Digital Biomarkers in Multiple Sclerosis
Abstract
:1. Introduction
2. Digital Biomarkers
2.1. Definition of Digital Biomarkers
2.2. Challenges of Digital Biomarkers
2.3. Classification of Digital Biomarkers
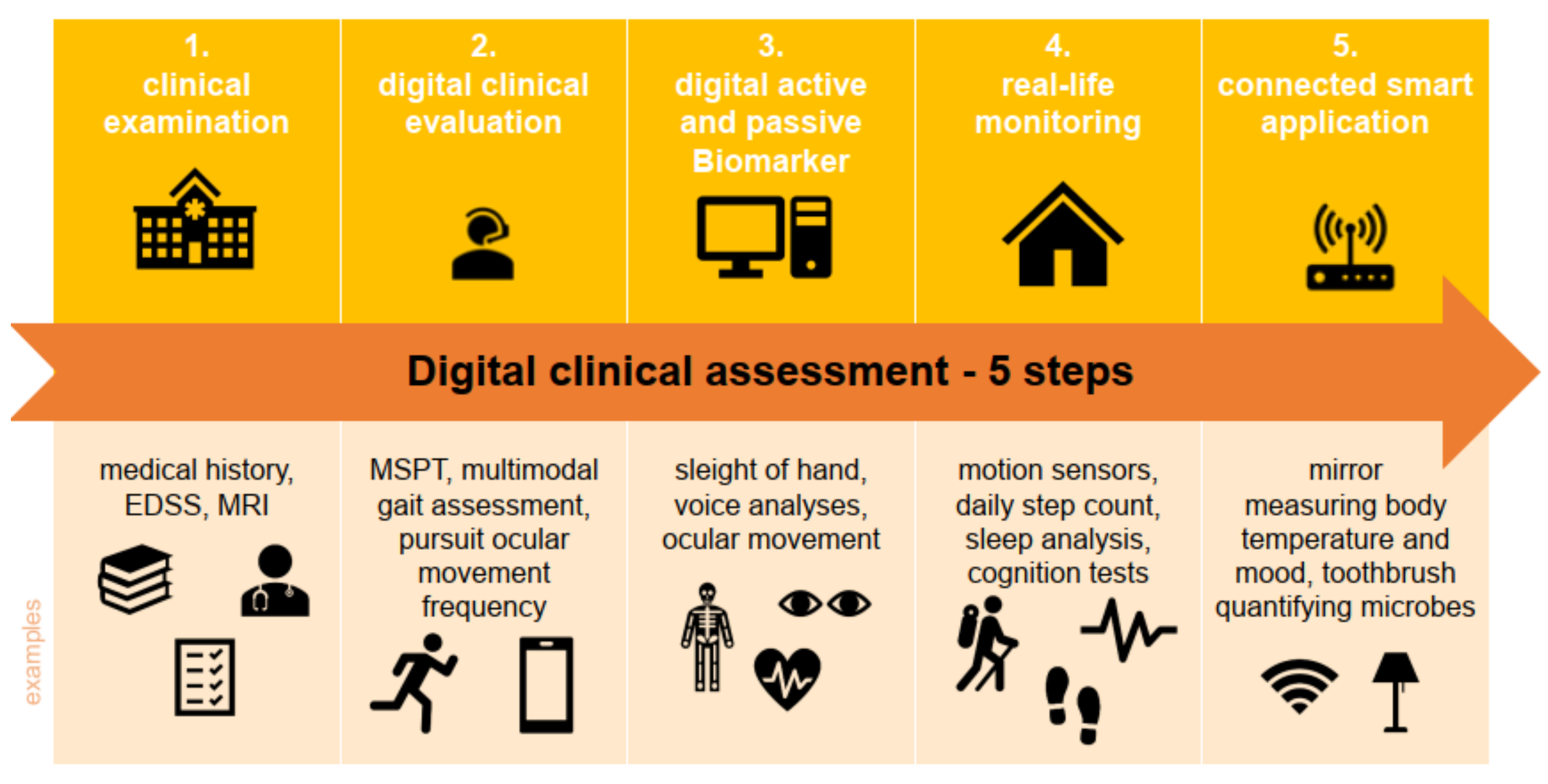
2.4. Clinical Digital Biomarkers in Multiple Sclerosis
3. Clinical Digital Biomarker by Functional Systems
3.1. Vision
3.2. Brainstem
3.3. Upper Extremity Motor Function
3.4. Lower Extremity Motor Function/Gait
3.4.1. Lower Extremity Function in MS Research
3.4.2. Lower Extremity Function in the Clinic
3.4.3. Lower Extremity Function at Home
3.5. Coordination/Balance
3.6. Cognition
Dual-Tasking
4. Collection of Digital Biomarkers
4.1. Smartphones and Smartphone Applications
4.2. Digital Questionnaires in MS
4.3. Digital Data Collection in MS
4.4. Magnet Resonance Imaging
4.5. The Future of Digital Biomarkers
5. Data Analysis
6. Digital Twins
7. Conclusions/Summary
Author Contributions
Funding
Conflicts of Interest
References
- Ziemssen, T.; Kern, R.; Thomas, K. Multiple Sclerosis: Clinical Profiling and Data Collection as Prerequisite for Personal-ized Medicine Approach. BMC Neurol. 2016, 16, 124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ziemssen, T. Multiple sclerosis beyond EDSS: Depression and fatigue. J. Neurol. Sci. 2009, 277, S37–S41. [Google Scholar] [CrossRef]
- Kourtis, L.; Regele, O.B.; Wright, J.M.; Jones, G.B. Digital biomarkers for Alzheimer’s disease: The mobile/wearable devices opportunity. NPJ Digit. Med. 2019, 2, 9. [Google Scholar] [CrossRef] [PubMed]
- Gold, M.; Amatniek, J.; Carrillo, M.C.; Cedarbaum, J.M.; Hendrix, J.A.; Miller, B.B.; Robillard, J.; Rice, J.J.; Soares, H.; Tome, M.B.; et al. Digital technologies as biomarkers, clinical outcomes assessment, and recruitment tools in Alzheimer’s disease clinical trials. Alzheimer’s Dement. Transl. Res. Clin. Interv. 2018, 4, 234–242. [Google Scholar] [CrossRef]
- Rykov, Y.; Thach, T.-Q.; Bojic, I.; Christopoulos, G.; Car, J. Digital Biomarkers for Depression Screening With Wearable Devices: Cross-sectional Study With Machine Learning Modeling. JMIR mHealth uHealth 2021, 9, e24872. [Google Scholar] [CrossRef] [PubMed]
- Ziemssen, T.; Akgün, K.; Brück, W. Molecular biomarkers in multiple sclerosis. J. Neuroinflamm. 2019, 16, 272. [Google Scholar] [CrossRef] [Green Version]
- Coravos, A.; Khozin, S.; Mandl, K.D. Erratum: Author Correction: Developing and Adopting Safe and Effective Digital Biomarkers to Improve Patient Outcomes. NPJ Digit. Med. 2019, 2, 40. [Google Scholar] [CrossRef]
- Dorsey, E.R.; Papapetropoulos, S.; Xiong, M.; Kieburtz, K. The First Frontier: Digital Biomarkers for Neurodegenerative Disorders. Digit. Biomark. 2017, 1, 6–13. [Google Scholar] [CrossRef]
- Wang, T.; Azad, T.; Rajan, R. The Emerging Influence of Digital Biomarkers on Healthcare. Available online: https://rockhealth.com/insights/the-emerging-influence-of-digital-biomarkers-on-healthcare/ (accessed on 18 October 2021).
