Understanding Parinaud’s Syndrome
Abstract
:1. Introduction
2. Materials and Methods
3. Discussion
3.1. Differential Diagnosis of Midbrain Syndromes
3.2. Etiologies
3.3. Pathophysiology of Parinaud’s Syndrome
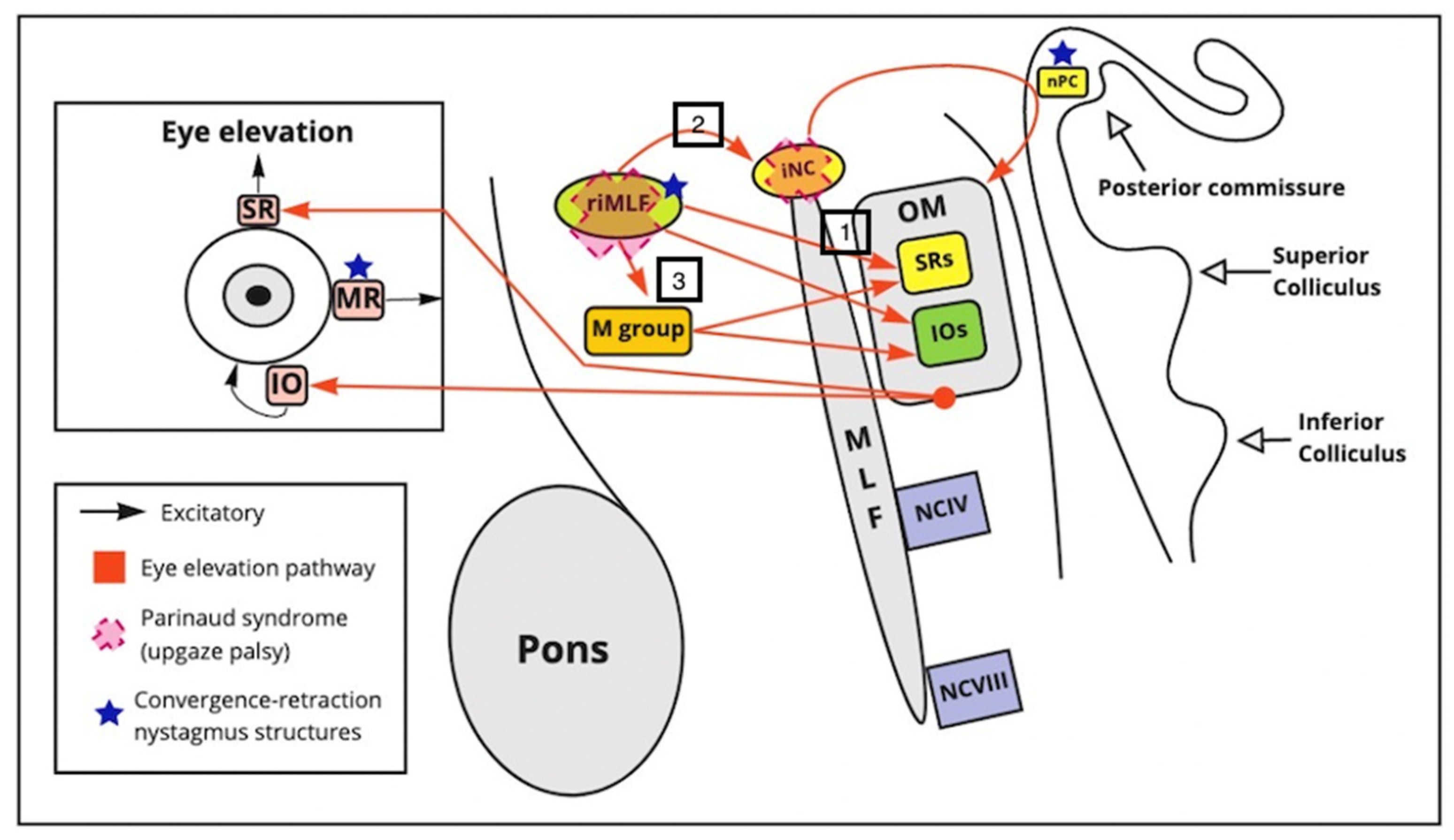
3.3.1. Upward Gaze Palsy
3.3.2. Convergence Retraction Nystagmus
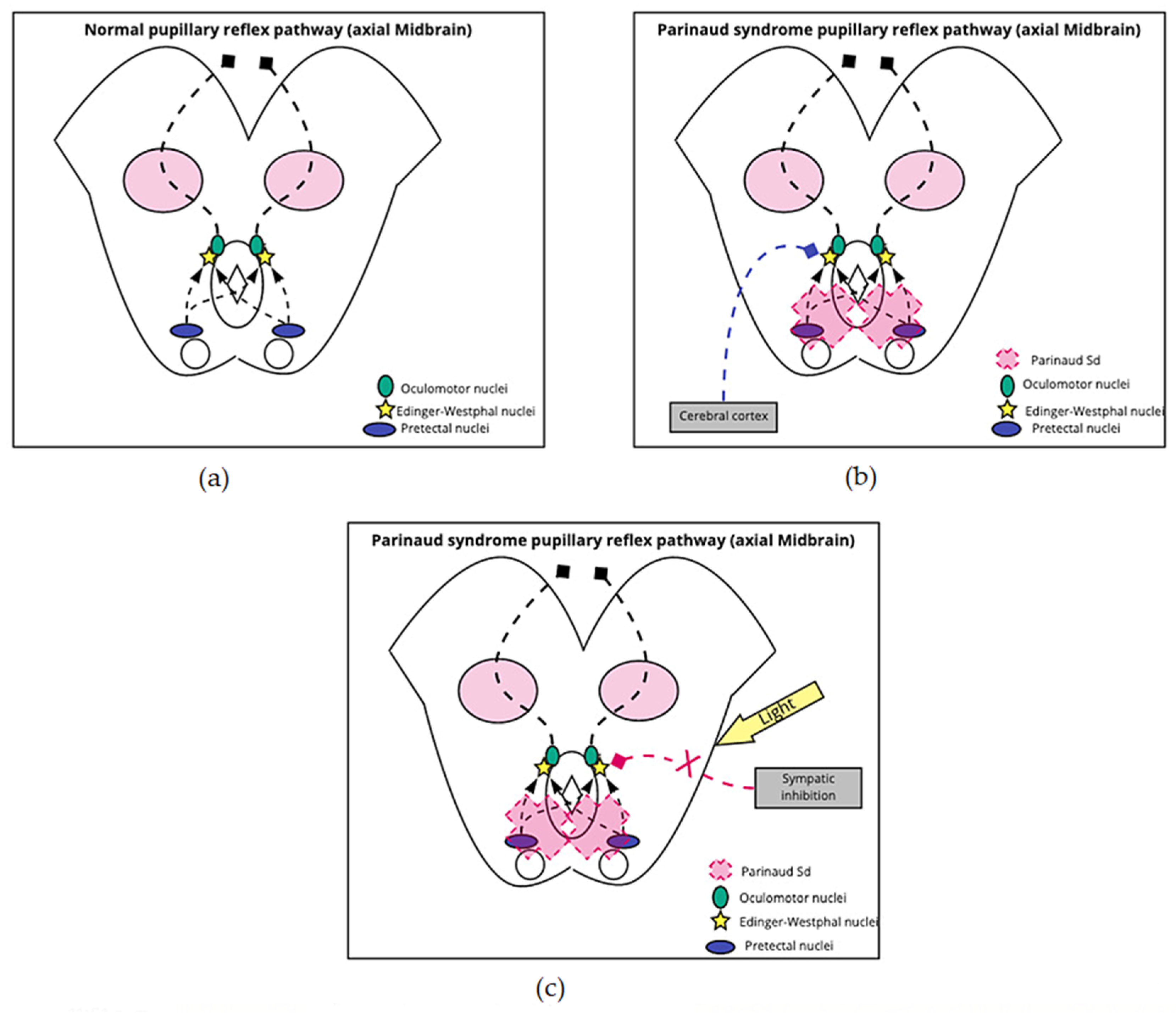
3.3.3. Light-Near Dissociation/Pseudo-Argyll Robertson Pupils
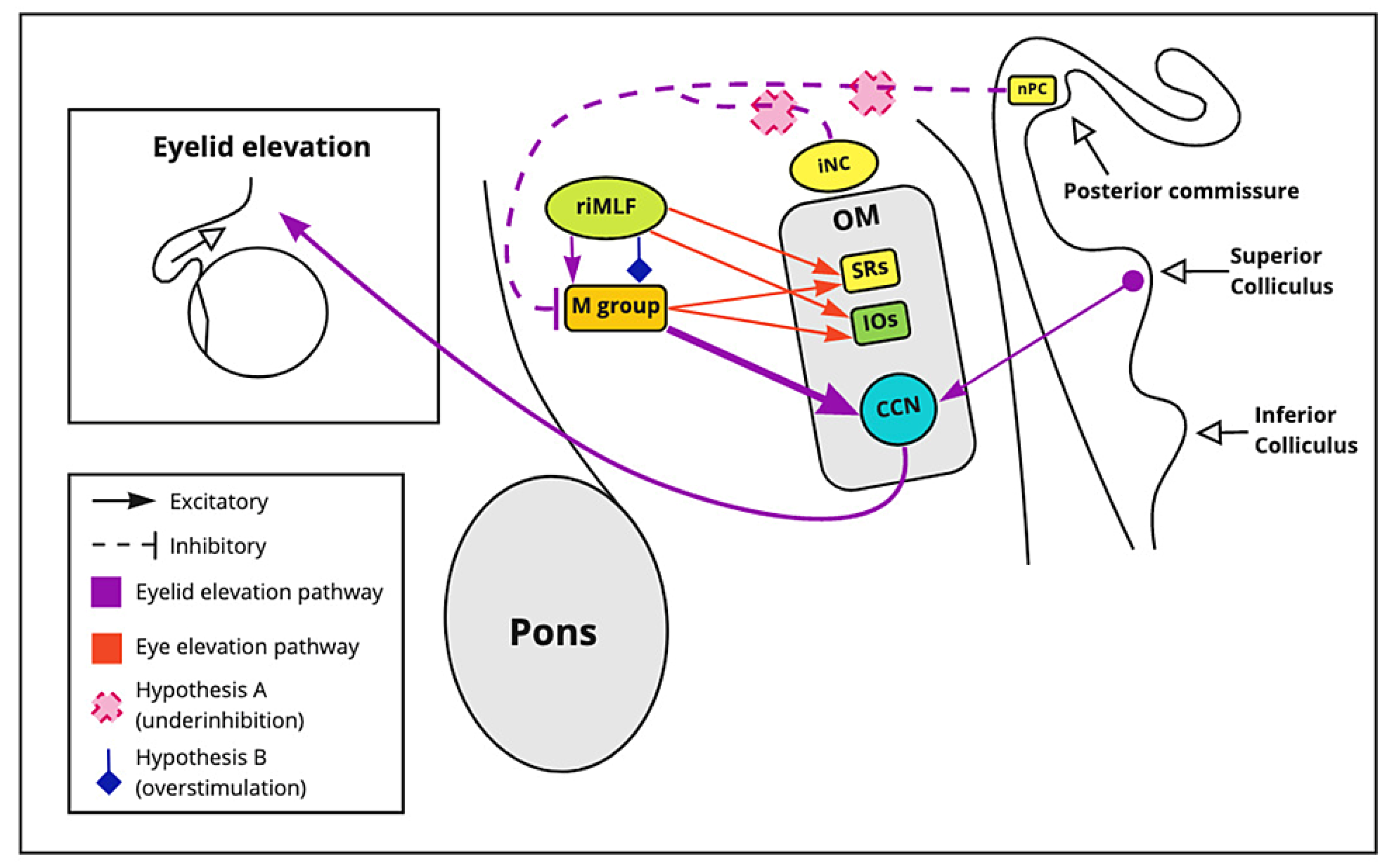
3.3.4. Collier’s Sign
3.3.5. III, IV, and VI Nerve Palsies
3.3.6. Blurred Vision and Visual Field Defects
3.3.7. Ptosis and Squint
3.3.8. Ataxia
3.3.9. Diplopia
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ruchalski, K.; Hathout, G.M. A Medley of Midbrain Maladies: A Brief Review of Midbrain Anatomy and Syndromology for Radiologists. Radiol. Res. Pract. 2012, 2012, 258524. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, N.; Tsehmaister-Abitbol, V.; Glikstein, R.; Torres, C. Too Much on Your “Plate”? Spectrum of Pathologies Involving the Tectal Plate. Can. Assoc. Radiol. J. 2020, 71, 186–194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levidou, G.; Korkolopoulou, P.; Agrogiannis, G.; Paidakakos, N.; Bouramas, D.; Patsouris, E. Low-grade oligodendroglioma of the pineal gland: A case report and review of the literature. Diagn. Pathol. 2010, 5, 59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Naqvi, S.; Rupareliya, C.; Shams, A.; Hameed, M.; Mahuwala, Z.; Giyanwani, P.R. Pineal Gland Tumor but not Pinealoma: A Case Report. Cureus 2017, 9, e1576. [Google Scholar] [CrossRef] [Green Version]
- Stavale, J.N.; Cavalheiro, S.; Lamis, F.C.; Neto, M.A.D.P. Low-Grade Oligodendroglioma of the Pineal Region: Case Report. J. Neurol. Surg. Rep. 2015, 76, e55–e58. [Google Scholar] [CrossRef] [Green Version]
- Moncayo, J. Midbrain Infarcts and Hemorrhages. Front. Neurol. Neurosci. 2012, 30, 158–161. [Google Scholar] [CrossRef]
