Economic Evaluation in Neurological Physiotherapy: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Bibliographic Search
2.2. Selection Criteria
2.3. Data Extraction
3. Results
3.1. Search Results
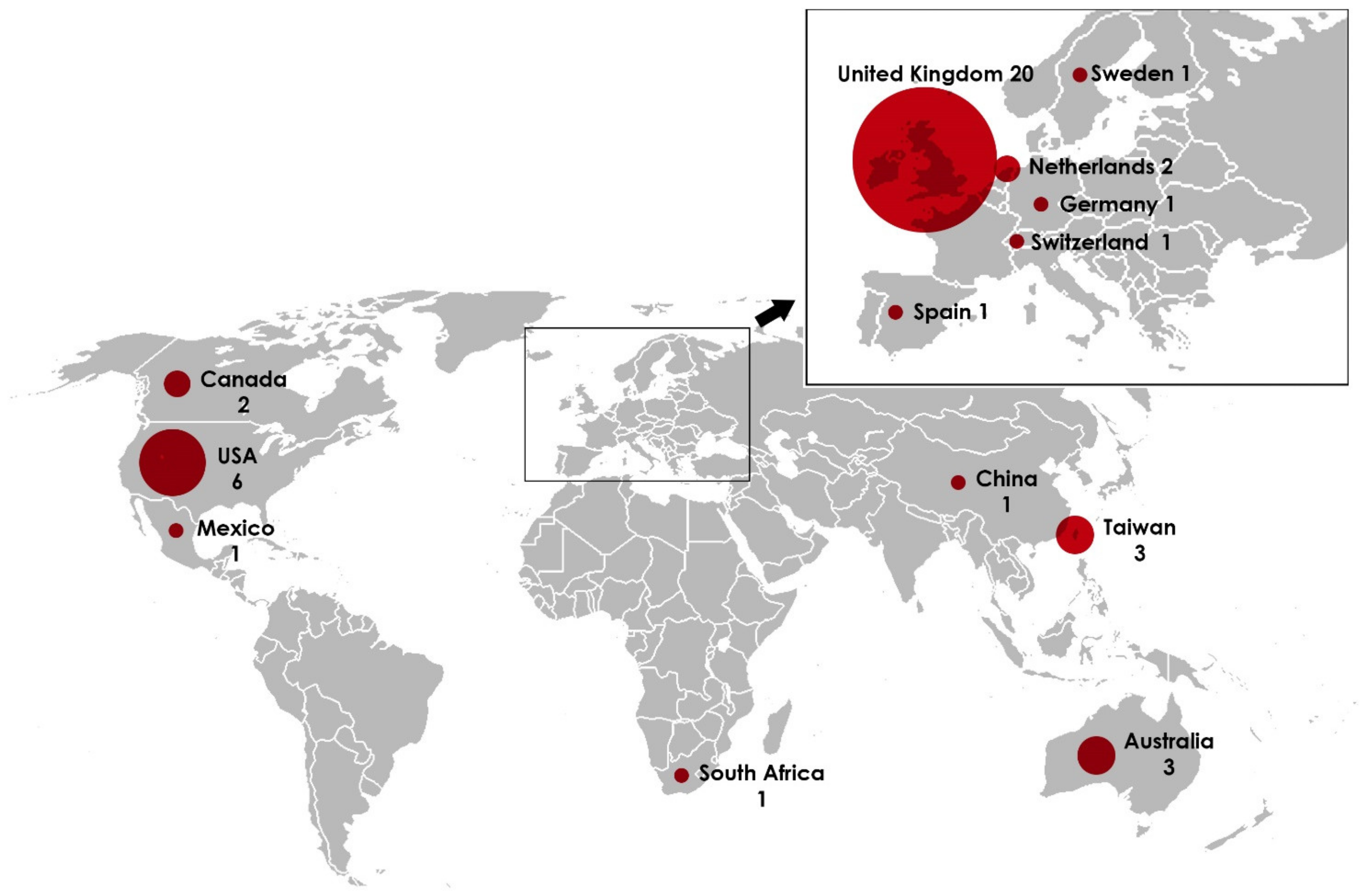
3.2. Description of Studies Included
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sackett, D.L.; Rosenberg, W.M.; Gray, J.A.; Haynes, R.B.; Richardson, W.S. Evidence based medicine: What it is and what it isn’t. BMJ 1996, 312, 71–72. [Google Scholar] [CrossRef]
- Guyatt, G.; Rennie, D.; Meade, M.O.; Cook, D.J. Users’ Guides to the Medical Literature: A Manual for Evidence-Based Clinical Practice, 3rd ed.; McGraw-Hill Education: New York, NY, USA, 2015. [Google Scholar]
- Finch, E.; Brooks, D.; Stratford, P.W. Physical Rehabilitation Outcome Measures: A Guide to Enhanced Clinical Decision Making; Canadian Physiotherapy Association: Ottawa, ON, Canada, 2002. [Google Scholar]
- Kennedy, N.; Stokes, E. Discussion paper—Why physiotherapy needs economics. Phys. Ther. Rev. 2003, 8, 27–30. [Google Scholar] [CrossRef]
- WCPT. Policy Statement: Description of Physical Therapy. Available online: http://www.wcpt.org/policy/ps-descriptionPT#appendix_1 (accessed on 10 July 2020).