- Babrak, L.M.; Menetski, J.; Rebhan, M.; Nisato, G.; Zinggeler, M.; Brasier, N.; Baerenfaller, K.; Brenzikofer, T.; Baltzer, L.; Vogler, C.; et al. Traditional and Digital Biomarkers: Two Worlds Apart? Digit. Biomark. 2019, 3, 92–102. [Google Scholar] [CrossRef]
- Bielekova, B.; Martin, R. Development of biomarkers in multiple sclerosis. Brain 2004, 127, 1463–1478. [Google Scholar] [CrossRef] [Green Version]
- Ziemssen, T.; Medin, J.; Couto, C.A.; Mitchell, C.R. Multiple Sclerosis in the Real World: A Systematic Review of Fin-golimod as a Case Study. Autoimmun. Rev. 2017, 16, 355–376. [Google Scholar] [CrossRef] [PubMed]
- Noffs, G.; Perera, T.; Kolbe, S.C.; Shanahan, C.J.; Boonstra, F.M.C.; Evans, A.; Butzkueven, H.; van der Walt, A.; Vogel, A.P. What speech can tell us: A systematic review of dysarthria characteristics in Multiple Sclerosis. Autoimmun. Rev. 2018, 17, 1202–1209. [Google Scholar] [CrossRef] [Green Version]
- Hoff, J.M.; Dhayalan, M.; Midelfart, A.; Tharaldsen, A.R.; Bo, L. Visual Dysfunction in Multiple Sclerosis. Tidsskr. Nor. Legeforening 2019, 139. [Google Scholar] [CrossRef] [Green Version]
- Green, A.J.; McQuaid, S.; Hauser, S.L.; Allen, I.V.; Lyness, R. Ocular pathology in multiple sclerosis: Retinal atrophy and inflammation irrespective of disease duration. Brain 2010, 133, 1591–1601. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martínez-Lapiscina, E.H.; Arnow, S.; Wilson, J.A.; Saidha, S.; Preiningerova, J.L.; Oberwahrenbrock, T.; Brandt, A.U.; Pablo, L.E.; Guerrieri, S.; González-Suárez, I.; et al. Retinal thickness measured with optical coherence tomography and risk of disability worsening in multiple sclerosis: A cohort study. Lancet Neurol. 2016, 15, 574–584. [Google Scholar] [CrossRef] [Green Version]
- Britze, J.; Frederiksen, J.L. Optical coherence tomography in multiple sclerosis. Eye 2018, 32, 884–888. [Google Scholar] [CrossRef] [Green Version]
- Balcer, L.J.; Raynowska, J.; Nolan, R.; Galetta, S.L.; Kapoor, R.; Benedict, R.; Phillips, G.; LaRocca, N.; Hudson, L.; Rudick, R.; et al. Validity of low-contrast letter acuity as a visual performance outcome measure for multiple sclerosis. Mult. Scler. J. 2017, 23, 734–747. [Google Scholar] [CrossRef]
- Fisher, J.B.; Jacobs, D.A.; Markowitz, C.E.; Galetta, S.L.; Volpe, N.J.; Nano-Schiavi, M.L.; Baier, M.L.; Frohman, E.M.; Winslow, H.; Frohman, T.C. Relation of Visual Function to Retinal Nerve Fiber Layer Thickness in Multiple Sclerosis. Ophthalmology 2006, 113, 324–332. [Google Scholar] [CrossRef]
- Maggio, M.G.; Russo, M.; Cuzzola, M.F.; Destro, M.; La Rosa, G.; Molonia, F.; Bramanti, P.; Lombardo, G.; De Luca, R.; Calabrò, R.S. Virtual reality in multiple sclerosis rehabilitation: A review on cognitive and motor outcomes. J. Clin. Neurosci. 2019, 65, 106–111. [Google Scholar] [CrossRef]
- Frohman, E.M.; Frohman, T.C.; Zee, D.S.; McColl, R.; Galetta, S. The neuro-ophthalmology of multiple sclerosis. Lancet Neurol. 2005, 4, 111–121. [Google Scholar] [CrossRef]
- Niestroy, A.; Rucker, J.; Leigh, R.J. Neuro-ophthalmologic aspects of multiple sclerosis: Using eye movements as a clinical and experimental tool. Clin. Ophthalmol. 2007, 1, 267–272. [Google Scholar] [PubMed]
- De Santi, L.; Lanzafame, P.; Spano’, B.; D’Aleo, G.; Bramanti, A.; Bramanti, P.; Marino, S. Pursuit ocular movements in multiple sclerosis: A video-based eye-tracking study. Neurol. Sci. 2010, 32, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Gibaldi, A.; Vanegas, M.; Bex, P.J.; Maiello, G. Evaluation of the Tobii EyeX Eye tracking controller and Matlab toolkit for research. Behav. Res. Methods 2017, 49, 923–946. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sheehy, C.K.; Beaudry-Richard, A.; Bensinger, E.; Theis, J.; Green, A.J. Methods to Assess Ocular Motor Dysfunction in Multiple Sclerosis. J. Neuro-Ophthalmol. 2018, 38, 488–493. [Google Scholar] [CrossRef]
- Reulen, J.P.; Sanders, E.A.; Hogenhuis, L.A. Eye Movement Disorders in Multiple Sclerosis and Optic Neuritis. Brain 1983, 106, 121–140. [Google Scholar] [CrossRef]
- Nygaard, G.O.; Benavent, S.A.D.R.; Harbo, H.F.; Laeng, B.; Sowa, P.; Damangir, S.; Nilsen, K.B.; Etholm, L.; Tønnesen, S.; Kerty, E.; et al. Eye and hand motor interactions with the Symbol Digit Modalities Test in early multiple sclerosis. Mult. Scler. Relat. Disord. 2015, 4, 585–589. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fielding, J.; Kilpatrick, T.; Millist, L.; White, O. Antisaccade performance in patients with multiple sclerosis. Cortex 2009, 45, 900–903. [Google Scholar] [CrossRef]
- Fielding, J.; Kilpatrick, T.; Millist, L.; White, O. Control of visually guided saccades in multiple sclerosis: Disruption to higher-order processes. Neuropsychology 2009, 47, 1647–1653. [Google Scholar] [CrossRef]
- Finke, C.; Pech, L.M.; Sömmer, C.; Schlichting, J.; Stricker, S.; Endres, M.; Ostendorf, F.; Ploner, C.J.; Brandt, A.U.; Paul, F. Dynamics of Saccade Parameters in Multiple Sclerosis Pa-tients with Fatigue. J. Neurol. 2012, 259, 2656–2663. [Google Scholar] [CrossRef]
- Tao, L.; Wang, Q.; Liu, D.; Wang, J.; Zhu, Z.; Feng, L. Eye tracking metrics to screen and assess cognitive impairment in patients with neurological disorders. Neurol. Sci. 2020, 41, 1697–1704. [Google Scholar] [CrossRef]
- Fielding, J.; Kilpatrick, T.; Millist, L.; White, O. Multiple sclerosis: Cognition and saccadic eye movements. J. Neurol. Sci. 2009, 277, 32–36. [Google Scholar] [CrossRef]
- Grillini, A.; Renken, R.J.; Vrijling, A.C.; Heutink, J.; Cornelissen, F.W. Eye Movement Evalua-tion in Multiple Sclerosis and Parkinson’s Disease Using a Standardized Oculomotor and Neuro-Ophthalmic Disorder As-sessment (Sonda). Front. Neurol. 2020, 11, 971. [Google Scholar] [CrossRef]
- Merson, R.M.; Rolnick, M.I. Speech-language Pathology and Dysphagia in Multiple Sclerosis. Phys. Med. Rehabil. Clin. N. Am. 1998, 9, 631–641. [Google Scholar] [CrossRef]
