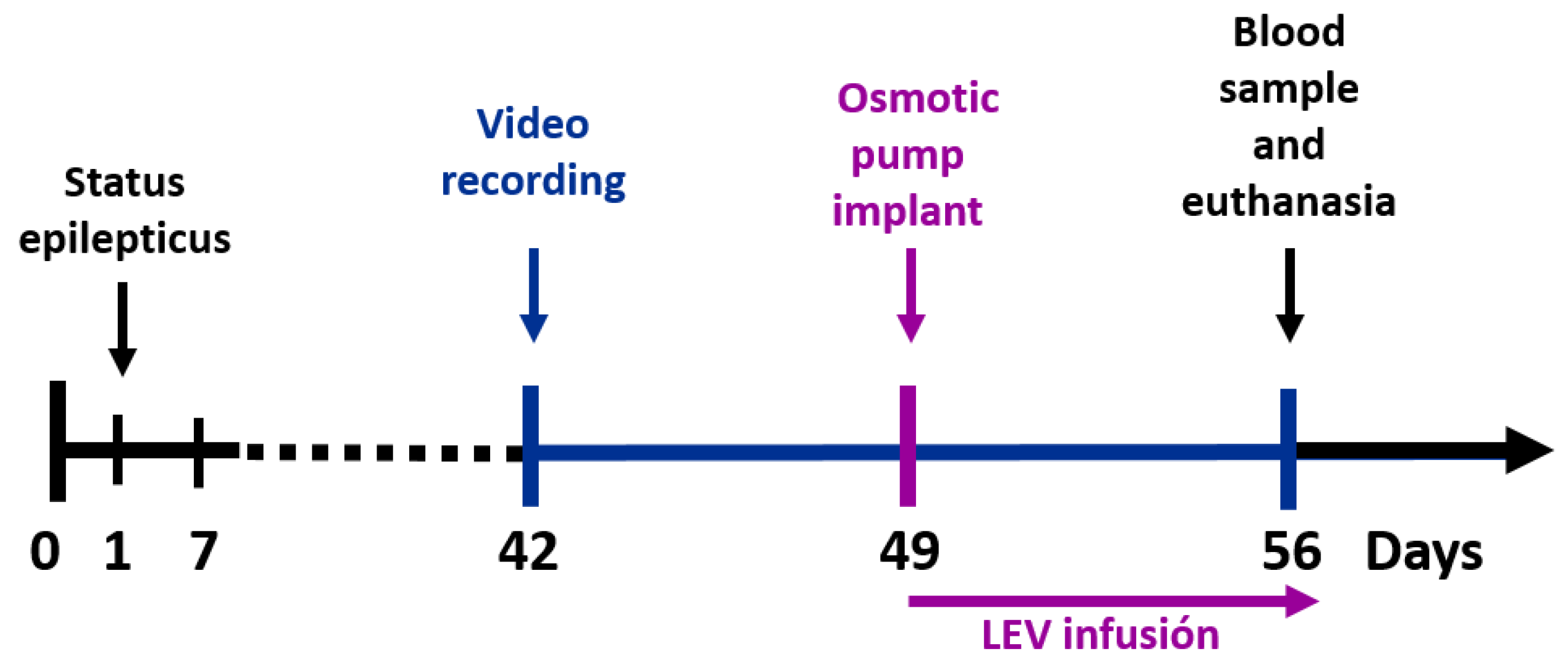
2.4. Behavioral Video-Monitoring of Seizures
2.5. Levetiracetam Treatment
2.6. Tissue Sample Collection and Processing
2.7. Immunohistochemistry and Triple Immunofluorescence
2.8. SV2A Immunoreactive Measurement
2.9. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Acknowledgments
Conflicts of Interest
References
- Lynch, B.A.; Lambeng, N.; Nocka, K.; Kensel-Hammes, P.; Bajjalieh, S.M.; Matagne, A.; Fuks, B. The synaptic vesicle protein SV2A is the binding site for the antiepileptic drug levetiracetam. Proc. Natl. Acad. Sci. USA 2004, 101, 9861–9866. [Google Scholar] [CrossRef]
- Mendoza-Torreblanca, J.G.; Vanoye-Carlo, A.; Phillips-Farfán, B.V.; Carmona-Aparicio, L.; Gómez-Lira, G. Synaptic vesicle protein 2A: Basic facts and role in synaptic function. Eur. J. Neurosci. 2013, 38, 3529–3539. [Google Scholar] [CrossRef]
- Pichardo, L.A.; Contreras, I.J.; Zamudio, S.R.; Mixcoha, E.; Mendoza, J.G. Synaptic Vesicle Protein 2A as a novel pharma-cological target with broad potential for new antiepileptic drugs. In Antiepileptic Drug Discovery: Novel Approaches, Methods in Pharmacology and Toxicology; Talevi, A., Rocha, L., Eds.; Springer: Berlin, Germany, 2016; pp. 53–65. [Google Scholar]
- Custer, K.L.; Austin, N.S.; Sullivan, J.M.; Bajjalieh, S.M. Synaptic Vesicle Protein 2 Enhances Release Probability at Quiescent Synapses. J. Neurosci. 2006, 26, 1303–1313. [Google Scholar] [CrossRef]
- Janz, R.; Goda, Y.; Geppert, M.; Missler, M.; Südhof, T.C. SV2A and SV2B Function as Redundant Ca2+ Regulators in Neurotransmitter Release. Neuron 1999, 24, 1003–1016. [Google Scholar] [CrossRef]
- Nowack, A.; Yao, J.; Custer, K.L.; Bajjalieh, S.M. SV2 regulates neurotransmitter release via multiple mechanisms. Am. J. Physiol. Physiol. 2010, 299, C960–C967. [Google Scholar] [CrossRef]
- Yao, J.; Nowack, A.; Kensel-Hammes, P.; Gardner, R.G.; Bajjalieh, S.M. Cotrafficking of SV2 and synaptotagmin at the synapse. J. Neurosci. 2010, 30, 5569–5578. [Google Scholar] [CrossRef] [PubMed]
- Bartholome, O.; Ackerveken, P.V.D.; Gil, J.S.; Bonardeaux, O.D.L.B.; Leprince, P.; Franzen, R.; Rogister, B. Puzzling out synaptic vesicle 2 family members functions. Front. Mol. Neurosci. 2017, 10, 148. [Google Scholar] [CrossRef]
- Crowder, K.M.; Gunther, J.M.; Jones, T.A.; Hale, B.D.; Zhang, H.Z.; Peterson, M.R.; Scheller, R.H.; Chavkin, C.; Bajjalieh, S.M. Abnormal neurotransmission in mice lacking synaptic vesicle protein 2A (SV2A). Proc. Natl. Acad. Sci. USA 1999, 96, 15268–15273. [Google Scholar] [CrossRef]
- Kaminski, R.M.; Gillard, M.; Leclercq, K.; Hanon, E.; Lorent, G.; Dassesse, D.; Matagne, A.; Klitgaard, H. Proepileptic phenotype of SV2A-deficient mice is associated with reduced anticonvulsant efficacy of levetiracetam. Epilepsia 2009, 50, 1729–1740. [Google Scholar] [CrossRef] [PubMed]
