Effectiveness of Dry Needling versus Placebo on Gait Performance, Spasticity, Electromyographic Activity, Pain, Range-of-Movement and Quality of Life in Patients with Multiple Sclerosis: A Randomized Controlled Trial Protocol
Abstract
1. Introduction
2. Materials and Methods
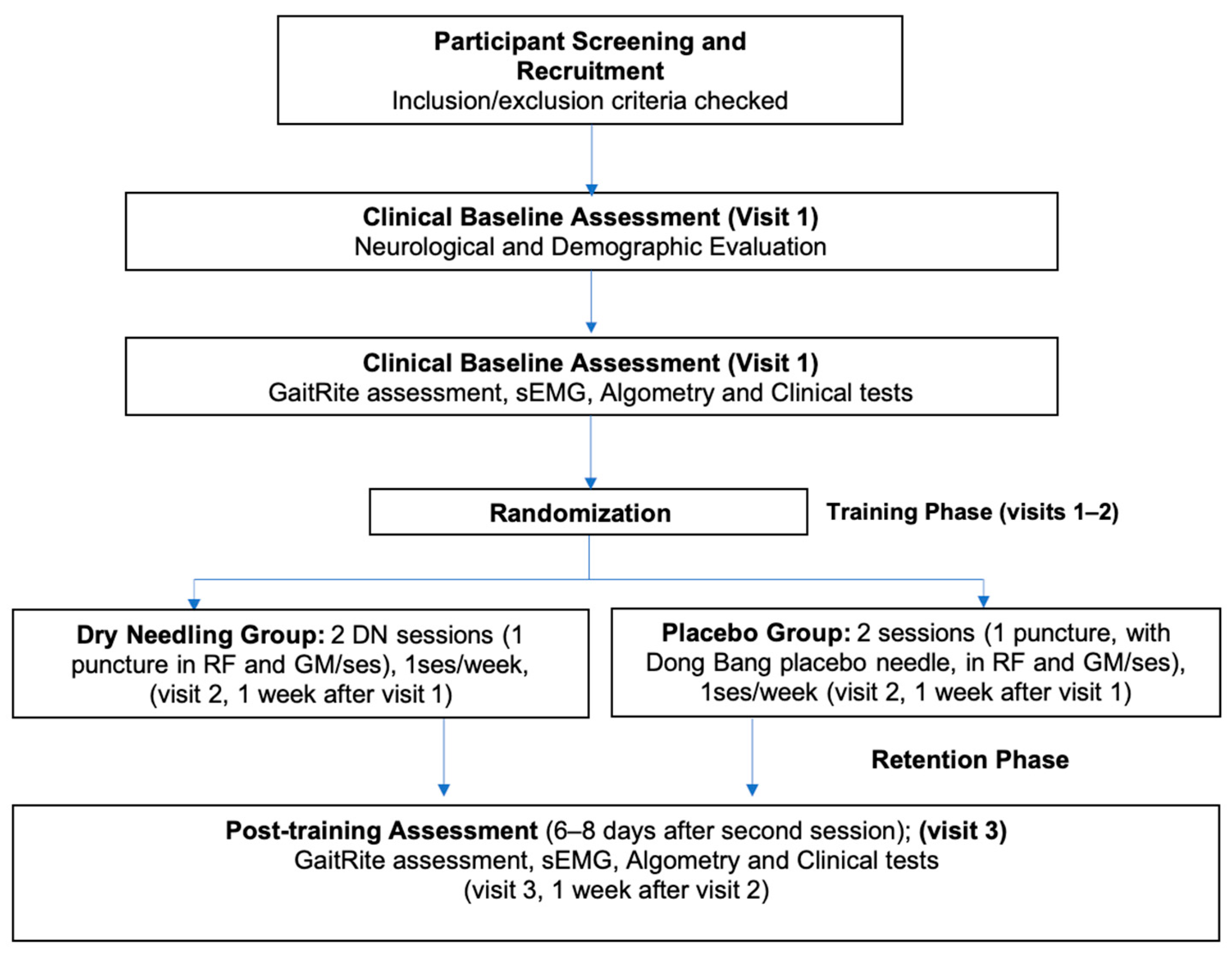
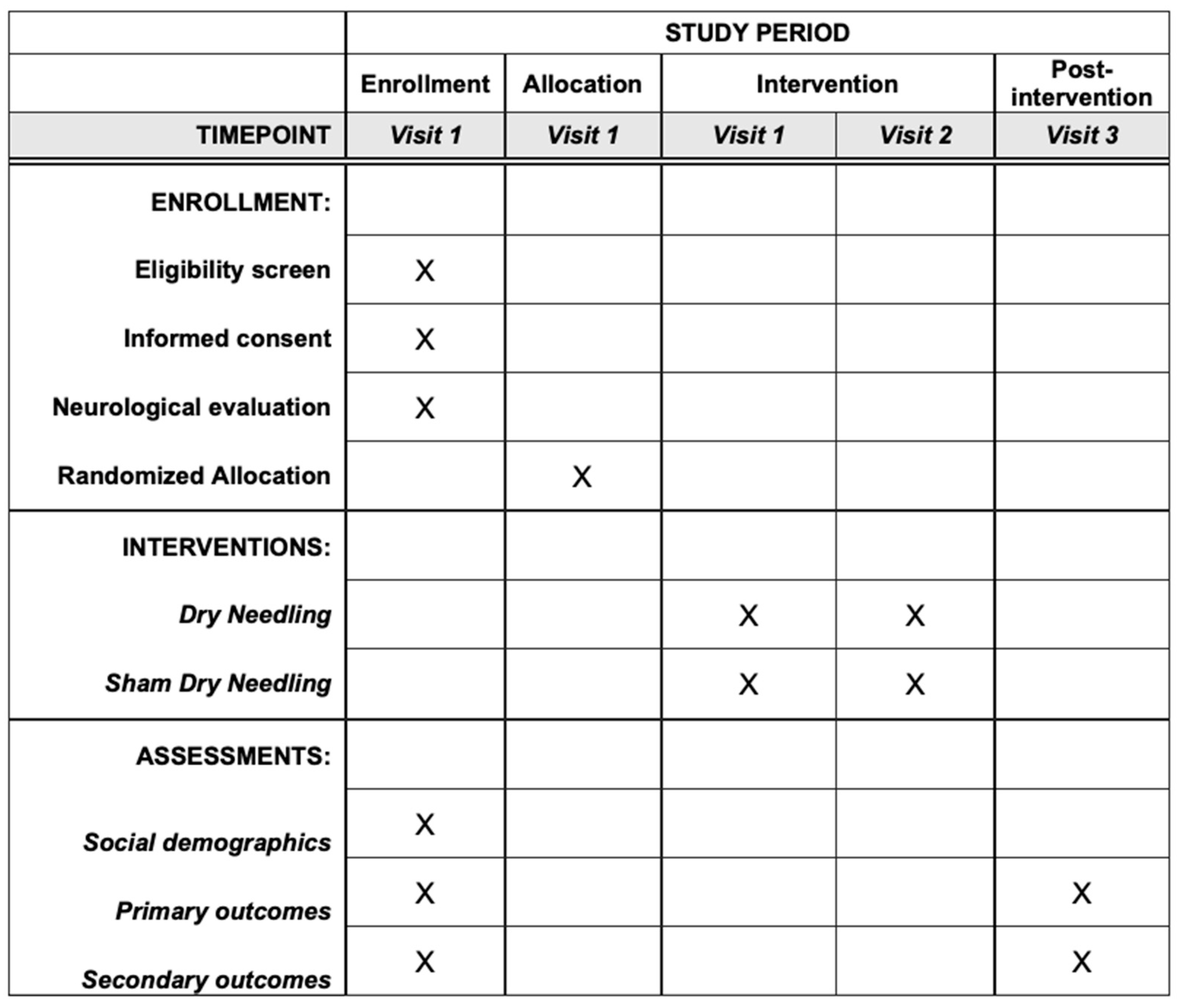
2.1. Study Design
2.2. Setting and Eligibility Criteria
2.3. Procedure
2.4. Interventions
2.5. Outcomes
2.5.1. Gait Performance
2.5.2. Spasticity
2.5.3. Electromyographic Activity
2.5.4. Pain
2.5.5. Range of Movement
2.5.6. Quality of Life
2.6. Recruitment, Allocation, and Blinding
2.7. Data Collection and Management
2.8. Statistical Methods
2.8.1. Sample Size
2.8.2. Data Analysis
2.8.3. Oversight and Monitoring
3. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Browne, P.; Chandraratna, D.; Angood, C.; Tremlett, H.; Baker, C.; Taylor, B.V.; Thompson, A.J. Atlas of Multiple Sclerosis 2013: A growing global problem with widespread inequity. Neurology 2014, 83, 1022–1024. [Google Scholar] [CrossRef]
- Dunn, S.E.; Steinman, L. The gender gap in multiple sclerosis: Intersection of science and society. JAMA Neurol. 2013, 70, 634–635. [Google Scholar] [CrossRef]
- Degenhardt, A.; Ramagopalan, S.V.; Scalfari, A.; Ebers, G.C. Clinical prognostic factors in multiple sclerosis: A natural history review. Nat. Rev. Neurol. 2009, 5, 672–682. [Google Scholar] [CrossRef]
- Comber, L.; Galvin, R.; Coote, S. Gait deficits in people with multiple sclerosis: A systematic review and meta-analysis. Gait Posture 2017, 51, 25–35. [Google Scholar] [CrossRef] [PubMed]
- Tajali, S.; Shaterzadeh-Yazdi, M.J.; Negahban, H.; van Dieën, J.H.; Mehravar, M.; Majdinasab, N.; Saki-Malehi, A.; Mofateh, R. Predicting falls among patients with multiple sclerosis: Comparison of patient-reported outcomes and performance-based measures of lower extremity functions. Mult. Scler. Relat. Disord. 2017, 17, 69–74. [Google Scholar] [CrossRef]
- Brandstadter, R.; Ayeni, O.; Krieger, S.C.; Harel, N.Y.; Escalon, M.X.; Katz Sand, I.; Leavitt, V.M.; Fabian, M.T.; Buyukturkoglu, K.; Klineova, S.; et al. Detection of subtle gait disturbance and future fall risk in early multiple sclerosis. Neurology 2020, 94, e1395–e1406. [Google Scholar] [CrossRef] [PubMed]