- Martin, P.J.; Chang, H.M.; Wityk, R.; Caplan, L.R. Midbrain infarction: Associations and aetiologies in the New England Medical Center Posterior Circulation Registry. J. Neurol. Neurosurg. Psychiatry 1998, 64, 392–395. [Google Scholar] [CrossRef] [Green Version]
- Paidakakos, N.A.; Rokas, E.; Theodoropoulos, S.; Dimogerontas, G.; Konstantinidis, E. Posttraumatic Benedikt’s Syndrome: A Rare Entity with Unclear Anatomopathological Correlations. World Neurosurg. 2012, 78, 715.e13–715.e15. [Google Scholar] [CrossRef]
- Sciacca, S.; Lynch, J.; Davagnanam, I.; Barker, R. Midbrain, Pons, and Medulla: Anatomy and Syndromes. RadioGraphics 2019, 39, 1110–1125. [Google Scholar] [CrossRef]
- Sajan, A.; Hewitt, K.; Soleiman, A.; Velayudhan, V. Pineal glioblastoma: Case report and literature review of an exceedingly rare etiology for pineal region mass. Clin. Imaging 2019, 60, 95–99. [Google Scholar] [CrossRef]
- Al-Hussaini, M.; Sultan, I.; Abuirmileh, N.; Jaradat, I.; Qaddoumi, I. Pineal gland tumors: Experience from the SEER database. J. Neuro-Oncol. 2009, 94, 351–358. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shields, M.; Sinkar, S.; Chan, W.; Crompton, J. Parinaud syndrome: A 25-year (1991–2016) review of 40 consecutive adult cases. Acta Ophthalmol. 2017, 95, 792–793. [Google Scholar] [CrossRef]
- Lyons, A.R.; Olson, S.L. Parinaud syndrome as an unusual presentation of intracranial hypotension. Surg. Neurol. Int. 2020, 11, 98. [Google Scholar] [CrossRef]
- Menezes, A.S.; Ribeiro, D.; Lima, A.F. Cat-scratch Disease with Parinaud’s Oculoglandular Syndrome. Turk. Arch. Otorhinolaryngol. 2020, 58, 48–51. [Google Scholar] [CrossRef] [PubMed]
- Survashe, P.T.; Guthe, S.; Velho, V.; Naik, H. Tectal Tuberculoma: An Unusual Cause of Parinaud’s Syndrome. Asian J. Neurosurg. 2018, 13, 400–402. [Google Scholar] [CrossRef]
- Eggenberger, E.R. Supranuclear Eye Movement Abnormalities. Contin. Lifelong Learn. Neurol. 2014, 20, 981–992. [Google Scholar] [CrossRef] [PubMed]
