Abstract
Study Objective: Tinnitus is a common disorder characterized by sound in the ear in the absence of external or internal stimuli. Low-level laser therapy (LLLT) was discovered enhancing tissue repair via increasing the blood microcirculation and cell proliferation in 1960s. In the last two decades, LLLT delivered to the cochlea has frequently been used to reduce the severity of tinnitus. However, whether LLLT effectively attenuates the severity of tinnitus remains controversial. We aimed to evaluate the efficacy of low-level laser therapy on adult patients with complaints of tinnitus. Design: Systematic review and meta-analysis with trial sequential analysis. Interventions: Low-level laser therapy (LLLT). Measurements: Tinnitus Handicap Inventory (THI) score; improvement rates of the visual analog scale (VAS), verbal rating scale (VRS) and numeric rating scale (NRS) scores. Methods: We searched PubMed, Embase, Scopus, Web of Science, and the Cochrane Library from inception through 17 September 2020. Randomized control trials that involved adult patients with complaints of tinnitus, compared LLLT to a placebo and provided sufficient information for meta-analysis were considered eligible. Main Results: Overall, 11 studies involving 670 patients were included. No significant difference in the overall effect according to the THI score (mean difference (MD), −2.85; 95% CI, −8.99 to 3.28; p = 0.362; I2 = 0%) and the rating scale score improvement rate (risk ratio (RR), 1.35; 95% CI, 0.81 to 2.27; p = 0.250; I2 = 67%) was demonstrated between patients receiving LLLT and those receiving a placebo. None of the subgroup analyses showed significant differences, regardless of underlying sensorineural hearing loss, the number of irradiation sessions or the wavelength used. Conclusions: Our meta-analysis suggests that the value of LLLT in controlling the severity of tinnitus remains unclear, in part due to the relatively small number of patients and underlying heterogeneity. More large-scale investigations of LLLT for tinnitus related to inner ear disease are required to further elucidate the therapeutic effects.
1. Introduction
Tinnitus is a common disorder characterized by sound in the ear in the absence of external or internal stimuli. Although there are numerous etiologies responsible for tinnitus, idiopathic tinnitus still accounts for most cases [1]. Persistent tinnitus can cause devastating disturbances and morbidities at the psychological and socioprofessional levels [2,3,4,5]; therefore, many attempts have been made to relieve tinnitus. However, none of the symptomatic treatments have resulted in significant and lasting improvement of tinnitus.
In contrast to high power lasers that are used to cut or destroy tissue, low-level laser therapy (LLLT) applies lasers with lower power to the surface of the body. LLLT acts by increasing blood microcirculation through sympathetic neural inhibition, prompting an increase in cell proliferation and enhancing adenosine triphosphate (ATP) synthesis in mitochondria. Together, it speeds up the repair and decreases the damage of cells and tissue [6,7,8]. However, it was not until Moon et al. [9] assessed the safety of LLLT in an animal model that a laser power of less than 200 mW could be safely administered to the tympanic membrane without adverse effects such as edema, vascular congestion and inflammation. Since the effectiveness of LLLT was shown for several conditions, including pain for rheumatoid arthritis [10], osteoarthritis [11], chronic low back pain [12], acute and chronic neck pain [13] and tendinopathy [14], LLLT has been considered a potential treatment for tinnitus in the past two decades.
However, the therapeutic efficacy of LLLT is still controversial, as only some studies have shown positive results. The differences may result from inconsistencies in several factors. First, as a higher wavelength laser would deliver a large amount of irradiance through greater penetration [15,16,17], different wavelength settings might affect the efficacy of LLLT. Second, LLLT delivered to the cochlea via the transmastoidal route is expected to be greatly absorbed by temporal bone, leading to therapeutically insufficient doses of irradiation. Trans-meatal delivery of LLLT, on the other hand, shows more irradiation penetration since a less solid structure hinders irradiation [15]. The delivery route may also influence the results of LLLT. Finally, different irradiance dose exposures could also account for the different results [17]. In addition, different types of measurements have been used in the evaluation of tinnitus severity, including self-reported questionnaires (e.g., Tinnitus Handicap Inventory (THI), Tinnitus Severity Index (TSI)) and rating scales (e.g., visual analog scale (VAS), verbal rating scale (VRS), numeric rating scale (NRS)). Measurement inconsistencies between studies further hinder authors and clinicians from making comparisons among studies.
In light of these issues, the present study aims to systematically review the current literature on LLLT. To explore the true effect of LLLT and the influence of concurrent factors, we identified randomized controlled trials (RCTs) and sought to evaluate the efficacy of LLLT in adult patients with tinnitus via meta-analysis.
2. Materials and Methods
2.1. Study Design
The present study is a meta-analysis and systematic review of randomized control trials. The primary objective of this study is to explore the effects of LLLT on patients with complaints of tinnitus. This study follows the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) statement [18]. This study is also registered in the International Prospective Register of Systematic Reviews (CRD42020209916).
2.2. Search Strategy
From their inception through 17 September 2020, databases including the Cochrane Library, PubMed, Embase, Web of Science, and Scopus were searched by two authors (C.-H. Chen and C.-Y. Chang). We used subject headings (Medical Subject Headings (MeSH) terms in the Cochrane Library and PubMed, and Emtree terms in Embase) and search field tags of title, abstract and keywords to facilitate searching. The Boolean operator “OR” was used to cover similar concepts, whereas “AND” was used to identify where different concepts intersect. We also consolidated MeSH and text words to create two subsets of citations: one including studies of lasers (“laser”, “pulsed laser”, “continuous wave laser”) and the second including studies on tinnitus (“tinnitus”, “subjective tinnitus”, “objective tinnitus”). Supplementary Table S1 shows the detailed search strategy. The identified records were screened by title, abstract, and keywords. Records with potential eligibility were then obtained and subjected to a full-text review. To identify additional studies, a manual search of the reference lists of the included studies was conducted.