- Ferraro, D.; Plantone, D.; Morselli, F.; Dallari, G.; Simone, A.M.; Vitetta, F.; Sola, P.; Primiano, G.; Nociti, V.; Pardini, M.; et al. Systematic assessment and characterization of chronic pain in multiple sclerosis patients. Neurol. Sci. 2018, 39, 445–453. [Google Scholar] [CrossRef]
- Givon, U.; Zeilig, G.; Achiron, A. Gait analysis in multiple sclerosis: Characterization of temporal-spatial parameters using GAITRite functional ambulation system. Gait Posture 2009, 29, 138–142. [Google Scholar] [CrossRef] [PubMed]
- Pau, M.; Coghe, G.; Corona, F.; Marrosu, M.G.; Cocco, E. Effect of spasticity on kinematics of gait and muscular activation in people with Multiple Sclerosis. J. Neurol. Sci. 2015, 358, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Eken, M.M.; Richards, R.; Beckerman, H.; van der Krogt, M.; Gerrits, K.; Rietberg, M.; de Groot, V.; Heine, M. Quantifying muscle fatigue during walking in people with multiple sclerosis. Clin. Biomech. 2020, 72, 94–101. [Google Scholar] [CrossRef]
- Manfredini, F.; Straudi, S.; Lamberti, N.; Patergnani, S.; Tisato, V.; Secchiero, P.; Bernardi, F.; Ziliotto, N.; Marchetti, G.; Basaglia, N.; et al. Rehabilitation Improves Mitochondrial Energetics in Progressive Multiple Sclerosis: The Significant Role of Robot-Assisted Gait Training and of the Personalized Intensity. Diagnostics 2020, 10, 834. [Google Scholar] [CrossRef] [PubMed]
- Vanbellingen, T.; Kamm, C.P. Neurorehabilitation Topics in Patients with Multiple Sclerosis: From Outcome Measurements to Rehabilitation Interventions. Semin. Neurol. 2016, 36, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Martinková, P.; Freeman, J.; Drabinová, A.; Erosheva, E.; Cattaneo, D.; Jonsdottir, J.; Baert, I.; Smedal, T.; Romberg, A.; Feys, P.; et al. Physiotherapeutic interventions in multiple sclerosis across Europe: Regions and other factors that matter. Mult. Scler. Relat. Disord. 2018. [Google Scholar] [CrossRef] [PubMed]
- Khan, F.; Amatya, B.; Bensmail, D.; Yelnik, A. Non-pharmacological interventions for spasticity in adults: An overview of systematic reviews. Ann. Phys. Rehabil. Med. 2019, 62, 265–273. [Google Scholar] [CrossRef]
- Amatya, B.; Young, J.; Khan, F. Non-pharmacological interventions for chronic pain in multiple sclerosis. Cochrane Database Syst. Rev. 2018, 12, CD012622. [Google Scholar] [CrossRef]
