Evaluation of Nociception Using Quantitative Pupillometry and Skin Conductance in Critically Ill Unconscious Patients: A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
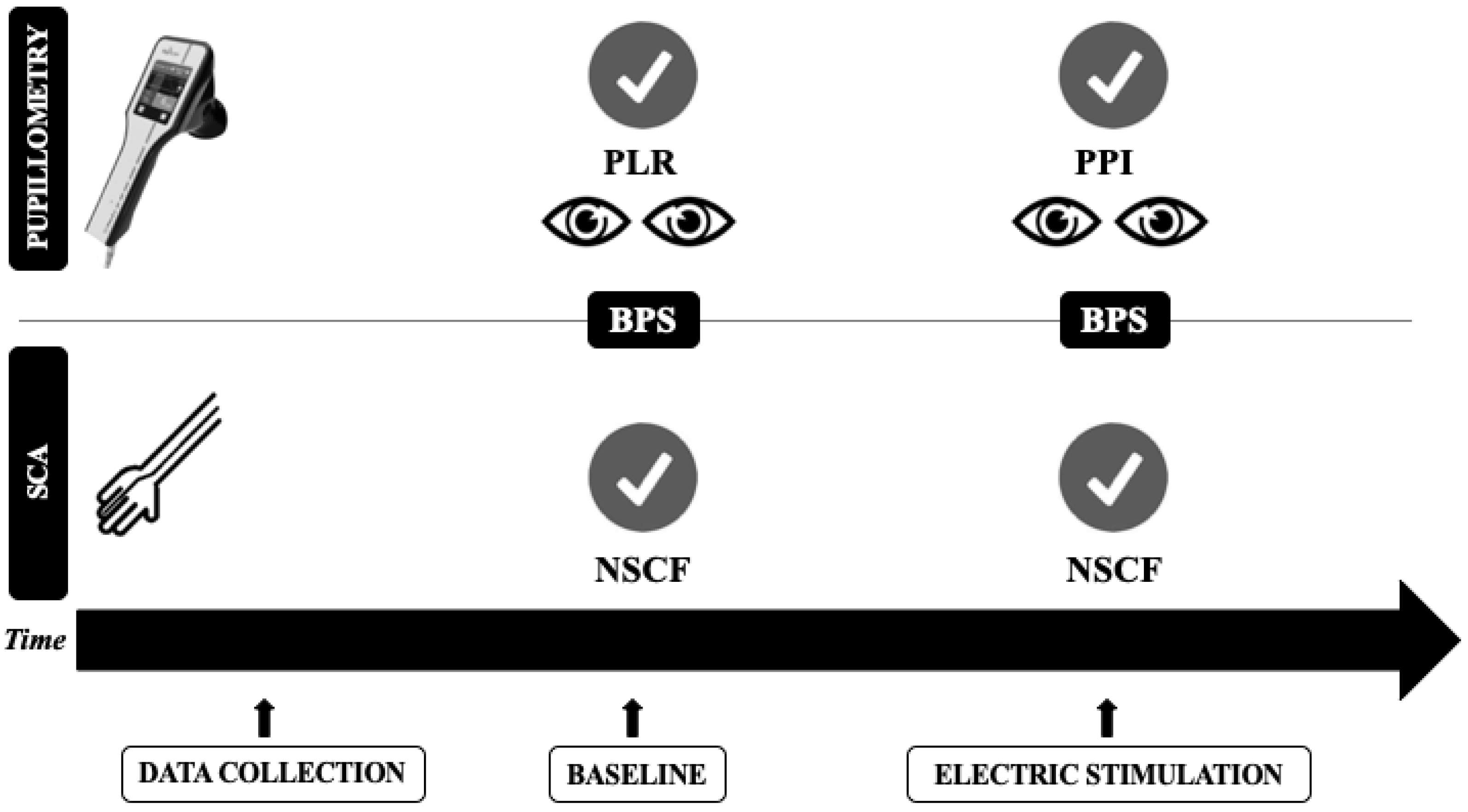
2.2. Quantitative Pupillometry
2.3. Skin Conductance Algesimeter
2.4. Data Collection
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics
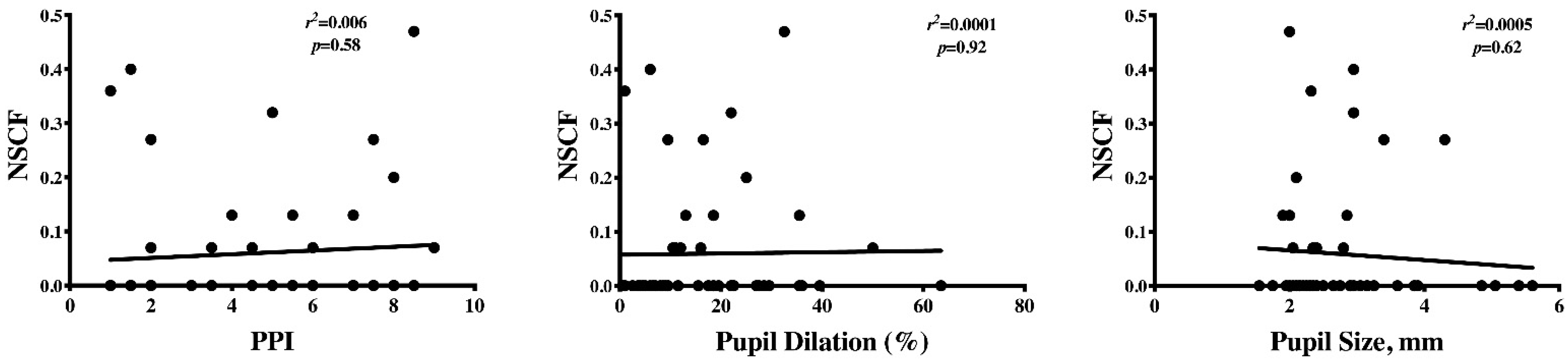
3.2. Automated Pupillometry and SCA Assessment
3.3. Subgroup Analysis of Patients with and without Brain Injury
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Devlin, J.W.; Skrobik, Y.; Gélinas, C.; Needham, D.M.; Slooter, A.J.C.; Pandharipande, P.P.; Watson, P.L.; Weinhouse, G.L.; Nunnally, M.E.; Rochwerg, B.; et al. Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU. Crit. Care Med. 2018, 46, 825–873. [Google Scholar] [CrossRef] [PubMed]
- Payen, J.F.; Bosson, J.L.; Chanques, G.; Mantz, J.; Labarere, J.; DOLOREA Investigators. Pain assessment is associated with decreased duration of mechanical ventilation in the intensive care unit: A post Hoc analysis of the DOLOREA study. Anesthesiology 2009, 111, 1308–1316. [Google Scholar] [CrossRef] [PubMed]
- Chanques, G.; Pohlman, A.; Kress, J.P.; Molinari, N.; De Jong, A.; Jaber, S.; Hall, J.B. Psychometric comparison of three behavioural scales for the assessment of pain in critically ill patients unable to self-report. Crit. Care 2014, 18, R160. [Google Scholar] [CrossRef] [PubMed]
- Payen, J.F.; Bru, O.; Bosson, J.L.; Lagrasta, A.; Novel, E.; Deschaux, I.; Lavagne, P.; Jacquot, C. Assessing pain in critically ill sedated patients by using a behavioural pain scale. Crit. Care Med. 2001, 29, 2258–2263. [Google Scholar] [CrossRef]
- Roulin, M.-J.; Ramelet, A.-S. Behavioral changes in brain-injured critical care adults with different levels of consciousness during nociceptive stimulation: An observational study. Intensive Care Med. 2014, 40, 1115–1123. [Google Scholar] [CrossRef] [PubMed]
- Arbour, C.; Choinière, M.; Topolovec-Vranic, J.; Loiselle, C.G.; Puntillo, K.; Gélinas, C. Detecting pain in traumatic brain-injured patients with different levels of consciousness during common procedures in the ICU: Typical or atypical behaviors? Clin. J. Pain 2014, 30, 960–969. [Google Scholar] [CrossRef] [PubMed]
- Broucqsault-Dédrie, C.; De Jonckheere, J.; Jeanne, M. Measurement of heart rate variability to assess pain in sedated criti-cally ill patients: A prospective observational study. PLoS ONE 2016, 11, e0147720. [Google Scholar] [CrossRef]