- Turrillas, M.; Sitjà-Rabert, M.; Pardo, H.; Casamitjana, J.V.; Fort-Vanmeerhaeghe, A.; Fernández, A.M.; Cebrià Iranzo, M.A.; Bonfill Cosp, X. Identification and description of controlled clinical trials published in physiotherapy journals in Spain. J. Eval. Clin. Pract. 2017, 23, 29–36. [Google Scholar] [CrossRef]
- Drummond, M.F.; Sculpher, M.J.; Claxton, K.; Stoddart, G.L.; Torrance, G.W. Methods for the Economic Evaluation of Health Care Programmes, 4th ed.; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- Perspective York. York Health Economics Consortium. 2016. Available online: https://yhec.co.uk/glossary/perspective/ (accessed on 12 July 2020).
- Tai, B.B.; Bae, Y.H.; Le, Q.A. A systematic review of health economic evaluation studies using the patient’s perspective. Value Health 2016, 19, 903–908. [Google Scholar] [CrossRef] [PubMed]
- Drummond, M.; Weatherly, H.; Ferguson, B. Economic evaluation of health interventions. BMJ 2008, 29, a1204. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Chapter 4: Conclusions and recommendations. In Neurological Disorders: Public Health Challenges; WHO Press, World Health Organization: Geneva, Switzerland, 2006; pp. 176–181. [Google Scholar]
- Urrutia, G.; Bonfill, X. PRISMA declaration: A proposal to improve the publication of systematic reviews and meta-analyses. Med. Clin. 2010, 135, 507–511. [Google Scholar]
- Barnhoorn, K.; Staal, J.B.; van Dongen, R.T.; Frölke, J.P.M.; Klomp, F.P.; van de Meent, H.; Adang, E.; Nijhuis-van der Sanden, M.W. Pain Exposure Physical Therapy versus conventional treatment in complex regional pain syndrome type 1-a cost-effectiveness analysis alongside a randomized controlled trial. Clin. Rehabil. 2018, 32, 790–798. [Google Scholar] [CrossRef] [PubMed]
- Den Hollander, M.; Heijnders, N.; de Jong, J.R.; Vlaeyen, J.W.; Smeets, R.J.; Goossens, M.E. Exposure in vivo versus pain-contingent physical therapy in complex regional pain syndrome type I: A cost-effectiveness analysis. Int. J. Technol. Assess Health Care 2018, 34, 400–409. [Google Scholar] [CrossRef]
- Hester, J.M.; Guin, P.R.; Danek, G.D.; Thomas, J.R.; Titsworth, W.L.; Reed, R.K.; Vasilopoulos, T.; Fahy, B.G. The economic and clinical impact of sustained use of a progressive mobility program in a neuro-ICU. Crit. Care Med. 2017, 45, 1037–1044. [Google Scholar] [CrossRef]
- Turner-Stokes, L.; Williams, H.; Bill, A.; Bassett, P.; Sephton, K. Cost-efficiency of specialist inpatient rehabilitation for working-aged adults with complex neurological disabilities: A multicentre cohort analysis of a national clinical data Set. BMJ Open. 2016, 6, e010238. [Google Scholar] [CrossRef] [PubMed]
- Ademi, Z.; Gloy, V.; Glinz, D.; Raatz, H.; Van Stiphout, J.; Bucher, H.C.; Schwenkglenks, M. Cost-effectiveness of primarily surgical versus primarily conservative treatment of acute and subacute radiculopathies due to intervertebral disc herniation from the Swiss perspective. Swiss Med. Wkly. 2016, 146, w14382. [Google Scholar] [CrossRef]
- Adie, K.; Schofield, C.; Berrow, M.; Wingham, J.; Humfryes, J.; Pritchard, C.; James, M.; Allison, R. Does the use of Nintendo Wii SportsTM improve arm function? Trial of WiiTM in stroke: A randomized controlled trial and economics analysis. Clin. Rehabil. 2016, 31, 173–185. [Google Scholar] [CrossRef]