- Hartelius, L.; Runmarker, B.; Andersen, O. Prevalence and Characteristics of Dysarthria in a Multiple-Sclerosis Inci-dence Cohort: Relation to Neurological Data. Folia Phoniatr. Logop. 2000, 52, 160–177. [Google Scholar] [CrossRef] [PubMed]
- Beukelman, D.R.; Kraft, G.H.; Freal, J. Expressive Communication Disorders in Persons with Multiple Sclerosis: A Sur-vey. Arch. Phys. Med. Rehabil. 1985, 66, 675–677. [Google Scholar]
- Stipancic, K.L.; Tjaden, K.; Wilding, G. Comparison of Intelligibility Measures for Adults with Parkinson’s Disease, Adults with Multiple Sclerosis, and Healthy Controls. J. Speech Lang. Hear. Res. 2016, 59, 230–238. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rusz, J.; Benova, B.; Ruzickova, H.; Novotny, M.; Tykalova, T.; Hlavnicka, J.; Uher, T.; Vaneckova, M.; Andelova, M.; Novotna, K.; et al. Characteristics of motor speech phenotypes in multiple sclerosis. Mult. Scler. Relat. Disord. 2018, 19, 62–69. [Google Scholar] [CrossRef]
- Greeley, H.P.; Friets, E.; Wilson, J.P.; Raghavan, S.; Picone, J.; Berg, J. Detecting Fatigue from Voice Using Speech Recog-nition. Proceedings 2006 IEEE International Symposium on Signal Processing and Information Technology, Vancouver, BC, Canada, 27–30 August 2006; pp. 567–571. [Google Scholar] [CrossRef]
- Amunts, J.; Camilleri, J.A.; Eickhoff, S.B.; Heim, S.; Weis, S. Executive functions predict verbal fluency scores in healthy participants. Sci. Rep. 2020, 10, 11141. [Google Scholar] [CrossRef] [PubMed]
- Mathew, M.M.; Bhat, J.S. Soft Phonation Index—A Sensitive Parameter? Indian J. Otolaryngol. Head Neck Surg. 2009, 61, 127–130. [Google Scholar] [CrossRef] [Green Version]
- Feijó, A.V.; Parente, M.A.; Behlau, M.; Haussen, S.; De Veccino, M.C.; Martignago, B.C.D.F. Acoustic analysis of voice in multiple sclerosis patients. J. Voice 2004, 18, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Dogan, M.; Midi, I.; Yazıcı, M.A.; Kocak, I.; Günal, D.; Sehitoglu, M.A. Objective and Subjective Evaluation of Voice Quality in Multiple Sclerosis. J. Voice 2007, 21, 735–740. [Google Scholar] [CrossRef]
- Hartelius, L.; Buder, E.H.; Strand, E.A. Long-Term Phonatory Instability in Individuals with Multiple Sclerosis. J. Speech Lang. Hear. Res. 1997, 40, 1056–1072. [Google Scholar] [CrossRef] [PubMed]
- Vizza, P.; Mirarchi, D.; Tradigo, G.; Redavide, M.; Bossio, R.B.; Veltri, P. Vocal signal analysis in patients affected by Multiple Sclerosis. Procedia Comput. Sci. 2017, 108, 1205–1214. [Google Scholar] [CrossRef]
- Noffs, G.; Boonstra, F.M.C.; Perera, T.; Kolbe, S.C.; Stankovich, J.; Butzkueven, H.; Evans, A.; Vogel, A.; Van Der Walt, A. Acoustic Speech Analytics Are Predictive of Cerebellar Dysfunction in Multiple Sclerosis. Cerebellum 2020, 19, 691–700. [Google Scholar] [CrossRef]
- Fagherazzi, G.; Fischer, A.; Ismael, M.; Despotovic, V. Voice for Health: The Use of Vocal Biomarkers from Research to Clinical Practice. Digit. Biomark. 2021, 5, 78–88. [Google Scholar] [CrossRef]
- Zhang, L.; Duvvuri, R.; Chandra, K.K.L.; Nguyen, T.; Ghomi, R.H. Automated Voice Biomarkers for Depression Symp-toms Using an Online Cross-Sectional Data Collection Initiative. Depress Anxiety 2020, 37, 657–669. [Google Scholar] [CrossRef]
- Cummins, N.; Scherer, S.; Krajewski, J.; Schnieder, S.; Epps, J.; Quatieri, T.F. A review of depression and suicide risk assessment using speech analysis. Speech Commun. 2015, 71, 10–49. [Google Scholar] [CrossRef]
- Henry, J.D.; Beatty, W.W. Verbal fluency deficits in multiple sclerosis. Neuropsychology 2006, 44, 1166–1174. [Google Scholar] [CrossRef] [PubMed]
- Barcellos, L.F.; Bellesis, K.H.; Shen, L.; Shao, X.; Chinn, T.; Frndak, S.; Drake, A.; Bakshi, N.; Marcus, J.; Schaefer, C.; et al. Remote assessment of verbal memory in MS patients using the California Verbal Learning Test. Mult. Scler. J. 2017, 24, 354–357. [Google Scholar] [CrossRef] [PubMed]
- Fischer, J.S. Using the wechsler memory scale-revised to detect and characterize memory deficits in multiple sclerosis. Clin. Neuropsychol. 1988, 2, 149–172. [Google Scholar] [CrossRef]
- Krajewski, J.; Wieland, R.; Batliner, A. An Acoustic Framework for Detecting Fatigue in Speech Based Hu-man-Computer-Interaction; Springer: Berlin/Heidelberg, Germany, 2008; pp. 54–61. [Google Scholar]
- Wallace, G.L.; Holmes, S. Cognitive-linguistic assessment of individuals with multiple sclerosis. Arch. Phys. Med. Rehabil. 1993, 74, 637–643. [Google Scholar] [CrossRef]
- Yozbatıran, N.; Baskurt, F.; Baskurt, Z.; Ozakbas, S.; Idiman, E. Motor assessment of upper extremity function and its relation with fatigue, cognitive function and quality of life in multiple sclerosis patients. J. Neurol. Sci. 2006, 246, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Holper, L.; Coenen, M.; Weise, A.; Stucki, G.; Cieza, A.; Kesselring, J. Characterization of functioning in multiple sclerosis using the ICF. J. Neurol. 2009, 257, 103–113. [Google Scholar] [CrossRef]
- Pellegrino, L.; Coscia, M.; Muller, M.; Solaro, C.; Casadio, M. Evaluating upper limb impairments in multiple sclerosis by exposure to different mechanical environments. Sci. Rep. 2018, 8, 2110. [Google Scholar] [CrossRef] [Green Version]
- Kraft, G.H.; Amtmann, D.; Bennett, S.E.; Finlayson, M.; Sutliff, M.H.; Tullman, M.; Sidovar, M.; Rabinowicz, A.L. As-sessment of Upper Extremity Function in Multiple Sclerosis: Review and Opinion. Postgrad. Med. 2014, 126, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Kahraman, T. Performance Measures for Upper Extremity Functions in Persons with Multiple Sclerosis. Arch. Neuropsychiatry 2018, 55, S41–S45. [Google Scholar] [CrossRef]
- Mollà-Casanova, S.; Llorens, R.; Borrego, A.; Salinas-Martínez, B.; Serra-Añó, P. Validity, reliability, and sensitivity to motor impairment severity of a multi-touch app designed to assess hand mobility, coordination, and function after stroke. J. Neuroeng. Rehabil. 2021, 18, 70. [Google Scholar] [CrossRef]
- Cirstea, M.C.; Mitnitski, A.B.; Feldman, A.G.; Levin, M.F. Interjoint coordination dynamics during reaching in stroke. Exp. Brain Res. 2003, 151, 289–300. [Google Scholar] [CrossRef]
