Extended fMRI-Guided Anodal and Cathodal Transcranial Direct Current Stimulation Targeting Perilesional Areas in Post-Stroke Aphasia: A Pilot Randomized Clinical Trial
Abstract
1. Introduction
2. Materials and Methods
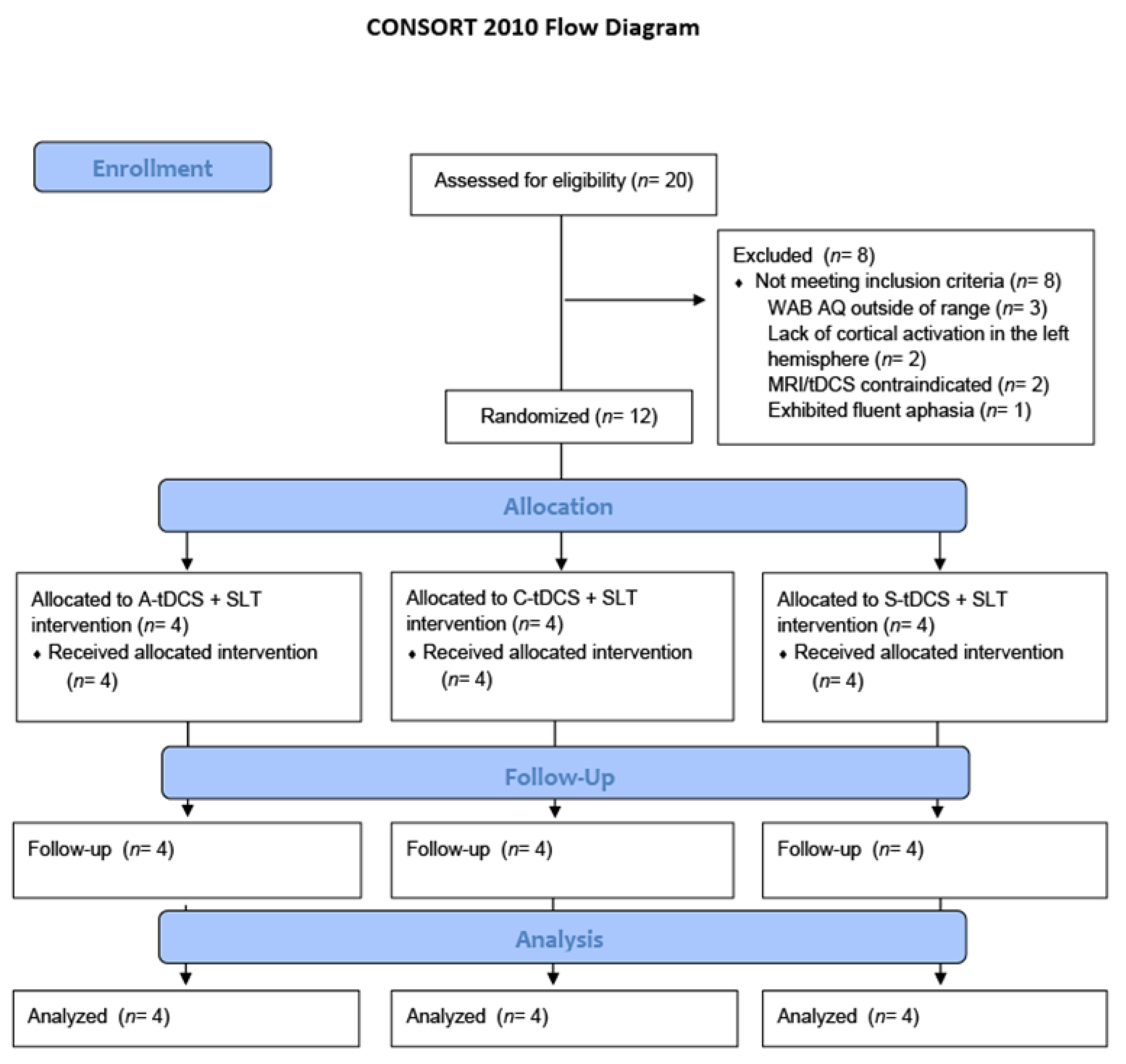
2.1. Participants
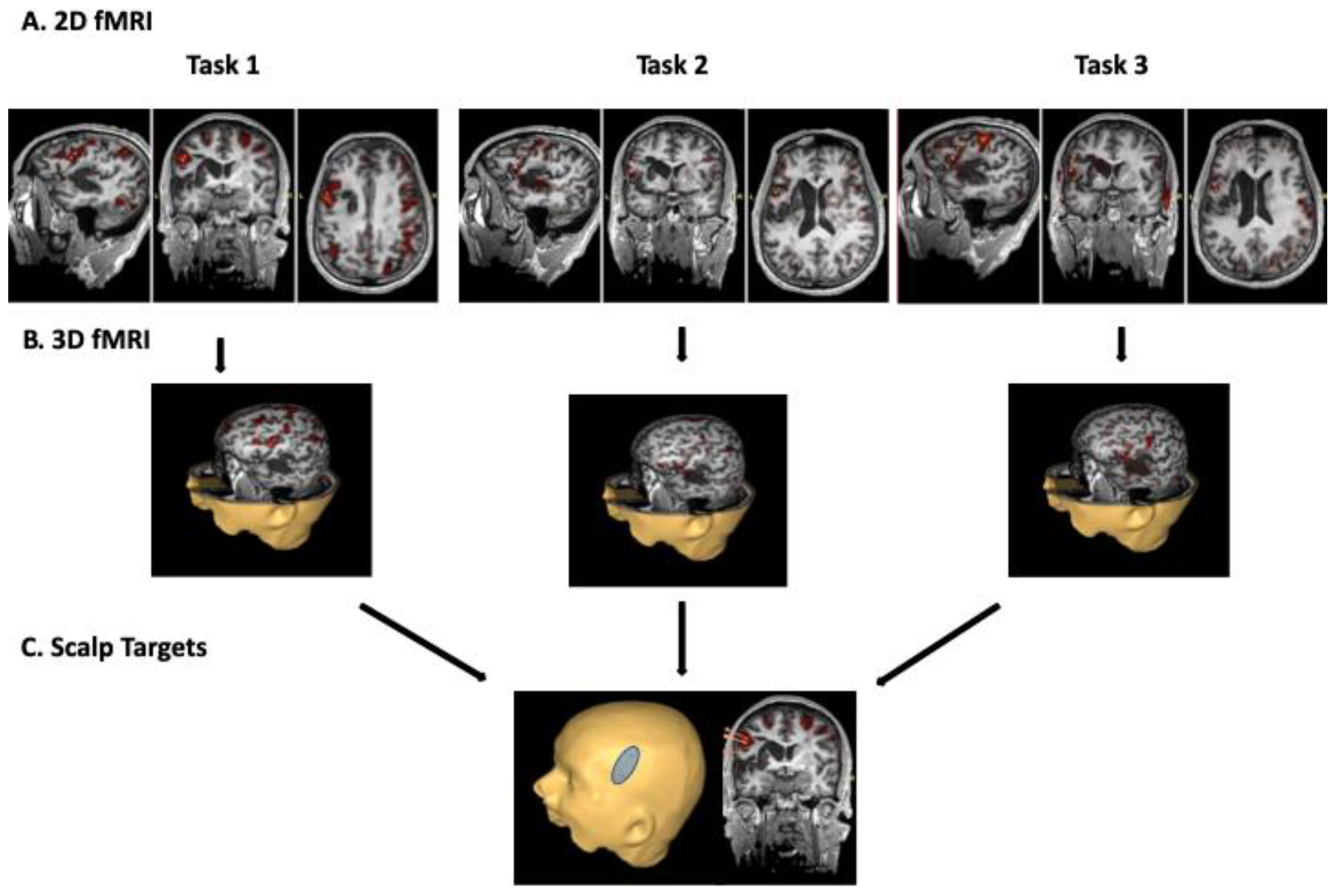
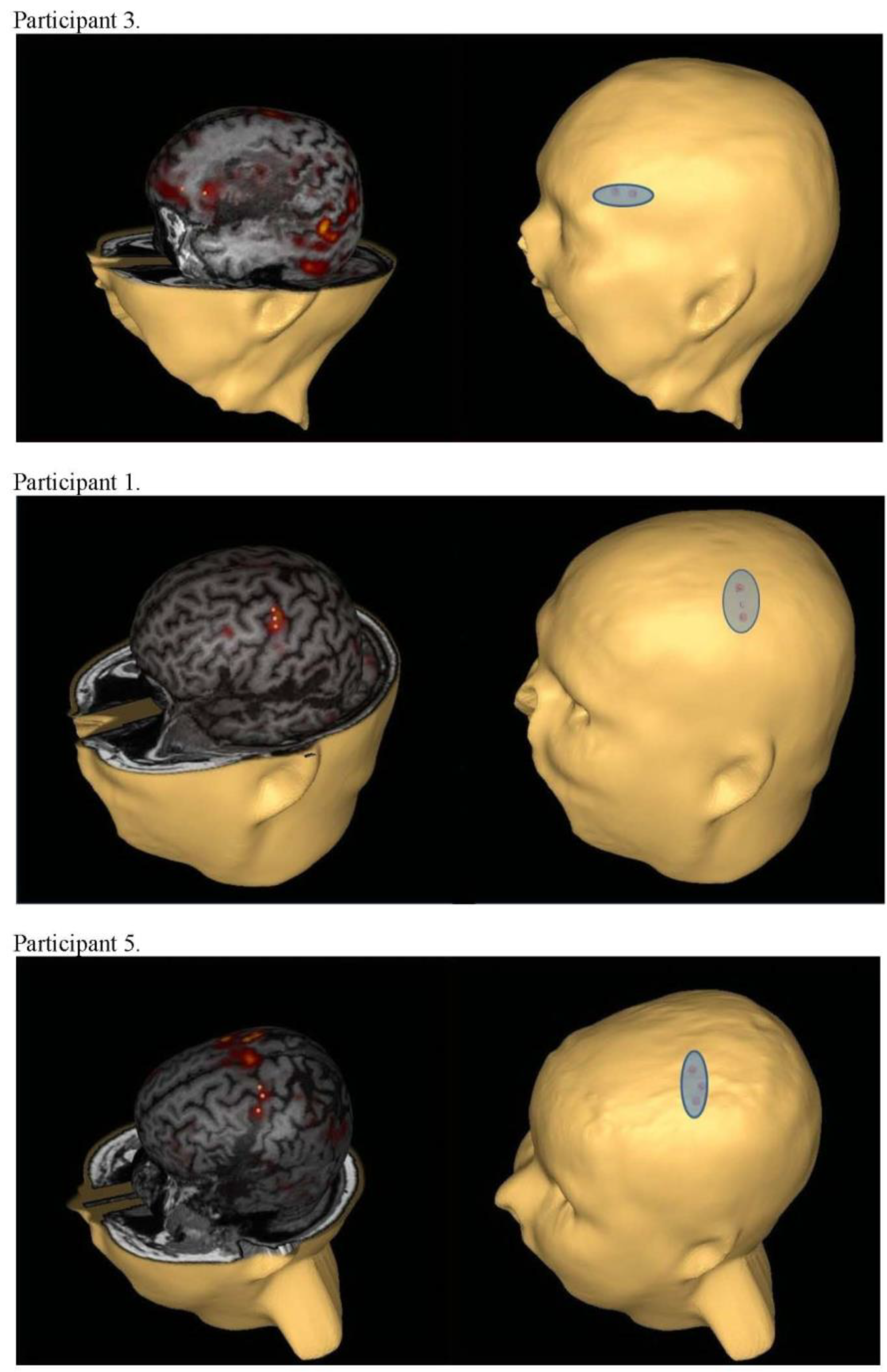
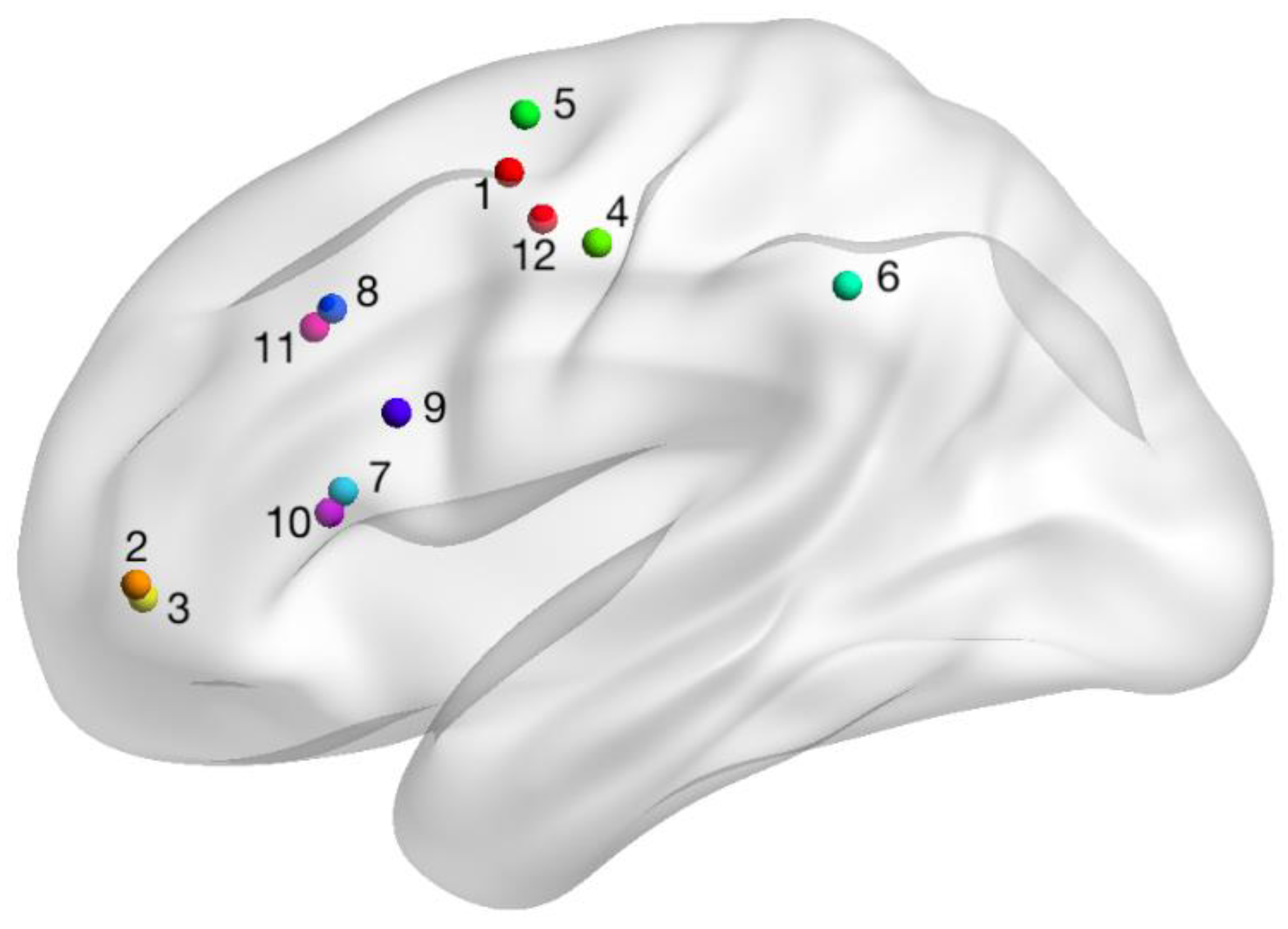
2.2. fMRI-Guided Localization of Perilesional Stimulation Site
2.3. Randomization and Blinding
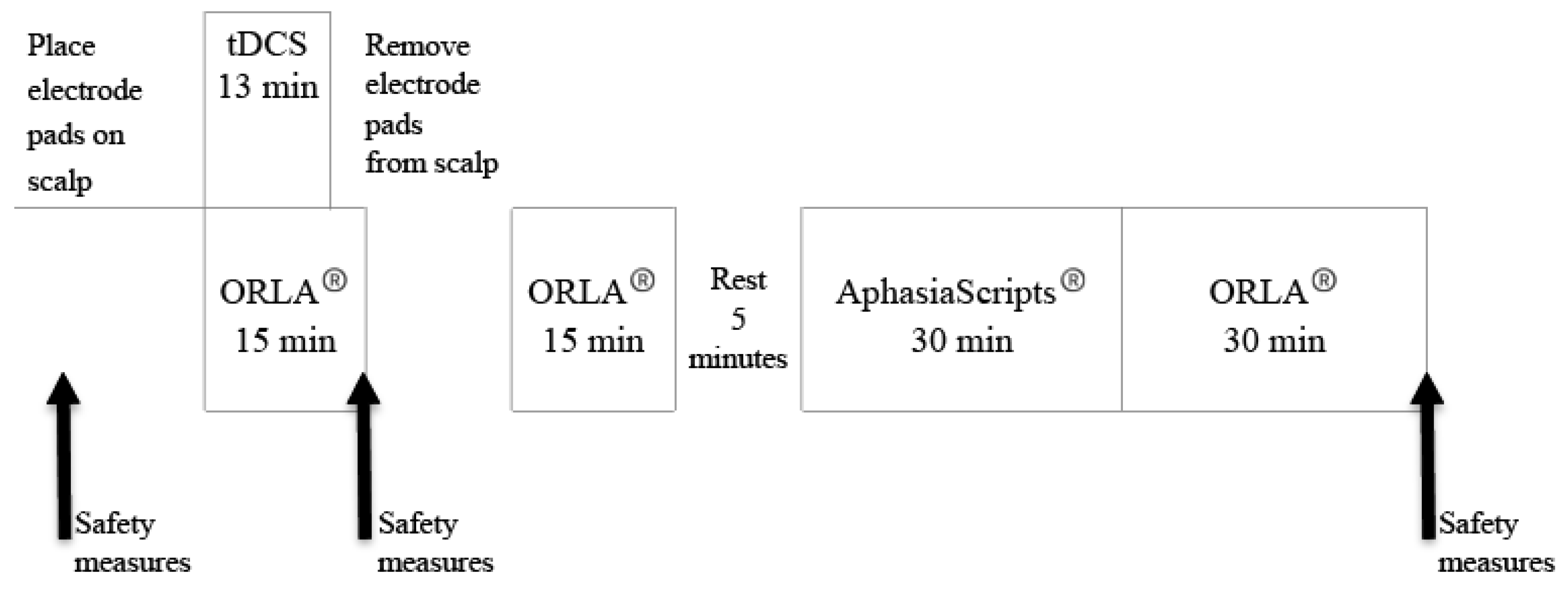
2.4. tDCS Intervention
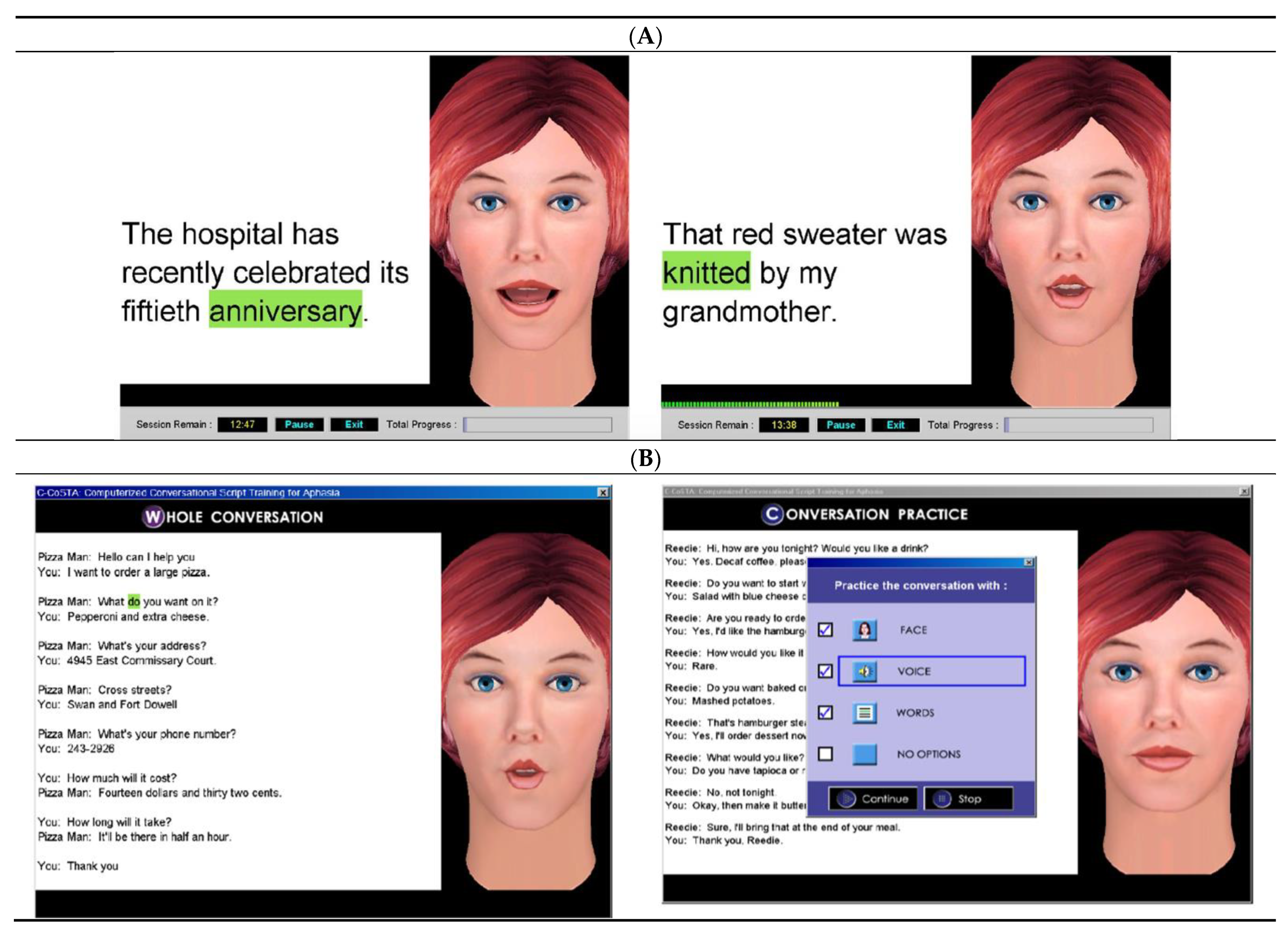
2.5. Concurrent Language Intervention
2.6. Outcome Measures
2.7. Analyses
3. Results
3.1. Safety and Tolerability of Prolonged tDCS
3.2. Language Outcome Measures
3.2.1. Primary Outcome Measure (WAB-R AQ)
3.2.2. Secondary Outcome Measures
3.3. fMRI Cortical Activation Patterns
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Avan, A.; Digaleh, H.; Di Napoli, M.; Stranges, S.; Behrouz, R.; Shojaeianbabaei, G.; Amiri, A.; Tabrizi, R.; Mokhber, N.; Spence, J.D.; et al. Socioeconomic status and stroke incidence, prevalence, mortality, and worldwide burden: An ecological analysis from the Global Burden of Disease Study 2017. BMC Med. 2019, 17, 1–30. [Google Scholar] [CrossRef]
- Flowers, H.L.; Silver, F.L.; Fang, J.; Rochon, E.; Martino, R. The incidence, co-occurrence, and predictors of dysphagia, dysarthria, and aphasia after first-ever acute ischemic stroke. J. Commun. Disord. 2013, 46, 238–248. [Google Scholar] [CrossRef]
- Flowers, H.L.; Skoretz, S.A.; Silver, F.L.; Rochon, E.; Fang, J.; Flamand-Roze, C.; Martino, R. Poststroke aphasia frequency, recovery, and outcomes: A systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 2016, 97, 2188–2201.e8. [Google Scholar] [CrossRef]
- Dalemans, R.J.P.; De Witte, L.P.; Wade, D.; Heuvel, W.V.D. Social participation through the eyes of people with aphasia. Int. J. Lang. Commun. Disord. 2010, 45, 537–550. [Google Scholar] [CrossRef]
- Hilari, K.; Northcott, S.; Roy, P.; Marshall, J.; Wiggins, R.D.; Chataway, J.; Ames, D. Psychological distress after stroke and aphasia: The first six months. Clin. Rehabil. 2010, 24, 181–190. [Google Scholar] [CrossRef]
- Bullier, B.; Cassoudesalle, H.; Villain, M.; Cogné, M.; Mollo, C.; De Gabory, I.; Dehail, P.; Joseph, P.-A.; Sibon, I.; Glize, B. New factors that affect quality of life in patients with aphasia. Ann. Phys. Rehabil. Med. 2020, 63, 33–37. [Google Scholar] [CrossRef]
- Ashaie, S.A.; Hurwitz, R.; Cherney, L.R. Depression and subthreshold depression in stroke-related aphasia. Arch. Phys. Med. Rehabil. 2019, 100, 1294–1299. [Google Scholar] [CrossRef]
- Brady, M.C.; Kelly, H.; Godwin, J.; Enderby, P.; Campbell, P. Speech and language therapy for aphasia following stroke. Cochrane Database Syst. Rev. 2016, CD000425. [Google Scholar] [CrossRef]
- Cherney, L.R.; Patterson, J.P.; Raymer, A.; Frymark, T.; Schooling, T. Evidence-based systematic review: Effects of intensity of treatment and constraint-induced language therapy for individuals with stroke-induced aphasia. J. Speech Lang. Hear. Res. 2008, 51, 1282–1299. [Google Scholar] [CrossRef]
- Elsner, B.; Kugler, J.; Pohl, M.; Mehrholz, J. Transcranial direct current stimulation (tDCS) for improving aphasia in adults with aphasia after stroke. Cochrane Database Syst. Rev. 2019, 2019, CD009760. [Google Scholar] [CrossRef]