- Alberts, J.L.; Modic, M.T.; Udeh, B.L.; Zimmerman, N.; Cherian, K.; Lu, X.; Gray, R.; Figler, R.; Russman, A.; Linder, S.M. A technology enabled concussion care pathway reduces costs and enhances care. Phys. Ther. 2020, 100, 136–148. [Google Scholar] [CrossRef]
- Allen, L.; John-Baptiste, A.; Meyer, M.; Richardson, M.; Speechley, M.; Ure, D.; Markle-Reid, M.; Teasell, R. Assessing the impact of a home-based stroke rehabilitation programme: A cost-effectiveness study. Disabil. Rehabil. 2019, 41, 2060–2065. [Google Scholar] [CrossRef]
- Ashburn, A.; Pickering, R.; McIntosh, E.; Hulbert, S.; Rochester, L.; Roberts, H.C.; Nieuwboer, A.; Kunkel, D.; Goodwin, V.A.; Lamb, S.E.; et al. Exercise-and strategy-based physiotherapy-delivered intervention for preventing repeat falls in people with Parkinson’s: The PDSAFE RCT. Health Technol. Assess 2019, 23, 1–147. [Google Scholar] [CrossRef] [PubMed]
- Bhattarai, N.; McMeekin, P.; Vale, L.; Rodgers, H.; Shaw, L.; Cant, R.; Cant, R.; Drummond, A.; Ford, G.A.; Forster, A.; et al. A trial to evaluate an extended rehabilitation service for stroke patients (EXTRAS): Economic evaluation. Int. J. Stroke. 2018, 13, 2–9. [Google Scholar]
- Bustamante Valles, K.; Montes, S.; Madrigal, M.J.; Burciaga, A.; Martínez, M.E.; Johnson, M.J. Technology-assisted stroke rehabilitation in Mexico: A pilot randomized trial comparing traditional therapy to circuit training in a robot/technology-assisted therapy gym. J. Neuroeng. Rehabil. 2016, 13, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Butler, A.; Housley, S.; Wu, D.; Richards, K.; Garlow, A.; Ducote, K.; Howard, A.; Thomas, T. Effect of home-based rehabilitation on access to cost effective therapy for rural veteran stroke survivors. Arch. Phys. Med. Rehabil. 2017, 98, e58–e59. [Google Scholar] [CrossRef]
- Chen, C.M.; Yang, Y.H.; Lee, M.; Chen, K.H.; Huang, S.S. Economic evaluation of transferring first-stroke survivors to rehabilitation wards: A 10-year longitudinal, population-based study. Top. Stroke Rehabil. 2019, 27, 8–14. [Google Scholar] [CrossRef]
- Christofi, G.; Chandratheva, A.; Walters, C.; Bretherton, E.; Yeardley, V.; Lally, D.; Brealey, R.; Warwick, H.; Tahtis, B.; Meechin, S.; et al. Integrated commissioning in London. Feasibility of a neurorehabilitation step down unit targeting patients from acute stroke units ready or «near ready» for early supported discharge. Eur. Stroke J. 2016, 1, 206–207. [Google Scholar]
- Clarke, C.E.; Patel, S.; Ives, N.; Rick, C.E.; Woolley, R.; Wheatley, K.; Walker, M.F.; Zhu, S.; Kandiyali, R.; Yao, G.; et al. Clinical effectiveness and cost-effectiveness of physiotherapy and occupational therapy versus no therapy in mild to moderate Parkinson’s disease: A large pragmatic randomised controlled trial (PD REHAB). Health Technol. Assess. 2016, 20, 1–96. [Google Scholar] [PubMed]
- Collins, M.; Clifton, E.; Wijck, F.; Mead, G.E. Cost-effectiveness of physical fitness training for stroke survivors. J. R. Coll. Physicians Edinb. 2018, 48, 62–68. [Google Scholar] [CrossRef]
- Cooney, M.T.; Carroll, A. Cost effectiveness of inpatient rehabilitation in patients with brain injury. Clin. Med. 2016, 16, 109–113. [Google Scholar] [CrossRef]
- Crotty, M.; van den Berg, M.; Liu, E.; van Wegen, E.K.; Kwakkel, G. Cost-effectiveness of caregiver-mediated exercises combined with e-health services after stroke. Cerebrovasc. Dis. 2016, 42, 156. [Google Scholar]
