Abstract
Aim: Early onset of psychopathology is often an index of a more severe clinical course and worse prognosis. This review examined the course of bipolar disorder (BD) with onset in childhood and adolescence, with a focus on persistence of symptoms, severity of illness, comorbidity, and functional impairment. Methods: The databases of PubMed, Embase, and PsycInfo were systematically searched for publications since 1990 reporting on long-term (12 months or longer) assessments of patients with early onset BD. Results: Forty-two relevant publications were identified, which reported on data derived from 15 different patient cohorts, including 7 prospective research psychopathology studies, 4 medical record reviews, 2 follow-ups of clinical trial samples, 1 managed care database, and 1 nationwide registry, for a total of 10,187 patients. The length of follow-ups ranged from 1.0 to 15 years. Diagnostic stability of BD ranged from 73% to 100% over ten years. Recovery rate from an index episode was 81.5–100% and recurrence rate was 35–67%. Suicide attempt cumulative prevalence in five years was 18–20%. Earlier age at the first episode predicted a more severe clinical course. Conclusions: Early onset BD persists over time through adolescence, with homotypic diagnostic continuity over the years, but heterogeneity in the severity of the clinical course. Whether early identification and treatment improves distal prognosis remains to be further investigated.
1. Introduction
Bipolar disorder (BD) is a chronic condition and a leading cause of morbidity and mortality, being associated with reduced life expectancy primarily due to cardiovascular disease and suicide [1]. Even though effective treatments exist and extended remission is possible, BD is a lifelong condition for which a definitive cure is not yet available. Lifetime prevalence is estimated to be about 1% worldwide [2], but rates up to 2.6% have been reported [3,4]. Based on retrospective reports, the mean age of onset of BD type I (BD-I) is around 18 years [5], with a peak in the incidence of the first manic episode between 21 and 23 years [3,6]. One study identified three peaks of onset in life, at 17, 26, and 35 years, respectively [7]. Thus, when also considering that a depressive episode can precede mania as the initial manifestation, it should be noted that onset of BD in adolescence is not uncommon.
Estimates of the prevalence of early onset BD (i.e., with onset under the age of 18 years) are variable. One epidemiological study in adolescents found a prevalence of 1.1% [8]. A subsequent meta-analysis of 12 epidemiological studies yielded a lifetime prevalence up to age 21 of 1.8% (95% CI, 1.1–3.0%) [9], but rates as high as 2.5% at age 18 have been reported [10]. The apparent incongruence between adult and adolescent prevalence rates is likely due to methodological differences in ascertainment. For years, controversy surrounded the diagnosis of BD in children with regard to whether extreme chronic irritability represented a BD manifestation [11]. There is now general acceptance that one should apply to children and adolescents the same diagnostic criteria as in adults, requiring the presence of discrete episodes of persistently abnormal mood elevation for a diagnosis of BD [5,12].
Long-term follow-up studies are especially useful for understanding developmental psychiatric phenomenology and linking child to adult psychopathology. By delineating the trajectory of the disorder and documenting its evolution in time, prospective studies can clarify if and to which extent a diagnosis of early onset BD (i.e., under the age of 18 years) is predictive of adult BD. These studies also help document the impact of the disorder on highly relevant outcomes, such as educational attainment, social functioning, medical complications, suicidal behavior, and hospitalization [13,14,15,16,17]. A growing body of research suggests that early onset BD is associated with a more severe course of illness, increased risk of suicidality and comorbid psychopathology, and worse functional outcomes (e.g., academic achievement, employment, living independently, marriage, and children) [9,18,19,20]. Some recent reviews reported that the most prevalent comorbid diagnoses in early onset BD are attention-deficit hyperactivity disorder (ADHD), oppositional defiant disorder/conduct disorder, substance use disorders, and anxiety disorders [11,12]. ADHD is more common in childhood, while comorbidity in late adolescence is similar to that in adulthood, with higher rates of substance abuse and anxiety disorders [12,21]. Comorbid ADHD or anxiety have been found to be associated with more severe mood symptoms, greater functional impairment, and worse clinical course [9,18].
We conducted a systematic review of prospective follow-up studies of early onset BD with the aim of evaluating the currently available evidence for diagnostic continuity, symptom persistence, and impact on functional outcomes. We did not include studies reporting on retrospectively derived child psychopathology obtained from patients first diagnosed with BD as adults because of the risk of selection and recall biases. To our knowledge, no similar systematic review had been published. The main questions guiding this systematic review were: (1) what is the stability of BD with onset in children and adolescents? Is there a homotypic or heterotypic continuity? (2) What are the outcomes for children and adolescents with BD in terms of functional outcomes, suicidality, hospitalization, response to treatment, and comorbidity? (3) Does early onset BD have a more severe clinical course than later onset BD? (4) Does early treatment lead to a more favorable outcome in adulthood?
2. Materials and Methods
2.1. Literature Search
A systematic review of relevant publications was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [18]. A literature search was conducted electronically in three databases (PubMed, Embase, and PsycInfo) on 13 November 2020. The search terms were: “bipolar disorder” or “mania” and “child” or “adolescent” and “outcome” or “prognosis” or “course” or “longitudinal”, with a time filter for date of publication set to after 1989. The time frame was limited to the last 30 years because the diagnostic construct of bipolar disorder was previously infrequently applied to children, but has become increasingly used since the 1990s [11]. The complete search string is available in Supplementary Table S1.