- Serajee, F.J.; Huq, A.M. Homozygous mutation in synaptic vesicle glycoprotein 2A gene results in intractable epilepsy, involuntary movements, microcephaly, and developmental and growth retardation. Pediatr. Neurol. 2015, 52, 642–646.e1. [Google Scholar] [CrossRef]
- Tokudome, K.; Okumura, T.; Terada, R.; Shimizu, S.; Kunisawa, N.; Mashimo, T.; Serikawa, T.; Sasa, M.; Ohno, Y. A missense mutation of the gene encoding synaptic vesicle glycoprotein 2a (sv2a) confers seizure susceptibility by disrupting amygdalar synaptic Gaba release. Front. Pharmacol. 2016, 7. [Google Scholar] [CrossRef]
- Löscher, W.; Gillard, M.; Sands, Z.A.; Kaminski, R.M.; Klitgaard, H. synaptic vesicle glycoprotein 2a ligands in the treatment of epilepsy and beyond. CNS Drugs 2016, 30, 1055–1077. [Google Scholar] [CrossRef] [PubMed]
- Klein, P.; Friedman, A.; Hameed, M.Q.; Kaminski, R.M.; Bar-Klein, G.; Klitgaard, H.; Koepp, M.; Jozwiak, S.; Prince, D.A.; Rotenberg, A.; et al. Repurposed molecules for antiepileptogenesis: Missing an opportunity to prevent epilepsy? Epilepsia 2020, 61, 359–386. [Google Scholar] [CrossRef]
- Bajjalieh, S.; Frantz, G.; Weimann, J.; McConnell, S.; Scheller, R. Differential expression of synaptic vesicle protein 2 (SV2) isoforms. J. Neurosci. 1994, 14, 5223–5235. [Google Scholar] [CrossRef] [PubMed]
- Grønborg, M.; Pavlos, N.J.; Brunk, I.; Chua, J.J.E.; Münster-Wandowski, A.; Riedel, D.; Ahnert-Hilger, G.; Urlaub, H.; Jahn, R. Quantitative comparison of glutamatergic and gabaergic synaptic vesicles unveils selectivity for few proteins including mal2, a novel synaptic vesicle protein. J. Neurosci. 2010, 30, 2–12. [Google Scholar] [CrossRef]
- Mendoza-Torreblanca, J.G.; García-Cruz, M.E.; Sánchez-Cruz, I.; Gomez-Gonzalez, B.; Juárez-Méndez, S.; Gómez-Lira, G. Analysis of differential expression of synaptic vesicle protein 2A in the adult rat brain. Neuroscience 2019, 419, 108–120. [Google Scholar] [CrossRef]
- Van Vliet, E.A.; Aronica, E.; Redeker, S.; Boer, K.; Gorter, J.A. Decreased expression of synaptic vesicle protein 2A, the binding site for levetiracetam, during epileptogenesis and chronic epilepsy. Epilepsia 2009, 50, 422–433. [Google Scholar] [CrossRef]
- Feng, G.; Xiao, F.; Lu, Y.; Huang, Z.; Yuan, J.; Xiao, Z.; Xi, Z.; Wang, X. Down-regulation synaptic vesicle protein 2A in the anterior temporal neocortex of patients with intractable epilepsy. J. Mol. Neurosci. 2009, 39, 354–359. [Google Scholar] [CrossRef]
- Crèvecœur, J.; Kaminski, R.M.; Rogister, B.; Foerch, P.; Vandenplas, C.; Neveux, M.; Mazzuferi, M.; Kroonen, J.; Poulet, C.; Martin, D.; et al. Expression pattern of synaptic vesicle protein 2 (SV2) isoforms in patients with temporal lobe epilepsy and hippocampal sclerosis. Neuropathol. Appl. Neurobiol. 2014, 40, 191–204. [Google Scholar] [CrossRef]
