Sleep, Function, Behaviour and Cognition in a Cohort of Children with Down Syndrome
Abstract
1. Introduction
2. Materials and Methods
2.1. Exclusion Criteria
2.2. Outcome Measures
2.2.1. Child Sleep Habits Questionnaire
2.2.2. Life Habits Questionnaire
2.2.3. Child Behaviour Checklist
2.2.4. Stanford–Binet Intelligence Scales-5th Edition
2.2.5. Polysomnography Data
2.3. Statisical Analysis
3. Results
3.1. Sleep Treatments Prior to Recruitment
3.2. Sleep Data
3.3. Functional Assessment
3.4. Behavioural Assessment
3.5. Psychology Assessment
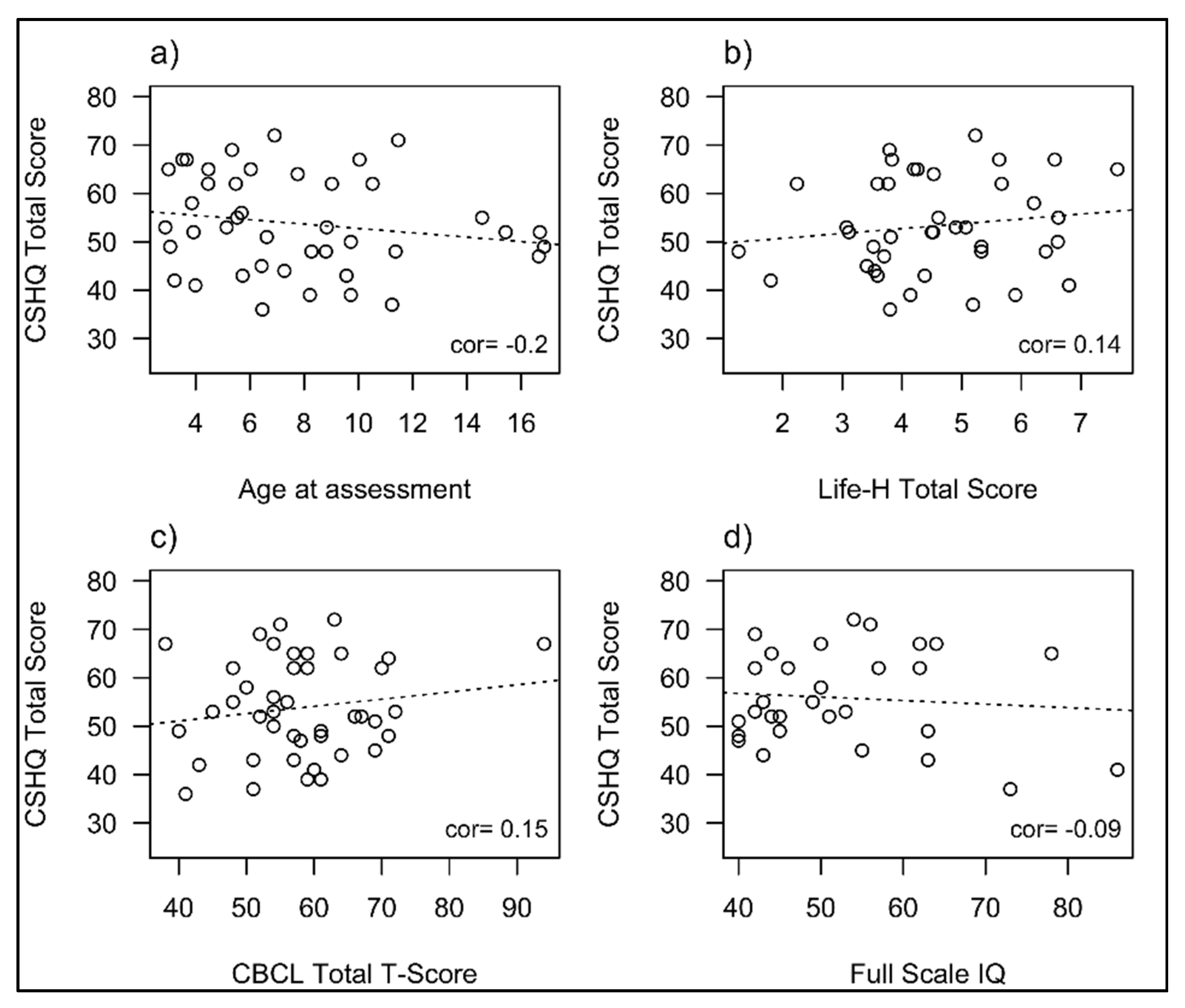
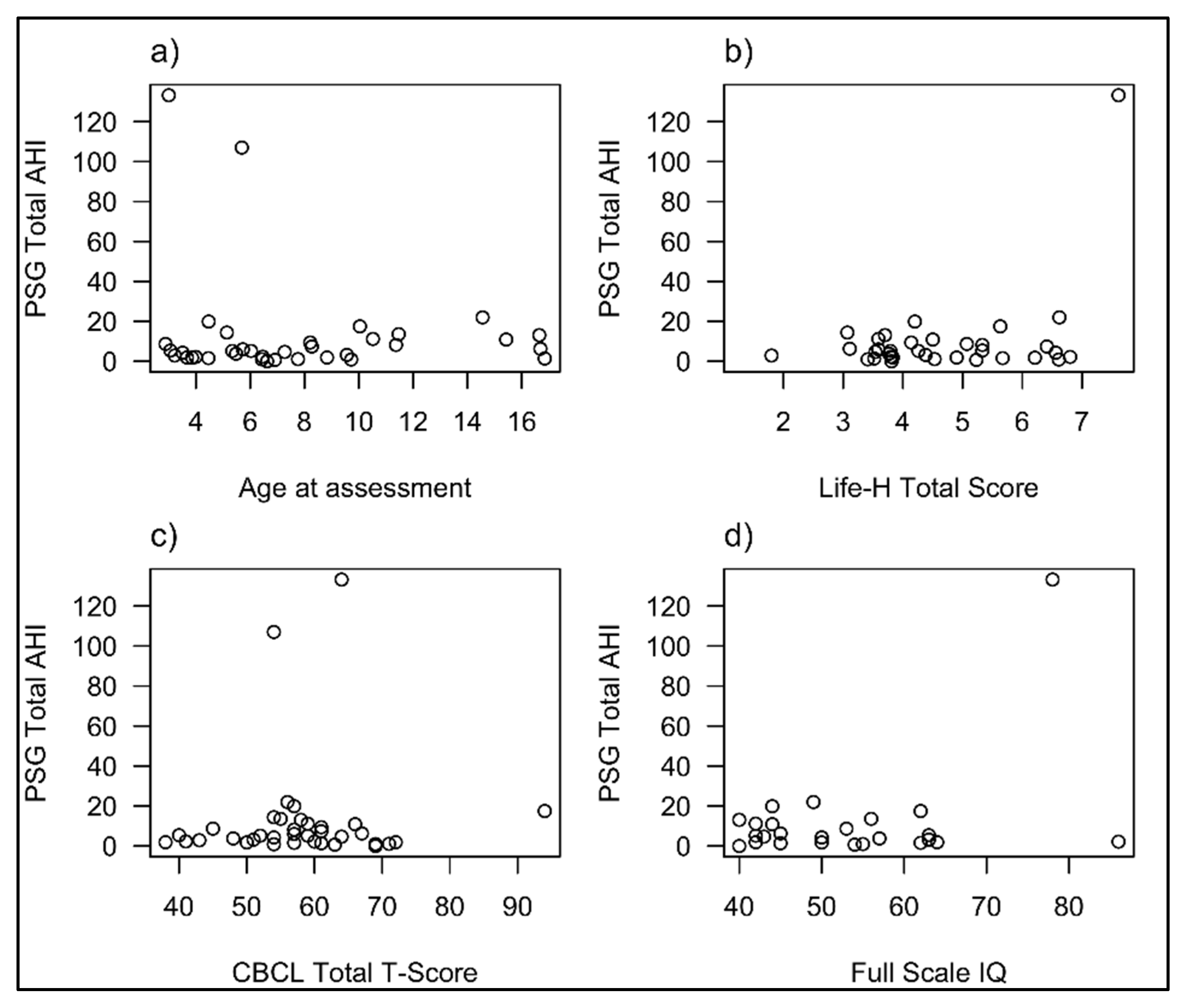
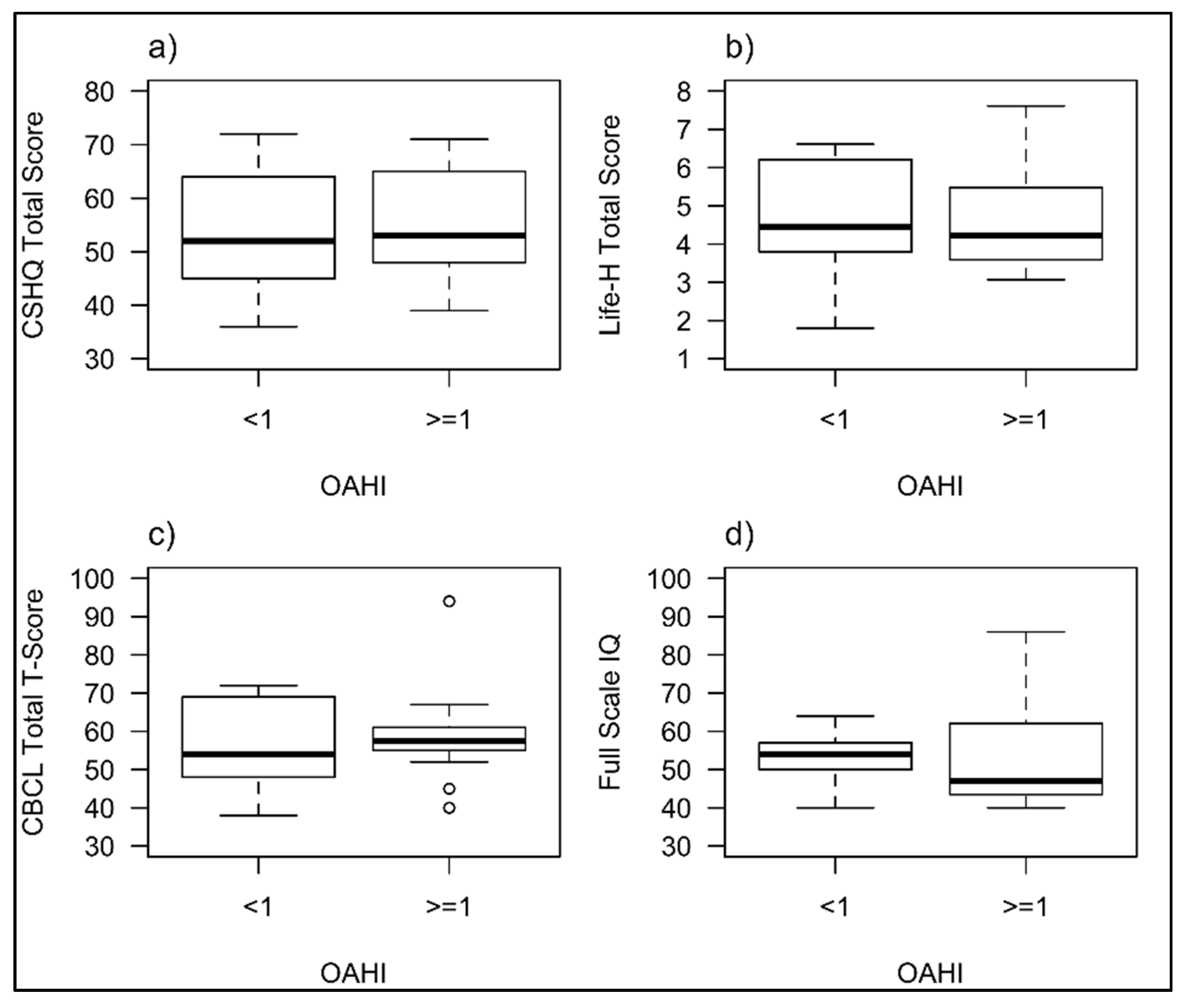
3.6. Relationship between Sleep and Outcomes at Baseline
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Irving, C.; Basu, A.; Richmond, S.; Burn, J.; Wren, C. Twenty-year trends in prevalence and survival of Down syndrome. Eur. J. Hum. Genet. 2008, 16, 1336–1340. [Google Scholar] [CrossRef]
- Sherman, S.; Allen, E.G.; Bean, L.H.; Freeman, S.B. Epidemiology of Down syndrome. Ment. Retard. Dev. Disabil. Res. Rev. 2007, 13, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Sommer, C.A.; Henrique-Silva, F. Trisomy 21 and Down syndrome: A short review. Braz. J. Biol. 2008, 68, 447–452. [Google Scholar] [CrossRef] [PubMed]
- Churchill, S.S.; Kieckhefer, G.M.; Landis, C.A.; Ward, T.M. Sleep measurement and monitoring in children with Down syndrome: A review of the literature, 1960–2010. Sleep Med. Rev. 2012, 16, 477–488. [Google Scholar] [CrossRef] [PubMed]
- Karmiloff-Smith, A.; Al-Janabi, T.; D’Souza, H.; Groet, J.; Massand, E.; Mok, K.; Startin, C.; Fisher, E.; Hardy, J.; Nizetic, D.; et al. The importance of understanding indivdiual differences in Down syndrome. F1000Research 2016, 5, 389. [Google Scholar] [CrossRef] [PubMed]
- Marcus, C.L.; Keens, T.G.; Bautista, D.B.; Von Pechmann, W.S.; Ward, S.L. Obstructive sleep apnea in children with Down Syndrome. Pediatrics 1991, 88, 132–139. [Google Scholar] [PubMed]
- De Miguel-Diez, J.; Villa-Asensi, J.R.; Alvarez-Sala, J.L. Prevalence of sleep-disordered breathing in children with Down syndrome: Polygraphic findings in 108 children. Sleep 2003, 26, 1006–1009. [Google Scholar] [CrossRef] [PubMed]
- Stebbens, V.; Dennis, J.; Samuels, M.P.; Croft, C.B.; Southall, D.P. Sleep related upper airway obstruction in a cohort with Down’s syndrome. Arch. Dis. Child. 1991, 66, 1333–1338. [Google Scholar] [CrossRef]