2.3. Eligibility Criteria
Two reviewers (C.-H. Chen and C.-Y. Chang) selected the studies that met all of the conditions of the following criteria: (a) the study was an RCT involving patients undergoing LLLT for tinnitus; (b) the study compared LLLT with a placebo and reported an outcome of interest (i.e., THI); and (c) the study provided adequate information to calculate the effect estimates for meta-analysis. We did not exclude studies based on publication date, language, or geographical area. When there were discrepancies regarding the inclusion of a study, a third author (Y.-F. Cheng) would provide consensus or discussion.
2.4. Risk of Bias Assessment
The revised Cochrane Risk of Bias Tool 2 was used to assess the methodological quality of the included studies. Disagreements between the two reviewers were resolved through either discussion or consensus with a third reviewer (Y.-F. Cheng).
2.5. Data Extraction
Two reviewers (C.-H. Chen and C.-Y. Chang) extracted datasets from the eligible studies. The extracted information included author’s name, publication year, country, number and mean age of patients, laser type and intensity, scale used for tinnitus measurement, timing of the measurement, adverse events that had been assessed and reported, and effect estimates
2.6. Statistical Analysis
The effect estimate for the Tinnitus Handicap Inventory (THI) was the mean difference (MD) and that for the improvement rate estimated by the rating scale scores was the risk ratio (RR). The MD and 95% confidence interval (CI) were calculated directly from data reported in tables or the main text. The pooled MD and RR were calculated using the inverse variance method. Based on the assumption that ethnicity, country, underlying disease and age differences existed in the patient populations across studies, random-effects meta-analysis models with the DerSimonian–Laird estimator were selected to account for a second source of error in addition to the sampling error that is expected with a fixed-effect model. The Cochran Q statistic and the I2 statistic were used to assess statistical heterogeneity. The heterogeneity was considered low, moderate and high for an I2 of <50%, 50–74%, and ≥75%, respectively [19].
Subgroup analyses were conducted to explore the influence of underlying disorders, including sensorineural hearing loss (SNHL) and idiopathic tinnitus, the length of the irradiation session and different wavelength settings, on the pooled effect estimates, as these factors might cause differences in the effects of LLLT [1,15,16]. In the influence analysis of the THI score after intervention, the pooled point estimates after omitting each included study one at a time lay within the 95% CI of the overall pooled results. Similarly, the influence analysis of the scale score improvement rate after intervention revealed the same results.
To obtain a conclusive meta-analysis and evaluate if the obtained results could have been type I or type II errors caused by sparse data and lack of power, the diversity-adjusted required information size (RIS) and trial sequential monitoring boundaries were calculated through trial sequential analysis (TSA) [20]. The models for all outcomes were based on an alpha of 5% and a power of 80%. All statistical analyses were performed using R version 4.0.2 with the “dmetar”, “meta”, and “metafor” packages [21]. TSA software version 0.9.5.10 Beta was used to perform the TSA. Statistical results were considered significant when there was a p-value < 0.05 [22].
3. Results
3.1. Study Identification and Selection
We identified 403 records in five databases, namely, the Cochrane Library (n = 48), PubMed (n = 84), Scopus (n = 172), Embase (n = 29) and Web of Science (n = 70). After removal of 195 duplicates, we screened the remaining studies for eligibility. Based on irrelevance, 181 studies in total were excluded after reviewing the title and abstract. Twenty-seven studies entered the full-text review. Sixteen studies were then excluded due to a lack of comparison with a placebo, insufficient data for meta-analysis and unavailability of the full text. As a result, 11 studies containing 670 patients were included. Figure 1 presents the exhaustive PRISMA flow diagram.
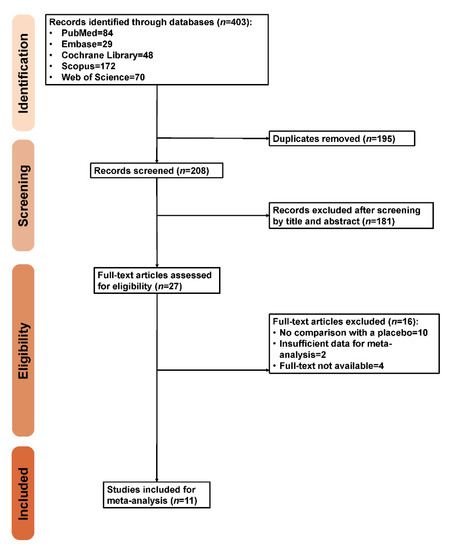
Figure 1.
Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) flow diagram.