- Ivry, R.; Diedrichsen, J.; Spencer, R.; Hazeltine, E.; Semjen, A. A Cognitive Neuroscience Per-spective on Bimanual Coordination and Interference. In Neuro-Behavioral Determinants of Interlimb Coordination; Springer: Boston, MA, USA, 2004; pp. 259–295. [Google Scholar]
- Lamers, I.; Feys, P. Assessing upper limb function in multiple sclerosis. Mult. Scler. J. 2014, 20, 775–784. [Google Scholar] [CrossRef]
- Tanigawa, M.; Stein, J.; Park, J.; Kosa, P.; Cortese, I.; Bielekova, B. Finger and foot tapping as alternative outcomes of upper and lower extremity function in multiple sclerosis. Mult. Scler. J. Exp. Transl. Clin. 2017, 3, 2055217316688930. [Google Scholar] [CrossRef]
- Floeter, M.K.; Mills, R. Progression in Primary Lateral Sclerosis: A Prospective Analysis. Amyotroph. Lateral Scler. 2009, 10, 339–346. [Google Scholar] [CrossRef] [Green Version]
- Creagh, A.; Simillion, C.; Scotland, A.; Lipsmeier, F.; Bernasconi, C.; Belachew, S.; Van Beek, J.; Baker, M.; Gossens, C.; Lindemann, M.; et al. Smartphone-based remote assessment of upper extremity function for multiple sclerosis using the Draw a Shape Test. Physiol. Meas. 2020, 41, 054002. [Google Scholar] [CrossRef] [PubMed]
- Kontschieder, P.; Dorn, J.F.; Morrison, C.; Corish, R.; Zikic, D.; Sellen, A.; D’Souza, M.; Kamm, C.P.; Burggraaff, J.; Tewarie, P.; et al. Quantifying Pro-gression of Multiple Sclerosis Via Classification of Depth Videos. In International Conference on Medical Image Computing and Computer-Assisted Intervention; Springer: Cham, Switzerland, 2014; pp. 429–437. [Google Scholar]
- Flachenecker, F.; Gassner, H.; Hannik, J.; Lee, D.H.; Flachenecker, P.; Winkler, J.; Eskofier, B.; Linker, R.A.; Klucken, J. Ob-jective Sensor-Based Gait Measures Reflect Motor Impairment in Multiple Sclerosis Patients: Reliability and Clinical Valida-tion of a Wearable Sensor Device. Mult. Scler. Relat. Disord. 2019, 39, 101903. [Google Scholar] [CrossRef]
- Larocca, N.G. Impact of Walking Impairment in Multiple Sclerosis: Perspectives of Patients and Care Partners. Patient 2011, 4, 189–201. [Google Scholar] [CrossRef] [PubMed]
- Bethoux, F. Gait Disorders in Multiple Sclerosis. Contin. Lifelong Learn. Neurol. 2013, 19, 1007–1022. [Google Scholar] [CrossRef]
- Sosnoff, J.J.; Sandroff, B.M.; Motl, R.W. Quantifying Gait Abnormalities in Persons with Multiple Sclerosis with Mini-mal Disability. Gait Posture 2012, 36, 154–156. [Google Scholar] [CrossRef]
- Martin, C.L.; Phillips, B.A.; Kilpatrick, T.; Butzkueven, H.; Tubridy, N.; McDonald, E.; Galea, M. Gait and balance impairment in early multiple sclerosis in the absence of clinical disability. Mult. Scler. J. 2006, 12, 620–628. [Google Scholar] [CrossRef] [PubMed]
- Cameron, M.H.; Wagner, J.M. Gait Abnormalities in Multiple Sclerosis: Pathogenesis, Evaluation, and Advances in Treatment. Curr. Neurol. Neurosci. Rep. 2011, 11, 507–515. [Google Scholar] [CrossRef]
- Trentzsch, K.; Weidemann, M.L.; Torp, C.; Inojosa, H.; Scholz, M.; Haase, R.; Schriefer, D.; Akgün, K.; Ziemssen, T. The Dresden Protocol for Multidimensional Walking Assessment (DMWA) in Clinical Practice. Front. Neurosci. 2020, 14, 582046. [Google Scholar] [CrossRef]
- Shanahan, C.J.; Boonstra, F.M.C.; Lizama, L.E.C.; Strik, M.; Moffat, B.A.; Khan, F.; Kilpatrick, T.J.; Van Der Walt, A.; Galea, M.P.; Kolbe, S.C. Technologies for Advanced Gait and Balance Assessments in People with Multiple Sclerosis. Front. Neurol. 2018, 8, 708. [Google Scholar] [CrossRef] [Green Version]
- Coghe, G.; Corona, F.; Pilloni, G.; Porta, M.; Frau, J.; Lorefice, L.; Fenu, G.; Cocco, E.; Pau, M. Is There Any Relationship between Upper and Lower Limb Impairments in People with Multiple Sclerosis? A Kinematic Quantitative Analysis. Mult. Scler. Int. 2019, 2019, 9149201. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Willimczik, K.; Roth, K. Bewegungslehre; Rowohlt-Taschenbuch-Verlag: Reinbek, Germany, 1988. [Google Scholar]
- Fang, X.; Liu, C.; Jiang, Z. Reference values of gait using APDM movement monitoring inertial sensor system. R. Soc. Open Sci. 2018, 5, 170818. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Washabaugh, E.P.; Kalyanaraman, T.; Adamczyk, P.; Claflin, E.S.; Krishnan, C. Validity and repeatability of inertial measurement units for measuring gait parameters. Gait Posture 2017, 55, 87–93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spain, R.I.; George, R.J.S.; Salarian, A.; Mancini, M.; Wagner, J.M.; Horak, F.B.; Bourdette, D. Body-Worn Motion Sen-sors Detect Balance and Gait Deficits in People with Multiple Sclerosis Who Have Normal Walking Speed. Gait Posture 2012, 35, 573–578. [Google Scholar] [CrossRef] [Green Version]
- Kurtzke, J.F. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology 1983, 33, 1444–1452. [Google Scholar] [CrossRef] [Green Version]
- Block, V.J.; Lizée, A.; Crabtree-Hartman, E.; Bevan, C.J.; Graves, J.S.; Bove, R.; Green, A.J.; Nourbakhsh, B.; Tremblay, M.; Gourraud, P.-A.; et al. Continuous daily assessment of multiple sclerosis disability using remote step count monitoring. J. Neurol. 2017, 264, 316–326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rhodes, J.K.; Schindler, D.; Rao, S.M.; Venegas, F.; Bruzik, E.T.; Gabel, W.; Williams, J.; Phillips, G.A.; Mullen, C.C.; Freiburger, J.L.; et al. Multiple Sclerosis Performance Test: Technical Development and Usability. Adv. Ther. 2019, 36, 1741–1755. [Google Scholar] [CrossRef] [Green Version]
- Rao, S.M.; Leo, G.J.; Bernardin, L.; Unverzagt, F. Cognitive dysfunction in multiple sclerosis: I. Frequency, patterns, and prediction. Neurology 1991, 41, 685–691. [Google Scholar] [CrossRef]
- Kaufman, M.; Moyer, D.; Norton, J. The Significant Change for the Timed 25-Foot Walk in the Multiple Sclerosis Func-tional Composite. Mult. Scler. 2000, 6, 286–290. [Google Scholar] [CrossRef]
