Efficacy of DiscoGel in Treatment of Degenerative Disc Disease: A Prospective 1-Year Observation of 67 Patients
Abstract
:1. Introduction
2. Materials and Methods
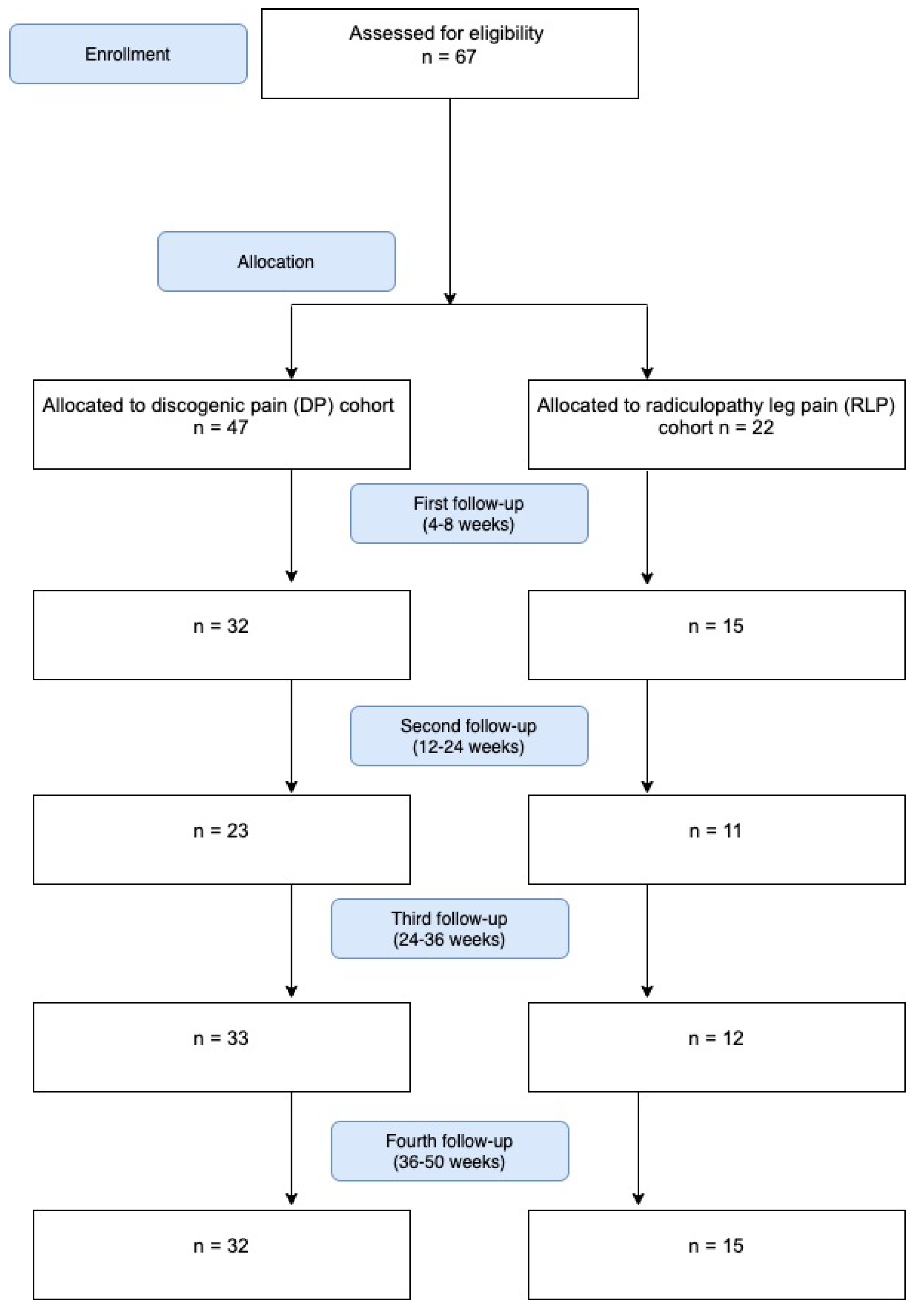
2.1. Study Design and Patient Recruitment
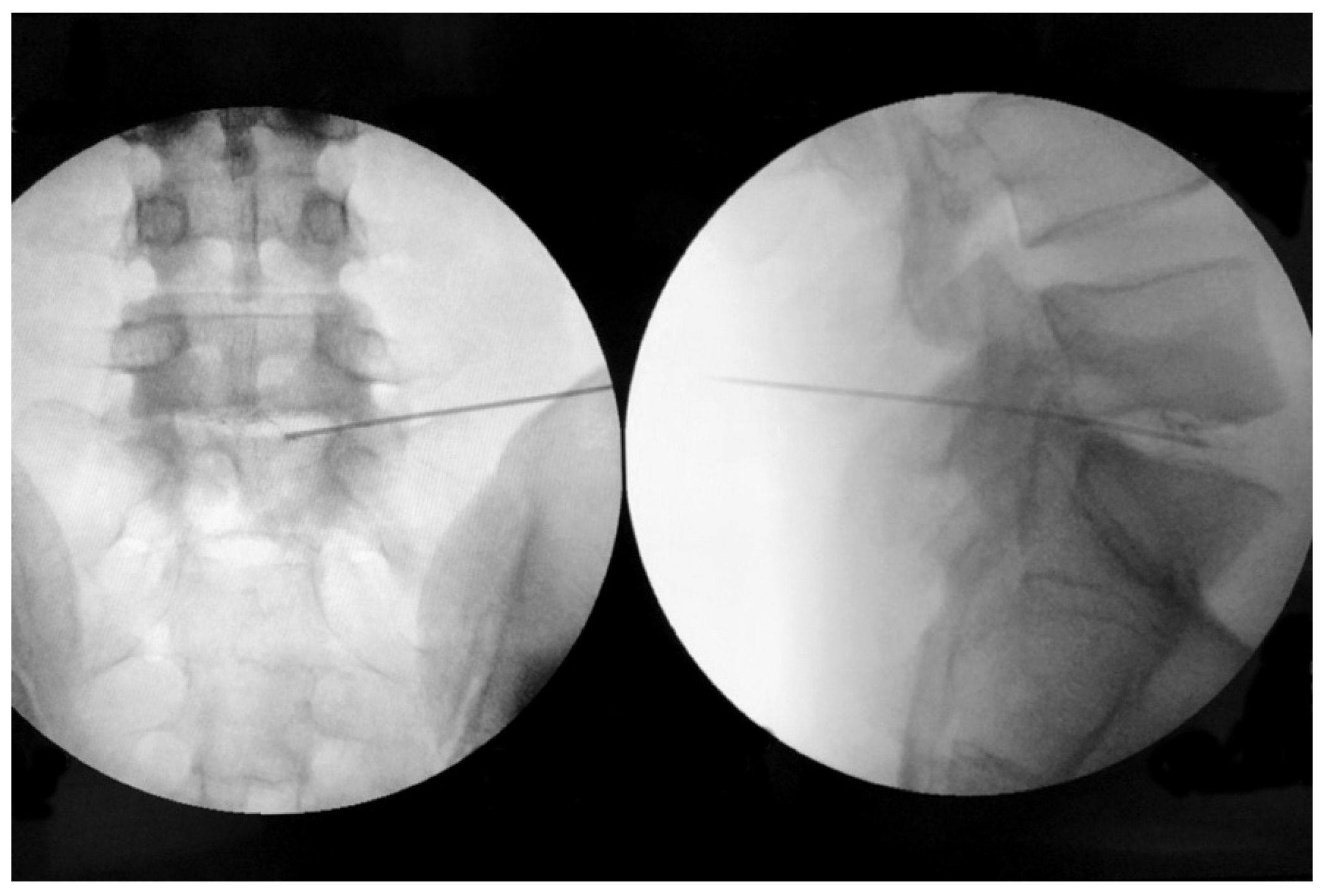