- Dean, S.G.; Poltawski, L.; Forster, A.; Taylor, R.S.; Spencer, A.; James, M.; Allison, R.; Stevens, S.; Norris, M.; Shepherd, A.I.; et al. Community-based rehabilitation training after stroke: Results of a pilot randomised controlled trial (ReTrain) investigating acceptability and feasibility. BMJ Open. 2018, 8, e018409. [Google Scholar] [CrossRef] [PubMed]
- Farag, I.; Sherrington, C.; Hayes, A.; Canning, C.G.; Lord, S.R.; Close, J.C.T.; Fung, V.S.; Howard, K. Economic evaluation of a falls prevention exercise program among people with Parkinson’s disease. Mov. Disord. 2015, 31, 53–61. [Google Scholar] [CrossRef]
- Farr, W.J.; Green, D.; Bremner, S.; Male, I.; Gage, H.; Bailey, S.; Speller, S.; Colville, V.; Jackson, M.; Memon, A.; et al. Feasibility of a randomised controlled trial to evaluate home-based virtual reality therapy in children with cerebral palsy. Disabil. Rehabil. 2019, 25, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Freeman, J.; Hendrie, W.; Jarrett, L.; Hawton, A.; Barton, A.; Dennett, R.; Jones, B.; Zajicek, J.; Creanor, S. Assessment of a home-based standing frame programme in people with progressive multiple sclerosis (SUMS): A pragmatic, multi-centre, randomised, controlled trial and cost-effectiveness analysis. Lancet Neurol. 2019, 18, 736–747. [Google Scholar] [CrossRef]
- George, P. Early rehabilitation in aneurysmal subarachnoid hemorrhage patients is associated with better cognitive outcomes and shorter ICU stay. Stroke 2019, 50, 555. [Google Scholar] [CrossRef]
- Hesse, S.; Buschfort, R.; Hess, A.; Kabbert, N.; Werner, C. Effect on arm function and cost of robot-assisted group therapy in subacute patients with stroke and a moderately to severely affected arm: A randomized controlled trial. Clin. Rehabil. 2014, 20, 67–73. [Google Scholar] [CrossRef]
- Hind, D.; Parkin, J.; Whitworth, V.; Rex, S.; Young, T.; Hampson, L.; Sheehan, J.; Maguire, C.; Cantrill, H.; Scott, E.; et al. Aquatic therapy for children with Duchenne muscular dystrophy: A pilot feasibility randomised controlled trial and mixed-methods process evaluation. Health Technol. Assess. 2017, 21, 1–120. [Google Scholar] [PubMed]
- Ho, T.H.; Yang, F.C.; Lin, R.C.; Chien, W.C.; Chung, C.H.; Chiang, S.L.; Chou, C.H.; Tsai, C.K.; Tsai, C.L.; Lin, Y.K.; et al. Impact of virtual reality-based rehabilitation on functional outcomes in patients with acute stroke: A retrospective case-matched study. J. Neurol. 2019, 266, 589–597. [Google Scholar] [CrossRef]
- Hunter, S.M.; Johansen-Berg, H.; Ward, N.; Kennedy, N.C.; Chandler, E.; Weir, C.J.; Rothwell, J.; Wing, A.M.; Grey, M.J.; Barton, G.; et al. Functional strength training and movement performance therapy for upper limb recovery early poststroke-efficacy, neural correlates, predictive markers, and cost-effectiveness: FAST-INdiCATE Trial. Front. Neurol. 2017, 8, 733. [Google Scholar] [CrossRef]
- Joseph, C.; Brodin, N.; Leavy, B.; Hagströmer, M.; Löfgren, N.; Franzén, E. Cost-effectiveness of the HiBalance training program for elderly with Parkinson’s disease: Analysis of data from a randomized controlled trial. Clin. Rehabil. 2019, 33, 222–232. [Google Scholar] [CrossRef]