- Lefaucheur, J.-P.; Antal, A.; Ayache, S.S.; Benninger, D.H.; Brunelin, J.; Cogiamanian, F.; Cotelli, M.; De Ridder, D.; Ferrucci, R.; Langguth, B.; et al. Evidence-based guidelines on the therapeutic use of transcranial direct current stimulation (tDCS). Clin. Neurophysiol. 2017, 128, 56–92. [Google Scholar] [CrossRef] [PubMed]
- Ulanov, M.; Shtyrov, Y.; Stroganova, T. Transcranial direct current stimulation as a tool to induce language recovery in patients with post-stroke aphasia. Neurosci. Behav. Physiol. 2019, 49, 1169–1180. [Google Scholar] [CrossRef]
- Marangolo, P. The potential effects of transcranial direct current stimulation (tDCS) on language functioning: Combining neuromodulation and behavioral intervention in aphasia. Neurosci. Lett. 2020, 719, 133329. [Google Scholar] [CrossRef] [PubMed]
- Nitsche, M.A.; Paulus, W. Excitability changes induced in the human motor cortex by weak transcranial direct current stimulation. J. Physiol. 2000, 527, 633–639. [Google Scholar] [CrossRef] [PubMed]
- Nitsche, M.A.; Paulus, W. Sustained excitability elevations induced by transcranial DC motor cortex stimulation in humans. Neurology 2001, 57, 1899–1901. [Google Scholar] [CrossRef]
- Nitsche, M.A.; Nitsche, M.S.; Klein, C.C.; Tergau, F.; Rothwell, J.C.; Paulus, W. Level of action of cathodal DC polarisation induced inhibition of the human motor cortex. Clin. Neurophysiol. 2003, 114, 600–604. [Google Scholar] [CrossRef]
- Kiran, S. What is the nature of poststroke language recovery and reorganization? ISRN Neurol. 2012, 2012, 786872. [Google Scholar] [CrossRef]
- Di Pino, G.; Pellegrino, G.; Assenza, G.; Capone, F.; Ferreri, F.; Formica, D.; Ranieri, F.; Tombini, M.; Ziemann, U.; Rothwell, J.C.; et al. Modulation of brain plasticity in stroke: A novel model for neurorehabilitation. Nat. Rev. Neurol. 2014, 10, 597–608. [Google Scholar] [CrossRef] [PubMed]
- Monti, A.; Cogiamanian, F.; Marceglia, S.; Ferrucci, R.; Mameli, F.; Mrakic-Sposta, S.; Vergari, M.; Zago, S.; Priori, A. Improved naming after transcranial direct current stimulation in aphasia. J. Neurol. Neurosurg. Psychiatry 2008, 79, 451–453. [Google Scholar] [CrossRef]
- Shah-Basak, P.P.; Norise, C.; Garcia, G.; Torres, J.; Faseyitan, O.; Hamilton, R.H. Individualized treatment with transcranial direct current stimulation in patients with chronic non-fluent aphasia due to stroke. Front. Hum. Neurosci. 2015, 9, 201. [Google Scholar] [CrossRef]
- Datta, A.; Baker, J.M.; Bikson, M.; Fridriksson, J. Individualized model predicts brain current flow during transcranial direct-current stimulation treatment in responsive stroke patient. Brain Stimul. 2011, 4, 169–174. [Google Scholar] [CrossRef]
- Galletta, E.E.; Cancelli, A.; Cottone, C.; Simonelli, I.; Tecchio, F.; Bikson, M.; Marangolo, P. Use of computational modeling to inform tDCS electrode montages for the promotion of language recovery in post-stroke aphasia. Brain Stimul. 2015, 8, 1108–1115. [Google Scholar] [CrossRef] [PubMed]
- Fridriksson, J.; Rorden, C.; Elm, J.; Sen, S.; George, M.S.; Bonilha, L. Transcranial direct current stimulation vs sham stimulation to treat aphasia after stroke: A randomized clinical trial. JAMA Neurol. 2018, 75, 1470–1476. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, M.F.; Armijo-Olivo, S.; Kim, E.S. Transcranial direct current stimulation (tDCS) to improve naming ability in post-stroke aphasia: A critical review. Behav. Brain Res. 2017, 332, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Kertesz, A. Western Aphasia Battery (Revised); PsychCorp: San Antonio, TX, USA, 2007. [Google Scholar]