- Ng, D.K.; Hui, H.N.; Chan, C.H.; Kwok, K.L.; Chow, P.Y.; Cheung, J.M.; Leung, S.Y. Obstructive sleep apnoea in children with Down syndrome. Singap. Med. J. 2006, 47, 774–779. [Google Scholar]
- Dyken, M.E.; Lin-Dyken, D.C.; Poulton, S.; Zimmerman, M.B.; Sedars, E. Prospective polysomnographic analysis of obstructive sleep apnea in Down syndrome. Arch. Pediatr. Adolesc. Med. 2003, 157, 655–660. [Google Scholar] [CrossRef]
- Marcus, C.; Brooks, L.J.; Draper, K.A.; Gozal, D.; Halbower, A.C.; Jones, J.; Schechter, M.S.; Sheldon, S.; Spruyt, K.; Ward, S.D.; et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Clinical report. Pediatrics 2012, 130, 576–584. [Google Scholar] [CrossRef]
- Carter, M.; McCaughey, E.; Annaz, D.; Hill, C.M. Sleep problems in a Down syndrome population. Arch. Dis. Child. 2009, 94, 308–310. [Google Scholar] [CrossRef]
- Hoffmire, C.A.; Magyar, C.I.; Connolly, H.V.; Fernandez, I.D.; Van Wijngaarden, E. High prevalence of sleep disorders and associated comorbidities in a community sample of children with Down syndrome. J. Clin. Sleep Med. 2014, 10, 411–419. [Google Scholar] [CrossRef] [PubMed]
- Rosen, D.; Lombardo, A.; Skotko, B.; Davidson, E.J. Parental perceptions of sleep disturbances and sleep disordered breathing in children with Down syndrome. Clin. Pediatr. 2011, 50, 121–125. [Google Scholar] [CrossRef] [PubMed]
- Cotton, S.; Richdale, A. Brief report: Parental descriptions if sleep problems in children with autism, Down syndrome and Prader-Willi syndrome. Res. Dev. Disabil. 2006, 27, 151–161. [Google Scholar] [CrossRef]
- Breslin, J.H.; Edgin, J.O.; Bootzin, R.R.; Goodwin, J.L.; Nadel, L. Parental report of sleep problems in Down syndrome. J. Intellect. Disabil. Res. 2011, 55, 1086–1091. [Google Scholar] [CrossRef] [PubMed]
- Maris, M.; Verhulst, S.; Woiciechowski, M.; Van de Heyning, P.; Boudewyns, A. Sleep problems and obstructive sleep apnoea in children with down syndrome, an overview. Int. J. Pediatric Otorhinolaryngol. 2016, 82, 12–15. [Google Scholar] [CrossRef] [PubMed]
- Maski, K.P.; Kothare, S. Sleep deprivation and neurobehavioral functioning in children. Int. J. Psychophysiol. 2013, 89, 259–264. [Google Scholar] [CrossRef]
- Beebe, D.W. Neurobehavioural morbidity associated with disordered breathing in sleep in children: A comprehensive review. Sleep 2006, 29, 1115–1134. [Google Scholar] [CrossRef]
- Blunden, S.; Lushington, K.; Lorenzen, B.; Martin, J.; Kennedy, D. Neuropsychological and psychosocial function in children with a history of snoring or behavioural problems. J. Pediatr. 2005, 146, 780–786. [Google Scholar] [CrossRef]