- Juckes, F.M.; Marceniuk, G.; Seary, C.; Stevenson, V.L. A cohort study of functional electrical stimulation in people with multiple sclerosis demonstrating improvements in quality of life and cost-effectiveness. Clin. Rehabil. 2019, 33, 1163–1170. [Google Scholar] [CrossRef]
- Lamb, S.E.; Mistry, D.; Alleyne, S.; Atherton, N.; Brown, D.; Copsey, B.; Dosanjh, S.; Finnegan, S.; Fordham, B.; Griffiths, F.; et al. Aerobic and strength training exercise programme for cognitive impairment in people with mild to moderate dementia: The DAPA RCT. Health Technol. Assess. 2018, 22, 1–202. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Harmer, P. Economic evaluation of a Tai Ji Quan intervention to reduce falls in people with Parkinson disease, Oregon, 2008–2011. Prev. Chronic Dis. 2015, 12, e120. [Google Scholar] [CrossRef]
- Lloréns, R.; Noé, E.; Colomer, C.; Alcañiz, M. Effectiveness, usability, and cost-benefit of a virtual reality-based telerehabilitation program for balance recovery after stroke: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2015, 96, 418–425. [Google Scholar] [CrossRef] [PubMed]
- Louw, Q.; Twizeyemariya, A.; Grimmer, K.; Leibbrandt, D. Estimating the costs and benefits of stroke rehabilitation in South Africa. J. Eval. Clin. Pract. 2019, 26, 1181–1187. [Google Scholar] [CrossRef] [PubMed]
- McClurg, D.; Harris, F.; Goodman, K.; Doran, S.; Hagen, S.; Treweek, S.; Norton, C.; Coggrave, M.; Norrie, J.; Rauchhaus, P.; et al. Abdominal massage plus advice, compared with advice only, for neurogenic bowel dysfunction in MS: A RCT. Health Technol. Assess. 2018, 22, 1–134. [Google Scholar] [CrossRef]
- Morris, M.E.; Taylor, N.F.; Watts, J.J.; Evans, A.; Horne, M.; Kempster, P.; Danoudis, M.; McGinley, J.; Martin, C.; Menz, H.B. A home program of strength training, movement strategy training and education did not prevent falls in people with Parkinson’s disease: A randomised trial. J. Physiother. 2017, 63, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Paganoni, S.; van de Rijn, M.; Drake, K.; Burke, K.; Doyle, M.; Ellrodt, A.S.; Nicholson, K.; Atassi, N.; de Marchi, F.; Babu, S.; et al. Adjusted cost analysis of video televisits for the care of people with amyotrophic lateral sclerosis. Muscle Nerve. 2019, 60, 147–154. [Google Scholar] [CrossRef]
- Renfrew, L.M.; Paul, L.; McFadyen, A.; Rafferty, D.; Moseley, O.; Lord, A.C.; Bowers, R.; Mattison, P. The clinical- and cost-effectiveness of functional electrical stimulation and ankle-foot orthoses for foot drop in Multiple Sclerosis: A multicentre randomized trial. Clin. Rehabil. 2019, 33, 1150–1162. [Google Scholar] [CrossRef]
- Rodgers, H.; Bosomworth, H.; Krebs, H.I.; van Wijck, F.; Howel, D.; Wilson, N.; Aird, L.; Alvarado, N.; Andole, S.; Cohen, D.L.; et al. Robot assisted training for the upper limb after stroke (RATULS): A multicentre randomised controlled trial. Lancet 2019, 394, 51–62. [Google Scholar] [CrossRef]
- Rodgers, H.; Howel, D.; Bhattarai, N.; Cant, R.; Drummond, A.; Ford, G.A.; Forster, A.; Francis, R.; Hills, K.; Laverty, A.M.; et al. Evaluation of an extended stroke rehabilitation service (EXTRAS): A randomized controlled trial and economic analysis. Stroke 2019, 50, 3561–3568. [Google Scholar] [CrossRef]
- Shen, L.; Zheng, J. Clinical economic evaluation of post-stroke rehabilitation at the acute stage in tertiary hospital. Eur. Stroke J. 2019, 4, 239. [Google Scholar]