3.2. Study Characteristics and Risk of Bias Assessment
The study characteristics are presented in Table 1. Two studies enrolled diseased ears as samples [23,24]. One study used a low laser device with an intensity of 100 mW and a wavelength of 650 nm for ten sessions [1], one used the device with an intensity of 5 mV and a wavelength of 650 nm for twenty sessions [25], one used the device with an intensity of 5 mW and a wavelength of 650 nm for twenty sessions [26], one used the device with an intensity of 5 mW and a wavelength of 650 nm for seventy sessions [27], two used the device with an intensity of 5 mW and a wavelength of 650 nm for ninety sessions [28,29], one used the device with an intensity of 5 mW and a wavelength of 650 nm for seven sessions [23], one used the device with an intensity of 67 mW and a wavelength of 830 nm for twelve sessions [30], one used the device with an intensity of 60 mW and a wavelength of 810 nm for four sessions [24], and one used the device with an intensity of 50 mW and a wavelength of 830 nm for fifteen sessions [31]. Five studies enrolled patients with SNHL [1,24,26,28,32], whereas four studies included patients with idiopathic tinnitus [25,27,30,31], and the other two studies included patients with mixed tinnitus involving hearing loss and idiopathic tinnitus [23,29]. Nine of the included studies enrolled patients with tinnitus lasting for more than 6 months [23,25,26,27,28,29,30,31,32], while one study enrolled patients with tinnitus lasting for more than three months [1] and the other one did not report the duration [24]. Ten of the included studies performed sham laser as placebo intervention [1,23,24,25,26,27,28,29,31,32], while the other one did not state the intervention in control group [30]. Five of the included studies performed laser unilaterally [1,23,25,28,31], while the other studies did not further report the treatment laterality [24,26,27,29,30,32]. Tinnitus severity and improvement were measured immediately after intervention in eight studies [1,25,26,27,28,29,31,32], while one study measured tinnitus severity two weeks after the intervention [23], and two measured tinnitus severity one week after the intervention [24,30]. The THI score was used in five studies [1,28,29,30,31], and rating scales were used to evaluate whether patients experienced improvement in the loudness of tinnitus in six studies [23,24,25,26,27,32]. Adverse event observations were reported qualitatively in four studies [1,23,24,30]. More detailed information regarding the timing of the measurements, study results, laser modalities used for the interventions, measurement scales used and reported adverse events are presented in Table 1. Moreover, Supplementary Figure S1 presents the risk of bias assessment for each included study.

Table 1.
Study characteristics.
3.3. Outcomes
3.3.1. THI Scores after LLLT
The THI scores were measured after LLLT and were reported in five studies [1,28,29,30,31] (Figure 2). Overall, the pooled THI level was lower in patients receiving low laser therapy than in those receiving a placebo, but this result did not reach statistical significance (MD, −2.85; 95% CI, −8.99 to 3.28; p = 0.362; I2 = 0%).
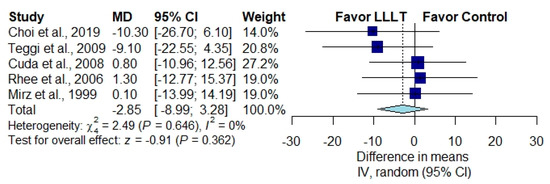
Figure 2.
Overall effect of low-level laser therapy (LLLT) as measured by the THI score [1,28,29,30,31].
3.3.2. Improvement Rate According to Rating Scale Scores
The pooled results of six studies for improvement in the loudness of tinnitus showed no significant difference in the improvement rate between patients receiving LLLT and those receiving a placebo [23,24,25,26,27,32] (Figure 3) (RR, 1.35; 95% CI, 0.81 to 2.27; p = 0.250; I2 = 67%).
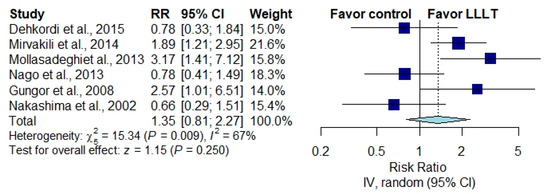
Figure 3.
Overall effect of LLLT as measured by the rating scale score improvement rate [23,24,25,26,27,32].
3.3.3. Subgroup Analysis in Patients with SNHL or Idiopathic Tinnitus
In patients with SNHL, the pooled THI score was not significantly different between the irradiation group and the placebo group in patients with SNHL [1,28] (Figure 4) (MD, −9.58; 95% CI, −19.98 to 0.82; p = 0.071; I2 = 0%) or in patients with idiopathic tinnitus [30,31] (Figure 4) (MD, −9.58; 95% CI, −19.98 to 0.82; p = 0.071; I2 = 0%). The pooled results for improvement in the loudness of tinnitus demonstrated no significant difference between patients receiving LLLT and those receiving a placebo in patients with SNHL [24,26,32] (Figure 5) (RR, 1.61; 95% CI, 0.75 to 3.47; p = 0.221; I2 = 73%) or in patients with idiopathic tinnitus [25,27] (Figure 5) (RR, 1.22; 95% CI, 0. to 2.16; p = 0.347; I2 = 71%).
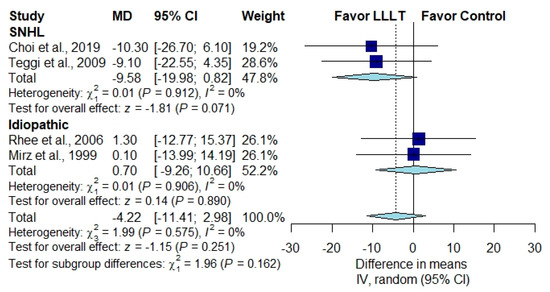
Figure 4.
Subgroup analysis of THI scores in patients with SNHL and patients with idiopathic tinnitus [1,28,30,31].
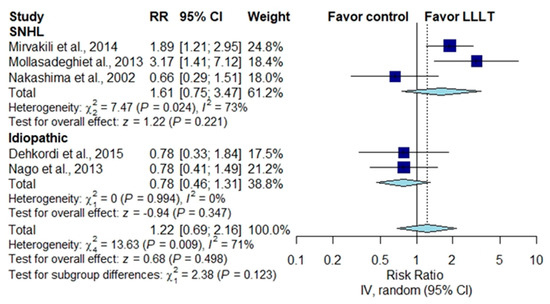
Figure 5.
Subgroup analysis of rating scale score improvement in patients with SNHL and patients with idiopathic tinnitus [23,24,25,26,31].
