Precision and Reliability of a Dynamometer for Trunk Extension Strength and Steadiness Assessment
Abstract
1. Introduction
2. Materials and Methods
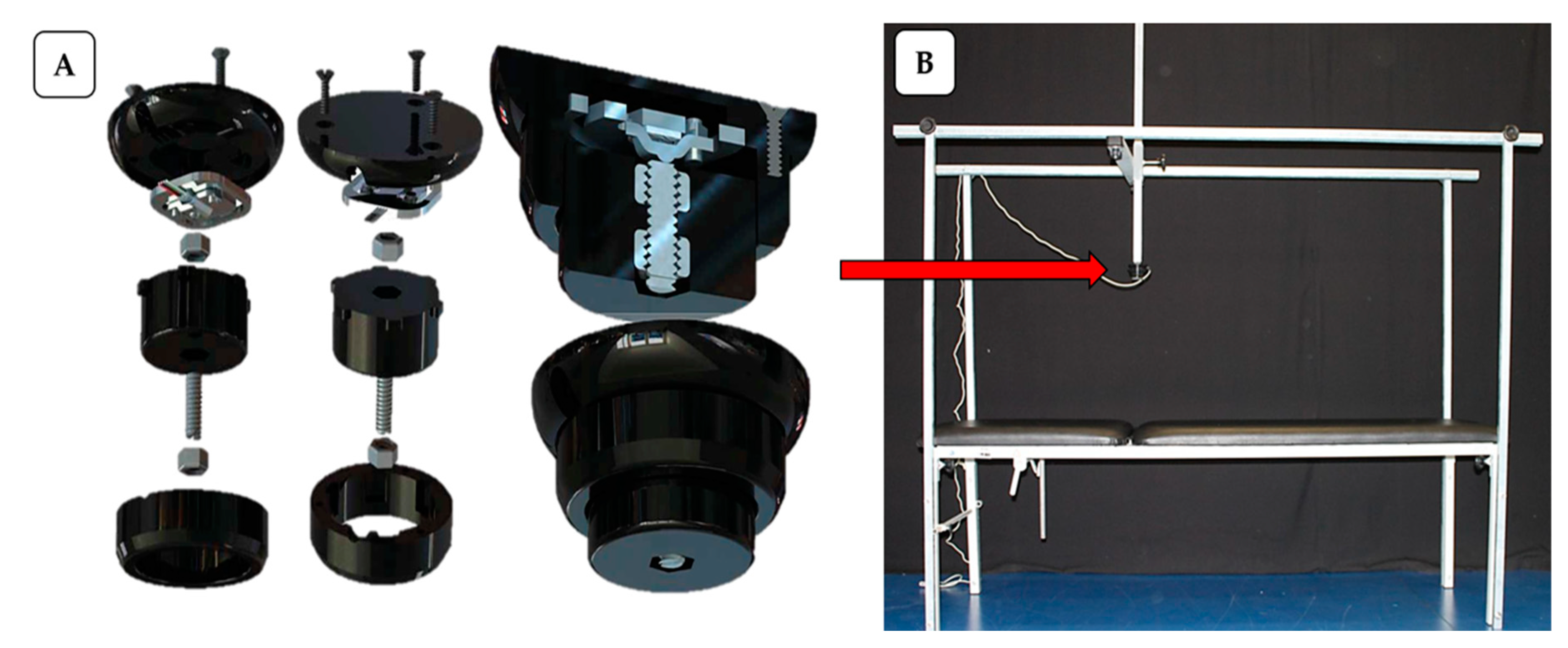
2.1. Force Measurement System
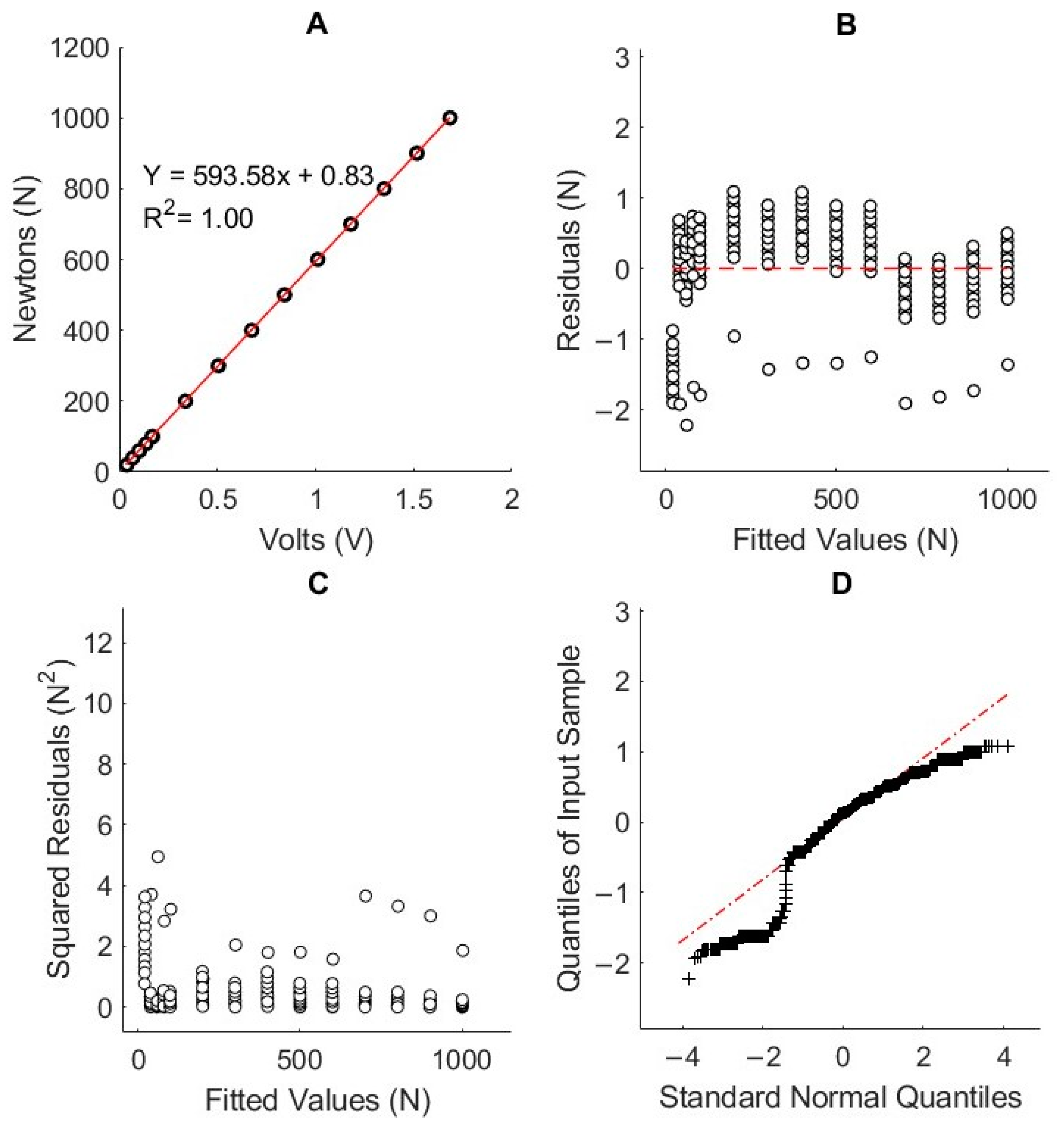
2.2. Calibration
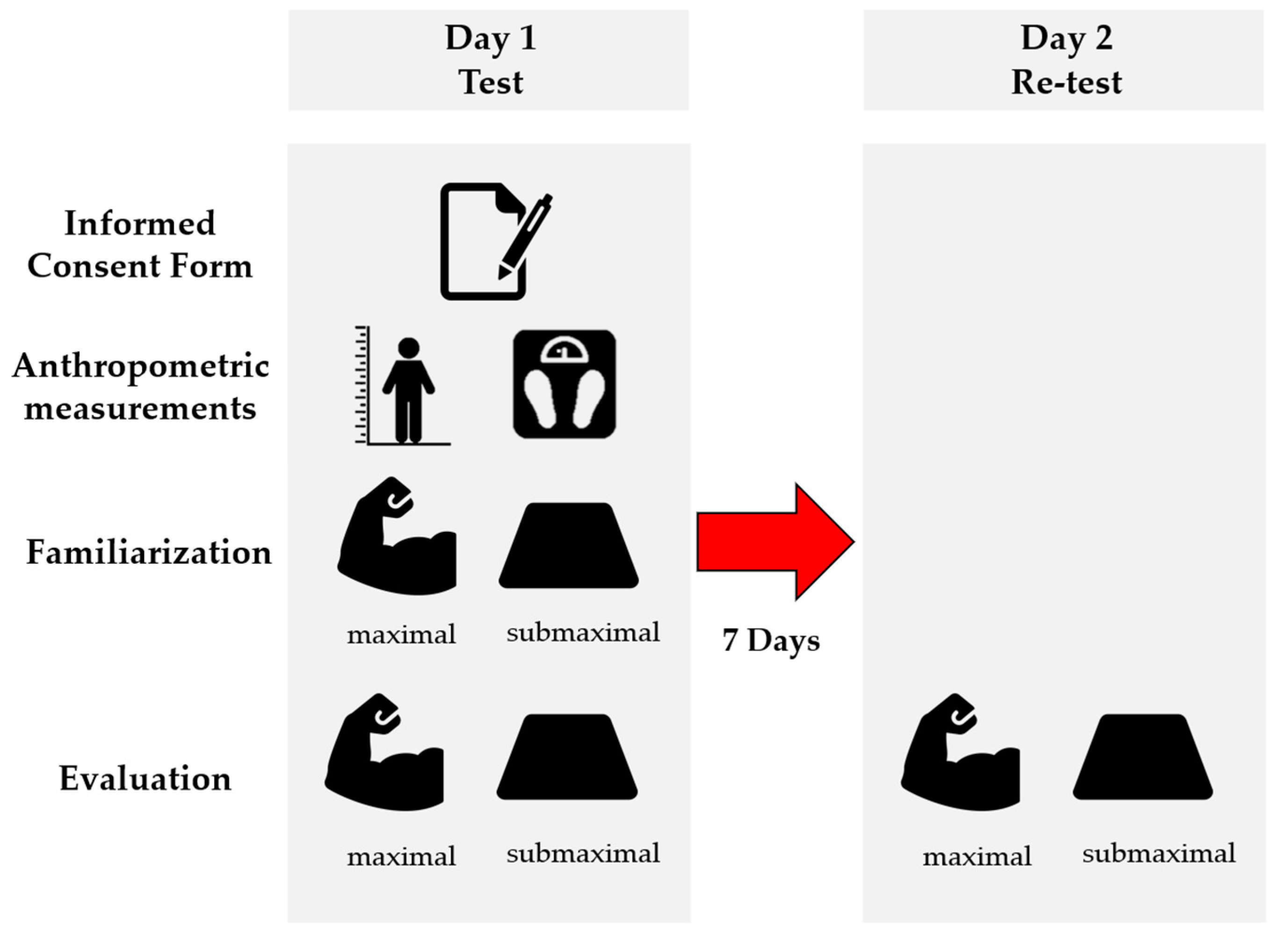
2.3. Reliability of Experimental Procedures
2.4. Sample
2.5. Familiarization and Evaluation
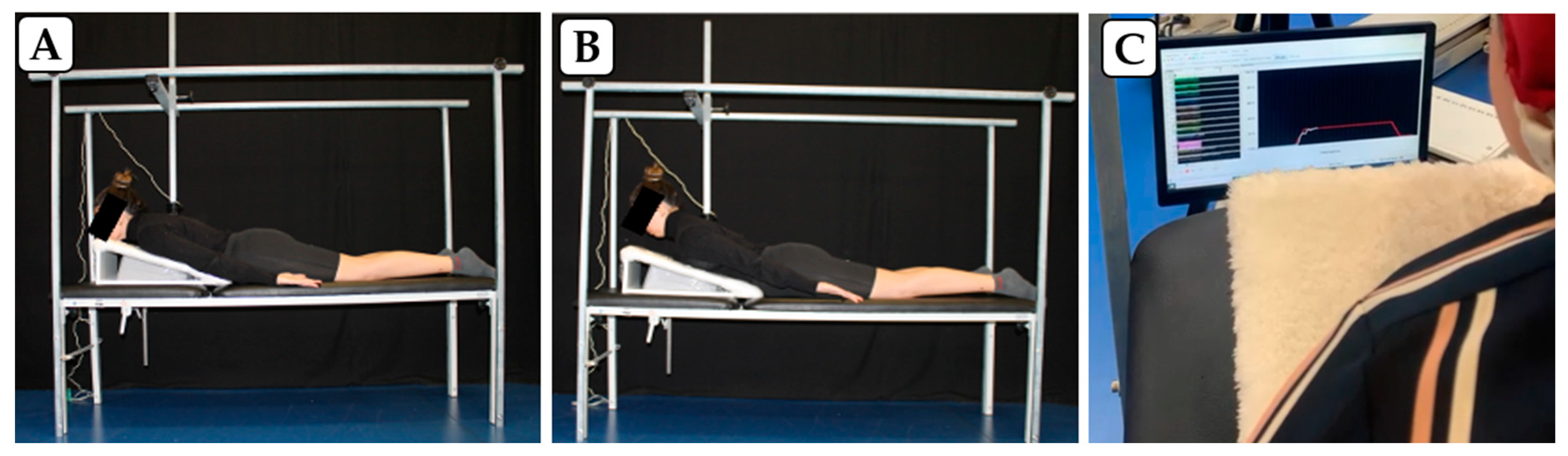
2.5.1. Participant Setup and Position
2.5.2. Familiarization Protocol
2.5.3. Evaluation Protocol
2.6. Data Processing
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vos, T.; Flaxman, A.D.; Naghavi, M.; Lozano, R.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; Aboyans, V.; et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2163–2196. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, T.; Mills, K.; Brown, B.T.; Herbert, R.D.; Maher, C.G.; Hancock, M.J. Risk of Recurrence of Low Back Pain: A Systematic Review. J. Orthop. Sports Phys. Ther. 2017, 47, 305–313. [Google Scholar] [CrossRef] [PubMed]
- McGill, S.M. Distribution of tissue loads in the low back during a variety of daily and rehabilitation tasks. J. Rehabil. Res. Dev. 1997, 34, 448–458. [Google Scholar] [PubMed]
- Arins, M.R.; Murara, N.; Bottamedi, X.; Ramos, J.d.S.; Woellner, S.S.; Soares, A.V. Physiotherapeutic treatment Schedule for chronic low back pain: Influence on pain, quality of life and functional capacity. Revista Dor 2016, 17, 192–196. [Google Scholar] [CrossRef][Green Version]
