Safety and Efficacy of Eculizumab Therapy in Multiple Sclerosis: A Case Series
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Filippi, M.; Bar-Or, A.; Piehl, F.; Preziosa, P.; Solari, A.; Vukusic, S.; Rocca, M.A. Multiple sclerosis. Nat. Rev. Dis. Primers. 2018, 4, 43. [Google Scholar] [CrossRef] [PubMed]
- Keegan, B.; Noseworthy, J. Multiple sclerosis. Annu Rev. Med. 2002, 53, 285–302. [Google Scholar] [CrossRef]
- Lucchinetti, C.; Bruck, W.; Parisi, J.; Scheithauer, B.; Rodriguez, M.; Lassmann, H. Heterogeneity of multiple sclerosis lesions: Implications for the pathogenesis of demyelination. Ann. Neurol. 2000, 47, 707–717. [Google Scholar] [CrossRef]
- Brennan, F.H.; Anderson, A.J.; Taylor, S.M.; Woodruff, T.M.; Ruitenberg, M.J. Complement activation in the injured central nervous system: Another dual-edged sword? J. Neuroinflamm. 2012, 9, 137. [Google Scholar] [CrossRef] [PubMed]
- Sellebjerg, F.; Jaliashvili, I.; Christiansen, M.; Garred, P. Intrathecal activation of the complement system and disability in multiple sclerosis. J. Neurol. Sci. 1998, 157, 168–174. [Google Scholar] [CrossRef]
- Kwok, J.Y.; Vaida, F.; Augst, R.M.; Yu, D.Y.; Singh, K.K. Mannose binding lectin mediated complement pathway in multiple sclerosis. J. Neuroimmunol. 2011, 239, 98–100. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ingram, G.; Hakobyan, S.; Hirst, C.L.; Harris, C.L.; Loveless, S.; Mitchell, J.P.; Pickersgill, T.P.; Robertson, N.P.; Morgan, B.P. Systemic complement profiling in multiple sclerosis as a biomarker of disease state. Mult. Scler. 2012, 18, 1401–1411. [Google Scholar] [CrossRef]
- Watkins, L.M.; Neal, J.W.; Loveless, S.; Michailidou, I.; Ramaglia, V.; Rees, M.I.; Reynolds, R.; Robertson, N.P.; Morgan, B.P.; Howell, O.W. Complement is activated in progressive multiple sclerosis cortical grey matter lesions. J. Neuroinflamm. 2016, 13, 161. [Google Scholar] [CrossRef] [PubMed]
- Loveless, S.; Neal, J.W.; Howell, O.W.; Harding, K.E.; Sarkies, P.; Evans, R.; Bevan, R.J.; Hakobyan, S.; Harris, C.L.; Robertson, N.P.; et al. Tissue microarray methodology identifies complement pathway activation and dysregulation in progressive multiple sclerosis. Brain Pathol. 2017, 28, 507–520. [Google Scholar] [CrossRef]