- Stalcup, S.T.; Tuan, A.S.; Hesselink, J.R. Intracranial Causes of Ophthalmoplegia: The Visual Reflex Pathways. RadioGraphics 2013, 33, E153–E169. [Google Scholar] [CrossRef]
- Büttner, U.; Büttner-Ennever, J.A. Present concepts of oculomotor organization. Prog. Brain Res. 2006, 151, 1–42. [Google Scholar] [CrossRef]
- Pierrot-Deseilligny, C. Nuclear, internuclear, and supranuclear ocular motor disorders. Handb. Clin. Neurol. 2011, 102, 319–331. [Google Scholar] [CrossRef]
- Rambold, H.; Kömpf, D.; Helmchen, C. Convergence retraction nystagmus: A disorder of vergence? Ann. Neurol. 2001, 50, 677–681. [Google Scholar] [CrossRef] [PubMed]
- Feroze, K.B.; Patel, B.C. Parinaud syndrome. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Gomez, C.R.; Gomez, S.M.; Selhorst, J.B. Acute thalamic esotropia. Neurology 1988, 38, 1759. [Google Scholar] [CrossRef]
- Yoo, H.; Mihaila, D.M. Neuroanatomy, pupillary light reflexes and pathway. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Binda, P.; Straßer, T.; Stingl, K.; Richter, P.; Peters, T.; Wilhelm, H.; Wilhelm, B.; Kelbsch, C. Pupil response components: Attention-light interaction in patients with Parinaud’s syndrome. Sci. Rep. 2017, 7, 10283. [Google Scholar] [CrossRef] [Green Version]
- Pearce, J.M.S. The Argyll Robertson pupil. J. Neurol. Neurosurg. Psychiatry 2004, 75, 1345. [Google Scholar] [CrossRef] [Green Version]
- Hamedani, A.G.; Gold, D.R. Eyelid Dysfunction in Neurodegenerative, Neurogenetic, and Neurometabolic Disease. Front. Neurol. 2017, 8, 329. [Google Scholar] [CrossRef] [PubMed]
- Ozdemir, N.G. The anatomy of the posterior commissure. Turk. Neurosurg. 2015, 25, 837–843. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ayberk, G.; Ozveren, M.F.; Yildirim, T.; Ercan, K.; Cay, E.K.; Koçak, A. Review of a series with abducens nerve palsy. Turk Neurosurg. 2008, 18, 366–373. [Google Scholar]
- Baloh, R.W.; Furman, J.M.; Yee, R.D. Dorsal midbrain syndrome: Clinical and oculographic findings. Neurology 1985, 35, 54. [Google Scholar] [CrossRef]