- Baier, M.L.; Cutter, G.R.; Rudick, R.A.; Miller, D.; Cohen, J.A.; Weinstock-Guttman, B.; Mass, M.; Balcer, L.J. Low-contrast letter acuity testing captures visual dysfunction in patients with multiple sclerosis. Neurology 2005, 64, 992–995. [Google Scholar] [CrossRef] [PubMed]
- Rudick, R.A.; Miller, D.; Bethoux, F.; Rao, S.M.; Lee, J.C.; Stough, D.; Reece, C.; Schindler, D.; Mamone, B.; Alberts, J. The Multiple Sclerosis Performance Test (Mspt): An Ipad-Based Disability Assessment Tool. J. Vis. Exp. 2014, 88, e51318. [Google Scholar] [CrossRef]
- Sumowski, J.F.; Benedict, R.; Enzinger, C.; Filippi, M.; Geurts, J.J.; Hamalainen, P.; Hulst, H.; Inglese, M.; Leavitt, V.M.; Rocca, M.A.; et al. Cognition in Multiple Sclerosis: State of the Field and Priorities for the Future. Neurology 2018, 90, 278–288. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rao, S.M.; Losinski, G.; Mourany, L.; Schindler, D.; Mamone, B.; Reece, C.; Kemeny, D.; Narayanan, S.; Miller, D.M.; Bethoux, F.; et al. Processing Speed Test: Validation of a Self-Administered, Ipad((R))-Based Tool for Screening Cognitive Dysfunction in a Clinic Setting. Mult. Scler. 2017, 23, 1929–1937. [Google Scholar] [CrossRef] [PubMed]
- Rao, S.M.; Galioto, R.; Sokolowski, M.; McGinley, M.; Freiburger, J.; Weber, M.; Dey, T.; Mourany, L.; Schindler, D.; Reece, C.; et al. Multi-ple Sclerosis Performance Test: Validation of Self-Administered Neuroperformance Modules. Eur. J. Neurol. 2020, 27, 878–886. [Google Scholar] [CrossRef] [PubMed]
- Learmonth, Y.C.; Motl, R.W.; Sandroff, B.M.; Pula, J.H.; Cadavid, D. Validation of patient determined disease steps (PDDS) scale scores in persons with multiple sclerosis. BMC Neurol. 2013, 13, 37. [Google Scholar] [CrossRef] [Green Version]
- Medina, L.D.; Torres, S.; Alvarez, E.; Valdez, B.; Nair, K.V. Patient-Reported Outcomes in Multiple Sclerosis: Validation of the Quality of Life in Neurological Disorders (Neuro-Qol) Short Forms. Mult. Scler. J. Exp. Transl. Clin. 2019, 5, 2055217319885986. [Google Scholar] [CrossRef]
- Cella, D.; Lai, J.S.; Nowinski, C.J.; Victorson, D.; Peterman, A.; Miller, D.; Bethoux, F.; Heinemann, A.; Rubin, S.; Cavazos, J.E.; et al. Neuro-Qol: Brief Measures of Health-Related Quality of Life for Clinical Re-search in Neurology. Neurology 2012, 78, 1860–1867. [Google Scholar] [CrossRef] [Green Version]
- Weidemann, M.L.; Trentzsch, K.; Torp, C.; Ziemssen, T. Enhancing Monitoring of Disease Progression-Remote Sensor-ing in Multiple Sclerosis. Nervenarzt 2019, 90, 1239–1244. [Google Scholar] [CrossRef]
- Block, V.A.; Pitsch, E.; Tahir, P.; Cree, B.A.; Allen, D.D.; Gelfand, J.M. Remote Physical Activity Monitoring in Neuro-logical Disease: A Systematic Review. PLoS ONE 2016, 11, e0154335. [Google Scholar] [CrossRef]
- Balto, J.M.; Kinnett-Hopkins, D.; Motl, R.W. Accuracy and precision of smartphone applications and commercially available motion sensors in multiple sclerosis. Mult. Scler. J. Exp. Transl. Clin. 2, 2055217316634754. [CrossRef] [PubMed] [Green Version]
- Block, V.J.; Bove, R.; Zhao, C.; Garcha, P.; Graves, J.; Romeo, A.R.; Green, A.J.; Allen, D.D.; Hollenbach, J.A.; Olgin, J.E.; et al. Association of Continuous Assessment of Step Count by Remote Monitoring With Disability Progression Among Adults With Multiple Sclerosis. JAMA Netw. Open 2019, 2, e190570. [Google Scholar] [CrossRef]
- Moon, Y.; McGinnis, R.S.; Seagers, K.; Motl, R.W.; Sheth, N.; Wright, J.A., Jr.; Ghaffari, R.; Sosnoff, J.J. Monitoring gait in multiple sclerosis with novel wearable motion sensors. PLoS ONE 2017, 12, e0171346. [Google Scholar] [CrossRef] [PubMed]
- Chitnis, T.; Glanz, B.I.; Gonzalez, C.; Healy, B.C.; Saraceno, T.J.; Sattarnezhad, N.; Diaz-Cruz, C.; Polgar-Turcsanyi, M.; Tummala, S.; Bakshi, R.; et al. Quantifying Neurologic Disease Using Bi-osensor Measurements in-Clinic and in Free-Living Settings in Multiple Sclerosis. NPJ Digit. Med. 2019, 2, 123. [Google Scholar] [CrossRef] [Green Version]
- Daley, M.L.; Swank, R.L. Changes in postural control and vision induced by multiple sclerosis. Agressologie 1983, 24, 327–329. [Google Scholar]
- Cameron, M.H.; Lord, S. Postural Control in Multiple Sclerosis: Implications for Fall Prevention. Curr. Neurol. Neurosci. Rep. 2010, 10, 407–412. [Google Scholar] [CrossRef]
- Matsuda, P.N.; Shumway-Cook, A.; Ciol, M.A.; Bombardier, C.H.; Kartin, D.A. Understanding Falls in Multiple Scle-rosis: Association of Mobility Status, Concerns About Falling, and Accumulated Impairments. Phys. Ther. 2012, 92, 407–415. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gunn, H.; Newell, P.; Haas, B.; Marsden, J.F.; Freeman, J.A. Identification of Risk Factors for Falls in Multiple Sclerosis: A Systematic Review and Meta-Analysis. Phys. Ther. 2013, 93, 504–513. [Google Scholar] [CrossRef]
- Mazumder, R.; Murchison, C.; Bourdette, D.; Cameron, M. Falls in People with Multiple Sclerosis Compared with Falls in Healthy Controls. PLoS ONE 2014, 9, e107620. [Google Scholar] [CrossRef]
- Horak, F.B.; Henry, S.M.; Shumway-Cook, A. Postural Perturbations: New Insights for Treatment of Balance Disor-ders. Phys. Ther. 1997, 77, 517–533. [Google Scholar] [CrossRef]
- Inojosa, H.; Schriefer, D.; Trentzsch, K.; Kloditz, A.; Ziemssen, T. Visual Feedback and Postural Control in Multiple Scle-rosis. J. Clin. Med. 2020, 9, 1291. [Google Scholar] [CrossRef] [PubMed]
- Pollock, A.S.; Durward, B.R.; Rowe, P.J.; Paul, J.P. What Is Balance? Clin. Rehabil. 2000, 14, 402–406. [Google Scholar] [CrossRef]
- Maki, B.E.; McIlroy, W.E. The Role of Limb Movements in Maintaining Upright Stance: The “Change-in-Support” Strategy. Phys. Ther. 1997, 77, 488–507. [Google Scholar] [CrossRef] [PubMed]
- Inojosa, H.; Schriefer, D.; Kloditz, A.; Trentzsch, K.; Ziemssen, T. Balance Testing in Multiple Sclerosis-Improving Neuro-logical Assessment with Static Posturography? Front. Neurol. 2020, 11, 135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- APDM Wearable Technologies Inc. Comprehensive Gait and Balance Analysis. Available online: https://apdm.com/mobility/ (accessed on 18 October 2021).