- Blunden, S.; Lorenzen, B.; Martin, J.; Kennedy, D. Behavior and neurocognitive performance in children aged 5-10 years who snore compared to controls. J. Clin. Exp. Neuropsych. 2000, 22, 554–568. [Google Scholar] [CrossRef]
- Bourke, R.; Anderson, V.; Yang, J.; Jackman, A.R.; Killedar, A.; Nixon, G.M.; Davey, M.J.; Walker, A.M.; Trinder, J.; Horne, R.S.C. Cognitive and academic functions are impaired in children with all severities of sleep-disordered breathing. Sleep Med. 2011, 12, 489–496. [Google Scholar] [CrossRef]
- Marcus, C.L.; Moore, R.H.; Rosen, C.L.; Giordani, B.; Garetz, S.L.; Taylor, H.G.; Mitchell, R.B.; Amin, R.; Katz, E.S.; Arens, R.; et al. A randomized trial of adenotonsillectomy for childhood sleep apnea. N. Engl. J. Med. 2013, 368, 2366–2376. [Google Scholar] [CrossRef] [PubMed]
- Breslin, J.; Spanò, G.; Bootzin, R.; Anand, P.; Nadel, L.; Edgin, J. Obstructive sleep apnea syndrome and cognition in Down Syndrome. Dev. Med. Child Neurol. 2014, 56, 657–664. [Google Scholar] [CrossRef] [PubMed]
- Churchill, S.S.; Kieckhefer, G.M.; Bjornson, K.F.; Herting, J.R. Relationship between sleep disturbance and functional outcomes in daily life habits of children with Down syndrome. Sleep 2015, 38, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Spano, G.; Edgin, J.O. The impact of sleep disruption on executive function in Down syndrome. Res. Dev. Disabil. 2013, 34, 2033–2039. [Google Scholar] [CrossRef] [PubMed]
- Edgin, J.O.; Tooley, U.; Demara, B.; Nyhuis, C.; Anand, P.; Spanò, G. Sleep disturbance and expressive language development in preschool-age children with Down syndrome. Child Dev. 2015, 86, 1984–1998. [Google Scholar] [CrossRef] [PubMed]
- Lukowski, A.; Milojevich, H.M. Sleep problems and temperament in young children with Down syndrome and typically develping controls. J. Intellect. Dis. Res 2017, 61, 221–232. [Google Scholar] [CrossRef] [PubMed]
- Esbensen, A.J.; Hoffman, E.K.; Beebe, D.W.; Byars, K.C.; Epstein, J. Links between sleep and daytime behaviour problems in children with Down syndrome. J. Intellect. Disabil. Res. 2018, 62, 115–125. [Google Scholar] [CrossRef] [PubMed]
- Kelmanson, I. Sleep disturbances, behavioural problems and adaptive skills in children with DS. Early Child Dev. Care 2017, 187, 1679–1693. [Google Scholar] [CrossRef]