2.2. Selection of Relevant Publications
After eliminating duplicate records, publication titles and abstracts were screened according to the following eligibility criteria:
Inclusion criteria: (a) peer-reviewed publications; (b) longitudinal studies of children and adolescents (up to 18 years of age) with a diagnosis of BD based on an internationally accepted definition; (c) for studies in which only some of the participants had a diagnosis of BD, the data on BD cases had to be reported separately; (d) minimum sample size of 30 patients with a diagnosis of BD; and (e) a minimum follow-up time of one year.
Exclusion criteria: (a) studies published before 1990; (b) publications in languages other than English; (c) reviews, meta-analyses, clinical trial reports, clinical case reports, editorials, commentaries, book chapters, and conference presentations.
2.3. Data Collection and Analysis
First, four reviewers (CD, IS, CC, and IF) independently evaluated the titles and abstracts of the first 300 and last 300 publications (by date of publication) that were identified with the electronic searches, with a rate of agreement of 86.2% [22] and consensus agreement on the remaining after group discussion. Then, the reviewers independently screened the remaining publications and selected the possibly relevant studies; in cases of doubt, each paper was discussed collectively among the reviewers. The full texts of the selected articles were then screened independently by two teams of two reviewers each (CC/IF and CD/IS). All papers with doubtful assignments were re-evaluated collectively to reach consensus agreement, with external supervision (BV). The data received a descriptive and qualitative analysis focused on the main questions that drove the review.
2.4. Risk-of-Bias Appraisal
The methodological quality of the included studies was assessed by three independent reviewers who reached agreement using a risk-of-bias assessment checklist (Supplementary Table S2) based on the Newcastle Ottawa Scale (NOS) for assessing the quality of non-randomized studies in meta-analyses [23]. The checklist included individual items about the study external (sample representativeness and use of validated diagnostic interviews) and internal validity (blind raters, adequate sample size, and sample retention). The risk of bias for each item was scored as low, moderate, or high. Each study was then given an overall score corresponding to the worst score received on among the item scores.
3. Results
3.1. Selected Publications
The search yielded a total of 12,750 records (Figure 1). After electronically eliminating duplicates, the titles and abstracts of the remaining 9703 records were manually screened for suitability based on the stated inclusion and exclusion criteria. Based on this review, another 624 duplicate publications were identified and therefore discarded. One article published after the bibliographic searches was added [17]. Among the remaining records, 79 were identified for possible inclusion, and their full texts were further evaluated for relevance. A total of 42 publications, reporting on 15 different patient cohorts, were eventually included in the systematic review (Table 1). The characteristics of each publication are summarized in Supplementary Table S3.
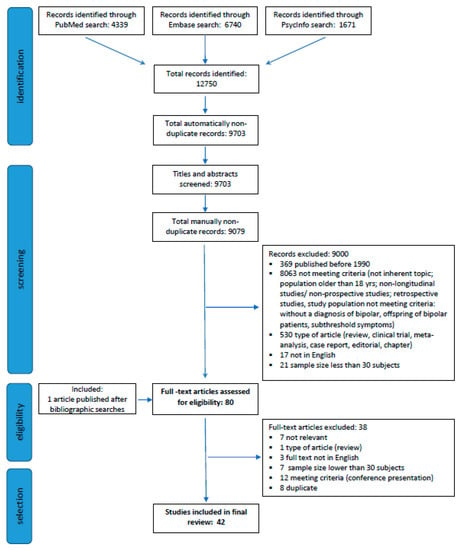
Figure 1.
Review flowchart.

Table 1.
Patient cohorts used to examine the course of bipolar disorder in children and adolescents.
According to the risk-of-bias analysis, of the 42 selected studies, three were deemed to be at low risk of bias for all the criteria and were determined to be of high quality. Twenty-six studies demonstrated moderate risk of bias in at least one of the criteria. Thirteen studies were judged to be at high risk of bias in at least one of the criteria. The most common risk of bias was lack of a blind rater, followed by lack of validated diagnostic interviews. Sample retention was very good (>80%) in most of the studies (Supplemental Table S3).
There were important differences in design and methods among the 15 identified patient cohorts. Some were samples of convenience, whose medical records had been prepared for clinical or administrative purposes and then analyzed by researchers to reconstruct the course of illness. Others were ad hoc research samples, specifically recruited for assessing psychopathology over time. Seven were prospective research assessments of patients using validated diagnostic and assessment research instruments (Table 1) [14,15,16,24,25,27,57]. Cumulatively, these cohorts included 956 patients with periods of observation between 1.0 and 12.5 years. Four cohorts were based on reviews of medical records from naturalistically treated patients, with a total of 363 patients and a period of observation between 1.5 and 15 years [29,30,53,55]. Two cohorts consisted of follow-up of clinical trial samples, for a total of 220 patients and a period of observation of two years [56,60]. One was a large managed care insurance database, which included 8129 patients and a period of observation of 1.4 years [52], and one was a nationwide population registry in Denmark, which included up to 519 patients over a 10-year period (Table 1) [59]. The large majority of the cohorts were assessed using the DSM criteria, especially DSM-IV. Only two used ICD-10 criteria [52,59] and one used the Research Diagnostic Criteria [24]. Most of the study cohorts were from the USA (11 out of 15), two were from Europe, including a nationwide registry database, and two were from India.