- Tam, A.; Mac, S.; Isaranuwatchai, W.; Bayley, M. Cost-effectiveness of a high-intensity rapid access outpatient stroke rehabilitation program. Int. J. Rehabil. Res. 2018, 42, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Tosh, J.; Dixon, S.; Carter, A.; Daley, A.; Petty, J.; Roalfe, A.; Sharrack, B.; Saxton, J.M. Cost effectiveness of a pragmatic exercise intervention (EXIMS) for people with multiple sclerosis: Economic evaluation of a randomised controlled trial. Mult. Scler. 2014, 20, 1123–1130. [Google Scholar] [CrossRef]
- Wang, C.Y.; Chen, Y.R.; Hong, J.P.; Chan, C.C.; Chang, L.C.; Shi, H.Y. Rehabilitative post-acute care for stroke patients delivered by per-diem payment system in different hospitalization paths: A Taiwan pilot study. Int. J. Qual Health Care. 2017, 29, 779–784. [Google Scholar] [CrossRef]
- Malone, C.; Barnabas, R.V.; Buist, D.S.M.; Tiro, J.A.; Winer, R.L. Cost-effectiveness studies of HPV self-sampling: A systematic review. Prev. Med. 2020, 132, 105953. [Google Scholar] [CrossRef]
- Brauer, C.A.; Neumann, P.J.; Rosen, A.B. Trends in cost effectiveness analyses in orthopaedic surgery. Clin. Orthop Relat Res. 2007, 457, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Mohit, B.; Cohen, J.T. Trends of cost-effectiveness studies in sleep medicine. Sleep Med. 2019, 53, 176–180. [Google Scholar] [CrossRef]
- Feigin, V.L.; Nguyen, G.; Cercy, K.; Johnson, C.O.; Alam, T.; Parmar, P.G. BD 2016 Lifetime Risk of Stroke Collaborators. Global, Regional, and Country-Specific Lifetime Risks of Stroke, 1990 and 2016. N. Engl. J. Med. 2018, 379, 2429–2437. [Google Scholar] [PubMed]
- Kotterba, S. Sleep disorders in neurological diseases. Nervenarzt 2015, 86, 759–770. [Google Scholar] [CrossRef]
- Johnson, C.O.; Nguyen, M.; Roth, G.A.; Nichols, E.; Alam, T.; Abate, D. Global, regional, and national burden of stroke, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 439–458. [Google Scholar] [CrossRef]
- Hardie, K.; Hankey, G.J.; Jamrozik, K.; Broadhurst, R.J.; Anderson, C. Ten-year risk of first recurrent stroke and disability after first-ever stroke in the Perth Community Stroke Study. Stroke 2004, 35, 731–735. [Google Scholar] [CrossRef]
- Hankey, G.J.; Jamrozik, K.; Broadhurst, R.J.; Forbes, S.; Anderson, C.S. Long-term disability after first-ever stroke and related prognostic factors in the Perth Community Stroke Study, 1989–1990. Stroke 2002, 33, 1034–1040. [Google Scholar] [CrossRef]
- Jönsson, A.C.; Delavaran, H.; Iwarsson, S.; Ståhl, A.; Norrving, B.; Lindgren, A. Functional status and patient-reported outcome 10 years after stroke: The Lund Stroke Register. Stroke 2014, 45, 1784–1790. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Shi, Y.Z.; Zhang, N.; Wang, S.; Ungvari, G.S.; Ng, C.H.; Wang, Y.L.; Zhao, X.Q.; Wang, Y.J.; Wang, C.X. The Disability Rate of 5-Year Post-Stroke and Its Correlation Factors: A National Survey in China. PLoS ONE 2016, 11, e0165341. [Google Scholar]
- Vos, T.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1211–1259. [Google Scholar] [CrossRef]
- Hay, S.I.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1260–1344. [Google Scholar] [CrossRef]
- Stroke Association. State of the Nation: Stroke Statistics 2017. Available online: https://www.stroke.org.uk/resources/state-nation-stroke-statistics (accessed on 11 September 2020).