3.3.4. Subgroup Analysis According to the Number of Irradiation Sessions
In studies in which effect estimates were measured by THI score, two studies with more than the median number of irradiation sessions showed no significant difference between the LLLT group and the placebo group [28,29] (Figure 6) (MD, −3.59; 95% CI, −13.23 to 6.05; p = 0.465; I2 = 15%), while another three studies with fewer than the median number of sessions showed no significant difference between the two groups [1,30,31] (Figure 6) (MD, −2.26; 95% CI, −10.77 to 6.25; p = 0.362; I2 = 0%). In studies in which effect estimates were measured by the improvement rate of the rating scale scores, four studies with more than the median number of irradiation sessions revealed no significant difference between the two groups [25,26,27,32] (Figure 7) (RR, 1.40; 95% CI, 0.75 to 2.60; p = 0.294; I2 = 71%), neither did another two studies with fewer than the median number of sessions [23,24] (Figure 7) (RR, 1.28; 95% CI, 0.34 to 4.85; p = 0.718; I2 = 78%).
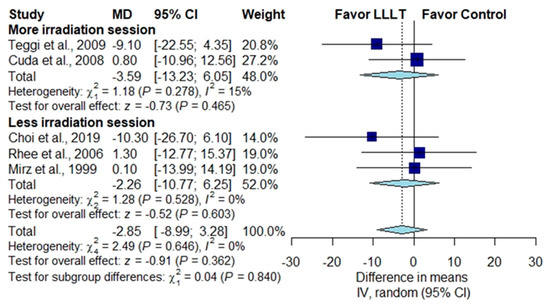
Figure 6.
Subgroup analysis of THI scores according to the number of irradiation sessions [1,28,29,30,31].
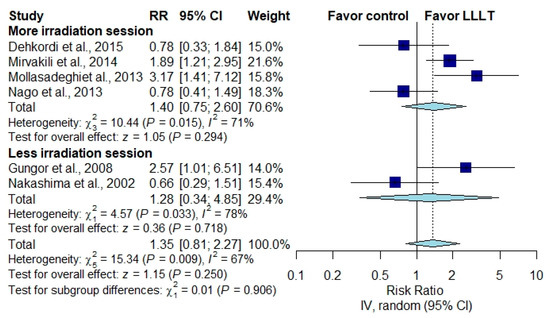
Figure 7.
Subgroup analysis of rating scale score improvement rates according to the number of irradiation sessions [23,24,25,26,29,31].
3.3.5. Subgroup Analysis According to Wavelength Setting
Three studies used a wavelength setting of 830 nm, and the pooled effect estimate demonstrated no significant difference between the LLLT group and the placebo group [1,30,31] (Figure 8) (MD, −2.26; 95% CI, −10.77 to 6.25; p = 0.362; I2 = 0%); similarly, two studies with a wavelength setting of 650 nm showed no significant difference between the two groups [28,29] (Figure 8) (MD, −3.59; 95% CI, −13.23 to 6.05; p = 0.465; I2 = 15%).
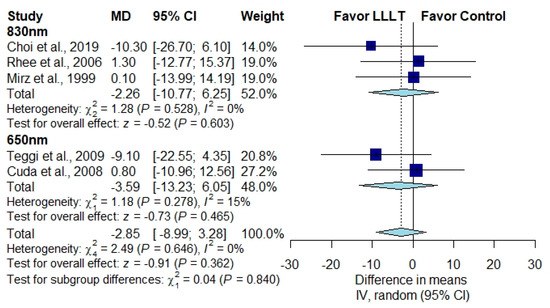
Figure 8.
Subgroup analysis according to wavelength setting [1,28,29,30,31].
3.4. Influence Analysis
In the influence analysis, the pooled point estimates after excluding every study one by one were contained within the 95% CI of the overall pooled results for these outcomes (Supplementary Figures S2 and S3).
3.5. Trial Sequential Analysis
None of the cumulative Z-curves surpassed the traditional significance boundary or the sequential monitoring boundaries for the adjusted significance threshold in favor of LLLT in the TSA of the overall effect or in the subgroup TSAs (Supplementary Figures S4–S15).
4. Discussion
In this study, we analyzed the efficacy of LLLT for patients with tinnitus using a meta-analysis to obtain a meaningful conclusion. For the five studies evaluating tinnitus improvement after intervention by THI score [1,28,29,30,31], the pooled effect estimate did not show a significant difference. Moreover, the pooled effect estimate did not reveal a difference in the improvement rate of the loudness of tinnitus within six studies [23,24,25,26,27,32]. To explore whether LLLT demonstrated different efficacy for tinnitus in patients with SNHL and idiopathic tinnitus, we conducted a subgroup analysis using nine studies, while the subgroup analysis of the influence of different wavelength and irradiation session settings was performed using all studies. None of the pooled estimates of the subgroup analysis demonstrated a significant difference between the low-level laser group and the control group. A visual summary of the results is presented in Figure 9.
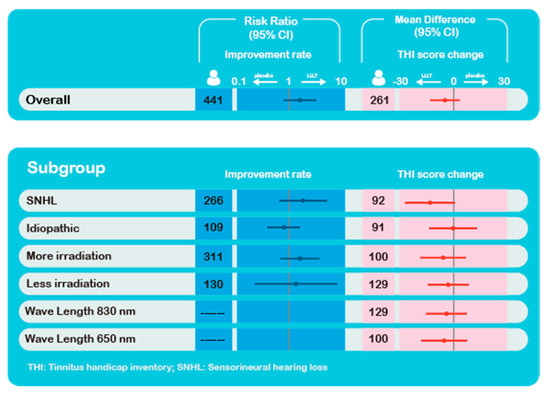
Figure 9.
Visual summary of the results.