- Jawahar, R.; Oh, U.; Yang, S.; Lapane, K.L. A systematic review of pharmacological pain management in multiple sclerosis. Drugs 2013, 73, 1711–1722. [Google Scholar] [CrossRef]
- Rieckmann, P.; Centonze, D.; Elovaara, I.; Giovannoni, G.; Havrdová, E.; Kesselring, J.; Kobelt, G.; Langdon, D.; Morrow, S.A.; Oreja-Guevara, C.; et al. Unmet needs, burden of treatment, and patient engagement in multiple sclerosis: A combined perspective from the MS in the 21st Century Steering Group. Mult. Scler. Relat. Disord. 2018, 19, 153–160. [Google Scholar] [CrossRef]
- Řasová, K.; Freeman, J.; Cattaneo, D.; Jonsdottir, J.; Baert, I.; Smedal, T.; Romberg, A.; Feys, P.; Alves-Guerreiro, J.; Habek, M.; et al. Content and Delivery of Physical Therapy in Multiple Sclerosis across Europe: A Survey. Int. J. Environ. Res. Public Health 2020, 17, 886. [Google Scholar] [CrossRef]
- Espejo-Antúnez, L.; Tejeda, J.F.-H.; Albornoz-Cabello, M.; Rodríguez-Mansilla, J.; de la Cruz-Torres, B.; Ribeiro, F.; Silva, A.G. Dry needling in the management of myofascial trigger points: A systematic review of randomized controlled trials. Complement. Ther. Med. 2017, 33, 46–57. [Google Scholar] [CrossRef]
- Gattie, E.; Cleland, J.A.; Snodgrass, S. The Effectiveness of Trigger Point Dry Needling for Musculoskeletal Conditions by Physical Therapists: A Systematic Review and Meta-analysis. J. Orthop. Sports Phys. Ther. 2017, 47, 133–149. [Google Scholar] [CrossRef]
- Salom-Moreno, J.; Sánchez-Mila, Z.; Ortega-Santiago, R.; Palacios-Ceña, M.; Truyol-Domínguez, S.; Fernández-de-las-Peñas, C. Changes in spasticity, widespread pressure pain sensitivity, and baropodometry after the application of dry needling in patients who have had a stroke: A randomized controlled trial. J. Manip. Physiol. Ther. 2014, 37, 569–579. [Google Scholar] [CrossRef] [PubMed]
- Mendigutia-Gómez, A.; Martín-Hernández, C.; Salom-Moreno, J.; Fernández-de-las-Peñas, C. Effect of Dry Needling on Spasticity, Shoulder Range of Motion, and Pressure Pain Sensitivity in Patients With Stroke: A Crossover Study. J. Manip. Physiol. Ther. 2016, 39, 348–358. [Google Scholar] [CrossRef] [PubMed]
- Valencia-Chulián, R.; Heredia-Rizo, A.M.; Moral-Munoz, J.A.; Lucena-Anton, D.; Luque-Moreno, C. Dry needling for the management of spasticity, pain, and range of movement in adults after stroke: A systematic review. Complement. Ther. Med. 2020, 52, 102515. [Google Scholar] [CrossRef] [PubMed]