3.2. Diagnostic Stability
Based on medical record reviews, 95.8% of the patients retained a BD diagnosis, with all BD-I patients maintaining their diagnosis and about half of BD-NOS patients converting to BD-I [54,55]. Among patients with multiple hospitalizations, 73% had diagnostic concordance between the first and second hospitalization [30]. Among the research prospective studies, the Course and Outcome of Bipolar Youth (COBY) found substantial diagnostic continuity of BD. There were diagnostic changes but within the BD spectrum, with 25% of BD-II converting to BD-I and 38% of BD-NOS converting to BD-I or BD-II over four years [14]. Exposure to antimanic medication was associated with a lower risk of conversion to BD-I [14]. Likewise, follow-up studies of clinical trial samples reported that 24% of patients with BD-NOS converted to BD-I [57].
In the Phenomenology and Course of Pediatric Bipolar Disorders study, the BD-I diagnosis had 100% continuity over an eight-year follow-up [27]. Another research prospective study reported that 73.1% of the patients continued to meet diagnostic criteria for BD-I [16].
Analysis of the Danish population database found that the stability of the diagnosis was 86% at three years and 73% at ten years [59]. By ten years, 17% had changed diagnosis to schizophrenia. The diagnostic change was more likely in patients who were males, had been diagnosed during a hospitalization, had abused substances, were given a previous diagnosis of schizophrenia spectrum disorder, or had parents with schizophrenia spectrum disorder [59].
3.3. Course of Illness
Rates of recovery (generally defined as euthymia for at least eight consecutive weeks) from index episode between 81.5% and 100% were reported [14,15,24,25,27,29,52]. Time to recovery was reported to be 36.0 weeks (SD 25.0) in one study [26], and 20 weeks (SD 13) in another [15]. Recovery time was found to be shorter when the index episode was manic (median 8 weeks) or mixed (11 weeks) rather than depressed (26 weeks) [24]. Predictors of recovery were more prolonged lithium treatment and living in an intact biological family [26,28]. In a one-year follow-up of hospitalized adolescents with first episode BD mania, functional recovery was 39%, as compared with the 85% symptomatic recovery rate [15].
A relapse (recurrence) rate of 62.5% at 1.5 years was reported in the COBY [14], and of 73% during the eight years of the Phenomenology and Course of Pediatric Bipolar Disorders study [27]. Other studies reported relapse rates from 35% to 67% at five years [24,25,29].
The course of illness was characterized by presence of mood symptoms for most of the time [27,31]. In one study, only 6.4% were euthymic after a four-year follow-up [16]. In a medical record review on a Spanish sample, children with BD had a chronic course with little inter-episodic recovery [54]. However, in a prospective follow-up of a clinical trial sample, a substantial proportion (25–30%) of youth with bipolar I or II disorder maintained euthymic states over extended periods [60].
In COBY, four different longitudinal mood trajectories were identified with latent class analysis: “predominantly euthymic” (24.0%), “moderately euthymic” (34.6%), “ill with improving course” (19.1%), and “predominantly ill” (22.3%) [38].
Early age at onset was found to predict a more severe course of illness [13,27,31,38,54]. Other negative prognostic predictors were family history of BD or substance abuse, sexual abuse, suicidality, more severe mood symptoms, and presence of psychotic symptoms [14,38,46]. Rates of psychosis of 40% and 61% were reported [28,53]. Psychosis was associated with a more severe symptomatic course and higher rates of suicide attempt and hospitalization [46].
Social and school impairment often persisted after symptomatic recovery. In COBY, 40.5% of the patients were impaired in interpersonal functioning and 92.8% in school activities [49]. A decline in psychosocial functioning was found to precede onset of depressive episodes [49]. No decline in cognitive functioning over time was detected within the 2.5 years of follow up [42]. Lithium therapy was associated with better psychosocial functioning over a ten-year period [48]. At least three studies reported an association of better outcomes with better quality of family relationships [27,51,56].
3.4. Suicidal Behavior
In COBY, 18% of the patients made a suicide attempt during a five-year period of observation [33]. Females were more likely to attempt suicide. The suicidality risk was greater among patients with more severe depression and family history of depression [33]. A 20% rate for suicide attempts was reported in another five-year prospective research follow-up study [24]. In a medical record review, 57% of the patients were found to have suicidal ideation and/or made attempts at suicide [53].
3.5. Comorbidity
A high rate of comorbidity with attention deficit/hyperactivity disorder was documented. In COBY, 58.6% of the sample met criteria for ADHD at study entry [31]. An anxiety disorder was present in most patients, persisted in time, and was associated with more recurrences of mood episodes and less time spent in euthymia [37,39].