- Hankinson, E.V.; Lyons, C.J.; Hukin, J.; Cochrane, D.D. Ophthalmological outcomes of patients treated for pineal region tumors. J. Neurosurg. Pediatr. 2016, 17, 558–563. [Google Scholar] [CrossRef] [Green Version]
- Yousif, J.E.; Liao, E.; Trobe, J.D. Dorsal Midbrain Syndrome. J. Neuro-Ophthalmol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Khan, Z.; Bollu, P.C. Horner syndrome. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Plowey, E.D.; Vogel, O.H.; Yeom, K.W.; Jung, H.; Chao, K.; Edwards, M.S. Tectal pineal cyst in a 1-year-old girl. Hum. Pathol. 2014, 45, 653–656. [Google Scholar] [CrossRef] [PubMed]
- Chang, M.C.; Seo, J.P. Injury of the dentato-rubro-thalamic tract in a patient with intentional tremor after mild traumatic brain injury: A case report. Brain Inj. 2020, 34, 1283–1286. [Google Scholar] [CrossRef]
- MRI of Claude’s Syndrome|Neurology. Available online: https://n.neurology.org/content/61/4/575 (accessed on 16 August 2021).
- Derakhshan, I.; Sabouri-Deylami, M.; Kaufman, B. Bilateral Nothnagel syndrome. Clinical and roentgenological observations. Stroke 1980, 11, 177–179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davis, L.E.; DeBiasi, R.; Goade, D.E.; Haaland, K.Y.; Harrington, J.A.; Harnar, J.B.; Pergam, S.; King, M.K.; DeMasters, B.K.; Tyler, K.L. West Nile virus neuroinvasive disease. Ann. Neurol. 2006, 60, 286–300. [Google Scholar] [CrossRef] [PubMed]
- Gnanapavan, S.; Sillery, E.; Acheson, J.; Toosy, A. Parinaud’s syndrome—A rare presentation of clinically isolated syndrome. Mult. Scler. Relat. Disord. 2014, 3, 398–401. [Google Scholar] [CrossRef] [PubMed]
- Quint, D.J.; Cornblath, W.T.; Trobe, J.D. Multiple sclerosis presenting as Parinaud syndrome. AJNR. Am. J. Neuroradiol. 1993, 14, 1200–1202. [Google Scholar] [PubMed]
- Bhola, R.; Olson, R.J. Dorsal Midbrain Syndrome with Bilateral Superior Oblique Palsy Following Brainstem Hemorrhage. Arch. Ophthalmol. 2006, 124, 1786. [Google Scholar] [CrossRef] [Green Version]