- Oldfield, R. The assessment and analysis of handedness: The Edinburgh inventory. Neuropsychology 1971, 9, 97–113. [Google Scholar] [CrossRef]
- Cherney, L.R.; Erickson, R.K.; Small, S.L. Epidural cortical stimulation as adjunctive treatment for non-fluent aphasia: Preliminary findings. J. Neurol. Neurosurg. Psychiatry 2010, 81, 1014–1021. [Google Scholar] [CrossRef]
- Cherney, L.R.; Small, S.L. Task-dependent changes in brain activation following therapy for nonfluent aphasia: Discussion of two individual cases. J. Int. Neuropsychol. Soc. 2006, 12, 828–842. [Google Scholar] [CrossRef]
- Cherney, L.R.; Babbitt, E.M.; Hurwitz, R.; Rogers, L.M.; Stinear, J.; Wang, X.; Harvey, R.L.; Parrish, T. Transcranial direct current stimulation and aphasia: The case of Mr. C. Top. Stroke Rehabil. 2013, 20, 5–20. [Google Scholar] [CrossRef][Green Version]
- Nitsche, M.A.; Cohen, L.G.; Wassermann, E.M.; Priori, A.; Lang, N.; Antal, A.; Paulus, W.; Hummel, F.; Boggio, P.S.; Fregni, F.; et al. Transcranial direct current stimulation: State of the art 2018. Brain Stimul. 2008, 1, 206–223. [Google Scholar] [CrossRef] [PubMed]
- Nitsche, M.A.; Liebetanz, D.; Lang, N.; Antal, A.; Tergau, F.; Paulus, W. Safety criteria for transcranial direct current stimulation (tDCS) in humans. Clin. Neurophysiol. 2003, 114, 2220–2222. [Google Scholar] [CrossRef]
- Bikson, M.; Grossman, P.; Thomas, C.; Zannou, A.L.; Jiang, J.; Adnan, T.; Mourdoukoutas, A.P.; Kronberg, G.; Truong, D.; Boggio, P.; et al. Safety of transcranial direct current stimulation: Evidence based update 2016. Brain Stimul. 2016, 9, 641–661. [Google Scholar] [CrossRef] [PubMed]
- Cherney, L.R.; Merbitz, C.T.; Grip, J.C. Efficacy of oral reading in aphasia treatment outcome. Rehabil. Lit. 1986, 47, 112–118. [Google Scholar] [PubMed]
- Cherney, L.R. Efficacy of oral reading in the treatment of two patients with chronic Broca’s aphasia. Top. Stroke Rehabil. 1995, 2, 57–67. [Google Scholar] [CrossRef]
- Cherney, L.R. Oral reading for language in aphasia (ORLA): Evaluating the efficacy of computer-delivered therapy in chronic nonfluent aphasia. Top. Stroke Rehabil. 2010, 17, 423–431. [Google Scholar] [CrossRef]
- Cherney, L.R.; Halper, A.S.; Holland, A.L.; Cole, R. Computerized script training for aphasia: Preliminary results. Am. J. Speech-Language Pathol. 2008, 17, 19–34. [Google Scholar] [CrossRef]
- Lee, J.B.; Kaye, R.C.; Cherney, L.R. Conversational script performance in adults with non-fluent aphasia: Treatment intensity and aphasia severity. Aphasiology 2009, 23, 885–897. [Google Scholar] [CrossRef]
- Manheim, L.M.; Halper, A.S.; Cherney, L. Patient-reported changes in communication after computer-based script training for aphasia. Arch. Phys. Med. Rehabil. 2009, 90, 623–627. [Google Scholar] [CrossRef] [PubMed]
- Wallace, S.J.; Worrall, L.; Rose, T.; Le Dorze, G.; Breitenstein, C.; Hilari, K.; Babbitt, E.; Bose, A.; Brady, M.; Cherney, L.R.; et al. A core outcome set for aphasia treatment research: The ROMA consensus statement. Int. J. Stroke 2019, 14, 180–185. [Google Scholar] [CrossRef]
- Lomas, J.; Pickard, L.; Bester, S.; Elbard, H.; Finlayson, A.; Zoghaib, C. The communicative effectiveness index: Development and psychometric evaluation of a functional communication measure for adult aphasia. J. Speech Hear. Disord. 1989, 54, 113–124. [Google Scholar] [CrossRef]