- Toering, S.T.; Boer, K.; De Groot, M.; Troost, D.; Heimans, J.J.; Spliet, W.G.M.; Van Rijen, P.C.; Jansen, F.E.; Gorter, J.A.; Reijneveld, J.C.; et al. Expression patterns of synaptic vesicle protein 2A in focal cortical dysplasia and TSC-cortical tubers. Epilepsia 2009, 50, 1409–1418. [Google Scholar] [CrossRef]
- Hanaya, R.; Hosoyama, H.; Sugata, S.; Tokudome, M.; Hirano, H.; Tokimura, H.; Kurisu, K.; Serikawa, T.; Sasa, M.; Arita, K. Low distribution of synaptic vesicle protein 2A and synaptotagimin-1 in the cerebral cortex and hippocampus of spontaneously epileptic rats exhibiting both tonic convulsion and absence seizure. Neuroscience 2012, 221, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Matveeva, E.A.; Vanaman, T.C.; Whiteheart, S.W.; Slevin, J.T. Asymmetric accumulation of hippocampal 7S SNARE complexes occurs regardless of kindling paradigm. Epilepsy Res. 2007, 73, 266–274. [Google Scholar] [CrossRef][Green Version]
- Matveeva, E.A.; Vanaman, T.C.; Whiteheart, S.W.; Slevin, J.T. Levetiracetam prevents kindling-induced asymmetric accumulation of hippocampal 7S SNARE complexes. Epilepsia 2008, 49, 1749–1758. [Google Scholar] [CrossRef]
- Contreras-García, I.J.; Pichardo-Macías, L.A.; Santana-Gómez, C.E.; Sánchez-Huerta, K.; Ramírez-Hernández, R.; Gómez-González, B.; Rocha, L.; Torreblanca, J.G.M. Differential expression of synaptic vesicle protein 2A after status epilepticus and during epilepsy in a lithium-pilocarpine model. Epilepsy Behav. 2018, 88, 283–294. [Google Scholar] [CrossRef]
- De Groot, M.; Aronica, E.; Heimans, J.J.; Reijneveld, J.C. Synaptic vesicle protein 2A predicts response to levetiracetam in patients with glioma. Neurology 2011, 77, 532–539. [Google Scholar] [CrossRef] [PubMed]
- Grimminger, T.; Pernhorst, K.; Surges, R.; Niehusmann, P.; Priebe, L.; Von Lehe, M.; Hoffmann, P.; Cichon, S.; Schoch, S.; Becker, A.J. Levetiracetam resistance: Synaptic signatures & corresponding promoter SNPs in epileptic hippocampi. Neurobiol. Dis. 2013, 60, 115–125. [Google Scholar] [CrossRef] [PubMed]
- Ohno, Y.; Tokudome, K. Therapeutic role of synaptic vesicle glycoprotein 2A (SV2A) in modulating epileptogenesis. CNS Neurol. Disord.-Drug Targets 2017, 16. [Google Scholar] [CrossRef]
- Vanoye-Carlo, A.; Gómez-Lira, G. Differential expression of SV2A in hippocampal glutamatergic and GABAergic terminals during postnatal development. Brain Res. 2019, 1715, 73–83. [Google Scholar] [CrossRef]
- Ohno, Y.; Ishihara, S.; Terada, R.; Kikuta, M.; Sofue, N.; Kawai, Y.; Serikawa, T.; Sasa, M. Preferential increase in the hippocampal synaptic vesicle protein 2A (SV2A) by pentylenetetrazole kindling. Biochem. Biophys. Res. Commun. 2009, 390, 415–420. [Google Scholar] [CrossRef]