- Siegel, J.E.; Torrance, G.W.; Russell, L.B.; Luce, B.R.; Weinstein, M.C.; Gold, M.R. Guidelines for pharmacoeconomic studies. Recommendations from the panel on cost effectiveness in health and medicine. Panel on cost Effectiveness in Health and Medicine. Pharmacoeconomics 1997, 11, 159–168. [Google Scholar] [CrossRef] [PubMed]
- NICE. Our Principles. Available online: https://www.nice.org.uk/about/who-we-are/our-principles (accessed on 7 May 2020).
- Queen’s Printer of Acts of Parliament. Health Soc. Care Act. 2012. Available online: http://www.legislation.gov.uk/ukpga/2012/7/section/233/enacted (accessed on 7 May 2020).



| Author | Year | Country | Pathology | Type of Analysis | Perspective | Effect Measurement |
|---|---|---|---|---|---|---|
| Ademi et al. [17] | 2016 | Switzerland | Radiculopathy | Cost-utility analysis | Healthcare payer/Societal | QALY a |
| Adie et al. [18] | 2016 | United Kingdom | Stroke | Cost-utility analysis | Payer | QALY |
| Alberts et al. [19] | 2019 | United States | Concussion | Partial evaluation | Healthcare payer | - |
| Allen et al. [20] | 2019 | Canada | Stroke | Cost-utility analysis | Payer | QALY |
| Ashburn et al. [21] | 2019 | United Kingdom | Parkinson | Cost-utility analysis | Payer | QALY |
| Barnhoorn et al. [13] | 2018 | Netherlands | Complex regional pain syndrome | Cost-effectiveness analysis Cost-utility analysis | Healthcare payer + travel expenses | Disability and pain QALY |
| Bhattarai et al. [22] | 2018 | United Kingdom | Stroke | Cost-effectiveness Cost-utility | Payer | NEADL b QALY |
| Bustamante et al. [23] | 2016 | Mexico | Stroke | Partial evaluation | Healthcare payer | - |
| Butler et al. [24] | 2017 | United States | Stroke | Partial evaluation | - | - |
| Chen et al. [25] | 2019 | Taiwan | Stroke | Cost-effectiveness analysis | Healthcare payer + co-payment | Years of life |
| Christofi et al. [26] | 2016 | United Kingdom | Stroke | Partial evaluation | Healthcare payer | - |
| Clarke et al. [27] | 2016 | United Kingdom | Parkinson | Cost-effectiveness analysis Cost-utility analysis | Payer | HRQL c QALY |
| Collins et al. [28] | 2018 | United Kingdom | Stroke | Cost-effectiveness analysis Cost-utility analysis | Healthcare payer | HRQL QALY |
| Cooney et al. [29] | 2016 | United Kingdom | Stroke | Partial evaluation | Healthcare payer | - |
| Crotty et al. [30] | 2016 | Australia | Stroke | Cost-effectiveness analysis | Healthcare payer | Readmission avoided |
| Dean et al. [31] | 2018 | United Kingdom | Stroke | Cost-effectiveness analysis Cost-utility analysis | Healthcare payer + travel expenses | HRQL QALY |
| den Hollander et al. [14] | 2018 | Netherlands | Complex regional pain syndrome | Cost-effectiveness analysis Cost-utility analysis | Societal | HRQL QALY |
| Farag et al. [32] | 2015 | Australia | Parkinson | Cost-effectiveness analysis Cost-utility analysis | Healthcare payer | Falls and mobility QALY |
| Farr et al. [33] | 2019 | United Kingdom | CCP d | Partial evaluation | Healthcare payer | |
| Freeman et al. [34] | 2019 | United Kingdom | Multiple sclerosis | Cost-utility analysis | Payer/Societal | QALY |
| George et al. [35] | 2019 | United States | Stroke | Partial evaluation | Healthcare payer | |