The course of BD was associated with a substance abuse disorder in about a third of the cases: 35% of the patients developed a substance abuse disorder by early adulthood in the Phenomenology and Course of Pediatric Bipolar Disorders study [27] and 32% in COBY [34]. In COBY, 12.2% of the patients met criteria for borderline personality disorder [40].
4. Discussion
This systematic review of studies reporting on the longitudinal course of BD in children and adolescents identified a substantial number of informative reports. The studies used different approaches, including recruitment of well-characterized research samples specifically aimed at assessing developmental psychopathology, convenience samples from clinical trials that received extensive follow-up, and reviews of naturalistically collected medical and administrative records. Considering the diversity of the studies and the heterogeneity of methods, there is a remarkable consistency in the results and convergence on several important issues.
There is evidence of diagnostic stability of BD over a period up to about ten years [55,59]. Stability was especially good within the BD spectrum, with a tendency for BD-NOS to convert to BD-I [14,32,55]. Overall, the reports document an episodic and recurrent chronic course of illness, with recovery from index episode but frequent recurrence, and the presence of mood symptoms for most of time [14,27]. There is also evidence of heterogeneity in the severity of the course of illness at the individual patient level. In COBY, about one-fourth of the patients remained predominantly euthymic (i.e., most of the time had a euthymic mood) and another one-third were euthymic about half of the time [38]. On this point, however, not all the studies were concordant, with one study reporting that a large majority of the patients remained with clinically significant mood symptoms at the end of a four-year follow-up [16]. These differences in findings likely reflect heterogeneity in sample recruitment across the studies.
The high comorbidity with ADHD, anxiety, and substance abuse was also consistently documented [27,31,37,39], as well as the significant impairment in psychosocial and school functioning, despite stable cognitive functioning [42]. The persistence of mood symptoms, even at sub-syndromic levels, was associated with functional impairment [16].
The data also documented the high rate of suicidal behavior in youth with BD. A suicide attempt incidence of 14.7% over 3.5 years among child and adolescent BD patients [64] was reported, and a rate of 18–20% over a five-year period of observation [24,33]. This is consistent overall with the increased suicidal risk in adults with BD [1]. Consistent with the epidemiology of suicide attempt in the general population [65], in early onset BD the suicide attempt rate was also higher among female patients and associated with the presence and severity of depression [33].
Finally, the relevance of the psychosocial context to the course of BD emerged from several studies. Thus, improvement was faster in children living in low-conflict families, low maternal warmth was associated with higher risk of relapse [27,56], and suicidal risk was greater if the quality of family relationships was poor [51].
While the level of information provided by these reports is considerable, there are a number of limitations that leave important issues unaddressed. First, even if the continuity of mania/hypomania in adolescence into early adulthood is well-documented, no study extended beyond early adulthood. In particular, the course of early onset BD in adulthood remains unexplored with respect to social and occupational functioning. Second, although there are some indications that lithium may have beneficial effect by shortening time to recovery, reducing suicidality, and improving functioning [28,48], and that antimanic medication may decrease risk of recurrence [14], little information is available on the possible impact of early treatment on the long-term psychopathological trajectory of the disorder. The report that 28% of the patients relapsed despite being on apparently adequate doses of lithium is difficult to interpret without a comparison group [29]. Finally, given that most of the studies were conducted in the USA, there is a need for more research on clinical samples from other socio-cultural contexts.
Our review has several limitations. Only publications since 1990 were considered; however, the diagnosis of BD was infrequently applied to children and adolescents until the 1990s. The initial screening of the titles and abstracts of the publications identified by the electronic searches was conducted by multiple reviewers only for a sample of 600 publications (7% of the total), while the remaining publications were screened by just one reviewer. This might have resulted in missing relevant publications. However, the four reviewers achieved good agreement during their group reviews.
5. Conclusions
In conclusion, across a variety of studies, diverse for sample selection and assessment methods, there was evidence of substantial homotypic diagnostic continuity of early onset BD from adolescence into early adulthood, but with heterogeneity in the severity of the clinical course and still limited information about the distal impact of the disorder and its treatment on functional outcomes in adulthood.
Supplementary Materials
The following are available online at https://www.mdpi.com/2076-3425/11/3/341/s1. Table S1: Complete search string. Table S2: Risk of bias evaluation. Table S3: Publications used to examine the course of bipolar disorder in children and adolescents.
Funding
This research received no external funding.
Acknowledgments
We thank Paolo Gardois and Nicoletta Colombi for their help with the bibliographic search. We also thank Daniele Marcotulli for statistical support and Marco Guerra for his help with reference editing.
Conflicts of Interest
In the last two years, BV has received consultant fees or honoraria from Medice, Lundbeck, and Angelini Pharmaceuticals, and from law firms Goodwin Procter and Haynes and Boone.