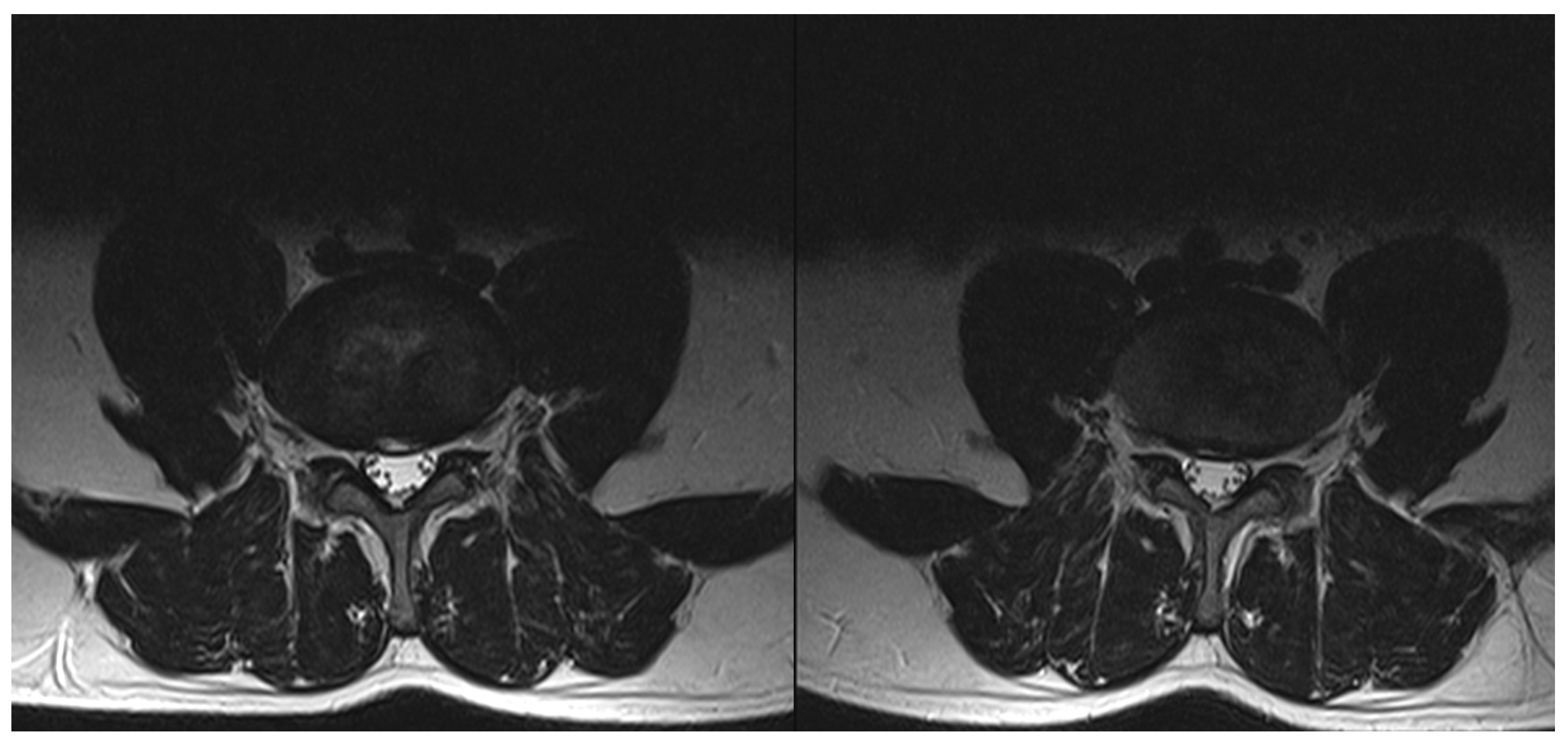
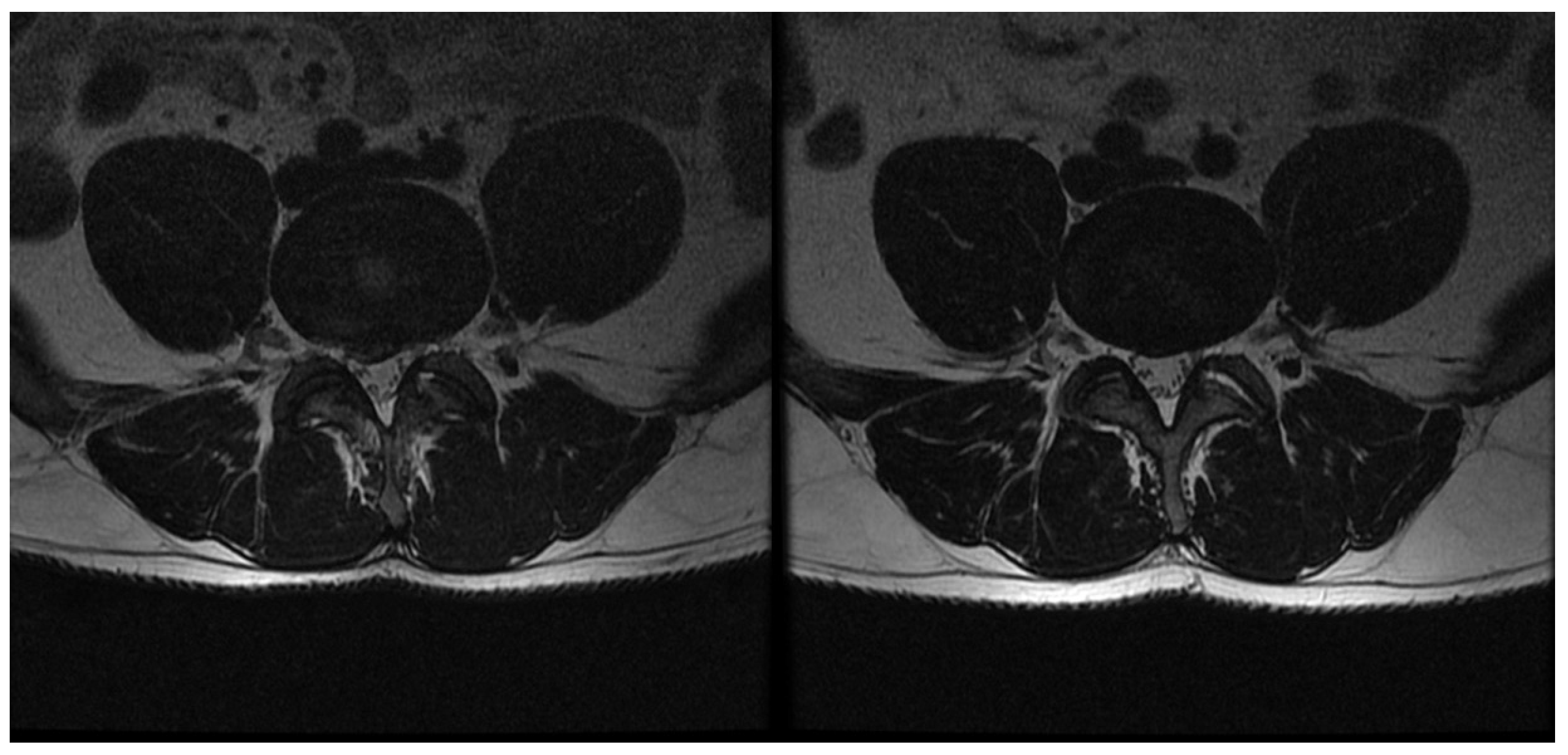
2.2. Procedure
2.3. Data Collection
- 0—I do not take any.