- Boyce, D.; Wempe, H.; Campbell, C.; Fuehne, S.; Zylstra, E.; Smith, G.; Wingard, C.; Jones, R. Adverse Events Associated With Therapeutic Dry Needling. Int. J. Sports Phys. Ther. 2020, 15, 103–113. [Google Scholar] [CrossRef]
- Ghannadi, S.; Shariat, A.; Ansari, N.N.; Tavakol, Z.; Honarpishe, R.; Dommerholt, J.; Noormohammadpour, P.; Ingle, L. The Effect of Dry Needling on Lower Limb Dysfunction in Poststroke Survivors. J. Stroke Cerebrovasc. Dis. 2020, 29, 104814. [Google Scholar] [CrossRef]
- Blasini, M.; Peiris, N.; Wright, T.; Colloca, L. The Role of Patient-Practitioner Relationships in Placebo and Nocebo Phenomena. Int. Rev. Neurobiol. 2018, 139, 211–231. [Google Scholar] [CrossRef]
- Quispe-Cabanillas, J.G.; Damasceno, A.; von Glehn, F.; Brandão, C.O.; Damasceno, B.P.; Silveira, W.D.; Santos, L.M.B. Impact of electroacupuncture on quality of life for patients with Relapsing-Remitting Multiple Sclerosis under treatment with immunomodulators: A randomized study. BMC Complement. Altern. Med. 2012, 12, 209. [Google Scholar] [CrossRef]
- Charles, D.; Hudgins, T.; MacNaughton, J.; Newman, E.; Tan, J.; Wigger, M. A systematic review of manual therapy techniques, dry cupping and dry needling in the reduction of myofascial pain and myofascial trigger points. J. Bodyw. Mov. Ther. 2019, 23, 539–546. [Google Scholar] [CrossRef]
- Luque-Moreno, C.; Granja-Domínguez, A.; Heredia-Rizo, A.M.; Lucena-Anton, D.; Galán-Mercant, A.; Moral-Munoz, J.A. Multiple sclerosis treatment: Dry needling, new therapeutic frontiers. J. Adv. Health Care 2020, 2, 1–5. [Google Scholar] [CrossRef]
- Cagnie, B.; Dewitte, V.; Barbe, T.; Timmermans, F.; Delrue, N.; Meeus, M. Physiologic effects of dry needling topical collection on myofascial pain. Curr. Pain Headache Rep. 2013, 17, 348. [Google Scholar] [CrossRef]
- Castro Sánchez, A.M.; García López, H.; Fernández Sánchez, M.; Pérez Mármol, J.M.; Aguilar-Ferrándiz, M.E.; Luque Suárez, A.; Matarán Peñarrocha, G.A. Improvement in clinical outcomes after dry needling versus myofascial release on pain pressure thresholds, quality of life, fatigue, pain intensity, quality of sleep, anxiety, and depression in patients with fibromyalgia syndrome. Disabil. Rehabil. 2019, 41, 2235–2246. [Google Scholar] [CrossRef] [PubMed]