References
- McIntyre, R.S.; Berk, M.; Brietzke, E.; I Goldstein, B.; López-Jaramillo, C.; Kessing, L.V.; Malhi, G.S.; A Nierenberg, A.; Rosenblat, J.D.; Majeed, A.; et al. Bipolar disorders. Lancet 2020, 396, 1841–1856. [Google Scholar] [CrossRef]
- Moreira, A.L.R.; Van Meter, A.; Genzlinger, J.; Youngstrom, E.A. Review and meta-analysis of epidemiologic studies of adult bipolar disorder. J. Clin. Psychiatry 2017, 78, e1259–e1269. [Google Scholar] [CrossRef]
- Kessler, R.C.; Chiu, W.T.; Demler, O.; Walters, E.E. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch. Gen. Psychiatry 2005, 62, 617–627. [Google Scholar] [CrossRef] [PubMed]
- Merikangas, K.R.; Jin, R.; He, J.-P.; Kessler, R.C.; Lee, S.; Sampson, N.A.; Viana, M.C.; Andrade, L.H.; Hu, C.; Karam, E.G.; et al. Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Arch. Gen. Psychiatry 2011, 68, 241–251. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Kennedy, N.; Everitt, B.; Boydell, J.; Van Os, J.; Jones, P.B.; Murray, R.M. Incidence and distribution of first-episode mania by age: Results from a 35-year study. Psychol. Med. 2005, 35, 855–863. [Google Scholar] [CrossRef]
- Lin, P.-I.; McInnis, M.G.; Potash, J.B.; Willour, V.; MacKinnon, D.F.; DePaulo, J.R.; Zandi, P.P. Clinical correlates and familial aggregation of age at onset in bipolar disorder. Am. J. Psychiatry 2006, 163, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Lewinsohn, P.M.; Klein, D.N.; Seeley, J.R. Bipolar disorder during adolescence and young adulthood in a community sample. Bipolar Disord. 2000, 2, 281–293. [Google Scholar] [CrossRef]
- Van Meter, A.R.; Moreira, A.L.R.; Youngstrom, E.A. Meta-analysis of epidemiologic studies of pediatric bipolar disorder. J. Clin. Psychiatry 2011, 72, 1250–1256. [Google Scholar] [CrossRef]
- Merikangas, K.R.; Cui, L.; Kattan, G.; Carlson, G.A.; Youngstrom, E.A.; Angst, J. Mania with and without depression in a community sample of US adolescents. Arch. Gen. Psychiatry 2012, 69, 943–951. [Google Scholar] [CrossRef] [PubMed]
- Duffy, A.; Carlson, G.; Dubicka, B.; Hillegers, M.H.J. Pre-pubertal bipolar disorder: Origins and current status of the controversy. Int J. Bipolar Disord 2020, 8, 18. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, B.I.; Birmaher, B.; Carlson, G.A.; DelBello, M.P.; Findling, R.L.; Fristad, M.; Kowatch, R.A.; Miklowitz, D.J.; Nery, F.G.; Perez-Algorta, G.; et al. The international society for bipolar disorders task force report on pediatric bipolar disorder: Knowledge to date and directions for future research. Bipolar Disord. 2017, 19, 524–543. [Google Scholar] [CrossRef] [PubMed]
- Geller, B.; Tillman, R.; Craney, J.L.; Bolhofner, K. Four-year prospective outcome and natural history of mania in children with a prepubertal and early adolescent bipolar disorder phenotype. Arch. Gen. Psychiatry 2004, 61, 459. [Google Scholar] [CrossRef]
- Birmaher, B.; Axelson, D.; Goldstein, B.; Strober, M.; Gill, M.K.; Hunt, J.; Houck, P.; Ha, W.; Iyengar, S.; Kim, E.; et al. Four-year longitudinal course of children and adolescents with bipolar spectrum disorders: The course and outcome of bipolar youth (COBY) study. Am. J. Psychiatry 2009, 10, 795–804. [Google Scholar] [CrossRef]
- DelBello, M.P.; Hanseman, D.; Adler, C.M.; Fleck, D.E.; Strakowski, S.M. Twelve-month outcome of adolescents with bipolar disorder following first hospitalization for a manic or mixed episode. Am. J. Psychiatry 2007, 9, 582–590. [Google Scholar] [CrossRef]
- Wozniak, J.; Petty, C.R.; Schreck, M.; Moses, A.; Faraone, S.V.; Biederman, J. High level of persistence of pediatric bipolar-I disorder from childhood onto adolescent years: A four year prospective longitudinal follow-up study. J. Psychiatr. Res. 2011, 45, 1273–1282. [Google Scholar] [CrossRef] [PubMed]
- Hafeman, D.M.; Goldstein, T.R.; Strober, J.M.; Merranko, J.; Gill, M.K.; Liao, F.; Diler, R.S.; Ryan, N.D.; Goldstein, B.I.; Axelson, D.A.; et al. Prospectively ascertained mania and hypomania among young adults with child- and adolescent-onset bipolar disorder. Bipolar Disord. 2020. [Google Scholar] [CrossRef]
- Findling, R.L.; Stepanova, E.; Youngstrom, E.A.; Young, A.S. Progress in diagnosis and treatment of bipolar disorder among children and adolescents: An international perspective. Evid. Based Ment. Health 2018, 21, 177–181. [Google Scholar] [CrossRef] [PubMed]
- Youngstrom, E.A.; Birmaher, B.; Findling, R.L. Pediatric bipolar disorder: Validity, phenomenology, and recommendations for diagnosis. Bipolar Disord. 2008, 10, 194–214. [Google Scholar] [CrossRef]
- Kowatch, R.A.; Youngstrom, E.A.; Danielyan, A.; Findling, R.L. Review and meta-analysis of the phenomenology and clinical characteristics of mania in children and adolescents. Bipolar Disord. 2005, 7, 483–496. [Google Scholar] [CrossRef] [PubMed]
- Sala, R.; Axelson, D.; Birmaher, B. Phenomenology, longitudinal course, and outcome of children and adolescents with bipolar spectrum disorders. Child. Adolesc. Psychiatr. Clin. N. Am. 2009, 18, 273–289. [Google Scholar] [CrossRef][Green Version]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2018; Available online: https://www.R-project.org/ (accessed on 5 March 2021).