- 1—I take them once a week.
- 2—I take them several times a week.
- 3—I take them once a day.
- 4—I take them several times a day.
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
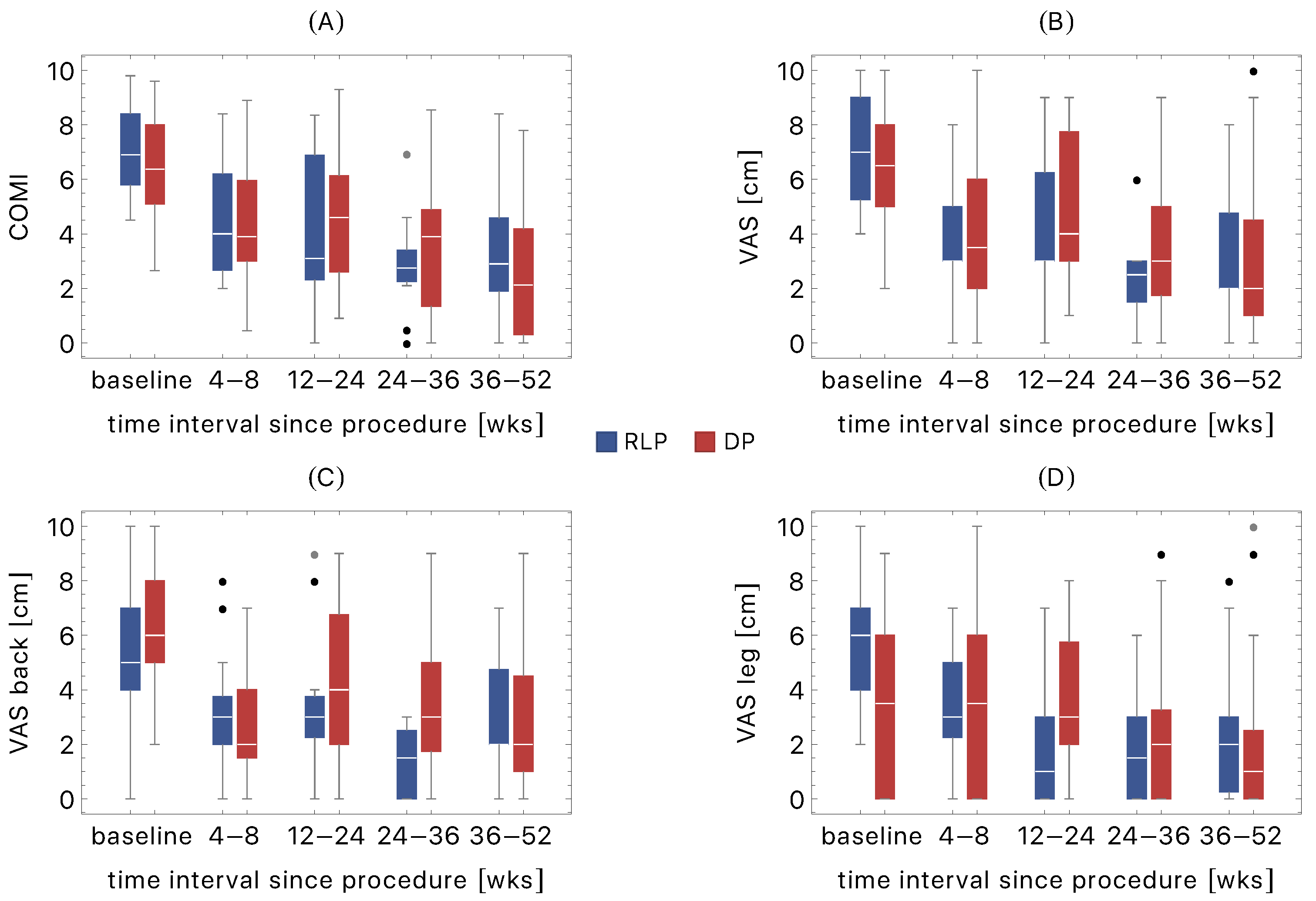
3.2. Follow-Up Evaluation
- COMI (both cohorts)
- VAS (RLP cohort)
- VAS leg (RLP cohort)
- VAS back (DP cohort).
3.3. Comparison of RLP and DP Cohorts
- The DP VAS back at F3 was higher (p = 0.02).
- The RLP VAS was higher at baseline (p = 0.001).