- Alaranta, H.; Luoto, S.; Heliövaara, M.; Hurri, H. Static back endurance and the risk of low-back pain. Clin. Biomech. 1995, 10, 323–324. [Google Scholar] [CrossRef]
- Larsen, L.H.; Hirata, R.P.; Graven-Nielsen, T. Experimental Low Back Pain Decreased Trunk Muscle Activity in Currently Asymptomatic Recurrent Low Back Pain Patients During Step Tasks. J. Pain 2018, 19, 542–551. [Google Scholar] [CrossRef]
- van Dieën, J.H.; Reeves, N.P.; Kawchuk, G.; van Dillen, L.R.; Hodges, P.W. Motor Control Changes in Low Back Pain: Divergence in Presentations and Mechanisms. J. Orthop. Sports Phys. Ther. 2019, 49, 370–379. [Google Scholar] [CrossRef]
- Neufuss, J.; Hesse, B.; Thorpe, S.K.; Vereecke, E.E.; D′Aout, K.; Fischer, M.S.; Schilling, N. Fibre type composition in the lumbar perivertebral muscles of primates: Implications for the evolution of orthogrady in hominoids. J. Anat. 2014, 224, 113–131. [Google Scholar] [CrossRef]
- Cholewicki, J.; McGill, S.M. Mechanical stability of the in vivo lumbar spine: Implications for injury and chronic low back pain. Clin. Biomech. 1996, 11, 1–15. [Google Scholar] [CrossRef]
- Hicks, G.E.; Fritz, J.M.; Delitto, A.; McGill, S.M. Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program. Arch. Phys. Med. Rehabil. 2005, 86, 1753–1762. [Google Scholar] [CrossRef]
- Ruiz, J.R.; Sui, X.; Lobelo, F.; Morrow, J.R., Jr.; Jackson, A.W.; Sjöström, M.; Blair, S.N. Association between muscular strength and mortality in men: Prospective cohort study. Bmj 2008, 337, a439. [Google Scholar] [CrossRef]