- Arbour, C.; Gélinas, C.; Loiselle, C.G.; Bourgault, P. An Exploratory Study of the Bilateral Bispectral Index for Pain Detection in Traumatic-Brain-Injured Patients with Altered Level of Consciousness. J. Neurosci. Nurs. 2015, 47, 166–177. [Google Scholar] [CrossRef]
- Ben-Israel, N.; Kliger, M.; Zuckerman, G.; Katz, Y.; Edry, R. Monitoring the nociception level: A multi-parameter approach. J. Clin. Monit. Comput. 2013, 27, 659–668. [Google Scholar] [CrossRef]
- Li, D.; Miaskowski, C.; Burkhardt, D. Evaluations of physiologic reactivity and reflexive behaviors during noxious pro-cedures in sedated critically ill patients. J. Crit. Care 2009, 24, 472.e9–472.e13. [Google Scholar] [CrossRef]
- Lukaszewicz, A.C.; Dereu, D.; Gayat, E.; Payen, D. The relevance of pupillometry for evaluation of analgesia before noxious proce-dures in the intensive care unit. Anesth. Analg. 2015, 120, 12971300. [Google Scholar] [CrossRef] [PubMed]
- Paulus, J.; Roquilly, A.; Beloeil, H.; Théraud, J.; Asehnoune, K.; Lejus-Bourdeau, C. Pupillary reflex measurement predicts insufficient analgesia before endotracheal suctioning in critically ill patients. Crit. Care 2013, 17, R161. [Google Scholar] [CrossRef] [PubMed]
- Vinclair, M.; Shilte, C.; Roudad, F.; Lavolaine, J.; Francony, G.; Bouzat, P.; Bosson, J.; Payen, J. Using Pupillary Pain Index to Assess Nociception in Sedated Critically Ill Patients. Anesth. Analg. 2019, 129, 1540–1546. [Google Scholar] [CrossRef] [PubMed]
- Storm, H. Changes in skin conductance as a tool to monitor nociceptive stimulation and pain. Curr. Opin. Anaesthesiol. 2008, 21, 796–804. [Google Scholar] [CrossRef]
- Ledowsky, T.; Bromilow, M.; Peacdh, M.J.; Storm, H.; Hacking, R.; Schug, S.A. Monitoring of skin conductance to assess postopera-tive pain intensity. Br. J. Anaesth. 2006, 97, 862–865. [Google Scholar] [CrossRef]
- Ledowski, T.; Pascoe, E.; Ang, B.; Schmarbeck, T.; Clarke, M.; Fuller, C.; Kapoor, V. Monitoring of intra-operative nociception: Skin conductance and surgical stress index versus stress hormone plasma levels. Anaesthesia 2010, 65, 1001–1006. [Google Scholar] [CrossRef]
- Storm, H.; Myre, K.; Rostrup, M.; Stokland, O.; Lien, M.D.; Raeder, J.C. Skin conductance correlates with perioperative stress. Acta Anaesthesiol. Scand. 2002, 46, 887–895. [Google Scholar] [CrossRef]