- Gilmore, N.; Dwyer, M.; Kiran, S. Benchmarks of significant change after aphasia rehabilitation. Arch. Phys. Med. Rehabil. 2019, 100, 1131–1139.e87. [Google Scholar] [CrossRef]
- Pitts, L.L.; Hurwitz, R.; Lee, J.B.; Carpenter, J.; Cherney, L.R. Validity, reliability and sensitivity of the NORLA-6: Naming and oral reading for language in aphasia 6-point scale. Int. J. Speech-Language Pathol. 2017, 20, 274–283. [Google Scholar] [CrossRef]
- Katz, R.C.; Wertz, R.T. The efficacy of computer-provided reading treatment for chronic aphasic adults. J. Speech Lang. Hear. Res. 1997, 40, 493–507. [Google Scholar] [CrossRef] [PubMed]
- Beeson, P.M.; Robey, R.R. Evaluating single-subject treatment research: Lessons learned from the aphasia literature. Neuropsychol. Rev. 2006, 16, 161–169. [Google Scholar] [CrossRef]
- Robey, R.R.; Schultz, M.C.; Crawford, A.B.; Sinner, C.A. Single-subject clinical-outcome research: Designs, data, effect sizes, and analyses. Aphasiology 1999, 13, 445–473. [Google Scholar] [CrossRef]
- Robey, R.R. A meta-analysis of clinical outcomes in the treatment of aphasia. J. Speech Lang. Hear. Res. 1998, 41, 172–187. [Google Scholar] [CrossRef] [PubMed]
- Fischl, B.; Sereno, M.I.; Dale, A.M. Cortical surface-based analysis: II: Inflation, flattening, and a surface-based coordinate system. Neuroimage 1999, 9, 195–207. [Google Scholar] [CrossRef]
- Greve, D.N.; Fischl, B. Accurate and robust brain image alignment using boundary-based registration. NeuroImage 2009, 48, 63–72. [Google Scholar] [CrossRef]
- Jenkinson, M.; Smith, S. A global optimisation method for robust affine registration of brain images. Med. Image Anal. 2001, 5, 143–156. [Google Scholar] [CrossRef]
- Jenkinson, M.; Bannister, P.; Brady, M.; Smith, S. Improved optimization for the robust and accurate linear registration and motion correction of brain images. NeuroImage 2002, 17, 825–841. [Google Scholar] [CrossRef]
- Brunoni, A.R.; Amadera, J.; Berbel, B.; Volz, M.S.; Rizzerio, B.G.; Fregni, F. A systematic review on reporting and assessment of adverse effects associated with transcranial direct current stimulation. Int. J. Neuropsychopharmacol. 2011, 14, 1133–1145. [Google Scholar] [CrossRef]
- Poreisz, C.; Boros, K.; Antal, A.; Paulus, W. Safety aspects of transcranial direct current stimulation concerning healthy subjects and patients. Brain Res. Bull. 2007, 72, 208–214. [Google Scholar] [CrossRef]
- List, J.; Lesemann, A.; Kübke, J.C.; Külzow, N.; Schreiber, S.J.; Flöel, A. Impact of tDCS on cerebral autoregulation in aging and in patients with cerebrovascular diseases. Neurology 2015, 84, 626–628. [Google Scholar] [CrossRef]
- Polanowska, K.; Leśniak, M.; Seniów, J. P 114.Anodal transcranial direct current stimulation in early treatment of post-stroke non-fluent aphasia. Clin. Neurophysiol. 2013, 124, e118–e119. [Google Scholar] [CrossRef]
- Duncan, E.S.; Nakkawita, S.G. Clinical feasibility of combining transcranial direct current stimulation with standard aphasia therapy. Ann. Indian Acad. Neurol. 2020, 23, S102–S108. [Google Scholar]
- Cherney, L.R.; Patterson, J.P.; Raymer, A.M. Intensity of aphasia therapy: Evidence and efficacy. Curr. Neurol. Neurosci. Rep. 2011, 11, 560–569. [Google Scholar] [CrossRef]
- Bütefisch, C.M.; Kleiser, R.; Seitz, R.J. Post-lesional cerebral reorganisation: Evidence from functional neuroimaging and transcranial magnetic stimulation. J. Physiol. 2006, 99, 437–454. [Google Scholar] [CrossRef] [PubMed]