- Camposo, L.; Pereira, R. Correlação entre os testes de dinamometria de preensão manual, escapular e lombar com o desempenho no Special Judo Fitness Test. Rev. Educ. Física/J. Phys. Educ. 2015, 84, 65–72. [Google Scholar] [CrossRef]
- Brill, P.A.; Macera, C.A.; Davis, D.R.; Blair, S.N.; Gordon, N. Muscular strength and physical function. Med. Sci. Sports Exerc. 2000, 32, 412–416. [Google Scholar] [CrossRef]
- Althobaiti, S.; Falla, D. Reliability and criterion validity of handheld dynamometry for measuring trunk muscle strength in people with and without chronic non-specific low back pain. Musculoskelet. Sci. Pract. 2023, 66, 102799. [Google Scholar] [CrossRef]
- Yang, S.; Wu, W.; Zhang, C.; Wang, D.; Chen, C.; Tang, Y.; Li, K.; Xu, J.; Luo, F. Reliability and validity of three isometric back extensor strength assessments with different test postures. J. Int. Med. Res. 2020, 48, 0300060519885268. [Google Scholar] [CrossRef] [PubMed]
- Vlažná, D.; Krkoška, P.; Kuhn, M.; Dosbaba, F.; Baťalík, L.; Vlčková, E.; Voháňka, S.; Adamová, B. Assessment of Lumbar Extensor Muscles in the Context of Trunk Function, a Pilot Study in Healthy Individuals. Appl. Sci. 2021, 11, 9518. [Google Scholar] [CrossRef]
- Gruther, W.; Wick, F.; Paul, B.; Leitner, C.; Posch, M.; Matzner, M.; Crevenna, R.; Ebenbichler, G. Diagnostic accuracy and reliability of muscle strength and endurance measurements in patients with chronic low back pain. J. Rehabil. Med. 2009, 41, 613–619. [Google Scholar] [CrossRef]