- NICHID SECCYD-Wisconsin. Children’s Sleep Habit Questionnaire (Abbreviated). 2014. Available online: http://njaap.org/wp-content/uploads/2016/04/Childrens-Sleep-Habits-Questionnaire.pdf (accessed on 26 July 2016).
- Owens, J.A.; Spirito, A.; McGuinn, M. The children’s sleep habits questionnaire (CSHQ): Psychometric properties of a survey instrument for school-aged children. Sleep 2000, 23, 1043–1051. [Google Scholar] [CrossRef] [PubMed]
- Bassell, J.L.; Phan, H.; Leu, R.; Kronk, R.; Visootsak, J. Sleep profiles in children with Down syndrome. Am. J. Med. Genet. Part A 2015, 167, 1830–1835. [Google Scholar] [CrossRef]
- Ashworth, A.; Hill, C.; Karmiloff-Smith, A.; Dimitriou, D. Cross syndrome comparison of sleep problems in children with Down syndrome and Williams syndrome. Res. Dev. Disabil. 2013, 34, 1572–1580. [Google Scholar] [CrossRef] [PubMed]
- Irwanto, N.; Rehatta, M.; Hartini, S.; Takada, S. Sleep problems of children with autistic spectrum disorder assessed by childrens sleep habits questionnaire-abbreviated in Indonesia and Japan. Kobe J. Med. Sci. 2016, 62, E22–E26. [Google Scholar]
- Palacio-Ortiz, J.; Gomez-Cano, S.; Aguirre-Acevedo, D.C. Sleep problems and profiles in attention deficit hyperactivity disorder assessed by the childrens sleep habit questionnaire abbreviated in colombia. Salud Ment. 2018, 41, 261–269. [Google Scholar] [CrossRef]
- Hartman, A.G.; Terhorst, L.; Little, N.; Bendixen, R.M. Uncovering sleep in young males with Duchenne muscular dystrophy. Eur. J. Paediatr. Neurol. 2020, 26, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Noreau, L.; Lepage, C.; Boissiere, L.; Picard, R.; Fougeyrollas, P.; Mathieu, J.; Desmarais, G.; Nadeau, L. Measuring participation in children with disabilities using the assessment of life habits. Dev. Med. Child Neurol. 2007, 49, 666–671. [Google Scholar] [CrossRef]
- Achenbach, T.M.; Rescorla, L.A. Manual for the ASEBA Preschool Forms and Profiles; University of Vermont: Burlington, VT, USA, 2000. [Google Scholar]
- Achenbach, T.M.; Rescorla, L.A. Manual for the ASEBA School-Age Forms and Profiles; University of Vermont: Burlington, VT, USA, 2001. [Google Scholar]
- Noterdaeme, M.; Mino, F.; Amorosa, H. Applicability of the child behaviour checklist in developmentally delayed children. Z. Kinder Jugendpsychiatrie Psychother. 1999, 27, 183–188. [Google Scholar] [CrossRef]
- De Ruiter, K.P.; Dekker, M.C.; Verhulst, F.C.; Koot, H.M. Developmental course of psychopathology in youths with and without intellectual disabilities. J. Child Psychol. Psychiatry 2007, 48, 498–507. [Google Scholar] [CrossRef]