- Wells, G.; Shea, B.; O’Connell, D. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses; The Ottawa Hospital: Ottawa, ON, Canada, 2018; Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 5 March 2021).
- Strober, M.; Schmidt-Lackner, S.; Freeman, R.; Bower, S.; Lampert, C.; Deantonio, M. Recovery and relapse in adolescents with bipolar affective illness: A five-year naturalistic, prospective follow-up. J. Am. Acad. Child. Adolesc. Psychiatry 1995, 34, 724–731. [Google Scholar] [CrossRef] [PubMed]
- Srinath, S.; Reddy, Y.C.J.; Girimaji, S.R.; Seshadri, S.P.; Subbakrishna, D.K.A. Prospective study of bipolar disorder in children and adolescents from India. Acta Psychiatr. Scand. 1998, 98, 437–442. [Google Scholar] [CrossRef]
- Geller, B.; Craney, J.L.; Bolhofner, K.; Nickelsburg, M.J.; Williams, M.; Zimerman, B. Two-year prospective follow-up of children with a prepubertal and early adolescent bipolar disorder phenotype. Am. J. Psychiatry 2002, 159, 927–933. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Geller, B.; Tillman, R.; Bolhofner, K.; Zimerman, B. Child bipolar I disorder: Prospective continuity with adult bipolar i disorder; characteristics of second and third episodes; predictors of 8-year outcome. Arch. Gen. Psychiatry 2008, 65, 1125. [Google Scholar] [CrossRef] [PubMed]
- Geller, B.; Tillman, R.; Bolhofner, K.; Zimerman, B. Pharmacological and non-drug treatment of child bipolar i disorder during prospective eight-year follow-up. Bipolar Disord. 2010, 12, 164–171. [Google Scholar] [CrossRef]
- Rajeev, J.; Srinath, S.; Girimaji, S.; Seshadri, S.P.; Singh, P. A systematic chart review of the naturalistic course and treatment of early-onset bipolar disorder in a child and adolescent psychiatry center. Compr. Psychiatry 2004, 45, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Pettit, J.W.; Morgan, S.; Paukert, A.L. The Stability of Axis I Diagnoses in Youth Across Multiple Psychiatric Hospitalizations. Child. Psychiatry Hum. Dev. 2005, 36, 53–71. [Google Scholar] [CrossRef] [PubMed]
- Birmaher, B.; Axelson, D.; Strober, M.; Gill, M.K.; Valeri, S.; Chiappetta, L.; Ryan, N.; Leonard, H.; Hunt, J.; Iyengar, S.; et al. Clinical course of children and adolescents with bipolar spectrum disorders. Arch. Gen. Psychiatry 2006, 63, 175–183. [Google Scholar] [CrossRef]
- Axelson, D.A.; Birmaher, B.; Strober, M.A.; Goldstein, B.I.; Ha, W.; Gill, M.K.; Goldstein, T.R.; Yen, S.; Hower, H.; Hunt, J.I.; et al. Course of subthreshold bipolar disorder in youth: Diagnostic progression from bipolar disorder not otherwise specified. J. Am. Acad. Child. Adolesc. Psychiatry 2011, 50, 1001–1016.e3. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, T.R.; Ha, W.; Axelson, D.A.; Goldstein, B.I.; Liao, F.; Gill, M.K.; Ryan, N.D.; Yen, S.; Hunt, J.; Hower, H.; et al. Predictors of prospectively examined suicide attempts among youth with bipolar disorder. Arch. Gen. Psychiatry 2012, 69, 1113–1122. [Google Scholar] [CrossRef]
- Goldstein, B.I.; Strober, M.; Axelson, D.; Goldstein, T.R.; Gill, M.K.; Hower, H.; Dickstein, D.; Hunt, J.; Yen, S.; Kim, E.; et al. Predictors of first-onset substance use disorders during the prospective course of bipolar spectrum disorders in adolescents. J. Am. Acad. Child. Adolesc. Psychiatry 2013, 52, 1026–1037. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hower, H.; Case, B.G.; Hoeppner, B.; Yen, S.; Goldstein, T.; Goldstein, B.; Birmaher, B.; Weinstock, L.; Topor, D.; Hunt, J.; et al. Use of mental health services in transition age youth with bipolar disorder. J. Psychiatr. Pr. 2013, 19, 464–476. [Google Scholar] [CrossRef]
- Hunt, J.I.; Case, B.G.; Birmaher, B.; Stout, R.L.; Dickstein, D.P.; Yen, S.; Goldstein, T.R.; Goldstein, B.I.; Axelson, D.A.; Hower, H.; et al. Irritability and elation in a large bipolar youth sample. J. Clin. Psychiatry 2013, 74, e110–e117. [Google Scholar] [CrossRef]