- Heilmann, F. Dynamische Posturographie—Entwicklung Und Validierung Einer Testbatterie Zur Gleichgewichtsdiagnostik Unter Verwendung Des Posturomeds; Monograph; Martin–Luther–Universität Halle–Wittenberg: Halle, Germany, 2019. [Google Scholar]
- Clark, R.A.; Mentiplay, B.; Pua, Y.-H.; Bower, K.J. Reliability and validity of the Wii Balance Board for assessment of standing balance: A systematic review. Gait Posture 2018, 61, 40–54. [Google Scholar] [CrossRef]
- Gunn, H.; Markevics, S.; Haas, B.; Marsden, J.; Freeman, J. Systematic Review: The Effectiveness of Interventions to Reduce Falls and Improve Balance in Adults With Multiple Sclerosis. Arch. Phys. Med. Rehabil. 2015, 96, 1898–1912. [Google Scholar] [CrossRef]
- Al-Sharman, A.; Khalil, H.; El-Salem, K.; Alghwiri, A.A.; Khazaaleh, S.; Khraim, M. Motor performance improvement through virtual reality task is related to fatigue and cognition in people with multiple sclerosis. Physiother. Res. Int. 2019, 24, e1782. [Google Scholar] [CrossRef]
- Schreck, L.M.; Ryan, S.P.P.; Monaghan, P.G. Cerebellum and cognition in multiple sclerosis. J. Neurophysiol. 2018, 120, 2707–2709. [Google Scholar] [CrossRef]
- Lovera, J.; Kovner, B. Cognitive Impairment in Multiple Sclerosis. Curr. Neurol. Neurosci. Rep. 2012, 12, 618–627. [Google Scholar] [CrossRef] [Green Version]
- Langdon, D.W. Cognition in Multiple Sclerosis. Curr. Opin. Neurol. 2011, 24, 244–249. [Google Scholar] [CrossRef]
- Rao, S.M.; Leo, G.J.; Ellington, L.; Nauertz, T.; Bernardin, L.; Unverzagt, F. Cognitive Dysfunction in Multiple Sclerosis. Ii. Impact on Employment and Social Functioning. Neurology 1991, 41, 692–696. [Google Scholar] [CrossRef]
- Banati, M.; Sandor, J.; Mike, A.; Illes, E.; Bors, L.; Feldmann, A.; Herold, R.; Illes, Z. Social cognition and Theory of Mind in patients with relapsing-remitting multiple sclerosis. Eur. J. Neurol. 2010, 17, 426–433. [Google Scholar] [CrossRef]
- Mitchell, A.J.; Benito-León, J.; González, J.M.; Rivera-Navarro, J. Quality of Life and Its Assessment in Multiple Sclero-sis: Integrating Physical and Psychological Components of Wellbeing. Lancet Neurol. 2005, 4, 556–566. [Google Scholar] [CrossRef]
- Bruce, J.M.; Hancock, L.M.; Arnett, P.; Lynch, S. Treatment Adherence in Multiple Sclerosis: Association with Emotion-al Status, Personality, and Cognition. J. Behav. Med. 2010, 33, 219–227. [Google Scholar] [CrossRef] [PubMed]
- Honarmand, K.; Akbar, N.; Kou, N.; Feinstein, A. Predicting Employment Status in Multiple Sclerosis Patients: The Util-ity of the Ms Functional Composite. J. Neurol. 2011, 258, 244–249. [Google Scholar] [CrossRef]
- Amato, M.P.; Ponziani, G.; Siracusa, G.; Sorbi, S. Cognitive Dysfunction in Early-Onset Multiple Sclerosis: A Reappraisal after 10 Years. Arch. Neurol. 2001, 58, 1602–1606. [Google Scholar] [CrossRef] [Green Version]
- Middleton, R.M.; Pearson, O.R.; Ingram, G.; Craig, E.M.; Rodgers, W.J.; Downing-Wood, H.; Hill, J.; Tuite-Dalton, K.; Roberts, C.; Watson, L.; et al. A Rapid Electronic Cognitive Assessment Measure for Multiple Sclerosis: Validation of Core (Cognitive Reaction), an Electronic Version of the Symbol Digit Modalities Test. J. Med Internet Res. 2020, 22, e18234. [Google Scholar] [CrossRef]
- Langdon, D.W.; Amato, M.P.; Boringa, J.; Brochet, B.; Foley, F.; Fredrikson, S.; Hämäläinen, P.; Hartung, H.P.; Krupp, L.; Penner, I.K.; et al. Recommendations for a Brief International Cognitive Assessment for Multiple Scle-rosis (Bicams). Mult. Scler. 2012, 18, 891–898. [Google Scholar] [CrossRef] [Green Version]
- Bever, C.T.; Grattan, L.; Panitch, H.S.; Johnson, K.P. The Brief Repeatable Battery of Neuropsychological Tests for Mul-tiple Sclerosis: A Preliminary Serial Study. Mult. Scler. J. 1995, 1, 165–169. [Google Scholar] [CrossRef] [PubMed]
- Benedict, R.H.; Fischer, J.S.; Archibald, C.J.; Arnett, P.A.; Beatty, W.W.; Bobholz, J.; Chelune, G.J.; Fisk, J.D.; Langdon, D.; Caruso, L.; et al. Minimal Neuropsychological Assessment of MS Patients: A Consensus Approach. Clin. Neuropsychol. 2002, 16, 381–397. [Google Scholar] [CrossRef] [PubMed]
- Benedict, R.H.; Cookfair, D.; Gavett, R.; Gunther, M.; Munschauer, F.; Garg, N.; Weinstock-Guttman, B. Validity of the minimal assessment of cognitive function in multiple sclerosis (MACFIMS). J. Int. Neuropsychol. Soc. 2006, 12, 549–558. [Google Scholar] [CrossRef]
- Bauer, R.M.; Iverson, G.; Cernich, A.N.; Binder, L.M.; Ruff, R.M.; Naugle, R.I. Computerized Neuropsychological Assessment Devices: Joint Position Paper of the American Academy of Clinical Neuropsychology and the National Academy of Neuropsychology. Arch. Clin. Neuropsychol. 2012, 27, 362–373. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wojcik, C.M.; Beier, M.; Costello, K.; DeLuca, J.; Feinstein, A.; Goverover, Y.; Gudesblatt, M.; Jaworski, M.; Kalb, R.; Kostich, L.; et al. Computerized Neuropsychological Assessment Devices in Multiple Sclerosis: A Systematic Review. Mult. Scler. 2019, 25, 1848–1869. [Google Scholar] [CrossRef] [PubMed]