- Dekker, M.C.; Koot, H.M.; Van Der Ende, J.; Verhulst, F.C. Emotional and behavioral problems in children and adolescents with and without intellectual disability. J. Child Psychol. Psychiatry 2002, 43, 1087–1098. [Google Scholar] [CrossRef]
- Guralnick, M.J.; Connor, R.T.; Johnson, L.C. The peer-related social competence of young children with Down syndrome. Am. J. Intellect. Dev. Disabil. 2011, 116, 48–64. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Van Gameren-Oosterom, H.B.M.; Fekkes, M.; Buitendijk, S.E.; Mohangoo, A.D.; Bruil, J.; Van Wouwe, J.P. Development, problem behavior, and quality of life in a population based sample of eight-year-old children with Down syndrome. PLoS ONE 2011, 6, e21879. [Google Scholar] [CrossRef] [PubMed]
- Roid, G.H. Stanford-Binet Intellegence Scales, 5th ed.; Riverside: Itascal, IL, USA, 2003. [Google Scholar]
- Brooks, L.J.; Olsen, M.N.; Bacevice, A.M.; Beebe, A.; Konstantinopoulou, S.; Taylor, H.G. Relationship between sleep, sleep apnea and neuropsychological function in children with Down syndrome. Sleep Breath. 2015, 19, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Esbensen, A.J.; Hoffman, E.K. Impact of sleep on executive functioning in school-age children with Down syndrome. J. Intellect. Disabil. Res. 2018, 62, 569–580. [Google Scholar] [CrossRef]
- Esbensen, A.; Hooper, S.R.; Fidler, D.; Hartley, S.L.; Edgin, J.; D’Ardhuy, X.L.; Capone, G.; Conners, F.A.; Mervis, C.B.; Abbeduto, L.; et al. Outcome measures for clinical trials in Down syndrome. Am. J. Intellect. Dev. Disabil. 2017, 122, 247–281. [Google Scholar] [CrossRef] [PubMed]
- Berry, R.; Brooks, R.; Gamaldo, C.E.; Harding, S.M.; Lloyd, R.M.; Marcus, C.L.; Vaughn, B.V. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications; Version 2.2.; American Academy of Sleep Medicine: Darien, IL, USA, 2016. [Google Scholar]
- Team, R.C. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2013. [Google Scholar]
- Heise, I.; Fisher, S.P.; Banks, G.; Wells, S.; Peirson, S.N.; Foster, R.G.; Nolan, P.M. Sleep-like behavior and 24-h rhythm disruption in the Tc1 mouse model of Down syndrome. Genes Brain Behav. 2015, 14, 209–216. [Google Scholar] [CrossRef]
- Richdale, A.; Wiggs, L. Behavioural approaches to the treatment of sleep problems in children with developmental disorders: What is state of the art? Int. J. Behav. Consult. Ther. 2005, 1, 165–188. [Google Scholar] [CrossRef]