| Hesse et al. [36] | 2014 | Germany | Stroke | Partial evaluation | Healthcare payer | |
| Hester et al. [15] | 2017 | United States | Heterogeneous group | Partial evaluation | Healthcare payer | - |
| Hind et al. [37] | 2017 | United Kingdom | Duchenne muscular dystrophy | Partial evaluation | Healthcare payer + co-payment | - |
| Ho et al. [38] | 2019 | Taiwan | Stroke | Cost-effectiveness analysis | Healthcare payer | Clinical stroke scales |
| Hunter et al. [39] | 2017 | United Kingdom | Stroke | Cost-utility analysis | Payer | QALY |
| Joseph et al. [40] | 2019 | Sweden | Parkinson | Cost-effectiveness analysis Cost-utility analysis | Societal | Balance and gait QALY |
| Juckes et al. [41] | 2019 | United Kingdom | Multiple sclerosis | Cost-utility analysis | Healthcare payer | QALY |
| Lamb et al. [42] | 2018 | United Kingdom | Dementia | Cost-utility analysis | Payer | QALY |
| Li et al. [43] | 2015 | United States | Parkinson | Cost-effectiveness analysis Cost-utility analysis | Societal | Fall avoided QALY |
| Llorens et al. [44] | 2014 | Spain | Stroke | Partial evaluation | Healthcare payer + travel expenses | - |
| Louw et al. [45] | 2019 | South Africa | Stroke | Cost-benefit analysis | Payer | - |
| McClrurg et al. [46] | 2018 | United Kingdom | Multiple sclerosis | Cost-utility analysis | Healthcare payer/Patient | QALY |
| Morris et al. [47] | 2017 | Australia | Parkinson | Cost-minimization analysis | Healthcare payer | Fall avoided |
| Paganoni et al. [48] | 2019 | United States | ALS e | Cost-effectiveness analysis | Healthcare payer/Patient | Perceived utility |
| Renfrew et al. [49] | 2019 | United Kingdom | Multiple sclerosis | Cost-utility analysis | Payer | QALY |
| Rodgers et al. [50] | 2019 | United Kingdom | Stroke | Cost-utility analysis | Payer | QALY |
| Rodgers et al. [51] | 2019 | United Kingdom | Stroke | Cost-utility analysis | Payer | QALY |
| Shen et al. [52] | 2019 | China | Stroke | Cost-effectiveness analysis | Healthcare payer | Barthel, Berg and NIHSS f |
| Tam et al. [53] | 2018 | Canada | Stroke | Cost-effectiveness analysis | Healthcare payer | Hospitalization day avoided |
| Tosh et al. [54] | 2014 | United Kingdom | Multiple sclerosis | Cost-utility analysis | Payer | QALY |
| Turner-Stokes et al. [16] | 2016 | United Kingdom | Heterogeneous group | Partial evaluation | Societal | |
| Wang et al. [55] | 2017 | Taiwan | Stroke | Partial evaluation | Healthcare payer | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Álvarez, D.; Sempere-Rubio, N.; Faubel, R. Economic Evaluation in Neurological Physiotherapy: A Systematic Review. Brain Sci. 2021, 11, 265. https://doi.org/10.3390/brainsci11020265
García-Álvarez D, Sempere-Rubio N, Faubel R. Economic Evaluation in Neurological Physiotherapy: A Systematic Review. Brain Sciences. 2021; 11(2):265. https://doi.org/10.3390/brainsci11020265
Chicago/Turabian StyleGarcía-Álvarez, David, Núria Sempere-Rubio, and Raquel Faubel. 2021. "Economic Evaluation in Neurological Physiotherapy: A Systematic Review" Brain Sciences 11, no. 2: 265. https://doi.org/10.3390/brainsci11020265
APA StyleGarcía-Álvarez, D., Sempere-Rubio, N., & Faubel, R. (2021). Economic Evaluation in Neurological Physiotherapy: A Systematic Review. Brain Sciences, 11(2), 265. https://doi.org/10.3390/brainsci11020265