- Sarmiento-Hernández, I.; Pérez-Marín, M.D.L.Á.; Nunez-Nagy, S.; Pecos-Martín, D.; Gallego-Izquierdo, T.; Sosa-Reina, M.D. Effectiveness of Invasive Techniques in Patients with Fibromyalgia: Systematic Review and Meta-Analysis. Pain Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.W.; Tetzlaff, J.M.; Gøtzsche, P.C.; Altman, D.G.; Mann, H.; Berlin, J.A.; Dickersin, K.; Hróbjartsson, A.; Schulz, K.F.; Parulekar, W.R.; et al. SPIRIT 2013 explanation and elaboration: Guidance for protocols of clinical trials. BMJ 2013, 346, e7586. [Google Scholar] [CrossRef] [PubMed]
- Polman, C.H.; Reingold, S.C.; Banwell, B.; Clanet, M.; Cohen, J.A.; Filippi, M.; Fujihara, K.; Havrdova, E.; Hutchinson, M.; Kappos, L.; et al. Diagnostic criteria for multiple sclerosis: 2010 Revisions to the McDonald criteria. Ann. Neurol. 2011, 69, 292–302. [Google Scholar] [CrossRef] [PubMed]
- Kurtzke, J.F. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology 1983, 33, 1444–1452. [Google Scholar] [CrossRef] [PubMed]
- Tang, L.; Yan, L.; Qiang-Min, H.; Yang, Y. Dry needling at myofascial trigger points mitigates chronic post-stroke shoulder spasticity. Neural Regen. Res. 2018, 13, 673–676. [Google Scholar] [CrossRef]
- Streitberger, K.; Kleinhenz, J. Introducing a placebo needle into acupuncture research. Lancet 1998, 352, 364–365. [Google Scholar] [CrossRef]
- Řasová, K.; Martinková, P.; Soler, B.; Freeman, J.; Cattaneo, D.; Jonsdottir, J.; Smedal, T.; Romberg, A.; Henze, T.; Santoyo-Medina, C.; et al. Real-world goal setting and use of outcome measures according to the international classification of functioning, disability and health: A european survey of physical therapy practice in multiple sclerosis. Int. J. Environ. Res. Public Health 2020, 17, 4774. [Google Scholar] [CrossRef]
- Hochsprung, A.; Heredia-Camacho, B.; Castillo, M.; Izquierdo, G.; Escudero-Uribe, S. Clinical validity of the quantitative gait variables in patients with multiple sclerosis. A comparison of the Timed 25-foot Walk Test and the GAITRite (R) Electronic Walkway system. Rev. Neurol. 2014, 59, 8–12. [Google Scholar]