The theoretical mechanism behind the therapy is assumed to involve several routes. Low-intensity laser irradiation increases blood microcirculation via sympathetic neural inhibition and prompts an increase in cell proliferation and division, thus speeding up the repair of damaged cells in the auditory system [7,8]. Additionally, another study noted that low-power laser stimulation is able to promote ATP synthesis in mitochondria by stimulating glucose combustion in the mitochondria, thus increasing the ATP supply for cell processes and decreasing cell damage [6]. Despite many studies that demonstrated a positive effect of laser irradiation on tinnitus, a previous study has shown that the transmission of light across the tympanic cavity and the promontory depends strongly on several factors. When irradiating the tympanic membrane or mastoid process, the transmitted light crosses anatomic structures in the middle ear, such as the eardrum, auditory ossicles, oval window, temporal bone and promontory bone, which may cause attenuation of laser irradiation. When different parts of the tympanic membrane or mastoid area are illuminated, a different light distribution within the cochlea results. Additionally, increasing the distance between the irradiation fiber tip and the irradiation target leads to attenuation of the transmitted irradiance [15,16]. Therefore, when laser irradiation is administered, the unique anatomy of the ear must be considered, as it may affect the penetration of the irradiance. In a retrospective study [33], a narrowed external acoustic meatus was found in up to 35% of normal people, which means that laser irradiance would be absorbed by the external acoustic meatus before reaching the cochlea. It is difficult to individualize laser treatments according to patients’ anatomical differences, which in turn makes it difficult to obtain the effect of laser irradiation since the majority of studies delivered irradiation transmeatally. Failure to perform controlled and constant irradiation may therefore represent a significant contributing factor to the widely varying therapeutic outcomes in existing studies of LLLT. We suggest more precise and constant delivery by techniques that can overcome the complexity of outer and middle ear structures in future studies to obtain the potential effect of LLLT.
Although some forms of tinnitus are most likely generated in the inner ear by abnormal activity of cochlear hair cells or by dysfunctions of the peripheral part of the auditory nerve, the central nervous system also accounts for some form of subjective tinnitus [4]. Several studies have indicated that the function of nuclei in the ascending auditory pathways is altered in those with tinnitus. Meanwhile, redirection of information to regions of the CNS that do not usually receive certain sources of auditory input occurs in those with tinnitus [34,35,36,37,38,39,40]. In one study that used voxel-based morphometry and functional magnetic resonance imaging to evaluate tinnitus-related functional and anatomical anomalies in the auditory and limbic systems, hyperactivity was present in the primary auditory cortices, posterior auditory cortices and nucleus accumbens of tinnitus patients [3]. Tinnitus associated with SNHL and idiopathic etiology has a certain degree of association with the CNS [4,41] and thus is unlikely to be eliminated by low-level laser irradiation, which affects mainly the peripheral components of the auditory system; these associations further explain the negative result in the subgroup analysis in the present study.
Among the included studies, Mollasadeghi et al. [32] was the only study that enrolled patients with tinnitus caused by noise-induced hearing loss and used transmastoid laser irradiation [32]. Although a previous study considered the transmastoidal route of laser irradiation to be therapeutically insufficient [15], the study demonstrated positive results for LLLT when delivered transmastoidally. As we discussed in the previous paragraph, LLLT might mainly affect the cochlea, and studies have shown that noise trauma can result in injury to hair cells in the inner ear and degeneration of the auditory nerve [42,43]. In this study, the patients who sustained injury from noise trauma to the cochlea might benefit the most from irradiation and therefore show the efficacy of irradiation for tinnitus. Nevertheless, further RCTs are required to support the effect of LLLT on tinnitus caused mainly by specific inner ear disease or injury.
Many studies were excluded due to lack of placebo control in the present meta-analysis. In those single-arm studies, a high percentage of improvement was reported. The favorable outcomes may come from the placebo effects. In one of the excluded studies showing a favorable effect of LLLT, patients also suffered from the comorbidity with of temporal-mandibular joint disorder (TMD) [44], which could benefit from LLLT too [45]. As somatosensory diseases like TMD [46,47,48], chronic headache [49], trigeminal neuralgia [50] or cervical spondylosis [51], could lead to tinnitus and the relief of those somatosensory diseases could also lead to improvement of tinnitus, the relationship between comorbidity and effect of LLLT would serve as the potential bias. To avoid the bias, it was worth emphasizing the importance on patient selection. In the present study, patients were composed of comorbidity of SNHL or idiopathic tinnitus and thus limited the potential bias, which would have been obtained in those excluded studies with comorbidity susceptible to LLLT.
Among the investigated studies, only one patient was reported to have developed sudden onset hearing impairment, and one patient developed dizziness during the course of LLLT [24]. No adverse effects after irradiation were reported or observed in other studies. Meta-analysis was not performed due to the lack of adequate effect estimates in the studies. We still consider the two sporadic adverse effects important, and these effects should be explained when obtaining informed consent from the patient before delivering the laser treatment. We look forward to further studies that analyze the safety of LLLT.