- Stores, G.; Stores, R. Sleep disorders and their clinical significant in children with Down syndrome. Dev. Med. Child Neurol. 2012, 55, 126–130. [Google Scholar] [CrossRef]
- Esbensen, A.J.; Beebe, D.W.; Byars, K.C.; Hoffman, E.K. Use of sleep evaluations and treatments in children with Down syndrome. J. Dev. Behav. Pediatr. 2016, 37, 629–636. [Google Scholar] [CrossRef] [PubMed]
- Esbensen, A.J.; Hoffman, E.K.; Shaffer, R.; Chen, E.; Patel, L.; Jacola, L. Reliability of parent report measures of behaviour in children with Down syndrome. J. Intellect. Disabil. Res. 2018, 62, 785–797. [Google Scholar] [CrossRef]
- Waters, K.; Chawla, J.; Harris, M.A.; Heussler, H.; Black, R.J.; Cheng, A.T.; Lushington, K. Cognition after early tonsillectomy for mild OSA. Pediatrics 2020, 145, e20191450. [Google Scholar] [CrossRef] [PubMed]
- Chawla, J.K.; Howard, A.; Burgess, S.; Heussler, H. Sleep problems in Australian children with Down syndrome: The need for greater awareness. Sleep Med. 2021, 78, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Owens, J.A.; Spirito, A.; McGuinn, M.; Nobile, C. Sleep habits and sleep disturbance in elementary school-aged children. J. Dev. Behav. Pediatr. 2000, 21, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Halstead, E.J.; Joyce, A.; Sullivan, E.; Tywyn, C.; Davies, K.; Jones, A.; Dimitriou, D. Sleep disturbances and patterns in children with neurodevelopmental conditions. Front. Pediatr. 2021, 9, 91. [Google Scholar] [CrossRef] [PubMed]
| Number of Participants (n) | Percentage (%) | |
|---|---|---|
| Male/Female | 20/22 | 48/52 |
| Respiratory Condition | 17 | 40 |
| Thyroid Disease | 12 | 29 |
| Cardiac Disease | 23 | 55 |
| Another Comorbidity | 19 | 45 |
| Median | IQR | |
| Age at Baseline Assessment (yrs) | 7.0 | (4.5, 9.9) |
| BMI Percentile | 50th | (25, 75) |
| Absolute BMI (Kg/m2) | 17.4 | (16.4, 21.6) |
| Number of Participants (n) | Percentage % | |
| Proportion of Children with BMI ≤2nd Percentile | 2 | 5 |
| Proportion of Children with BMI ≥90th Percentile | 6 | 14 |
| Sum | 8 | 19 |
| Surgical Treatment Prior to Recruitment | ||
| Adenotonsillectomy | 24 | 57.14 |
| No Surgery | 10 | 23.81 |
| Adenoidectomy only | 6 | 14.29 |
| Tonsillectomy only | 2 | 4.76 |
| Sum | 42 | 100.00 |
| CSHQ Total Score | Percentage (%) |
|---|---|
| Proportion of Children clinically elevated total score >41 | 86 (n = 36) |
| CSHQ Total Score | 52.5 (46.5, 62.5) |
| CSHQ Sub-scores (max possible score) | Median (IQR) |