- Sala, R.; Axelson, D.A.; Castro-Fornieles, J.; Goldstein, T.R.; Goldstein, B.I.; Ha, W.; Liao, F.; Gill, M.K.; Iyengar, S.; Strober, M.A.; et al. Factors associated with the persistence and onset of new anxiety disorders in youth with bipolar spectrum disorders. J. Clin. Psychiatry 2011, 73, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Birmaher, B.; Gill, M.K.; Axelson, D.A.; Goldstein, B.I.; Goldstein, T.R.; Yu, H.; Liao, F.; Iyengar, S.; Diler, R.S.; Strober, M.; et al. Longitudinal trajectories and associated baseline predictors in youths with bipolar spectrum disorders. Am. J. Psychiatry 2014, 171, 990–999. [Google Scholar] [CrossRef] [PubMed]
- Sala, R.; Strober, M.A.; Axelson, D.A.; Gill, M.K.; Castro-Fornieles, J.; Goldstein, T.R.; Goldstein, B.I.; Ha, W.; Liao, F.; Iyengar, S.; et al. Effects of comorbid anxiety disorders on the longitudinal course of pediatric bipolar disorders. J. Am. Acad. Child. Adolesc. Psychiatry 2014, 53, 72–81. [Google Scholar] [CrossRef] [PubMed]
- Yen, S.; Frazier, E.; Hower, H.; Weinstock, L.M.; Topor, D.R.; Hunt, J.; Goldstein, T.R.; Goldstein, B.I.; Gill, M.K.; Ryan, N.D.; et al. Borderline personality disorder in transition age youth with bipolar disorder. Acta Psychiatr. Scand. 2015, 132, 270–280. [Google Scholar] [CrossRef]
- Borue, X.; Mazefsky, C.; Rooks, B.T.; Strober, M.; Keller, M.B.; Hower, H.; Yen, S.; Gill, M.K.; Diler, R.S.; Axelson, D.A.; et al. Longitudinal Course of Bipolar Disorder in Youth with High-Functioning Autism Spectrum Disorder. J. Am. Acad. Child. Adolesc. Psychiatry 2016, 55, 1064–1072.e6. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Frías, Á.; Dickstein, D.P.; Merranko, J.; Gill, M.K.; Goldstein, T.R.; Goldstein, B.I.; Hower, H.; Yen, S.; Hafeman, D.M.; Liao, F.; et al. Longitudinal cognitive trajectories and associated clinical variables in youth with bipolar disorder. Bipolar Disord. 2017, 19, 273–284. [Google Scholar] [CrossRef]
- Krantz, M.; Goldstein, T.; Rooks, B.; Merranko, J.; Liao, F.; Gill, M.K.; Diler, R.; Hafeman, D.; Ryan, N.; Goldstein, B.; et al. Sexual risk behavior among youth with bipolar disorder: Identifying demographic and clinical risk factors. J. Am. Acad. Child. Adolesc. Psychiatry 2018, 57, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Hower, H.; Lee, E.J.; Jones, R.N.; Birmaher, B.; Strober, M.; Goldstein, B.I.; Merranko, J.; Keller, M.B.; Goldstein, T.R.; Weinstock, L.M.; et al. Predictors of longitudinal psychosocial functioning in bipolar youth transitioning to adults. J. Affect. Disord. 2019, 246, 578–585. [Google Scholar] [CrossRef] [PubMed]
- Pascual, M.A.; Levenson, J.C.; Merranko, J.; Gill, M.K.; Hower, H.; Yen, S.; Strober, M.; Goldstein, T.R.; Goldstein, B.I.; Ryan, N.D.; et al. The effect of traumatic events on the longitudinal course and outcomes of youth with bipolar disorder. J. Affect. Disord. 2020, 274, 126–135. [Google Scholar] [CrossRef]
- Shalev, A.; Merranko, J.; Gill, M.K.; Goldstein, T.; Liao, F.; Goldstein, B.I.; Hower, H.; Ryan, N.; Strober, M.; Iyengar, S.; et al. Longitudinal course and risk factors associated with psychosis in bipolar youths. Bipolar Disord. 2019, 22, 139–154. [Google Scholar] [CrossRef] [PubMed]
- Frazier, E.A.; Hunt, J.I.; Hower, H.; Jones, R.N.; Birmaher, B.; Strober, M.; Goldstein, B.I.; Keller, M.B.; Goldstein, T.R.; Weinstock, L.M.; et al. Correlates, course, and outcomes of increased energy in youth with bipolar disorder. J. Affect. Disord. 2020, 271, 248–254. [Google Scholar] [CrossRef] [PubMed]
- Hafeman, D.M.; Rooks, B.; Merranko, J.; Liao, F.; Gill, M.K.; Goldstein, T.R.; Diler, R.; Ryan, N.; Goldstein, B.I.; Axelson, D.A.; et al. Lithium versus other mood-stabilizing medications in a longitudinal study of youth diagnosed with bipolar disorder. J. Am. Acad. Child. Adolesc. Psychiatry 2020, 59, 1146–1155. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.J.; Hower, H.; Jones, R.N.; Birmaher, B.; Strober, M.; Goldstein, B.I.; Merranko, J.; Keller, M.B.; Goldstein, T.R.; Weinstock, L.M.; et al. Course of longitudinal psychosocial functioning in bipolar youth transitioning to adults. J. Affect. Disord. 2020, 268, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, R.H.B.; Hower, H.; Birmaher, B.; Strober, M.; Merranko, J.; Rooks, B.; Goldstein, T.R.; Hunt, J.I.; Dickstein, D.P.; Diler, R.S.; et al. Sex differences in the longitudinal course and outcome of bipolar disorder in youth. J. Clin. Psychiatry 2020, 81, 19m13159. [Google Scholar] [CrossRef]