| Data Search | ||||
|---|---|---|---|---|
| (“Parinaud syndrome”[Title/Abstract] OR “dorsal midbrain syndrome”[Title/Abstract]) AND “Diplopia”[Title/Abstract] | (“Parinaud syndrome”[Title/Abstract] OR “dorsal midbrain syndrome”[Title/Abstract]) AND “Ataxia”[Title/Abstract] | (“Parinaud syndrome”[Title/Abstract] OR “dorsal midbrain syndrome”[Title/Abstract]) AND “Nerve Palsy”[Title/Abstract] | “Parinaud syndrome”[Title/Abstract] OR “dorsal midbrain syndrome”[Title/Abstract]) AND “Blurred vision”[Title/Abstract] | (“Parinaud syndrome”[Title/Abstract] OR “dorsal midbrain syndrome”[Title/Abstract]) AND “Ptosis”[Title/Abstract] |
| (“Parinaud syndrome”[Title/Abstract] OR “dorsal midbrain syndrome”[Title/Abstract]) AND “Collier’s sign”[Title/Abstract] | (“Parinaud syndrome”[Title/Abstract] OR “dorsal midbrain syndrome”[Title/Abstract]) AND “Pseudo Argyll Robertson Pupils”[Title/Abstract] | (“Parinaud syndrome”[Title/Abstract] OR “dorsal midbrain syndrome”[Title/Abstract]) AND “Up gaze Palsy”[Title/Abstract] | (“Parinaud syndrome”[Title/Abstract] OR “dorsal midbrain syndrome”[Title/Abstract]) AND “Converse retraction nystagmus”[Title/Abstract] | (Dorsal midbrain syndrome [Title/Abstract]) AND (Pathophysiology [Title/Abstract]) |
| Midbrain Syndrome | Structures Involved | Clinical Features | Cause |
|---|---|---|---|
| Weber syndrome [1] | Oculomotor nucleus, cerebral peduncle, substantia nigra at times, and superior cerebellar peduncles (ventral tegmentum) | Ipsilateral oculomotor palsy, contralateral ataxia, and contralateral hemiparesis. Parkinsonism is seen at times | Branches of the posterior cerebral artery |
| Claude syndrome [9] | Red nucleus, oculomotor nucleus, superior cerebellar peduncles | Ipsilateral oculomotor palsy and contralateral ataxia | Branches of the posterior cerebral artery |