- Moreland, J.; Finch, E.; Stratford, P.; Balsor, B.; Gill, C. Interrater reliability of six tests of trunk muscle function and endurance. J. Orthop. Sports Phys. Ther. 1997, 26, 200–208. [Google Scholar] [CrossRef]
- Essendrop, M.; Schibye, B.; Hansen, K. Reliability of isometric muscle strength tests for the trunk, hands and shoulders. Int. J. Ind. Ergon. 2001, 28, 379–387. [Google Scholar] [CrossRef]
- Larivière, C.; Gagnon, D.; Loisel, P. The effect of load on the coordination of the trunk for subjects with and without chronic low back pain during flexion-extension & lateral bending tasks. Clin. Biomech. 2000, 15, 407–416. [Google Scholar]
- Kell, R.T.; Bell, G.; Quinney, A. Musculoskeletal fitness, health outcomes and quality of life. Sports Med. 2001, 31, 863–873. [Google Scholar] [CrossRef]
- Steele, J.; Fisher, J.; Perrin, C.; Conway, R.; Bruce-Low, S.; Smith, D. Does change in isolated lumbar extensor muscle function correlate with good clinical outcome? A secondary analysis of data on change in isolated lumbar extension strength, pain, and disability in chronic low back pain. Disabil. Rehabil. 2019, 41, 1287–1295. [Google Scholar]
- De Vet, H.C.; Terwee, C.B.; Mokkink, L.B.; Knol, D.L. Measurement in Medicine: A Practical Guide; Cambridge University Press: Cambridge, UK, 2011. [Google Scholar]
- Chou, R.; Shekelle, P. Will this patient develop persistent disabling low back pain? JAMA 2010, 303, 1295–1302. [Google Scholar] [CrossRef]
- Pincus, T.; Burton, A.; Vogel, S.; Field, A. A Systematic Review of Psychological Factors as Predictors of Chronicity/Disability in Prospective Cohorts of Low Back Pain. Spine 2002, 27, E109–E120. [Google Scholar] [CrossRef]