3.4. Consumption of Analgesics
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| AF | Annulus fibrosus |
| COMI | Core Outcome Measures Index |
| DDD | Degenerative Disc Disease |
| DP | Discogenic pain group |
| GBD | Global Burden of Disease Study |
| GEI | Gelified ethanol injection |
| IVD | Intervertebral disc |
| LBP | Low back pain |
| MRI | Magnetic Resonance Imaging |
| NP | Nucleus pulposus |
| RLP | Radiculopathy leg pain group |
| VAS | Visual Analogue Scale |
| VEP | Vertebral end-plate |
References
- Whatley, B.R.; Wen, X. Intervertebral disc (IVD): Structure, degeneration, repair and regeneration. Mater. Sci. Eng. C 2012, 32, 61–77. [Google Scholar] [CrossRef]
- Adams, M.A.; Roughley, P.J. What is intervertebral disc degeneration, and what causes it? Spine 2006, 31, 2151–2161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fujii, K.; Yamazaki, M.; Kang, J.D.; Risbud, M.V.; Cho, S.K.; Qureshi, S.A.; Hecht, A.C.; Iatridis, J.C. Discogenic back pain: Literature review of definition, diagnosis, and treatment. JBMR Plus 2019, 3, e10180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zehra, U.; Bow, C.; Lotz, J.C.; Williams, F.M.; Rajasekaran, S.; Karppinen, J.; Luk, K.D.; Battiê, M.C.; Samartzis, D. Structural vertebral endplate nomenclature and etiology: A study by the ISSLS Spinal Phenotype Focus Group. Eur. Spine J. 2018, 27, 2–12. [Google Scholar] [CrossRef] [PubMed]
- Berry, J.A.; Elia, C.; Saini, H.S.; Miulli, D.E. A review of lumbar radiculopathy, diagnosis, and treatment. Cureus 2019, 11, e5934. [Google Scholar] [CrossRef] [Green Version]
- Patel, E.A.; Perloff, M.D. Radicular pain syndromes: Cervical, lumbar, and spinal stenosis. In Seminars in Neurology; Thieme Medical Publishers: New York, NY, USA, 2018; Volume 38, pp. 634–639. [Google Scholar]
- Amirdelfan, K.; Webster, L.; Poree, L.; Sukul, V.; McRoberts, P. Treatment options for failed back surgery syndrome patients with refractory chronic pain: An evidence based approach. Spine 2017, 42, S41–S52. [Google Scholar] [CrossRef]
- Kallewaard, J.W.; Terheggen, M.A.; Groen, G.J.; Sluijter, M.E.; Derby, R.; Kapural, L.; Mekhail, N.; Van Kleef, M. 15. Discogenic low back pain. Pain Pract. 2010, 10, 560–579. [Google Scholar] [CrossRef]
- Freemont, A.; Peacock, T.; Goupille, P.; Hoyland, J.; O’brien, J.; Jayson, M. Nerve ingrowth into diseased intervertebral disc in chronic back pain. Lancet 1997, 350, 178–181. [Google Scholar] [CrossRef]
- Takahashi, K.; Aoki, Y.; Ohtori, S. Resolving discogenic pain. Eur. Spine J. 2008, 17, 428–431. [Google Scholar] [CrossRef] [Green Version]
- García-Cosamalón, J.; Del Valle, M.E.; Calavia, M.G.; García-Suárez, O.; López-Muñiz, A.; Otero, J.; Vega, J.A. Intervertebral disc, sensory nerves and neurotrophins: Who is who in discogenic pain? J. Anat. 2010, 217, 1–15. [Google Scholar] [CrossRef]
- Hoy, D.; Bain, C.; Williams, G.; March, L.; Brooks, P.; Blyth, F.; Woolf, A.; Vos, T.; Buchbinder, R. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012, 64, 2028–2037. [Google Scholar] [CrossRef] [PubMed]
- Wong, A.Y.; Karppinen, J.; Samartzis, D. Low back pain in older adults: Risk factors, management options and future directions. Scoliosis Spinal Disord. 2017, 12, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Meucci, R.D.; Fassa, A.G.; Faria, N.M.X. Prevalence of chronic low back pain: Systematic review. Rev. De Saude Publica 2015, 49, 73. [Google Scholar] [CrossRef] [PubMed]
- Calvo-Muñoz, I.; Gómez-Conesa, A.; Sánchez-Meca, J. Prevalence of low back pain in children and adolescents: A meta-analysis. BMC Pediatr. 2013, 13, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Wang, S.M.; Dezinno, P.; Maranets, I.; Berman, M.R.; Caldwell-Andrews, A.A.; Kain, Z.N. Low back pain during pregnancy: Prevalence, risk factors, and outcomes. Obstet. Gynecol. 2004, 104, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Verrills, P.; Nowesenitz, G.; Barnard, A. Prevalence and characteristics of discogenic pain in tertiary practice: 223 consecutive cases utilizing lumbar discography. Pain Med. 2015, 16, 1490–1499. [Google Scholar] [CrossRef] [Green Version]