- Ohno, Y.; Okumura, T.; Terada, R.; Ishihara, S.; Serikawa, T.; Sasa, M. Kindling-associated SV2A expression in hilar GABAergic interneurons of the mouse dentate gyrus. Neurosci. Lett. 2012, 510, 93–98. [Google Scholar] [CrossRef]
- Tokudome, K.; Okumura, T.; Shimizu, S.; Mashimo, T.; Takizawa, A.; Serikawa, T.; Terada, R.; Ishihara, S.; Kunisawa, N.; Sasa, M.; et al. Synaptic vesicle glycoprotein 2A (SV2A) regulates kindling epileptogenesis via GABAergic neurotransmission. Sci. Rep. 2016, 6, 27420. [Google Scholar] [CrossRef]
- Venkatesan, K.; Alix, P.; Marquet, A.; Doupagne, M.; Niespodziany, I.; Rogister, B.; Seutin, V. Altered balance between excitatory and inhibitory inputs onto CA1 pyramidal neurons from SV2A-deficient but not SV2B-deficient mice. J. Neurosci. Res. 2012, 90, 2317–2327. [Google Scholar] [CrossRef] [PubMed]
- Pichardo-Macías, L.A.; Ramírez-Mendiola, B.A.; Contreras-García, I.J.; Zamudio-Hernández, S.R.; Chávez-Pacheco, J.L.; Sánchez-Huerta, K.B.; Mendoza-Torreblanca, J.G. Effect of levetiracetam on extracellular amino acid levels in the dorsal hippocampus of rats with temporal lobe epilepsy. Epilepsy Res. 2018, 140, 111–119. [Google Scholar] [CrossRef]
- Glien, M.; Brandt, C.; Potschka, H.; Löscher, W. Effects of the novel antiepileptic drug levetiracetam on spontaneous recurrent seizures in the rat pilocarpine model of temporal lobe epilepsy. Epilepsia 2002, 43, 350–357. [Google Scholar] [CrossRef] [PubMed]
- Racine, R.J. Modification of seizure activity by electrical stimulation: II. Motor seizure. Electroencephalogr. Clin. Neurophysiol. 1972, 32, 281–294. [Google Scholar] [CrossRef]
- Arida, R.M.; Scorza, F.A.; Peres, C.D.A.; Cavalheiro, E.A. The course of untreated seizures in the pilocarpine model of epilepsy. Epilepsy Res. 1999, 34, 99–107. [Google Scholar] [CrossRef]
- Olah, E.; Bacsói, G.; Fekete, J.; Sharma, V.K. Determination of ng/mL levetiracetam using ultra-high-performance liquid chromatography-photodiode absorbance. J. Chromatogr. Sci. 2012, 50, 253–258. [Google Scholar] [CrossRef]
- Surges, R.; Volynski, K.E.; Walker, M.C. Review: Is levetiracetam different from other antiepileptic drugs? Levetiracetam and its cellular mechanism of action in epilepsy revisited. Ther. Adv. Neurol. Disord. 2008, 1, 13–24. [Google Scholar] [CrossRef]
- Lyseng-Williamson, K.A. Levetiracetam: A review of its use in epilepsy. Drugs 2011, 71, 489–514. [Google Scholar] [PubMed]
- Klitgaard, H.; Matagne, A.; Gobert, J.; Wülfert, E. Evidence for a unique profile of levetiracetam in rodent models of seizures and epilepsy. Eur. J. Pharmacol. 1998, 353, 191–206. [Google Scholar] [CrossRef]