| Bedtime Resistance (35) | 16.5 (12.0, 20.3) |
| Sleep Onset Delay (5) | 2.0 (2.0, 3.0) |
| Sleep Anxiety (10) | 5.0 (2.0, 6.0) |
| Night Wakings (15) | 7.0 (5.8, 9.2) |
| Parasomnias (15) | 7.5 (6.0, 9.0) |
| Sleep Disordered Breathing (5) | 3.0 (2.8, 4.0) |
| Daytime Sleepiness (20) | 9.0 (7.8, 11.0) |
| Questions with >20% Respondents scoring >3 | Percentage Respondents (%) |
| Q3: Child falls asleep alone in own bed | 45.2 |
| Q7: Child needs parent in the room to fall asleep | 45.2 |
| Q8: Child resists going to bed at bedtime | 21.5 |
| Q11: Child is restless and moves a lot during sleep | 76.2 |
| Q12: Child moves to someone else’s bed during the night | 23.8 |
| Q14: Child snores loudly | 45.2 |
| Q16: Child naps during the day | 28.5 |
| Q17: Child wakes up once during the night | 23.8 |
| Q20: Child wakes up very early in the morning | 40.4 |
| Q21: Child falls asleep while involved in activities | 47.6 |
| OSA on PSG | |
| Proportion of children with total OAHI ≥ 1/h | 61% (n = 22) |
| Proportion of children with total OAHI > 2/h | 44% (n = 16) |
| Proportion of children with No OSA (OAHI < 1/h) | 39% (n = 14) |
| Proportion of children with Mild OSA (OAHI (1–5/h) | 28%(n = 10) |
| Proportion of children with Moderate OSA (OAHI 5–10/h) | 14% (n = 5) |
| Proportion of children with Severe OSA (OAHI > 10/h) | 19% (n = 7) |
| PSG Parameter | Median (IQR) |
| PSG Sleep Efficiency (%) | 89 (80.5, 94) |
| PSG Total AHI (per h) | 5.2 (1.90, 11.1) |
| PSG Total OAHI (per h) | 1.6 (0.4, 6.7) |
| PSG REM OAHI (per h) | 3.2 (1.3, 17.4) |
| PSG Total CAI (per h) | 1.9 (0.7, 3.5) |
| PSG REM CAI (per h) | 2.9 (1.0, 6.6) |
| PSG CO2 Maximum (mmHg) | 50.7 (48.6, 56.9) |
| PSG Total Arousal Index (per h) | 8.05 (5.5, 10.1) |
| Measure | DSstudy (3–16 yrs) Median (IQR) n = 40 |
|---|---|
| Life H Total Score | 4.4 (3.6, 5.6) |
| Life H Nutrition Score | 4.2 (2.3, 5.6) |
| Life H Fitness Score | 6.7 (5.6, 8.5) |
| Life H Personal Score | 3.3 (1.9, 5.0) |
| Life H Communication Score | 2.9 (2.0, 4.4) |
| Life H Housing Score | 7.0 (5.2, 8.7) |
| Life H Mobility Score | 4.4 (2.9, 6.4) |
| Life H Responsibilities Score | 3.1 (1.4, 4.6) |
| Life H Relationships Score | 8.3 (6.7, 10.0) |
| Life H Community Score | 3.3 (0, 3.7) |
| Life H Education Score | 3.3 (2.1, 5.4) |
| Life H Recreation Score | 3.6 (2.8, 4.9) |
| Measure | Median (IQR) | Participants in Clinical Concern/ Borderline Clinical Concern Range (%) |
|---|---|---|