- Ares-Benítez, I.; Luque-Moreno, C.; Alonso-Enríquez, L.; Moral-Munoz, J.A.; Lucena-Anton, D.; Izquierdo-Ayuso, G.; Granja-Domínguez, A. Physical therapy and Spanish dance in the reeducation of gait disturbances in multiple sclerosis: A case report. Rev. Cient. Soc. Esp. Enferm. Neurol. 2020. [Google Scholar] [CrossRef]
- Gijbels, D.; Eijnde, B.O.; Feys, P. Comparison of the 2- and 6-minute walk test in multiple sclerosis. Mult. Scler. J. 2011, 17, 1269–1272. [Google Scholar] [CrossRef] [PubMed]
- Ghotbi, N.; Nakhostin Ansari, N.; Naghdi, S.; Hasson, S. Measurement of lower-limb muscle spasticity: Intrarater reliability of Modified Modified Ashworth Scale. J. Rehabil. Res. Dev. 2011, 48, 83–88. [Google Scholar] [CrossRef]
- Banos, O.; Moral-Munoz, J.A.; Diaz-Reyes, I.; Arroyo-Morales, M.; Damas, M.; Herrera-Viedma, E.; Hong, C.S.; Lee, S.; Pomares, H.; Rojas, I.; et al. MDurance: A novel mobile health system to support trunk endurance assessment. Sensors 2015, 15, 13159–13183. [Google Scholar] [CrossRef] [PubMed]
- Molina-Molina, A.; Ruiz-Malagón, E.J.; Carrillo-Pérez, F.; Roche-Seruendo, L.E.; Damas, M.; Banos, O.; García-Pinillos, F. Validation of mDurance, A Wearable Surface Electromyography System for Muscle Activity Assessment. Front. Physiol. 2020, 11, 606287. [Google Scholar] [CrossRef]
- Hermens, H.; Freriks, B.; Disselhorst-Klug, C.; Rau, G. Development of recommendations for SEMG sensors and sensor placement procedures. J. Electromyogr. Kinesiol. 2000, 10, 361–374. [Google Scholar] [CrossRef]
- Beretta-Piccoli, M.; Cescon, C.; Barbero, M.; Villiger, M.; Clijsen, R.; Kool, J.; Kesselring, J.; Bansi, J. Upper and lower limb performance fatigability in people with multiple sclerosis investigated through surface electromyography: A pilot study. Physiol. Meas. 2020, 41, 025002. [Google Scholar] [CrossRef]
- Fernández-de-Las-Peñas, C.; Ortega-Santiago, R.; Ortíz-Gutiérrez, R.; Caminero, A.B.; Salom-Moreno, J.; Arendt-Nielsen, L. Widespread pressure pain hypersensitivity in patients with multiple sclerosis with and without pain as sign of central sensitization. Clin. J. Pain 2015, 31, 66–72. [Google Scholar] [CrossRef]
- Fernández, O.; Fernández, V.; Baumstarck-Barrau, K.; Muñoz, L.; Gonzalez Alvarez, M.d.M.; Arrabal, J.C.; León, A.; Alonso, A.; López-Madrona, J.C.; Bustamante, R.; et al. Validation of the spanish version of the Multiple Sclerosis International Quality of Life (Musiqol) questionnaire. BMC Neurol. 2011, 11, 127. [Google Scholar] [CrossRef]