- Storm, H.; Fremming, A.; Odegaard, S.; Martinsen, O.G.; Morkrid, L. The development of a software program for analyzing spon-taneous and externally elicited skin conductance changes in infants and adults. Clin. Neurophysiol. 2000, 111, 1889–1898. [Google Scholar] [CrossRef]
- Sessler, C.N.; Gosnell, M.S.; Grap, M.J.; Brophy, G.M.; O’Neal, P.V.; Keane, K.A.; Tesoro, E.P.; Elswick, R.K. The Richmond Agita-tion-Sedation Scale: Validity and reliability in adult intensive care unit patients. Am. J. Respir. Crit. Care Med. 2002, 166, 1338–1344. [Google Scholar] [CrossRef]
- Couret, D.; Boumaza, D.; Grisotto, C.; Triglia, T.; Pellegrini, L.; Ocquidant, P.; Bruder, N.J.; Velly, L. Reliability of standard pupillometry practice in neurocritical care: An observational, double-blinded study. Crit. Care 2016, 20, 99. [Google Scholar] [CrossRef]
- Ly-Liu, D.; Reinoso-Barbero, F. Immediate postoperative pain can also be predicted by pupillary pain index in children. Br. J. Anaesth. 2015, 114, 345–346. [Google Scholar] [CrossRef] [PubMed]
- Khanna, P.; Chandralekha, C.; Pandey, R.K.; Sharma, A. Pain assessment in the critically ill mechanically ventilated adult pa-tients: Comparison between skin conductance algesimeter index and physiologic indicators. Saudi J. Anaesth. 2018, 12, 204–208. [Google Scholar] [PubMed]
- Günther, A.C.; Bottai, M.; Schandl, A.; Storm, H.; Rossi, P.; Sackey, P.V. Palmar skin conductance variability and the relation to stimulation, pain and the motor activity assessment scale in intensive care unit patients. Crit. Care 2013, 17, R51. [Google Scholar] [CrossRef] [PubMed]
- Kieser, M.; Wassmer, G. On the use of the upper confidence limit for the variance from a pilot sample for sample size determi-nation. Biom. J. 1996, 8, 941–949. [Google Scholar] [CrossRef]
- Gélinas, C.; Fillion, L.; Puntillo, K.A.; Viens, C.; Fortier, M. Validation of the critical-care pain observation tool in adult patients. Am. J. Crit. Care 2006, 15, 420–427. [Google Scholar] [CrossRef] [PubMed]
- Larson, M.D.; Sessler, D.I.; Washington, D.E.; Merrifield, B.R.; Hynson, J.A.; McGuire, J. Pupillary Response to Noxious Stimulation During Isoflurane and Propofol Anesthesia. Anesth. Analg. 1993, 76, 1072–1078. [Google Scholar] [CrossRef] [PubMed]
- Barvais, L.; Engelman, E.; Eba, J.; Coussaert, E.; Cantraine, F.; Kenny, G. Effect site concentrations of remifentanil and pupil response to noxious stimulation. Br. J. Anaesth. 2003, 91, 347–352. [Google Scholar] [CrossRef]