- Kalb, R.; Beier, M.; Benedict, R.H.; Charvet, L.; Costello, K.; Feinstein, A.; Gingold, J.; Goverover, Y.; Halper, J.; Harris, C.; et al. Recommendations for Cognitive Screening and Man-agement in Multiple Sclerosis Care. Mult. Scler. 2018, 24, 1665–1680. [Google Scholar] [CrossRef] [Green Version]
- Etemadi, Y. Dual task cost of cognition is related to fall risk in patients with multiple sclerosis: A prospective study. Clin. Rehabil. 2016, 31, 278–284. [Google Scholar] [CrossRef]
- Woollacott, M.; Shumway-Cook, A. Attention and the control of posture and gait: A review of an emerging area of research. Gait Posture 2002, 16, 1–14. [Google Scholar] [CrossRef]
- Fritz, N.E.; Kloos, A.D.; Kegelmeyer, D.A.; Kaur, P.; Nichols-Larsen, D.S. Supplementary motor area connectivity and dual-task walking variability in multiple sclerosis. J. Neurol. Sci. 2019, 396, 159–164. [Google Scholar] [CrossRef]
- Krause, I.; Kern, S.; Horntrich, A.; Ziemssen, T. Employment status in multiple sclerosis: Impact of disease-specific and non-disease-specific factors. Mult. Scler. J. 2013, 19, 1792–1799. [Google Scholar] [CrossRef]
- Beste, C.; Mückschel, M.; Paucke, M.; Ziemssen, T. Dual-Tasking in Multiple Sclerosis—Implications for a Cognitive Screening Instrument. Front. Hum. Neurosci. 2018, 12, 24. [Google Scholar] [CrossRef] [Green Version]
- Hamilton, F.; Rochester, L.; Paul, L.; Rafferty, D.; O’Leary, C.P.; Evans, J.J. Walking and talking: An investigation of cognitive—motor dual tasking in multiple sclerosis. Mult. Scler. J. 2009, 15, 1215–1227. [Google Scholar] [CrossRef]
- Butchard-MacDonald, E.; Paul, L.; Evans, J.J. Balancing the Demands of Two Tasks: An Investigation of Cognitive–Motor Dual-Tasking in Relapsing Remitting Multiple Sclerosis. J. Int. Neuropsychol. Soc. 2018, 24, 247–258. [Google Scholar] [CrossRef] [Green Version]
- Monticone, M.; Ambrosini, E.; Fiorentini, R.; Rocca, B.; Liquori, V.; Pedrocchi, A.; Ferrante, S. Reliability of spatial–temporal gait parameters during dual-task interference in people with multiple sclerosis. A cross-sectional study. Gait Posture 2014, 40, 715–718. [Google Scholar] [CrossRef]
- Holtzer, R.; Wang, C.; Verghese, J. Performance Variance on Walking While Talking Tasks: Theory, Findings, and Clini-cal Implications. Age 2014, 36, 373–381. [Google Scholar] [CrossRef] [Green Version]
- Learmonth, Y.C.; Ensari, I.; Motl, R.W. Cognitive Motor Interference in Multiple Sclerosis: Insights from a Systematic Quantitative Review. Arch. Phys. Med. Rehabil. 2017, 98, 1229–1240. [Google Scholar] [CrossRef]
- Downer, M.B.; Kirkland, M.C.; Wallack, E.M.; Ploughman, M. Walking impairs cognitive performance among people with multiple sclerosis but not controls. Hum. Mov. Sci. 2016, 49, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Wajda, D.A.; Sosnoff, J.J. Cognitive-Motor Interference in Multiple Sclerosis: A Systematic Review of Evi-dence, Correlates, and Consequences. BioMed Res. Int. 2015, 2015, 720856. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holtzer, R.; Mahoney, J.; Verghese, J. Intraindividual Variability in Executive Functions but Not Speed of Processing or Conflict Resolution Predicts Performance Differences in Gait Speed in Older Adults. J. Gerontol. Ser. A Boil. Sci. Med. Sci. 2014, 69, 980–986. [Google Scholar] [CrossRef]
- Welford, A. The “Psychological Refractory Period” and the Timing of High Speed Performance: A Review and a Theory. Br. J. Psychol. Gen. Sect. 2011, 43, 2–19. [Google Scholar] [CrossRef]
- Pashler, H. Dual-task interference in simple tasks: Data and theory. Psychol. Bull. 1994, 116, 220–244. [Google Scholar] [CrossRef]
- Böttrich, N.; Mückschel, M.; Dillenseger, A.; Lange, C.; Kern, R.; Ziemssen, T.; Beste, C. On the Reliability of Examining Dual-Tasking Abilities Using a Novel E-Health Device—A Proof of Concept Study in Multiple Sclerosis. J. Clin. Med. 2020, 9, 3423. [Google Scholar] [CrossRef] [PubMed]
- Sim, I. Mobile Devices and Health. N. Engl. J. Med. 2019, 381, 956–968. [Google Scholar] [CrossRef] [PubMed]
- Maillart, E.; Labauge, P.; Cohen, M.; Maarouf, A.; Vukusic, S.; Donzé, C.; Gallien, P.; De Sèze, J.; Bourre, B.; Moreau, T.; et al. MSCopilot, a new multiple sclerosis self-assessment digital solution: Results of a comparative study versus standard tests. Eur. J. Neurol. 2020, 27, 429–436. [Google Scholar] [CrossRef]
- Montalban, X.; Graves, J.; Midaglia, L.; Mulero, P.; Julian, L.; Baker, M.; Schadrack, J.; Gossens, C.; Ganzetti, M.; Scotland, A.; et al. A Smartphone Sensor-Based Digital Outcome Assessment of Multiple Sclero-sis. Mult. Scler. J. 2021, 13524585211028561. [Google Scholar] [CrossRef]
- Healthcare, Orikami Personalized. Ms Sherpa. Available online: https://www.mssherpa.nl/en/ (accessed on 18 October 2021).
- Biogen. Validation of Digicog and Konectom Tools to Support Digitalized Clinical Assessment in Multiple Sclerosis (Digi-toms). Available online: https://www.clinicaltrials.gov/ct2/show/NCT04756700?term=biogen&recrs=a&cond=Multiple+Sclerosis&draw=2 (accessed on 18 October 2021).
- Medizinprodukte, Bundesinstitut für Arzneimittel und. Diga-Verzeichnis. Available online: https://diga.bfarm.de/de/verzeichnis (accessed on 20 October 2021).