- Lang, N.; Nitsche, M.A.; Paulus, W.; Rothwell, J.C.; Lemon, R.N. Effects of transcranial direct current stimulation over the human motor cortex on corticospinal and transcallosal excitability. Exp. Brain Res. 2004, 156, 439–443. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, T.; Hosaki, A.; Hino, T.; Sato, M.; Komori, T.; Hirai, S.; Rossini, P.M. Motor cortical disinhibition in the unaffected hemisphere after unilateral cortical stroke. Brain 2002, 125, 1896–1907. [Google Scholar] [CrossRef]
- Finger, S.; Buckner, R.L.; Buckingham, H. Does the right hemisphere take over after damage to Broca’s area? the Barlow case of 1877 and its history. Brain Lang. 2003, 85, 385–395. [Google Scholar] [CrossRef]
- Hillis, A.E.; Seeley, W.W.; Marty, F.M.; Holmes, T.M.; Upchurch, K.; Soiffer, R.J.; Antin, J.H.; Baden, L.R.; Bromfield, E.B. Aphasia: Progress in the last quarter of a century. Neurology 2007, 69, 200–213. [Google Scholar] [CrossRef]
- Kiran, S.; Meier, E.L.; Johnson, J.P. Neuroplasticity in aphasia: A proposed framework of language recovery. J. Speech Lang. Hear. Res. 2019, 62, 3973–3985. [Google Scholar] [CrossRef] [PubMed]
- Saur, D.; Lange, R.; Baumgaertner, A.; Schraknepper, V.; Willmes, K.; Rijntjes, M.; Weiller, C. Dynamics of language reorganization after stroke. Brain 2006, 129, 1371–1384. [Google Scholar] [CrossRef] [PubMed]
- Winhuisen, L.; Thiel, A.; Schumacher, B.; Kessler, J.; Rudolf, J.; Haupt, W.F.; Heiss, W.D. Role of the contralateral inferior frontal gyrus in recovery of language function in poststroke aphasia: A combined repetitive transcranial magnetic stimulation and positron emission tomography study. Stroke 2005, 36, 1759–1763. [Google Scholar] [CrossRef]
- Winhuisen, L.; Thiel, A.; Schumacher, B.; Kessler, J.; Rudolf, J.; Haupt, W.F.; Heiss, W.D. The right inferior frontal gyrus and poststroke aphasia: A follow-up investigation. Stroke 2007, 38, 1286–1292. [Google Scholar] [CrossRef] [PubMed]
- Batsikadze, G.; Moliadze, V.; Paulus, W.; Kuo, M.-F.; Nitsche, M.A. Partially non-linear stimulation intensity-dependent effects of direct current stimulation on motor cortex excitability in humans. J. Physiol. 2013, 591, 1987–2000. [Google Scholar] [CrossRef]
- Solomons, C.D.; Shanmugasundaram, V. Transcranial direct current stimulation: A review of electrode characteristics and materials. Med. Eng. Phys. 2020, 85, 63–74. [Google Scholar] [CrossRef]
- Bastani, A.; Jaberzadeh, S. a-tDCS differential modulation of corticospinal excitability: The effects of electrode size. Brain Stimul. 2013, 6, 932–937. [Google Scholar] [CrossRef] [PubMed]
- Fritsch, B.; Reis, J.; Martinowich, K.; Schambra, H.M.; Ji, Y.; Cohen, L.G.; Lu, B. Direct current stimulation promotes BDNF-dependent synaptic plasticity: Potential implications for motor learning. Neuron 2010, 66, 198–204. [Google Scholar] [CrossRef] [PubMed]
- Fridriksson, J.; Elm, J.; Stark, B.C.; Basilakos, A.; Rorden, C.; Sen, S.; George, M.S.; Gottfried, M.; Bonilha, L. BDNF genotype and tDCS interaction in aphasia treatment. Brain Stimul. 2018, 11, 1276–1281. [Google Scholar] [CrossRef] [PubMed]
- Brunoni, A.R.; Nitsche, M.A.; Bolognini, N.; Bikson, M.; Wagner, T.; Merabet, L.; Edwards, D.J.; Valero-Cabre, A.; Rotenberg, A.; Pascual-Leone, A.; et al. Clinical research with transcranial direct current stimulation (tDCS): Challenges and future directions. Brain Stimul. 2012, 5, 175–195. [Google Scholar] [CrossRef]