- Tatomir, A.; Talpos-Caia, A.; Anselmo, F.; Kruszewski, A.M.; Boodhoo, D.; Rus, V.; Rus, H. The complement system as a biomarker of disease activity and response to treatment in multiple sclerosis. Immunol. Res. 2017, 65, 1103–1109. [Google Scholar] [CrossRef]
- Morgan, B.P.; Harris, C.L. Complement, a target for therapy in inflammatory and degenerative diseases. Nat. Rev. Drug Discov. 2015, 14, 857–877. [Google Scholar] [CrossRef] [PubMed]
- Hunt, D.; Kavanagh, D.; Drummond, I.; Weller, B.; Bellamy, C.; Overell, J.; Evans, S.; Jackson, A.; Chandran, S. Thrombotic microangiopathy associated with interferon β. N. Engl. J. Med. 2014, 370, 1270–1271. [Google Scholar] [CrossRef] [PubMed]
- Allinovi, M.; Cirami, C.L.; Caroti, L.; Antognoli, G.; Farsetti, S.; Amato, M.P.; Minetti, E.E. Thrombotic microangiopathy induced by interferon β in patients with multiple sclerosis: Three cases treated with Eculizumab. Clin. Kidney J. 2017, 10, 625–631. [Google Scholar] [CrossRef][Green Version]
- Gianassi, I.; Allinovi, M.; Caroti, L.; Cirami, C. Broad spectrum of interferon-related nephropathies: Glomerulonephritis, systemic lupus erythematosus-like syndrome and thrombotic microangiopathy. A case report and review of literature. World J. Nephrol. 2019, 8, 109–117. [Google Scholar]
- Dauvergne, M.; Buob, D.; Rafat, C.; Hennino, M.F.; Lemoine, M.; Audard, V.; Chauveau, D.; Ribes, D.; Cornec-Le Gall, E.; Daugas, E.; et al. Renal diseases secondary to interferon-beta treatment: A multicenter clinico-pathological study and a systematic literature review. Clin. Kidney J. 2021, 1–10. [Google Scholar] [CrossRef]
- Aigner, C.; Schmidt, A.; Gaggl, M.; Sunder-Plassmann, G. An updated classification of thrombotic microangiopathies and treatment of complement gene variant-mediated thrombotic microangiopathy. Clin. Kidney J. 2019, 12, 333–337. [Google Scholar] [CrossRef]
- Legendre, C.M.; Licht, C.; Muus, P.; Greenbaum, L.A.; Babu, S.; Bedrosian, C.; Bingham, C.; Cohen, D.J.; Delmas, Y.; Douglas, K.; et al. Terminal complement inhibitor eculizumab in atypical hemolytic-uremic syndrome. N. Engl. J. Med. 2013, 368, 2169–2181. [Google Scholar] [CrossRef]
- Román, E.; Mendizábal, S.; Jarque, I.; de la Rubia, J.; Sempere, A.; Morales, E.; Praga, M.; Ávila, A.; Górriz, J.L. Secondary thrombotic microangiopathy and eculizumab: A reasonable therapeutic option. Nefrologia 2017, 37, 478–491. [Google Scholar] [CrossRef]