- Charier, D.; Vogler, M.C.; Zantour, D.; Pichot, V.; Martins-Baltar, A.; Courbon, M.; Roche, F.; Vassal, F.; Molliex, S. Assessing pain in the postoperative period: Analgesia Nociception IndexTM versus pupillometry. Br. J. Anaesth. 2019, 123, e322–e327. [Google Scholar] [CrossRef]
- Ploghaus, A.; Narain, C.; Beckmann, C.F.; Clare, S.; Bantick, S.; Wise, R.; Matthews, P.M.; Rawlins, J.N.P.; Tracey, I. Exacerbation of pain by anxiety is associated with activity in a hippocampal net-work. J. Neurosci. 2001, 21, 9896–9903. [Google Scholar] [CrossRef]
- Aslanidis, T.; Grosomanidis, V.; Karakoulas, K.; Chatzisotiriou, A. Electrodermal Activity Monitoring during Endotracheal Suction in Sedated Adult Intensive Care Unit Patients. Folia Medica 2018, 60, 92–101. [Google Scholar] [CrossRef]
- Szabadi, E. Modulation of physiological reflexes by pain: Role of the locus coeruleus. Front. Integr. Neurosci. 2012, 6, 94. [Google Scholar] [CrossRef] [PubMed]

| ALL (n = 51) | NEURO (n = 32) | NON-NEURO (n = 19) | |
|---|---|---|---|
| Age, years | 60 (49–70) | 58 (48–70) | 61 (50–70) |
| Male, n (%) | 39 (76) | 19 (59) | 13 (68) |
| ICU admission to test, days | 2 (1–4) | 2 (1–4) | 2 (1–6) |
| COMORBID DISEASES | |||
| COPD/asthma, n (%) | 9 (18) | 5(16) | 4 (21) |
| Heart failure, n (%) | 11 (22) | 5 (16) | 6 (32) |
| Hypertension, n (%) | 27 (53) | 15 (47) | 12 (63) |
| Diabetes, n (%) | 9 (18) | 8 (25) | 1 (5) |
| Immunosuppression, n (%) | 4 (8) | 1 (3) | 3 (16) |
| Liver cirrhosis, n (%) | 3 (6) | 1 (3) | 2 (10) |
| Chronic renal failure, n (%) | 9 (18) | 5 (16) | 4 (21) |
| SOFA score on admission | 9 (8–12) | 9 (8–11) | 11 (8–13) |
| LIFE-SUPPORT THERAPIES | |||
| CRRT, n (%) | 8 (16) | 3 (9) | 5 (26) |
| ECMO, n (%) | 4 (8) | 0 (0) | 4 (21) * |
| DRUGS | |||
| Opioids, n (%) | 39 (76) | 24 (75) | 15 (78) |
| Sedatives, n (%) | 38 (75) | 19 (59) | 19 (100) * |
| NMBAs, n (%) | 15 (29) | 9 (28) | 6 (32) |
| Vasopressors, n (%) | 34 (67) | 18 (56) | 16 (84) |
| Inotropic agents, n (%) | 5 (10) | 1 (3) | 4 (21) |
| OUTCOME | |||
| ICU mortality, n (%) | 19 (37) | 14 (44) | 5 (26) |
| ALL (n = 51) | NEURO (n= 32) | NON-NEURO (n = 19) | |
|---|---|---|---|
| VITAL PARAMETERS | |||
| MAP, mmHg | 83 (71–99) | 92 (72–106) | 73 (69–83) * |
| Heart rate, bpm | 81 (71–99) | 79 (72–98) | 84 (68–101) |
| Respiratory rate, bpm | 22 (15–30) | 21 (13–30) | 24 (19–30) |
| Arterial saturation, % | 98 (96–100) | 99 (96–100) | 96 (95–99) * |
| Temperature, °C | 36.8 (36–37.2) | 36.9 (35.0–37.3) | 36.8 (36.3–37.2) |
| GCS | 3 (3–3) | 3 (3–3) | 3 (3–3) |