- Alexander, C.E.; Varacallo, M. Lumbosacral radiculopathy. Neurol. Clin. 2021, 25, 387–405. [Google Scholar]
- Gore, M.; Sadosky, A.; Stacey, B.R.; Tai, K.S.; Leslie, D. The burden of chronic low back pain: Clinical comorbidities, treatment patterns, and health care costs in usual care settings. Spine 2012, 37, E668–E677. [Google Scholar] [CrossRef] [Green Version]
- Hoy, D.; March, L.; Brooks, P.; Blyth, F.; Woolf, A.; Bain, C.; Williams, G.; Smith, E.; Vos, T.; Barendregt, J. The global burden of low back pain: Estimates from the Global Burden of Disease 2010 study. Ann. Rheum. Dis. 2014, 73, 968–974. [Google Scholar] [CrossRef] [Green Version]
- Hurwitz, E.L.; Randhawa, K.; Yu, H.; Côté, P.; Haldeman, S. The Global Spine Care Initiative: A summary of the global burden of low back and neck pain studies. Eur. Spine J. 2018, 27, 796–801. [Google Scholar] [CrossRef]
- Wu, A.; March, L.; Zheng, X.; Huang, J.; Wang, X.; Zhao, J.; Blyth, F.M.; Smith, E.; Buchbinder, R.; Hoy, D. Global low back pain prevalence and years lived with disability from 1990 to 2017: Estimates from the Global Burden of Disease Study 2017. Ann. Transl. Med. 2020, 8, 299. [Google Scholar] [CrossRef]
- Knezevic, N.N.; Mandalia, S.; Raasch, J.; Knezevic, I.; Candido, K.D. Treatment of chronic low back pain–new approaches on the horizon. J. Pain Res. 2017, 10, 1111. [Google Scholar] [CrossRef] [Green Version]
- Migliore, A.; Sorbino, A.; Bacciu, S.; Bellelli, A.; Frediani, B.; Tormenta, S.; Pirri, C.; Foti, C. The technique of intradiscal injection: A narrative review. Ther. Clin. Risk Manag. 2020, 16, 953. [Google Scholar] [CrossRef] [PubMed]
- Smith, L. Enzyme dissolution of the nucleus pulposus in humans. Jama 1964, 187, 137–140. [Google Scholar] [CrossRef] [PubMed]
- Simmons, J.W.; Fraser, R.D. The rise and fall of chemonucleolysis. In Arthroscopic and Endoscopic Spinal Surgery; Springer: Berlin/Heidelberg, Germany, 2005; pp. 351–358. [Google Scholar]
- Theron, J.; Guimaraens, L.; Casasco, A.; Sola, T.; Cuellar, H.; Courtheoux, P. Percutaneous treatment of lumbar intervertebral disk hernias with radiopaque gelified ethanol: A preliminary study. Clin. Spine Surg. 2007, 20, 526–532. [Google Scholar] [CrossRef] [PubMed]
- Volpentesta, G.; De Rose, M.; Bosco, D.; Stroscio, C.; Guzzi, G.; Bombardieri, C.; Chirchiglia, D.; Plastino, M.; Romano, M.; Cristofalo, S. Lumbar percutaneous intradiscal injection of radiopaque gelified ethanol (“Discogel”) in patients with low back and radicular pain. J Pain Relief 2014, 3, 145. [Google Scholar]
- Touraine, S.; Damiano, J.; Tran, O.; Laredo, J.D. Cohort study of lumbar percutaneous chemonucleolysis using ethanol gel in sciatica refractory to conservative treatment. Eur. Radiol. 2015, 25, 3390–3397. [Google Scholar] [CrossRef]
- Marcia, S.; Bellini, M.; Hirsch, J.A.; Chandra, R.V.; Piras, E.; Marras, M.; Sanna, A.M.; Saba, L. Efficacy of an ethyl alcohol gel in symptomatic disc herniation. Eur. J. Radiol. 2018, 109, 101–107. [Google Scholar] [CrossRef]
- La Torre, D.; Volpentesta, G.; Stroscio, C.; Bombardieri, C.; Chirchiglia, D.; Guzzi, G.; Pugliese, D.; De Bartolo, E.; Lavano, A. Percutaneous intradiscal injection of radiopaque gelified ethanol: Short-and long-term functional outcome and complication rate in a consecutive series of patients with lumbar disc herniation. Br. J. Pain 2021, 15, 234–241. [Google Scholar] [CrossRef]
- Stagni, S.; De Santis, F.; Cirillo, L.; Dall’Olio, M.; Princiotta, C.; Simonetti, L.; Stafa, A.; Leonardi, M. A minimally invasive treatment for lumbar disc herniation: DiscoGel® chemonucleolysis in patients unresponsive to chemonucleolysis with oxygen-ozone. Interv. Neuroradiol. 2012, 18, 97–104. [Google Scholar] [CrossRef]
- DePalma, M.J. (Ed.) Therapeutic Intradiscal Procedures for Lumbosacral Radiculopathy; Demos Medical Publishing: New York, NY, USA, 2011. [Google Scholar]
- Papadopoulos, D.; Kostopanagiotou, G.; Lemonis, A.; Batistaki, C. Intradiscal combination of pulsed radiofrequency and gelified ethanol for the treatment of chronic discogenic low back pain. Pain Med. 2014, 15, 881–883. [Google Scholar] [CrossRef]