- Apti, A.; Akalan, N.E.; Kuchimov, S.; Özdinçler, A.R.; Temelli, Y.; Nene, A. Plantar flexor muscle weakness may cause stiff-knee gait. Gait Posture 2016, 46, 201–207. [Google Scholar] [CrossRef]
- Lencioni, T.; Jonsdottir, J.; Cattaneo, D.; Crippa, A.; Gervasoni, E.; Rovaris, M.; Bizzi, E.; Ferrarin, M. Are Modular Activations Altered in Lower Limb Muscles of Persons with Multiple Sclerosis during Walking? Evidence from Muscle Synergies and Biomechanical Analysis. Front. Hum. Neurosci. 2016, 10, 620. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luque-Moreno, C.; Granja-Domínguez, A.; Moral-Munoz, J.A.; Izquierdo-Ayuso, G.; Lucena-Anton, D.; Heredia-Rizo, A.M. Effectiveness of Dry Needling versus Placebo on Gait Performance, Spasticity, Electromyographic Activity, Pain, Range-of-Movement and Quality of Life in Patients with Multiple Sclerosis: A Randomized Controlled Trial Protocol. Brain Sci. 2020, 10, 997. https://doi.org/10.3390/brainsci10120997
Luque-Moreno C, Granja-Domínguez A, Moral-Munoz JA, Izquierdo-Ayuso G, Lucena-Anton D, Heredia-Rizo AM. Effectiveness of Dry Needling versus Placebo on Gait Performance, Spasticity, Electromyographic Activity, Pain, Range-of-Movement and Quality of Life in Patients with Multiple Sclerosis: A Randomized Controlled Trial Protocol. Brain Sciences. 2020; 10(12):997. https://doi.org/10.3390/brainsci10120997
Chicago/Turabian StyleLuque-Moreno, Carlos, Anabel Granja-Domínguez, Jose A. Moral-Munoz, Guillermo Izquierdo-Ayuso, David Lucena-Anton, and Alberto Marcos Heredia-Rizo. 2020. "Effectiveness of Dry Needling versus Placebo on Gait Performance, Spasticity, Electromyographic Activity, Pain, Range-of-Movement and Quality of Life in Patients with Multiple Sclerosis: A Randomized Controlled Trial Protocol" Brain Sciences 10, no. 12: 997. https://doi.org/10.3390/brainsci10120997
APA StyleLuque-Moreno, C., Granja-Domínguez, A., Moral-Munoz, J. A., Izquierdo-Ayuso, G., Lucena-Anton, D., & Heredia-Rizo, A. M. (2020). Effectiveness of Dry Needling versus Placebo on Gait Performance, Spasticity, Electromyographic Activity, Pain, Range-of-Movement and Quality of Life in Patients with Multiple Sclerosis: A Randomized Controlled Trial Protocol. Brain Sciences, 10(12), 997. https://doi.org/10.3390/brainsci10120997