- Caravaca-Fontan, F.; Praga, M. Complement inhibitors are useful in secondary hemolytic uremic syndromes. Kidney Int. 2019, 96, 826–829. [Google Scholar] [CrossRef]
- Carpanini, S.M.; Torvell, M.; Morgan, B.P. Therapeutic Inhibition of the Complement System in Diseases of the Central Nervous System. Front. Immunol. 2019, 10, 362. [Google Scholar] [CrossRef]
- Howard, J.F., Jr.; Barohn, R.J.; Cutter, G.R.; Freimer, M.; Juel, V.C.; Mozaffar, T.; Mellion, M.L.; Benatar, M.G.; Farrugia, M.E.; Wang, J.J.; et al. A randomized, double-blind, placebo-controlled phase II study of Eculizumab in patients with refractory generalized myasthenia gravis. Muscle Nerve. 2013, 48, 76–84. [Google Scholar] [CrossRef]
- Pittock, S.J.; Berthele, A.; Fujihara, K.; Kim, H.J.; Levy, M.; Palace, J.; Nakashima, I.; Terzi, M.; Totolyan, N.; Viswanathan, S.; et al. Eculizumab in Aquaporin-4-Positive Neuromyelitis Optica Spectrum Disorder. N. Engl. J. Med. 2019, 381, 614–625. [Google Scholar] [CrossRef] [PubMed]
- Lublin, F.D.; Reingold, S.C.; Cohen, J.A.; Cutter, G.R.; Sørensen, P.S.; Thompson, A.J.; Wolinsky, J.S.; Balcer, L.J.; Banwell, B.; Barkhof, F.; et al. Defining the clinical course of multiple sclerosis: The 2013 revisions. Neurology 2014, 83, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Lublin, F.D.; Reingold, S.C. Defining the clinical course of multiple sclerosis: Results of an international survey. National Multiple Sclerosis Society (USA) Advisory Committee on Clinical Trials of New Agents in Multiple Sclerosis. Neurology 1996, 46, 907–911. [Google Scholar] [CrossRef]
- Milan Manani, S.; Virzì, G.M.; Gastaldon, F.; Proglio, M.; Brocca, A.; Ronco, C. Brief Review and a Clinical Case of Hemolytic Uremic Syndrome Associated with Interferon β Treatment. Blood Purif. 2017, 43, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Parisi, M.; Manni, A.; Caputo, F.; Trojano, M.; Paolicelli, D. A case report of late-onset atypical Hemolytic Uremic Syndrome during interferon beta in multiple sclerosis: Open issues in literature review. Brain Behav. 2020, 11, e01930. [Google Scholar] [CrossRef]
- Rus, H.; Cudrici, C.; Niculescu, F. C5b-9 complement complex in autoimmune demyelination: Dual role in neuroinflammation and neuroprotection. Adv. Exp. Med. Biol. 2006, 586, 139–151. [Google Scholar] [PubMed]