- Papadopoulos, D.; Batistaki, C.; Kostopanagiotou, G. Comparison of the efficacy between intradiscal gelified ethanol (DiscoGel) injection and intradiscal combination of pulsed radiofrequency and gelified ethanol (DiscoGel) injection for chronic discogenic low back pain treatment. A randomized double-blind clinical study. Pain Med. 2020, 21, 2713–2718. [Google Scholar] [PubMed]
- Willems, P.C.; Jacobs, W.; Duinkerke, E.S.; De Kleuver, M. Lumbar discography: Should we use prophylactic antibiotics?: A study of 435 consecutive discograms and a systematic review of the literature. Clin. Spine Surg. 2004, 17, 243–247. [Google Scholar] [CrossRef]
- Miekisiak, G.; Kollataj, M.; Dobrogowski, J.; Kloc, W.; Libionka, W.; Banach, M.; Latka, D.; Sobolewski, T.; Sulewski, A.; Nowakowski, A.; et al. Cross-cultural adaptation and validation of the Polish version of the Core Outcome Measures Index for low back pain. Eur. Spine J. 2013, 22, 995–1001. [Google Scholar] [CrossRef] [Green Version]
- Lozano-Álvarez, C.; Pérez-Prieto, D.; Saló, G.; Molina, A.; Lladó, A.; Ramírez, M. Usefulness of the core outcome measures index in daily clinical practice for assessing patients with degenerative lumbar disease. Adv. Orthop. 2012, 2012, 474685. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dagenais, S.; Yelland, M.J.; Mar, C.D.; Schoene, M.L. Prolotherapy injections for chronic low-back pain. Cochrane Database Syst. Rev. 2007, 2. [Google Scholar] [CrossRef] [Green Version]
- Tuakli-Wosornu, Y.A.; Terry, A.; Boachie-Adjei, K.; Harrison, J.R.; Gribbin, C.K.; LaSalle, E.E.; Nguyen, J.T.; Solomon, J.L.; Lutz, G.E. Lumbar intradiskal platelet-rich plasma (prp) injections: A prospective, double-blind, randomized controlled study. PM&R 2016, 8, 1–10. [Google Scholar]
- El-Kadiry, A.E.-H.; Lumbao, C.; Rafei, M.; Shammaa, R. Autologous bmac therapy improves spinal degenerative joint disease in lower back pain patients. Front. Med. 2021, 8, 309. [Google Scholar] [CrossRef] [PubMed]
- Kumar, H.; Ha, D.-H.; Lee, E.-J.; Park, J.H.; Shim, J.H.; Ahn, T.-K.; Kim, K.-T.; Ropper, A.E.; Sohn, S.; Kim, C.-H.; et al. Safety and tolerability of intradiscal implantation of combined autologous adipose-derived mesenchymal stem cells and hyaluronic acid in patients with chronic discogenic low back pain: 1-year follow-up of a phase i study. Stem Cell Res. Ther. 2017, 8, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Magalhaes, F.N.; Dotta, L.; Sasse, A.; Teixeira, M.J.; Fonoff, E.T. Ozone therapy as a treatment for low back pain secondary to herniated disc: A systematic review and meta-analysis of randomized controlled trials. Pain Physician 2012, 15, E115–E129. [Google Scholar] [PubMed]
- Estefan, M.; Estefan, V. Intradiscal Electrothermal Therapy. StatPearls [Internet]. Available online: https://www.ncbi.nlm.nih.gov/books/NBK549805/ (accessed on 20 October 2020).
- Bonaldi, G. Automated percutaneous lumbar discectomy: Technique, indications and clinical follow-up in over 1000 patients. Neuroradiology 2003, 45, 735–743. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S.; Wu, P.H.; Jang, I.T. Lumbar degenerative disease part 1: Anatomy and pathophysiology of intervertebral discogenic pain and radiofrequency ablation of basivertebral and sinuvertebral nerve treatment for chronic discogenic back pain: A prospective case series and review of literature. Int. J. Mol. Sci. 2020, 21, 1483. [Google Scholar]
- Cunha, C.; Silva, A.J.; Pereira, P.; Vaz, R.; Gonçalves, R.M.; Barbosa, M.A. The inflammatory response in the regression of lumbar disc herniation. Arthritis Res. Ther. 2018, 20, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chiu, C.C.; Chuang, T.Y.; Chang, K.H.; Wu, C.H.; Lin, P.W.; Hsu, W.Y. The probability of spontaneous regression of lumbar herniated disc: A systematic review. Clin. Rehabil. 2015, 29, 184–195. [Google Scholar] [CrossRef]
- Takada, E.; Takahashi, M.; Shimada, K. Natural history of lumbar disc hernia with radicular leg pain: Spontaneous MRI changes of the herniated mass and correlation with clinical outcome. J. Orthop. Surg. 2001, 9, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Peng, B.; Fu, X.; Pang, X.; Li, D.; Liu, W.; Gao, C.; Yang, H. Prospective clinical study on natural history of discogenic low back pain at 4 years of follow-up. Pain Physician 2012, 15, 525–532. [Google Scholar] [CrossRef] [PubMed]