- Warburton, E.; Price, C.J.; Swinburn, K.; Wise, R.J.S. Mechanisms of recovery from aphasia: Evidence from positron emission tomography studies. J. Neurol. Neurosurg. Psychiatry 1999, 66, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Biou, E.; Cassoudesalle, H.; Cogné, M.; Sibon, I.; De Gabory, I.; Dehail, P.; Aupy, J.; Glize, B. Transcranial direct current stimulation in post-stroke aphasia rehabilitation: A systematic review. Ann. Phys. Rehabil. Med. 2019, 62, 104–121. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, C.; Wagner, S.; Burger, M.; Van Rienen, U.; Wolters, C. Impact of uncertain head tissue conductivity in the optimization of transcranial direct current stimulation for an auditory target. J. Neural Eng. 2015, 12, 046028. [Google Scholar] [CrossRef] [PubMed]
- Datta, A.; Bikson, M.; Fregni, F. Transcranial direct current stimulation in patients with skull defects and skull plates: High-resolution computational FEM study of factors altering cortical current flow. NeuroImage 2010, 52, 1268–1278. [Google Scholar] [CrossRef] [PubMed]
- Wagner, T.; Fregni, F.; Eden, U.; Ramos-Estebanez, C.; Grodzinsky, A.; Zahn, M.; Pascual-Leone, A. Transcranial magnetic stimulation and stroke: A computer-based human model study. NeuroImage 2006, 30, 857–870. [Google Scholar] [CrossRef] [PubMed]
| Participant | Age (Years) | Sex | Lesion Size (mL) | TPO (Months) | Educ (Years) | AQ | LQ | CQ | SS | Comp | Rpt | Nmg | Polarity vs. Sham | Stimulation Site |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| WAB-R AQ > 55 | ||||||||||||||
| 1 JONRA | 46.1 | M | 66.9 | 6.3 | 16 | 70.3 | 64.0 | 70.9 | 12 | 8.0 | 6.6 | 8.6 | A-tDCS | MFG |
| 2 SHAER | 51.5 | M | 80.3 | 29.2 | 16 | 61.3 | 61.9 | 69.7 | 10 | 9.1 | 4.7 | 6.9 | A-tDCS | FP |
| 3 LEELO | 57.1 | F | 92.8 | 38.9 | 17 | 74.3 | 74.8 | 76.2 | 14 | 8.8 | 7.4 | 7.0 | C-tDCS | FP |
| 4 TONMA | 57.8 | F | 94.7 | 50.9 | 16 | 63.9 | 71.1 | 73.5 | 12 | 9.4 | 5.7 | 4.9 | C-tDCS | M1 |
| 5 PEACA | 55.3 | F | 76.6 | 155.7 | 12 | 70.1 | 65.1 | 69.8 | 12 | 8.7 | 7.3 | 7.1 | S-tDCS | MFG |
| 6 PIWTO | 61.4 | M | 155.8 | 53.3 | 13 | 75.3 | 65.8 | 70.3 | 13 | 8.1 | 9.5 | 7.1 | S-tDCS | SMG |
| WAB-R AQ < 55 | ||||||||||||||
| 7 ANDJA | 46.1 | M | 118.6 | 35.6 | 12 | 45.2 | 46.4 | 54.2 | 8 | 5.5 | 4.8 | 4.3 | A-tDCS | MFG |
| 8 HOWSH | 55.7 | F | 136.4 | 9.2 | 17 | 47.1 | 37.4 | 42.2 | 9 | 6.1 | 5.6 | 2.9 | A-tDCS | MFG |
| 9 KARYA | 58.8 | M | 46.5 | 6.2 | 16 | 38.7 | 37.6 | 45.8 | 9 | 5.2 | 4.1 | 1.1 | C-tDCS | IFG |
| 10 TRAWI | 64.9 | M | 83.3 | 18.6 | 18 | 44.0 | 58.0 | 61.6 | 7 | 8.3 | 2.8 | 3.9 | C-tDCS | IFG |
| 11 KANJO | 71.1 | M | 24.5 | 6.2 | 16 | 54.3 | 60.3 | 65.6 | 7 | 7.6 | 4.8 | 7.8 | S-tDCS | MFG |
| 12 BUTFR | 54.7 | M | 56.1 | 7.3 | 18 | 22.3 | 30.0 | 38.4 | 4 | 4.8 | 1.9 | 0.5 | S-tDCS | M1 |
| Side Effect | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Tingling/Itching | Fatigue | Headache | Dizzy | Dry Mouth | ||||||||||||
| ID | Arm * | Number of Sessions 1 | Avg 2 | Week 3 | Number of Sessions | Avg | Week | Number of Sessions | Avg | Week | Number of Sessions | Avg | Week | Number of Sessions | Avg | Week |
| 1 | A | 6 | 2.2 | 1–2 | 6 | 2.9 | 4–6 | - | - | - | - | - | - | 1 | 1.0 | 1 |
| 2 | A | 3 | 5.3 | 1 | 7 | 3.0 | 3–5 | - | - | - | 1 | 1.0 | 3 | - | - | - |
| 3 | C | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 4 | C | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 5 | S | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 6 | S | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 7 | A | - | - | - | 10 | 4.1 | 2–6 | - | - | - | 1 | 2.0 | 1 | - | - | - |