| Benedikt syndrome [8] | Red nucleus, superior cerebellar oculomotor nucleus, cerebral peduncle (paramedial midbrain) | Ipsilateral oculomotor palsy, contralateral cerebellar ataxia, choreoathetosis, and contralateral hemiparesis | Branches of the posterior cerebral artery. Lower frequency of ischemic infarcts compared to Weber and Claude |
| Nothnagel’s syndrome [6,9] | Superior cerebellar peduncle, oculomotor nucleus (dorsomedial) | Ipsilateral or bilateral oculomotor palsy, ipsilateral limb ataxia | Usually involves a mass compressing the midbrain |
| Midbrain Infarction | Encephalitis | Trauma | Intracranial Hypotension | Others |
|---|---|---|---|---|
| Multiple sclerosis | Toxoplasmosis | Obstructive hydrocephalus | Neuromyelitis optica | Miller Fisher syndrome |
| Midbrain hemorrhage | Cat scratch disease | Tonic clonic seizures | Tectal tuberculoma | Arterio-venous malformations |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ortiz, J.F.; Eissa-Garces, A.; Ruxmohan, S.; Cuenca, V.; Kaur, M.; Fabara, S.P.; Khurana, M.; Parwani, J.; Paez, M.; Anwar, F.; et al. Understanding Parinaud’s Syndrome. Brain Sci. 2021, 11, 1469. https://doi.org/10.3390/brainsci11111469
Ortiz JF, Eissa-Garces A, Ruxmohan S, Cuenca V, Kaur M, Fabara SP, Khurana M, Parwani J, Paez M, Anwar F, et al. Understanding Parinaud’s Syndrome. Brain Sciences. 2021; 11(11):1469. https://doi.org/10.3390/brainsci11111469
Chicago/Turabian StyleOrtiz, Juan Fernando, Ahmed Eissa-Garces, Samir Ruxmohan, Victor Cuenca, Mandeep Kaur, Stephanie P. Fabara, Mahika Khurana, Jashank Parwani, Maria Paez, Fatima Anwar, and et al. 2021. "Understanding Parinaud’s Syndrome" Brain Sciences 11, no. 11: 1469. https://doi.org/10.3390/brainsci11111469
APA StyleOrtiz, J. F., Eissa-Garces, A., Ruxmohan, S., Cuenca, V., Kaur, M., Fabara, S. P., Khurana, M., Parwani, J., Paez, M., Anwar, F., Tamton, H., & Cueva, W. (2021). Understanding Parinaud’s Syndrome. Brain Sciences, 11(11), 1469. https://doi.org/10.3390/brainsci11111469