- Latka, D.; Miekisiak, G.; Jarmuzek, P.; Lachowski, M.; Kaczmarczyk, J. Treatment of lumbar disc herniation with radiculopathy. Clinical practice guidelines endorsed by The Polish Society of Spinal Surgery. Neurol. I Neurochir. Pol. 2016, 50, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Bono, C.M.; Ghiselli, G.; Gilbert, T.J.; Kreiner, D.S.; Reitman, C.; Summers, J.T.; Baisden, J.L.; Easa, J.; Fernand, R.; Lamer, T.; et al. An evidence-based clinical guideline for the diagnosis and treatment of cervical radiculopathy from degenerative disorders. The Spine J. 2011, 11, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; Manchikanti, L.; Kaye, A.D.; Abd-Elsayed, A. Treatment of discogenic low back pain: Current treatment strategies and future options—a literature review. Curr. Pain Headache Rep. 2019, 23, 1–9. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Discogenic Pain | Radiculopathy |
|---|---|---|
| Sex | 37 M, 8 F | 12 M, 10 F |
| Age | 44 (10) | 50 (10) |
| Profession | WCW: 6, LW: 12, HW: 19, UN: 8 | WCW: 3, LW: 11, HW: 2, UN: 6 |
| Operated levels | L2/L3: 5, L3/L4: 9, L4/L5: 24 L5/L6: 3, L5/S1: 4 | L3/L4: 6, L4/L5: 13 L5/L6: 1, L5/S1: 2 |
| Parameter | Baseline | F1 (4–8 wks) | F2 (12–24 wks) | F3 (24–36 wks) | F4 (36–52 wks) |
|---|---|---|---|---|---|
| Discogenic pain | |||||
| COMI | 6.40 | 4.61 | 3.90 | 3.16 | 2.20 |
| (5.88–6.92) | (3.80–5.43) | (2.81–4.99) | (2.37–3.95) | (1.53–2.87) | |
| VA [cm] | 6.33 | 4.03 | 4.91 | 3.55 | 2.97 |
| (5.74–6.92) | (3.17–4.89) | (3.76–6.06) | (2.66–4.44) | (2.02–3.92) | |
| VAS back [cm] | 6.15 | 3.68 | 3.30 | 2.84 | 1.80 |
| (5.57–6.73) | (2.70–4.66) | (2.21–4.39) | (2.01–3.67) | (1.22–2.38) | |
| VAS leg [cm] | 3.57 | 2.76 | 2.62 | 2.26 | 1.60 |
| (2.71–4.30) | (1.59–3.81) | (1.45–3.79) | (1.38–3.14) | (1.00–2.20) | |
| Radiculopathy | |||||
| COMI | 7.05 | 4.13 | 3.62 | 2.57 | 3.68 |
| (6.33–7.76) | (3.10–5.16) | (2.06–5.18) | (1.20–3.94) | (2.48–4.88) | |
| VAS [cm] | 6.77 | 4.00 | 4.00 | 2.33 | 3.13 |
| (5.89–7.65) | (2.84–5.16) | (2.19–5.81) | (1.35–3.31) | (1.79–4.47) | |
| VAS back [cm] | 5.14 | 3.17 | 2.76 | 1.55 | 3.14 |
| (3.98–6.30) | (2.14–4.20) | (1.19–4.33) | (0.68–2.42) | (2.14–4.14) | |
| VAS leg [cm] | 5.95 | 3.33 | 2.24 | 1.45 | 2.57 |
| (4.94–6.96) | (2.19–4.47) | (0.83–3.65) | (0.23–2.67) | (1.19–3.95) |
| Consumption of Analgesics | Discogenic Pain | Radiculopathy | ||
|---|---|---|---|---|
| Pre | Post | Pre | Post | |
| 0 (no) | 5 | 28 | 2 | 13 |
| 1 (once a week) | 4 | 7 | 2 | 3 |
| 2 (several times a week) | 5 | 1 | 4 | 0 |
| 3 (once a day) | 8 | 0 | 2 | 0 |
| 4 (several times a day) | 16 | 2 | 6 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Latka, K.; Kozlowska, K.; Waligora, M.; Kolodziej, W.; Olbrycht, T.; Chowaniec, J.; Hendryk, S.; Latka, M.; Latka, D. Efficacy of DiscoGel in Treatment of Degenerative Disc Disease: A Prospective 1-Year Observation of 67 Patients. Brain Sci. 2021, 11, 1434. https://doi.org/10.3390/brainsci11111434
Latka K, Kozlowska K, Waligora M, Kolodziej W, Olbrycht T, Chowaniec J, Hendryk S, Latka M, Latka D. Efficacy of DiscoGel in Treatment of Degenerative Disc Disease: A Prospective 1-Year Observation of 67 Patients. Brain Sciences. 2021; 11(11):1434. https://doi.org/10.3390/brainsci11111434
Chicago/Turabian StyleLatka, Kajetan, Klaudia Kozlowska, Marek Waligora, Waldemar Kolodziej, Tomasz Olbrycht, Jacek Chowaniec, Stanislaw Hendryk, Miroslaw Latka, and Dariusz Latka. 2021. "Efficacy of DiscoGel in Treatment of Degenerative Disc Disease: A Prospective 1-Year Observation of 67 Patients" Brain Sciences 11, no. 11: 1434. https://doi.org/10.3390/brainsci11111434
APA StyleLatka, K., Kozlowska, K., Waligora, M., Kolodziej, W., Olbrycht, T., Chowaniec, J., Hendryk, S., Latka, M., & Latka, D. (2021). Efficacy of DiscoGel in Treatment of Degenerative Disc Disease: A Prospective 1-Year Observation of 67 Patients. Brain Sciences, 11(11), 1434. https://doi.org/10.3390/brainsci11111434