Limitations were present in our study. First, different measurement methods were used in the included studies, including THI and various rating scales (VAS, VRS and NRS). Among studies that report effect estimates with rating scales, converting the original score to the same effect estimate is not feasible. We therefore extracted dichotomous data from studies using the corresponding rating scale. At the same time, we did not stratify the degree of improvement, as some of the included studies did [24,32]. In the present extraction and adjustment, we obtained expanded effect estimates but may have overestimated the efficacy of LLLT. As a result, no significant difference in pooled effect estimates of the rating scale scores is seen, as in the pooled effect estimates of the THI score. Second, heterogeneity exists among the studies in terms of the technical parameters used. Tauber et al. [15] showed that the wavelength of the laser strongly influences the transmission of irradiation to the cochlea since a longer wavelength induces more transmission of the irradiation. The use of different wavelengths among the studies may have influenced cochlear irradiance and the effects of LLLT. Subgroup analysis on the influence of wavelength showed no difference between the two groups, as an identical overall effect was observed. Third, the timing of the effect estimates was examined in the studies. In Mirvakili et al. [26] and Mollasadeghi et al. [32], the treatment effects weakened over time. To minimize the effect of timing and obtain maximal LLLT efficacy, we pooled the effect estimate measured at the earliest timepoint after the intervention. No favorable result was demonstrated despite the adjustment. Finally, different numbers of irradiation sessions were addressed among various studies in this meta-analysis. The median treatment lasted 20 sessions, and we conducted subgroup analysis according to the effect estimate of those who underwent fewer than 20 sessions and those who underwent more than 20 sessions. No significant improvement has been shown with more irradiation sessions. Despite the subgroup analysis comparing the effects under different settings, there are still a number of factors that we were unable to analyze (e.g., different machines, races), and the existing heterogeneity underpowered the analysis. Meanwhile, the relatively small number of patients and studies might further underestimate the potential effect of LLLT, as we may glimpse a better but nonsignificant effect of LLLT in all the analyses. From these perspectives, we suggest that further large-scale, detailed RCTs are essential.
5. Conclusions
We evaluated the efficacy of LLLT in patients with tinnitus by meta-analysis. The results showed no favorable effect of LLLT, regardless of the measurement method and technical parameters. We suggest further large-scale studies to evaluate the efficacy of the therapy on tinnitus.
Supplementary Materials
The following are available online at https://www.mdpi.com/2076-3425/10/12/931/s1, Table S1: Detailed search strategy, Figure S1: Risk of Bias, Figure S2: Influence analysis of studies with THI measurement, Figure S3: Influence analysis of studies with improvement rate by rating scale, Figure S4: TSA for LLLT on overall THI, Figure S5: TSA for LLLT on THI with SNHL, Figure S6: TSA for LLLT on THI with idiopathic tinnitus, Figure S7: TSA for LLLT on THI with more irradiation, Figure S8: TSA for LLLT on THI with less irradiation, Figure S9: TSA for LLLT on THI with 650 nm wavelength, Figure S10: TSA for LLLT on THI with 830 nm wavelength, Figure S11: TSA for LLLT on overall improvement rate, Figure S12: TSA for LLLT on improvement rate with SNHL, Figure S13: TSA for LLLT on improvement rate with idiopathic tinnitus, Figure S14: TSA for LLLT on improvement rate with more irradiation, Figure S15: TSA for LLLT on improvement rate with less irradiation.
Author Contributions
C.-H.C. wrote the paper; C.-Y.H. contributed to the formal analysis and the resources organization of the figures; C.-Y.C. contributed to the investigation and the methodology; Y.-F.C. provided the conceptual input, funding acquisition, project administration and supervision. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by Taipei Veterans General Hospital (V108C-145, V109C-135).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Choi, J.E.; Lee, M.Y.; Chung, P.S.; Jung, J.Y. A preliminary study on the efficacy and safety of low level light therapy in the management of cochlear tinnitus: A single blind randomized clinical trial. Int. Tinnitus J. 2019, 23, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Zarenoe, R.; Ledin, T. A cohort study of patients with tinnitus and sensorineural hearing loss in a Swedish population. Auris Nasus Larynx 2013, 40, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Leaver, A.M.; Renier, L.; Chevillet, M.A.; Morgan, S.; Kim, H.J.; Rauschecker, J.P. Dysregulation of Limbic and Auditory Networks in Tinnitus. Neuron 2011, 69, 33–43. [Google Scholar] [CrossRef]
- Møller, A.R. Pathophysiology of tinnitus. Otolaryngol. Clin. N. Am. 2003, 36, 249–266. [Google Scholar] [CrossRef]