| BASELINE NOCICEPTION PARAMETERS | |||
| Pupillometry Values | |||
| Size, mm | 2.7 (2.2–3.2) | 2.7 (2.3–3.3) | 2.5 (2.1–2.9) |
| Constriction rate, % | 20 (13–25) | 19 (11–24) | 23 (15–33) * |
| Constriction velocity, mm/s | 1.26 (0.98–2.19) | 1.11 (0.71–2) | 1.66 (1.20–2.49) * |
| Anisocoria | 3 (6) | 3 (9) | 0 (0) |
| Algesimeter Values | |||
| Area huge peak, | 0 (0–0) | 0 (0–0) | 0 (0–0) |
| Peak/sec (NSCF) | 0 (0–0) | 0 (0–0) | 0 (0–0) |
| Average rise, μSs | 0 (0–0) | 0 (0–0) | 0 (0–0) |
| Average peak, μSs | 0 (0–0) | 0 (0–0) | 0 (0–0) |
| Pre-Stimulation Values | Post-Stimulation Values | |
|---|---|---|
| Area huge peak, | 0 (0–0) | 0.30 (0–1.12) * |
| Peak/sec (NSCF) | 0 (0–0) | 0.13 (0.07–0.27) * |
| Average rise, μSs | 0 (0–0) | 0.01 (0–0.01) * |
| Average peak, μSs | 0 (0–0) | 0.02 (0.01–0.06) * |
| PPI ≤ 4 (Adequate Control) | PPI > 4 (Inadequate Control) | |
|---|---|---|
| NSCF < 0.07 (No Pain Detection) | 17 | 19 |
| NSCF ≥ 0.07 (Pain Detection) | 6 | 9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fratino, S.; Peluso, L.; Talamonti, M.; Menozzi, M.; Costa Hirai, L.A.; Lobo, F.A.; Prezioso, C.; Creteur, J.; Payen, J.-F.; Taccone, F.S. Evaluation of Nociception Using Quantitative Pupillometry and Skin Conductance in Critically Ill Unconscious Patients: A Pilot Study. Brain Sci. 2021, 11, 109. https://doi.org/10.3390/brainsci11010109
Fratino S, Peluso L, Talamonti M, Menozzi M, Costa Hirai LA, Lobo FA, Prezioso C, Creteur J, Payen J-F, Taccone FS. Evaluation of Nociception Using Quantitative Pupillometry and Skin Conductance in Critically Ill Unconscious Patients: A Pilot Study. Brain Sciences. 2021; 11(1):109. https://doi.org/10.3390/brainsci11010109
Chicago/Turabian StyleFratino, Sara, Lorenzo Peluso, Marta Talamonti, Marco Menozzi, Lucas Akira Costa Hirai, Francisco A Lobo, Chiara Prezioso, Jacques Creteur, Jean-François Payen, and Fabio Silvio Taccone. 2021. "Evaluation of Nociception Using Quantitative Pupillometry and Skin Conductance in Critically Ill Unconscious Patients: A Pilot Study" Brain Sciences 11, no. 1: 109. https://doi.org/10.3390/brainsci11010109
APA StyleFratino, S., Peluso, L., Talamonti, M., Menozzi, M., Costa Hirai, L. A., Lobo, F. A., Prezioso, C., Creteur, J., Payen, J.-F., & Taccone, F. S. (2021). Evaluation of Nociception Using Quantitative Pupillometry and Skin Conductance in Critically Ill Unconscious Patients: A Pilot Study. Brain Sciences, 11(1), 109. https://doi.org/10.3390/brainsci11010109