| Total T-Score | 57 (51.8, 64) | 35.7 |
| Internalising Problems T-Score | 54.5 (49.8, 61) | 31 |
| Externalising Problems T-Score | 55.5 (46.8, 61.3) | 33.3 |
| Anxious/Depressed T-Score | 51 (50, 53) | 7.1 |
| Withdrawn/Depressed T-Score | 59.5 (53.8, 64.5) | 19 |
| Somatic Complaints T-Score | 59.5 (55.3, 65.3) | 21.4 |
| Social Problems T-Score | 62 (54, 69) | 21.4 |
| Thought Problems T-Score | 62 (54, 70) | 23.8 |
| Attention Problems T-Score | 60 (55, 68.3) | 31 |
| Rule Breaking Behaviour T-Score | 56 (51, 63) | 9.5 |
| Aggressive Behaviour T-Score | 54 (50, 61) | 16.7 |
| Measure | Median (IQR) | No. Participants within Normal Range (Score ≥70) | No. Participants with Mild Impairment (Score 55–69) | No. Participants with Moderate Impairment (Score 40–54) | No. Participants with Severe Impairment (Score <40) |
|---|---|---|---|---|---|
| SB-5 Non-Verbal IQ Score | 52.5 (47.0, 69.8) | 7 (23%) | 7 (23%) | 16 (53%) | 0 |
| SB-5 Verbal IQ Score | 50.0 (43.0, 58.3) | 1 (3%) | 8 (27%) | 21 (70%) | 0 |
| SB-5 Full Scale IQ Score | 50.0 (43.0, 62.0) | 3 (10%) | 8 (27%) | 19 (63%) | 0 |
| SB-5 Fluid Reasoning Score | 54.5 (47.0, 65.8) | 6 (20%) | 9 (30%) | 15 (50%) | 0 |
| SB-5 Knowledge Score | 58.5 (55.0, 77.8) | 10 (33%) | 14 (47%) | 6 (20%) | 0 |
| SB-5 Quantitative Reasoning Score | 56.0 (50.0, 77.75) | 4 (13%) | 13 (43%) | 13 (43%) | 0 |
| SB-5 Visual-Spatial Processing Score | 56.0 (48.0, 62.0) | 3 (10%) | 13 (43%) | 14 (47%) | 0 |
| SB-5 Working Memory Score | 54.0 (48.0, 60.8) | 5 (17%) | 9 (30%) | 16 (53%) | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chawla, J.K.; Bernard, A.; Heussler, H.; Burgess, S. Sleep, Function, Behaviour and Cognition in a Cohort of Children with Down Syndrome. Brain Sci. 2021, 11, 1317. https://doi.org/10.3390/brainsci11101317
Chawla JK, Bernard A, Heussler H, Burgess S. Sleep, Function, Behaviour and Cognition in a Cohort of Children with Down Syndrome. Brain Sciences. 2021; 11(10):1317. https://doi.org/10.3390/brainsci11101317
Chicago/Turabian StyleChawla, Jasneek K., Anne Bernard, Helen Heussler, and Scott Burgess. 2021. "Sleep, Function, Behaviour and Cognition in a Cohort of Children with Down Syndrome" Brain Sciences 11, no. 10: 1317. https://doi.org/10.3390/brainsci11101317
APA StyleChawla, J. K., Bernard, A., Heussler, H., & Burgess, S. (2021). Sleep, Function, Behaviour and Cognition in a Cohort of Children with Down Syndrome. Brain Sciences, 11(10), 1317. https://doi.org/10.3390/brainsci11101317