- Haider, H.F.; Hoare, D.J.; Costa, R.F.P.; Potgieter, I.; Kikidis, D.; Lapira, A.; Nikitas, C.; Caria, H.; Cunha, N.T.; Paço, J.C. Pathophysiology, Diagnosis and Treatment of Somatosensory Tinnitus: A Scoping Review. Front. Neurosci. 2017, 11. [Google Scholar] [CrossRef]
- Passarella, S.; Casamassima, E.; Molinari, S.; Pastore, D.; Quagliariello, E.; Catalano, I.M.; Cingolani, A. Increase of proton electrochemical potential and ATP synthesis in rat liver mitochondria irradiated in vitro by helium-neon laser. FEBS Lett. 1984, 175, 95–99. [Google Scholar] [CrossRef]
- Van Breugel, H.H.; Bär, P.R. Power density and exposure time of He-Ne laser irradiation are more important than total energy dose in photo-biomodulation of human fibroblasts in vitro. Lasers Surg. Med. 1992, 12, 528–537. [Google Scholar] [CrossRef]
- Schaffer, M.; Bonel, H.; Sroka, R.; Schaffer, P.M.; Busch, M.; Reiser, M.; Dühmke, E. Effects of 780 nm diode laser irradiation on blood microcirculation: Preliminary findings on time-dependent T1-weighted contrast-enhanced magnetic resonance imaging (MRI). J. Photochem. Photobiol. B 2000, 54, 55–60. [Google Scholar] [CrossRef]
- Moon, T.-H.; Lee, M.Y.; Jung, J.Y.; Ahn, J.-C.; Chang, S.-Y.; Chung, P.-S.; Rhee, C.-K.; Kim, Y.-H.; Suh, M.-W. Safety assessment of trans-tympanic photobiomodulation. Lasers Med. Sci. 2016, 31, 323–333. [Google Scholar] [CrossRef]
- Brosseau, L.; Robinson, V.; Wells, G.; Debie, R.; Gam, A.; Harman, K.; Morin, M.; Shea, B.; Tugwell, P. Low level laser therapy (Classes I, II and III) for treating rheumatoid arthritis. Cochrane Database Syst. Rev. 2005, 4, CD002049. [Google Scholar] [CrossRef]
- Stausholm, M.B.; Naterstad, I.F.; Joensen, J.; Lopes-Martins RÁ, B.; Sæbø, H.; Lund, H.; Fersum, K.V.; Bjordal, J.M. Efficacy of low-level laser therapy on pain and disability in knee osteoarthritis: Systematic review and meta-analysis of randomised placebo-controlled trials. BMJ Open 2019, 9, e031142. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.; Ma, J.; Chen, J.; Shen, B.; Pei, F.; Kraus, V.B. The effectiveness of low-level laser therapy for nonspecific chronic low back pain: A systematic review and meta-analysis. Arthritis Res. Ther. 2015, 17, 360. [Google Scholar] [CrossRef] [PubMed]
- Chow, R.T.; Johnson, M.I.; Lopes-Martins, R.A.; Bjordal, J.M. Efficacy of low-level laser therapy in the management of neck pain: A systematic review and meta-analysis of randomised placebo or active-treatment controlled trials. Lancet 2009, 374, 1897–1908. [Google Scholar] [CrossRef]
- Bjordal, J.M.; Lopes-Martins, R.A.; Joensen, J.; Couppe, C.; Ljunggren, A.E.; Stergioulas, A.; Johnson, M.I. A systematic review with procedural assessments and meta-analysis of low level laser therapy in lateral elbow tendinopathy (tennis elbow). BMC Musculoskelet. Disord. 2008, 9, 75. [Google Scholar] [CrossRef]
- Tauber, S.; Baumgartner, R.; Schorn, K.; Beyer, W. Lightdosimetric quantitative analysis of the human petrous bone: Experimental study for laser irradiation of the cochlea. Lasers Surg. Med. 2001, 28, 18–26. [Google Scholar] [CrossRef]
- Lee, J.-H.; Kim, S.; Jung, J.Y.; Lee, M.Y. Applications of photobiomodulation in hearing research: From bench to clinic. Biomed. Eng. Lett. 2019, 9, 351–358. [Google Scholar] [CrossRef]
- Laakso, L.; Richardson, C.; Cramond, T. Factors affecting low level laser therapy. Aust. J. Physiother. 1993, 39, 95–99. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Wetterslev, J.; Jakobsen, J.C.; Gluud, C. Trial Sequential Analysis in systematic reviews with meta-analysis. BMC Med. Res. Methodol. 2017, 17, 1–18. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020; Available online: https://www.R-project.org/ (accessed on 1 December 2020).
- Trial Sequential Analysis Software; Copenhagen Trial Unit, Centre for Clinical Intervention Research, Rigshospitalet: Copenhagen, Denmark, 2016; Available online: http://www.ctu.dk/tsa (accessed on 1 December 2020).
- Gungor, A.; Dogru, S.; Cincik, H.; Erkul, E.; Poyrazoglu, E. Effectiveness of transmeatal low power laser irradiation for chronic tinnitus. J. Laryngol. Otol. 2008, 122, 447–451. [Google Scholar] [CrossRef]
- Nakashima, T.; Ueda, H.; Misawa, H.; Suzuki, T.; Tominaga, M.; Ito, A.; Numata, S.; Kasai, S.; Asahi, K.; Vernon, J.A.; et al. Transmeatal low-power laser irradiation for tinnitus. Otol. Neurotol. 2002, 23, 296–300. [Google Scholar] [CrossRef]
- Dehkordi, M.A.; Einolghozati, S.; Ghasemi, S.M.; Abolbashari, S.; Meshkat, M.; Behzad, H. Effect of low-level laser therapy in the treatment of cochlear tinnitus: A double-blind, placebo-controlled study. Ear Nose Throat J. 2015, 94, 32–36. [Google Scholar] [PubMed]
- Mirvakili, A.; Mehrparvar, A.; Mostaghaci, M.; Mollasadeghi, A.; Mirvakili, M.; Baradaranfar, M. Low level laser effect in treatment of patients with intractable tinnitus due to sensorineural hearing loss. J. Lasers Med. Sci. 2014, 5, 71–74. [Google Scholar] [PubMed]
- Ngao, C.F.; Tan, T.S.; Narayanan, P.; Raman, R. The effectiveness of transmeatal low-power laser stimulation in treating tinnitus. Eur. Arch. Oto Rhino Laryngol. 2014, 271, 975–980. [Google Scholar] [CrossRef] [PubMed]
- Teggi, R.; Bellini, C.; Piccioni, L.O.; Palonta, F.; Bussi, M. Transmeatal low-level laser therapy for chronic tinnitus with cochlear dysfunction. Audiol. Neuro Otol. 2009, 14, 115–120. [Google Scholar] [CrossRef]