| 8 | A | 24 | 3.0 | 1–6 | - | - | - | 1 | 1.5 | 4 | - | - | - | - | - | - |
| 9 | C | 13 | 4.6 | 1–5 | 5 | 2.0 | 1,3,4 | 1 | 2.0 | 3 | 13 | 2.0 | 2–6 | - | - | - |
| 10 | C | - | - | - | 3 | 1.9 | 1,2,4 | 2 | 1.5 | 1,4 | - | - | - | - | - | - |
| 11 | S | 6 | 1.0 | 1–3 | 2 | 6.0 | 1,6 | 1 | 2.0 | 1 | - | - | - | 2 | 1.0 | 1,3 |
| 12 | S | 14 | 3.4 | 1–3 | - | - | - | - | - | - | - | - | - | - | - | - |
| Group | Number of Participants | AQ Pre-Post | AQ Pre-F | LQ Pre-Post | LQ Pre-F | CETI Pre-Post | CETI Pre-F |
|---|---|---|---|---|---|---|---|
| A-tDCS | 4 | 5.2 (1.7) | 7.4 (2.2) | 5.7 (1.8) | 6.6 (1.4) 1 | 13.9 (13.3) 1 | 14.5 (17.6) 1 |
| C-tDCS | 4 | 5.4 (2.5) | 5.7 (5.6) | 3.7 (2.6) | 6.2 (2.6) | 17.2 (2.3) | 20.8 (2.1) |
| S-tDCS | 4 | 4.8 (7.7) | 3.1 (8.4) | 4.6 (2.2) | 3.3 (4.0) | 7.2 (6.3) | 10.2 (8.0) |
| Participant | Polarity vs. Sham | AQ Pre | AQ Post | AQ F | AQ Pre-Post | AQ Pre-F | LQ Pre | LQ Post | LQ F | LQ Pre-Post | LQ Pre-F | CETI Pre | CETI Post | CETI F | CETI Pre-Post | CETI Pre-F |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| WAB-R AQ > 55 | ||||||||||||||||
| 1 | A-tDCS | 70.3 | 76.6 | 77.1 | 6.3 | 6.8 | 64.0 | 67.8 | 69.7 | 3.8 | 5.7 | 47.6 | 76.9 | 82.3 | 29.3 | 34.7 |
| 2 | A-tDCS | 61.3 | 68.3 | 71.7 | 7.0 | 10.4 | 61.9 | 66.4 | 70.1 | 4.5 | 8.2 | 33.3 | 38.9 | 39.8 | 5.7 | 6.6 |
| 3 | C-tDCS | 74.3 | 77.7 | 75.5 | 3.4 | 1.2 | 74.8 | 77.4 | 79.6 | 2.6 | 4.8 | 45.9 | 60.2 | 65.8 | 14.3 | 19.9 |
| 4 | C-tDCS | 63.9 | 67.6 | 71.5 | 3.7 | 7.6 | 71.1 | 72.1 | 74.4 | 1.0 | 3.3 | 54.8 | 71.3 | 75.1 | 16.4 | 20.3 |
| 5 | S-tDCS | 70.1 | 72.7 | 69.5 | 2.6 | -0.6 | 65.1 | 67.9 | 63.2 | 2.8 | -1.9 | 53.8 | 54.9 | 55.9 | 1.1 | 2.1 |
| 6 | S-tDCS | 75.3 | 73.7 | 71.4 | -1.6 | -3.9 | 65.8 | 69.7 | 68.1 | 3.9 | 2.3 | 47.6 | 50.6 | 54.3 | 3.0 | 6.8 |
| WAB-R AQ < 55 | ||||||||||||||||
| 7 | A-tDCS | 45.2 | 49.1 | 52.2 | 3.9 | 7.0 | 46.4 | 53.4 | 52.2 | 7.0 | 5.8 | 70.1 | 76.9 | 72.4 | 6.9 | 2.3 |
| 8 | A-tDCS | 47.1 | 50.7 | 52.4 | 3.6 | 5.3 | 37.4 | 44.8 | NA | 7.4 | NA | NA | NA | NA | NA | NA |
| 9 | C-tDCS | 38.7 | 44.5 | 39.8 | 5.8 | 1.1 | 37.6 | 44.4 | 46.6 | 6.8 | 9.0 | 70.4 | 88.8 | 94.3 | 18.3 | 23.9 |
| 10 | C-tDCS | 44.0 | 52.7 | 56.8 | 8.7 | 12.8 | 58.0 | 62.4 | 65.8 | 4.4 | 7.8 | 44.2 | 63.8 | 63.4 | 19.6 | 19.2 |
| 11 | S-tDCS | 54.3 | 70.3 | 69.6 | 16 | 15.3 | 60.3 | 68.1 | 66.8 | 7.8 | 6.5 | 24.7 | 39.1 | 45.7 | 14.4 | 21.0 |
| 12 | S-tDCS | 22.3 | 24.6 | 24.4 | 2.3 | 1.9 | 30.0 | 33.9 | 36.3 | 3.9 | 6.3 | 38.2 | 48.7 | 48.4 | 10.5 | 10.2 |
| Group | Number of Participants | Oral Reading Accuracy Gain (SD) at Post- Treatment | Oral Reading Accuracy Gain (SD) at Follow-Up Testing | Oral Reading Rate Gain (SD) at Post-Treatment | Oral Reading Rate Gain (SD) at Follow-Up Testing |
|---|---|---|---|---|---|
| A-tDCS | 4 | 47.3 (34.7) | 25.7 (0.6) 1 | 63.2 (62.8) | 120.7 (74.3) 1 |
| C-tDCS | 4 | 47.6 (37.5) | 30.2 (47.3) | 43.7 (53.4) | 140.4 (96.3) |
| S-tDCS | 4 | 19.9 (22.8) | 32.5 (12.7) | 21.4 (55.2) | 15.8 (41.6) |
| Participant | Polarity vs. Sham | Oral Reading Accuracy Gain (ES) at Post-Treatment | Oral Reading Accuracy Gain (ES) at Follow-Up Testing | Oral Reading Rate Gain (ES) at Post-Treatment | Oral Reading Rate Gain (ES) at Follow-Up Testing |
|---|---|---|---|---|---|
| WAB-R AQ > 55 | |||||
| 1 | A-tDCS | 36.2 (5.2) | 26.0 (3.8) | 58.0 (4.5) | 28.2 (2.2) |
| 2 | A-tDCS | 91.5 (8.1) | NA | 47.7 (9.5) | NA |