- Sewall, C.J.; Girard, J.M.; Merranko, J.; Hafeman, D.; Goldstein, B.I.; Strober, M.; Hower, H.; Weinstock, L.M.; Yen, S.; Ryan, N.D.; et al. A Bayesian multilevel analysis of the longitudinal associations between relationship quality and suicidal ideation and attempts among youth with bipolar disorder. J. Child. Psychol. Psychiatry 2020. [Google Scholar] [CrossRef] [PubMed]
- Castilla-Puentes, R. multiple episodes in children and adolescents with bipolar disorder: Comorbidity, hospitalization, and treatment (data from a cohort of 8129 patients of a national managed care database). Int. J. Psychiatry Med. 2008, 38, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Jerrell, J.M.; Prewette, E.D. Outcomes for youths with early- and very-early-onset bipolar I disorder. J. Behav. Heal. Serv. Res. 2008, 35, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Escamilla, I.; Wozniak, J.; Soutullo, C.A.; Gamazo-Garrán, P.; Figueroa-Quintana, A.; Biederman, J. Pediatric bipolar disorder in a Spanish sample: Results after 2.6years of follow-up. J. Affect. Disord. 2011, 132, 270–274. [Google Scholar] [CrossRef]
- Ribeiro-Fernández, M.; Díez-Suárez, A.; Soutullo, C. Phenomenology and diagnostic stability of paediatric bipolar disorder in a Spanish sample. J. Affect. Disord. 2019, 242, 224–233. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, A.E.; Judd, C.M.; Axelson, D.A.; Miklowitz, D.J. Family functioning and the course of adolescent bipolar disorder. Behav. Ther. 2012, 43, 837–847. [Google Scholar] [CrossRef] [PubMed]
- Findling, R.L.; Jo, B.; Frazier, T.W.; A Youngstrom, E.; A Demeter, C.; A Fristad, M.; Birmaher, B.; A Kowatch, R.; Arnold, E.; A Axelson, D.; et al. The 24-month course of manic symptoms in children. Bipolar Disord. 2013, 15, 669–679. [Google Scholar] [CrossRef]
- Kessing, L.V.; Vradi, E.; Andersen, P.K. Diagnostic stability in pediatric bipolar disorder. J. Affect. Disord. 2015, 172, 417–421. [Google Scholar] [CrossRef] [PubMed]
- Laursen, M.F.; Licht, R.W.; Correll, C.U.; Kallehauge, T.; Christensen, A.-E.; Rodrigo-Domingo, M.; Nielsen, R.E. Diagnostic stability in children and adolescents with bipolar disorder, a nationwide register-based study. Int. J. Bipolar Disord. 2020, 8, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Weintraub, M.J.; Schneck, C.D.; Axelson, D.A.; Birmaher, B.; Kowatch, R.A.; Miklowitz, D.J. Classifying mood symptom trajectories in adolescents with bipolar disorder. J. Am. Acad. Child. Adolesc. Psychiatry 2020, 59, 381–390. [Google Scholar] [CrossRef] [PubMed]
- Diagnostic and Statistical Manual of Mental Disorder, 4th ed.; American Psychiatric Association: Washington DC, USA, 1994.
- World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic Criteria for Research; World Health Organization: Geneva, Switzerland, 1993. [Google Scholar]
- Spitzer, R.L.; Endicott, J.; Robins, E. Research diagnostic criteria. Arch. Gen. Psychiatry 1978, 35, 773–782. [Google Scholar] [CrossRef]
- Hauser, M.; Galling, B.; Correll, C.U. Suicidal ideation and suicide attempts in children and adolescents with bipolar disorder: A systematic review of prevalence and incidence rates, correlates, and targeted interventions. Bipolar Disord. 2013, 15, 507–523. [Google Scholar] [CrossRef]
- Nock, M.K.; Green, J.G.; Hwang, I.; McLaughlin, K.A.; Sampson, N.A.; Zaslavsky, A.M.; Kessler, R.C. Prevalence, Correlates, and Treatment of Lifetime Suicidal Behavior Among Adolescents. JAMA Psychiatry 2013, 70, 300–310. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).