- Cuda, D.; De Caria, A. Effectiveness of combined counseling and low-level laser stimulation in the treatment of disturbing chronic tinnitus. Int. Tinnitus J. 2008, 14, 175–180. [Google Scholar]
- Rhee, C.K.; Lim, E.S.; Kim, Y.S.; Chung, Y.W.; Jung, J.Y.; Chung, P.S. Effect of low level laser (LLL) on cochlear and vestibular inner ear including tinnitus. In Proceedings of the SPIE Photonics West conference, San Jose, CA, USA, 21–26 January 2006. [Google Scholar] [CrossRef]
- Mirz, F.; Zachariae, R.; Andersen, S.E.; Nielsen, A.G.; Johansen, L.V.; Bjerring, P.; Pedersen, C.B. The low-power laser in the treatment of tinnitus. Clin. Otolaryngol. Allied Sci. 1999, 24, 346–354. [Google Scholar] [CrossRef]
- Mollasadeghi, A.; Mirmohammadi, S.J.; Mehrparvar, A.H.; Davari, M.H.; Shokouh, P.; Mostaghaci, M.; Baradaranfar, M.H.; Bahaloo, M. Efficacy of low-level laser therapy in the management of tinnitus due to noise-induced hearing loss: A double-blind randomized clinical trial. Sci. World J. 2013, 2013. [Google Scholar] [CrossRef]
- Kumar, R.S.; Kumar, K.; Bhavan, D.; Anandaraj, A. Variations in the External Auditory Canal of 185 Adult Individuals: A Clinico-Morphological Study. Int. J. Sci. Res. Publ. 2013, 3, 1–5. [Google Scholar]
- Gerken, G.M.; Saunders, S.S.; Paul, R.E. Hypersensitivity to electrical stimulation of auditory nuclei follows hearing loss in cats. Hear. Res. 1984, 13, 249–259. [Google Scholar] [CrossRef]
- Kaltenbach, J.A.; Afman, C.E. Hyperactivity in the dorsal cochlear nucleus after intense sound exposure and its resemblance to tone-evoked activity: A physiological model for tinnitus. Hear. Res. 2000, 140, 165–172. [Google Scholar] [CrossRef]
- Lockwood, A.H.; Salvi, R.; Coad, M.; Towsley, M.; Wack, D.; Murphy, B. The functional neuroanatomy of tinnitus: Evidence for limbic system links and neural plasticity. Neurology 1998, 50, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Møller, A.R.; Møller, M.B.; Yokota, M. Some forms of tinnitus may involve the extralemniscal auditory pathway. Laryngoscope 1992, 102, 1165–1171. [Google Scholar] [CrossRef] [PubMed]
- Moller, A.R. Similarities between Severe. J. Am. Acad. Audiol. 2000, 11, 115–124. [Google Scholar] [PubMed]
- Shore, S.E.; Roberts, L.E.; Langguth, B. Maladaptive plasticity in tinnitus—Triggers, mechanisms and treatment. Nat. Rev. Neurol. 2016, 12, 150. [Google Scholar] [CrossRef]
- Marks, K.L.; Martel, D.T.; Wu, C.; Basura, G.J.; Roberts, L.E.; Schvartz-Leyzac, K.C.; Shore, S.E. Auditory-somatosensory bimodal stimulation desynchronizes brain circuitry to reduce tinnitus in guinea pigs and humans. Sci. Transl. Med. 2018, 10. [Google Scholar] [CrossRef]
- Zenner, H.-P.; Delb, W.; Kröner-Herwig, B.; Jäger, B.; Peroz, I.; Hesse, G.; Mazurek, B.; Goebel, G.; Gerloff, C.; Trollmann, R. A multidisciplinary systematic review of the treatment for chronic idiopathic tinnitus. Eur. Arch. Oto Rhino Laryngol. 2017, 274, 2079–2091. [Google Scholar] [CrossRef]
- Le, T.N.; Straatman, L.V.; Lea, J.; Westerberg, B. Current insights in noise-induced hearing loss: A literature review of the underlying mechanism, pathophysiology, asymmetry, and management options. J. Otolaryngol. Head Neck Surg. 2017, 46, 41. [Google Scholar] [CrossRef]
- Wang, Y.; Hirose, K.; Liberman, M.C. Dynamics of noise-induced cellular injury and repair in the mouse cochlea. J. Assoc. Res. Otolaryngol. 2002, 3, 248–268. [Google Scholar] [CrossRef]
- Demirkol, N.; Usumez, A.; Demirkol, M.; Sari, F.; Akcaboy, C. Efficacy of Low-Level Laser Therapy in Subjective Tinnitus Patients with Temporomandibular Disorders. Photomed. Laser Surg. 2017, 35, 427–431. [Google Scholar] [CrossRef] [PubMed]
- Madani, A.S.; Ahrari, F.; Nasiri, F.; Abtahi, M.; Tunér, J. Low-level laser therapy for management of TMJ osteoarthritis. Cranio® 2014, 32, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Omidvar, S.; Jafari, Z. Association Between Tinnitus and Temporomandibular Disorders: A Systematic Review and Meta-Analysis. Ann. Otol. Rhinol. Laryngol. 2019, 128, 662–675. [Google Scholar] [CrossRef] [PubMed]
- Cox, K.W. Temporomandibular Disorder and New Aural Symptoms. Arch. Otolaryngol. Head Neck Surg. 2008, 134, 389–393. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kuttila, S.; Kuttila, M.; Le Bell, Y.; Alanen, P.; Jouko, S. Aural Symptoms and Signs of Temporomandibular Disorder in Association With Treatment Need and Visits to a Physician. Laryngoscope 1999, 109, 1669–1673. [Google Scholar] [CrossRef] [PubMed]
- Nowaczewska, M.; Wiciński, M.; Straburzyński, M.; Kaźmierczak, W. The Prevalence of Different Types of Headache in Patients with Subjective Tinnitus and Its Influence on Tinnitus Parameters: A Prospective Clinical Study. Brain Sci. 2020, 10, 776. [Google Scholar] [CrossRef]
- Cheng, Y.F.; Xirasagar, S.; Yang, T.H.; Wu, C.S.; Kao, Y.W.; Shia, B.C.; Lin, H.C. Increased risk of tinnitus following a trigeminal neuralgia diagnosis: A one-year follow-up study. J. Headache Pain 2020, 21, 46. [Google Scholar] [CrossRef]
- Cheng, Y.F.; Xirasagar, S.; Yang, T.H.; Wu, C.S.; Kuo, N.W.; Lin, H.C. A population-based case-control study of the association between cervical spondylosis and tinnitus. Int J. Audiol. 2020, 1–5. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).