| 3 | C-tDCS | 17.2 (2.3) | 20.1 (2.7) | 15.8 (2.2) | 134.7 (18.9) |
| 4 | C-tDCS | 89.5 (4.8) | 92.0 (5.0) | 13.7 (0.7) | 110.3 (5.0) |
| 5 | S-tDCS | 40.0 (6.0) | 27.8 (4.2) | 67.7 (11.7) | 50.5 (8.8) |
| 6 | S-tDCS | 26.6 (4.2) | 21.2 (3.4) | 55.1 (11.2) | −27.3 (−5.5) |
| WAB-R AQ < 55 | |||||
| 7 | A-tDCS | 8.7 (0.4) | 25.2 (1.0) | −5.0 (0.0) | 455.0 (14.2) |
| 8 | A-tDCS | 52.5 (5.8) | NA | 146.7 (6.0) | NA |
| 9 | C-tDCS | 14.5 (0.7) | 30.8 (1.6) | 124.0 (6.7) | 353.6 (19.0) |
| 10 | C-tDCS | 69.3 (2.4) | −22.5 (−0.8) | 20.8 (0.4) | 31.3 (0.6) |
| 11 | S-tDCS | 25.7 (2.4) | 30.1 (2.8) | 16.5 (2.2) | 1.2 (0.2) |
| 12 | S-tDCS | −13.0 (−5.4) | 50.4 (21.2) | −54.0 (−1.6) | −54.0 (−1.6) |
| Participant | Polarity vs. Sham | Lesion Size (mL) | Perilesional Activation | Left/Right Ratio | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Task 1 | Task 2 | Task 3 | Task 1 | Task 2 | Task 3 | |||||||||
| Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | |||
| WAB-R AQ > 55 | ||||||||||||||
| 1 | A-tDCS | 66.9 | 57 | 0 | 0 | 0 | 135 | 122 | 0.74 | 0.56 | 0.91 | 0.76 | 0.56 | 0.86 |
| 2 | A-tDCS | 80.3 | 339 | 92 | 86 | 6 | 142 | 284 | 0.75 | 0.71 | 0.68 | 4.31 | 0.47 | 0.70 |
| 3 | C-tDCS | 92.8 | 816 | 375 | 45 | 2151 | 103 | 2244 | 0.68 | 0.75 | 0.51 | 1.53 | 0.81 | 1.60 |
| 4 | C-tDCS | 94.7 | 34 | 81 | 317 | 114 | 357 | 434 | 0.76 | 0.86 | 0.35 | 0.66 | 0.58 | 0.65 |
| 5 | S-tDCS | 76.6 | 768 | 641 | 181 | 117 | 216 | 600 | 0.45 | 0.69 | 0.35 | 0.44 | 0.53 | 0.71 |
| 6 | S-tDCS | 155.8 | 238 | 238 | 24 | 0 | 154 | 412 | 0.67 | 0.43 | 0.12 | 0.17 | 0.39 | 0.81 |
| WAB-R AQ < 55 | ||||||||||||||
| 7 | A-tDCS | 118.6 | 227 | 467 | NA | NA | NA | NA | 0.89 | 0.94 | NA | NA | NA | NA |
| 8 | A-tDCS | 136.4 | 234 | 494 | 62 | 670 | 48 | 539 | 0.97 | 0.67 | 0.84 | 1.67 | 0.58 | 0.80 |
| 9 | C-tDCS | 46.5 | 121 | 28 | 0 | 36 | 255 | 43 | 0.60 | 0.78 | 0.73 | 0.28 | 0.64 | 0.32 |
| 10 | C-tDCS | 83.3 | 98 | 139 | 19 | 71 | 96 | 147 | 0.91 | 0.85 | 1.02 | 0.74 | 1.07 | 0.93 |
| 11 | S-tDCS | 24.5 | 57 | 0 | 0 | 0 | 135 | 122 | 1.27 | 1.00 | 0.78 | 1.08 | 1.12 | 0.80 |
| 12 | S-tDCS | 56.1 | 0 | 88 | 205 | 380 | 232 | 292 | 0.12 | 1.76 | 0.25 | 2.56 | 0.83 | 5.09 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cherney, L.R.; Babbitt, E.M.; Wang, X.; Pitts, L.L. Extended fMRI-Guided Anodal and Cathodal Transcranial Direct Current Stimulation Targeting Perilesional Areas in Post-Stroke Aphasia: A Pilot Randomized Clinical Trial. Brain Sci. 2021, 11, 306. https://doi.org/10.3390/brainsci11030306
Cherney LR, Babbitt EM, Wang X, Pitts LL. Extended fMRI-Guided Anodal and Cathodal Transcranial Direct Current Stimulation Targeting Perilesional Areas in Post-Stroke Aphasia: A Pilot Randomized Clinical Trial. Brain Sciences. 2021; 11(3):306. https://doi.org/10.3390/brainsci11030306
Chicago/Turabian StyleCherney, Leora R., Edna M. Babbitt, Xue Wang, and Laura L. Pitts. 2021. "Extended fMRI-Guided Anodal and Cathodal Transcranial Direct Current Stimulation Targeting Perilesional Areas in Post-Stroke Aphasia: A Pilot Randomized Clinical Trial" Brain Sciences 11, no. 3: 306. https://doi.org/10.3390/brainsci11030306
APA StyleCherney, L. R., Babbitt, E. M., Wang, X., & Pitts, L. L. (2021). Extended fMRI-Guided Anodal and Cathodal Transcranial Direct Current Stimulation Targeting Perilesional Areas in Post-Stroke Aphasia: A Pilot Randomized Clinical Trial. Brain Sciences, 11(3), 306. https://doi.org/10.3390/brainsci11030306