- Kaminski, R.M.; Gillard, M.; Klitgaard, H. Targeting SV2A for discovery of antiepileptic drugs. In Jasper’s Basic Mechanisms of the Epilepsies, 4th ed.; Noebels, J.L., Avoli, M., Rogawski, M.A., Olsen, R.W., Delgado-Escueta, A.V., Eds.; National Center for Biotechnology Information: Bethesda, MD, USA, 2012; Available online: http://www.ncbi.nlm.nih.gov/books/NBK98183/ (accessed on 16 November 2020).
- Loewen, B.J.L.; Barker-Haliski, M.L.; Dahle, M.E.J.; White, H.S.; Wilcox, K.S. Neuronal injury, gliosis, and glial proliferation in two models of temporal lobe epilepsy. J. Neuropathol. Exp. Neurol. 2016, 75, 366–378. [Google Scholar] [CrossRef]
- Ambrogini, P.; Torquato, P.; Bartolini, D.; Albertini, M.C.; Lattanzi, D.; Di Palma, M.; Marinelli, R.; Betti, M.; Minelli, A.; Cuppini, R.; et al. Excitotoxicity, neuroinflammation and oxidant stress as molecular bases of epileptogenesis and epilepsy-derived neurodegeneration: The role of vitamin E. Biochim. et Biophys. Acta (BBA)-Mol. Basis Dis. 2019, 1865, 1098–1112. [Google Scholar] [CrossRef]
- Pitkänen, A.; Sutula, T.P. Is epilepsy a progressive disorder? Prospects for new therapeutic approaches in temporal-lobe epilepsy. Lancet Neurol. 2002, 1, 173–181. [Google Scholar] [CrossRef]
- Farrell, J.S.; Wolff, M.D.; Teskey, G.C. Neurodegeneration and pathology in epilepsy: Clinical and basic perspectives. Neurodegenerative Dis. 2017, 15, 317–334. [Google Scholar] [CrossRef]
- Ma, D.L.; Tang, Y.C.; Chen, P.M.; Chia, S.C.; Jiang, F.L.; Burgunder, J.-M.; Lee, W.L.; Tang, F.R. Reorganization of CA3 area of the mouse hippocampus after pilocarpine induced temporal lobe epilepsy with special reference to the CA3-septum pathway. J. Neurosci. Res. 2005, 83, 318–331. [Google Scholar] [CrossRef]
- Nowack, A.; Malarkey, E.B.; Yao, J.; Bleckert, A.; Hill, J.; Bajjalieh, S.M. Levetiracetam reverses synaptic deficits produced by overexpression of SV2A. PLoS ONE 2011, 6, e29560. [Google Scholar] [CrossRef]
- Meldrum, B.S. Excitotoxicity and selective neuronal loss in epilepsy. Brain Pathol. 1993, 3, 405–412. [Google Scholar] [CrossRef]
- Scorza, F.A.; Arida, R.M.; Naffah-Mazzacoratti, M.D.G.; Scerni, D.A.; Calderazzo, L.; Cavalheiro, E.A. The pilocarpine model of epilepsy: What have we learned? An. da Acad. Bras. de Ciências 2009, 81, 345–365. [Google Scholar] [CrossRef]
- Meehan, A.L.; Yang, X.; McAdams, B.D.; Yuan, L.; Rothman, S.M. A new mechanism for antiepileptic drug action: Vesicular entry may mediate the effects of levetiracetam. J. Neurophysiol. 2011, 106, 1227–1239. [Google Scholar] [CrossRef] [PubMed]