- Klose, K.; Kreimeier, S.; Tangermann, U.; Aumann, I.; Damm, K. RHO Group Patient- and person-reports on healthcare: Preferences, outcomes, experiences, and satisfaction—An essay. Health Econ. Rev. 2016, 6, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heesen, C.; Bohm, J.; Reich, C.; Kasper, J.; Goebel, M.; Gold, S.M. Patient Perception of Bodily Functions in Multiple Scle-rosis: Gait and Visual Function Are the Most Valuable. Mult. Scler. 2008, 14, 988–991. [Google Scholar] [CrossRef] [PubMed]
- D’Amico, E.; Haase, R.; Ziemssen, T. Review: Patient-reported outcomes in multiple sclerosis care. Mult. Scler. Relat. Disord. 2019, 33, 61–66. [Google Scholar] [CrossRef]
- Wiklund, I. Assessment of patient-reported outcomes in clinical trials: The example of health-related quality of life. Fundam. Clin. Pharmacol. 2004, 18, 351–363. [Google Scholar] [CrossRef] [PubMed]
- Van Munster, C.E.; Uitdehaag, B.M. Outcome Measures in Clinical Trials for Multiple Sclerosis. CNS Drugs 2017, 31, 217–236. [Google Scholar] [CrossRef] [Green Version]
- Ziemssen, T.; Hillert, J.; Butzkueven, H. The Importance of Collecting Structured Clinical Information on Multiple Scle-rosis. BMC Med. 2016, 14, 81. [Google Scholar] [CrossRef] [Green Version]
- Kern, R.; Haase, R.; Eisele, J.C.; Thomas, K.; Ziemssen, T. Designing an Electronic Patient Management System for Multi-ple Sclerosis: Building a Next Generation Multiple Sclerosis Documentation System. Interact. J. Med. Res. 2016, 5, e4549. [Google Scholar] [CrossRef] [Green Version]
- Ho, B.; Houck, J.R.; Flemister, A.S.; Ketz, J.; Oh, I.; DiGiovanni, B.F.; Baumhauer, J.F. Preoperative PROMIS Scores Predict Postoperative Success in Foot and Ankle Patients. Foot Ankle Int. 2016, 37, 911–918. [Google Scholar] [CrossRef] [PubMed]
- Gausden, E.B.; Levack, A.; Nwachukwu, B.U.; Sin, D.; Wellman, D.S.; Lorich, D.G. Computerized Adaptive Testing for Patient Reported Outcomes in Ankle Fracture Surgery. Foot Ankle Int. 2018, 39, 1192–1198. [Google Scholar] [CrossRef] [PubMed]
- Hung, M.; Hon, S.D.; Cheng, C.; Franklin, J.D.; Aoki, S.K.; Anderson, M.B.; Kapron, A.L.; Peters, C.L.; Pelt, C.E. Psychometric Evaluation of the Lower Extremity Computerized Adaptive Test, the Modified Harris Hip Score, and the Hip Outcome Score. Orthop. J. Sports Med. 2014, 2, 2325967114562191. [Google Scholar] [CrossRef] [Green Version]
- Haase, R.; Scholz, M.; Dillenseger, A.; Kern, R.; Akgün, K.; Ziemssen, T. Improving multiple sclerosis management and collecting safety information in the real world: The MSDS3D software approach. Expert Opin. Drug Saf. 2018, 17, 369–378. [Google Scholar] [CrossRef]
- Ziemssen, T.; Kern, R.; Voigt, I.; Haase, R. Data Collection in Multiple Sclerosis: The MSDS Approach. Front. Neurol. 2020, 11, 445. [Google Scholar] [CrossRef]
- Wattjes, M.P.; Rovira, À.; Miller, D.; Yousry, T.A.; Sormani, M.P.; de Stefano, M.P.; Tintoré, M.; Auger, C.; Tur, C.; Filippi, M.; et al. Evidence-Based Guidelines: Magnims Consensus Guidelines on the Use of Mri in Multiple Sclerosis--Establishing Disease Prognosis and Monitoring Patients. Nat. Rev. Neurol. 2015, 11, 597–606. [Google Scholar]
- Manjón, J.V.; Coupé, P. volBrain: An Online MRI Brain Volumetry System. Front. Aging Neurosci. 2016, 10, 30. [Google Scholar] [CrossRef] [Green Version]
- Rovira, À.; on behalf of the MAGNIMS study group; Wattjes, M.P.; Tintoré, M.; Tur, C.; Yousry, T.A.; Sormani, M.P.; De Stefano, N.; Filippi, M.; Auger, C.; et al. MAGNIMS consensus guidelines on the use of MRI in multiple sclerosis—clinical implementation in the diagnostic process. Nat. Rev. Neurol. 2015, 11, 471–482. [Google Scholar] [CrossRef] [Green Version]
- Schwab, P.; Karlen, W. A Deep Learning Approach to Diagnosing Multiple Sclerosis from Smartphone Data. IEEE J. Biomed. Health Inform. 2021, 25, 1284–1291. [Google Scholar] [CrossRef]
- Zhao, Y.; Wang, T.; Bove, R.; Cree, B.; Henry, R.; Lokhande, H.; Polgar-Turcsanyi, M.; Anderson, M.; Bakshi, R.; Weiner, H.L.; et al. Ensemble learning predicts multiple sclerosis disease course in the SUMMIT study. NPJ Digit. Med. 2020, 3, 135. [Google Scholar] [CrossRef] [PubMed]
- Corral-Acero, J.; Margara, F.; Marciniak, M.; Rodero, C.; Loncaric, F.; Feng, Y.; Gilbert, A.; Fernandes, J.F.; Bukhari, H.A.; Wajdan, A.; et al. The ‘Digital Twin’ to Enable the Vision of Precision Cardiology. Eur. Heart J. 2020, 41, 4556–4564. [Google Scholar] [CrossRef] [PubMed]
- Voigt, I.; Inojosa, H.; Dillenseger, A.; Haase, R.; Akgün, K.; Ziemssen, T. Digital Twins for Multiple Sclerosis. Front. Immunol. 2021, 12, 669811. [Google Scholar] [CrossRef] [PubMed]

| Benefits | Challenges |
|---|---|
| Continuous real-time data | Privacy |
| Better real-world evidence | Adherence/retention |
| Greater power | High variability |
| Novel, sensitive endpoints | Validation required |
| Faster decisions | Complex analysis |
| Big data | Data storage |
| Outcome Measures | Advantages | Disadvantages | |
|---|---|---|---|
| Standardized clinical measures. |
|
|
|
| Timed measures (e.g., T25FW, 6MWT). | Quantified aspect of gait, such as speed and endurance. |
| Do not identify mechanisms underlying gait dysfunction. |
| Patient-based measures (e.g., MSWS-12; EMIQ). | Patient’s perspective of their walking disability. |
| Do not identify mechanisms underlying gait dysfunction. |
| Observational gait analysis (e.g., during T25FT or other walking conditions). | Gait pattern in terms of kinematic and spatiotemporal parameters. |
|
|
Sensor floor plates:
|
|
|
|
| Three-dimensional gait analysis (reflecting markers places on a person and recording movement with infrared cameras). | Detailed quantitative measures of kinematic, kinetic and spatiotemporal parameters. |
| Require expensive equipment and skilled examiner. |
Video-based:
| (a) and (b):
|
|
|
Wearable sensors:
|
|
|
|
| Assessment Technology | Method | Outcomes * | Device ǂ (Manufacturer) |
|---|---|---|---|
| Video-based |
| (a) Joint range of motion |
|
| Sensor floor plates |
|
|
|
| Wearable sensors |
| (a) Spatiotemporal measures, joint range of motion |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dillenseger, A.; Weidemann, M.L.; Trentzsch, K.; Inojosa, H.; Haase, R.; Schriefer, D.; Voigt, I.; Scholz, M.; Akgün, K.; Ziemssen, T. Digital Biomarkers in Multiple Sclerosis. Brain Sci. 2021, 11, 1519. https://doi.org/10.3390/brainsci11111519
Dillenseger A, Weidemann ML, Trentzsch K, Inojosa H, Haase R, Schriefer D, Voigt I, Scholz M, Akgün K, Ziemssen T. Digital Biomarkers in Multiple Sclerosis. Brain Sciences. 2021; 11(11):1519. https://doi.org/10.3390/brainsci11111519
Chicago/Turabian StyleDillenseger, Anja, Marie Luise Weidemann, Katrin Trentzsch, Hernan Inojosa, Rocco Haase, Dirk Schriefer, Isabel Voigt, Maria Scholz, Katja Akgün, and Tjalf Ziemssen. 2021. "Digital Biomarkers in Multiple Sclerosis" Brain Sciences 11, no. 11: 1519. https://doi.org/10.3390/brainsci11111519
APA StyleDillenseger, A., Weidemann, M. L., Trentzsch, K., Inojosa, H., Haase, R., Schriefer, D., Voigt, I., Scholz, M., Akgün, K., & Ziemssen, T. (2021). Digital Biomarkers in Multiple Sclerosis. Brain Sciences, 11(11), 1519. https://doi.org/10.3390/brainsci11111519