- Kavanagh, D.; McGlasson, S.; Jury, A.; Williams, J.; Scolding, N.; Bellamy, C.; Gunther, C.; Ritchie, D.; Gale, D.P.; Kanwar, Y.S.; et al. Type I interferon causes thrombotic microangiopathy by a dose-dependent toxic effect on the microvasculature. Blood 2016, 128, 2824. [Google Scholar] [CrossRef] [PubMed]

| Patients (n = 9) | |
|---|---|
| Females, n (%) | 5 (55.6) |
| Age, mean, years (SD) | 45.3 (5.3) |
| Age at MS onset, mean, years (SD) | 24.2 (7) |
| Length of IFN-β therapy, mean, years (SD) | 13.9 (3.9) |
| Length of follow-up on eculizumab therapy, mean, years (SD) | 3.72 (2.58) |
| Pre-Eculizumab (n = 9) | Post-Eculizumab (n = 9) | p | |
|---|---|---|---|
| Relapses, n (%) | 1 (11.1) | 1 (11.1) | 0.999 3 |
| New MRI T2 lesions, n (%) | 4 (45) | 2 (22.2) 1 | 0.625 3 |
| New MRI Gd+ lesions, n (%) | 1 (11.1) | 0 (0.0) 2 | 0.999 3 |
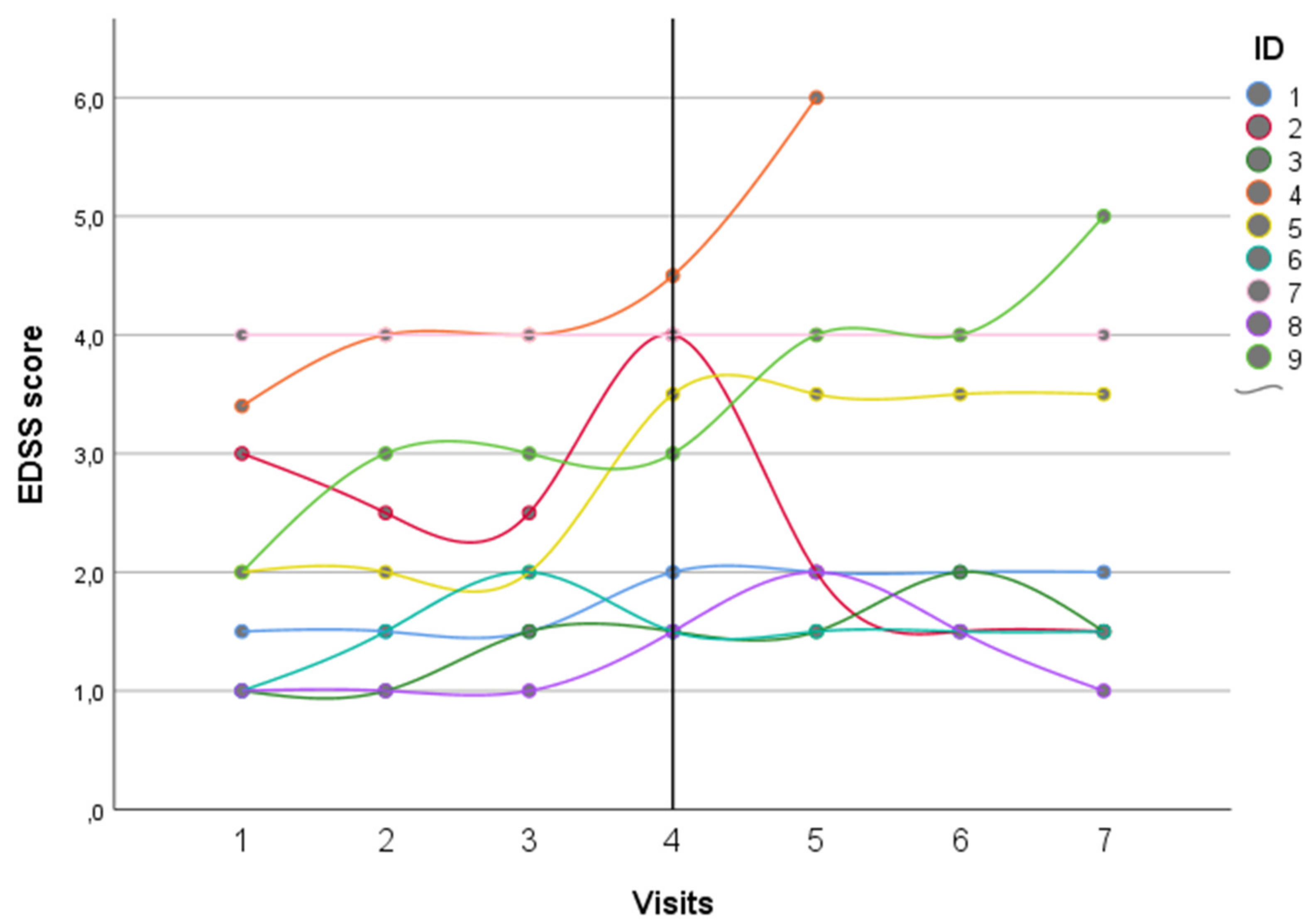
| EDSS Score, median (IQR) | 2 (1.5–4.5) | 3 (1.5–4.0) | 0.898 4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Allinovi, M.; Bellinvia, A.; Pesce, F.; Milan Manani, S.; Razzolini, L.; Brezzi, B.; Protopapa, P.; Mantero, V.; Caroti, L.; Cirami, C.L.; et al. Safety and Efficacy of Eculizumab Therapy in Multiple Sclerosis: A Case Series. Brain Sci. 2021, 11, 1341. https://doi.org/10.3390/brainsci11101341
Allinovi M, Bellinvia A, Pesce F, Milan Manani S, Razzolini L, Brezzi B, Protopapa P, Mantero V, Caroti L, Cirami CL, et al. Safety and Efficacy of Eculizumab Therapy in Multiple Sclerosis: A Case Series. Brain Sciences. 2021; 11(10):1341. https://doi.org/10.3390/brainsci11101341
Chicago/Turabian StyleAllinovi, Marco, Angelo Bellinvia, Francesco Pesce, Sabrina Milan Manani, Lorenzo Razzolini, Brigida Brezzi, Paolo Protopapa, Vittorio Mantero, Leonardo Caroti, Calogero Lino Cirami, and et al. 2021. "Safety and Efficacy of Eculizumab Therapy in Multiple Sclerosis: A Case Series" Brain Sciences 11, no. 10: 1341. https://doi.org/10.3390/brainsci11101341
APA StyleAllinovi, M., Bellinvia, A., Pesce, F., Milan Manani, S., Razzolini, L., Brezzi, B., Protopapa, P., Mantero, V., Caroti, L., Cirami, C. L., Amato, M. P., & Del Vecchio, L. (2021). Safety and Efficacy of Eculizumab Therapy in Multiple Sclerosis: A Case Series. Brain Sciences, 11(10), 1341. https://doi.org/10.3390/brainsci11101341