- Harvey, B.D.; Sloviter, R.S. Hippocampal granule cell activity and c-Fos expression during spontaneous seizures in awake, chronically epileptic, pilocarpine-treated rats: Implications for hippocampal epileptogenesis. J. Comp. Neurol. 2005, 488, 442–463. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, A.H.; Joseph, S.A. CA3 axonal sprouting in kainate-induced chronic epilepsy. Brain Res. 2005, 1066, 129–146. [Google Scholar] [CrossRef] [PubMed]
- Correa-Basurto, J.; Cuevas-Hernández, R.I.; Phillips-Farfán, B.V.; Martínez-Archundia, M.; Romo-Mancillas, A.; Ramírez-Salinas, G.L.; Pérez-González, Ó.A.; Trujillo-Ferrara, J.; Mendoza-Torreblanca, J.G. Identification of the antiepileptic racetam binding site in the synaptic vesicle protein 2A by molecular dynamics and docking simulations. Front. Cell. Neurosci. 2015, 9. [Google Scholar] [CrossRef] [PubMed]




| Group | Sample Size (n) | SE Induced | Osmotic Pump Implanted |
|---|---|---|---|
| Control C | 6 | NO | NO |
| Control + Levetiracetam C+LEV | 7 | NO | YES |
| Epileptic EPI | 6 | YES | NO |
| Responders R | 7 | YES | YES |
| Non-responders NR | 5 | YES | YES |
| Group | Pretreatment | During LEV Treatment |
|---|---|---|
| R | 5.0 (3.0–7.0) | 0.0 + (0.0–1.0) |
| NR | 4.0 (2.5–28.5) | 4.0 ** (2.5–16.5) |
| Group | Serum Levetiracetam Day 56 (µg/mL) |
|---|---|
| C+LEV | 59.74 ± 14.49 (36.5–75.6) |
| R | 44.89 ± 14.06 (32–66.3) |
| NR | 49.52 ± 18.56 (36.6–76.7) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Contreras-García, I.J.; Gómez-Lira, G.; Phillips-Farfán, B.V.; Pichardo-Macías, L.A.; García-Cruz, M.E.; Chávez-Pacheco, J.L.; Mendoza-Torreblanca, J.G. Synaptic Vesicle Protein 2A Expression in Glutamatergic Terminals Is Associated with the Response to Levetiracetam Treatment. Brain Sci. 2021, 11, 531. https://doi.org/10.3390/brainsci11050531
Contreras-García IJ, Gómez-Lira G, Phillips-Farfán BV, Pichardo-Macías LA, García-Cruz ME, Chávez-Pacheco JL, Mendoza-Torreblanca JG. Synaptic Vesicle Protein 2A Expression in Glutamatergic Terminals Is Associated with the Response to Levetiracetam Treatment. Brain Sciences. 2021; 11(5):531. https://doi.org/10.3390/brainsci11050531
Chicago/Turabian StyleContreras-García, Itzel Jatziri, Gisela Gómez-Lira, Bryan Víctor Phillips-Farfán, Luz Adriana Pichardo-Macías, Mercedes Edna García-Cruz, Juan Luis Chávez-Pacheco, and Julieta G. Mendoza-Torreblanca. 2021. "Synaptic Vesicle Protein 2A Expression in Glutamatergic Terminals Is Associated with the Response to Levetiracetam Treatment" Brain Sciences 11, no. 5: 531. https://doi.org/10.3390/brainsci11050531
APA StyleContreras-García, I. J., Gómez-Lira, G., Phillips-Farfán, B. V., Pichardo-Macías, L. A., García-Cruz, M. E., Chávez-Pacheco, J. L., & Mendoza-Torreblanca, J. G. (2021). Synaptic Vesicle Protein 2A Expression in Glutamatergic Terminals Is Associated with the Response to Levetiracetam Treatment. Brain Sciences, 11(5), 531. https://doi.org/10.3390/brainsci11050531