- Gonçalves, M.; Barbosa, F.S.S. Análise de parâmetros de força e resistência dos músculos eretores da espinha lombar durante a realização de exercício isométrico em diferentes níveis de esforço. Rev. Bras. Med. Esporte 2005, 11, 109–114. [Google Scholar]
- Jain, S.; Shetty, G.; Munje, P.; Bhan, A.; Linjhara, S.; Ram, C.S. Gender-based Variations in Trunk Motion and Isometric Strength in Young Adults with Low Back Pain: A Prospective Case-control Study. Rev. Bras. Ortop. 2022, 57, 392–401. [Google Scholar]
- Valentin, G.; Maribo, T. Hand-held dynamometry fixated with a tripod is reliable for assessment of back extensor strength in women with osteoporosis. Osteoporos. Int. 2014, 25, 2143–2149. [Google Scholar] [CrossRef]
- Eichinger, F.; Soares, A.; Júnior, J.; Gevaerd, M.; Domenech, S.; Júnior, N. Dinamometria lombar: Um teste funcional para o tronco. Rev. Bras. Med. Trab. 2016, 14, 120–126. [Google Scholar] [CrossRef]
- Müller, I.; Machado de Brito, R.; Pereira, C.; Brusamarello, V. Load cells in force sensing analysis—Theory and a novel application. IEEE Instrum. Meas. Mag. 2010, 13, 15–19. [Google Scholar] [CrossRef]
- Freitas, C.D.D.; Greve, J.M.D.A. Estudo comparativo entre exercícios com dinamômetro isocinético e bola terapêutica na lombalgia crônica de origem mecânica. Fisioter. Pesqui. 2008, 15, 380–386. [Google Scholar]
- Guilhem, G.; Giroux, C.; Couturier, A.; Maffiuletti, N.A. Validity of trunk extensor and flexor torque measurements using isokinetic dynamometry. J. Electromyogr. Kinesiol. 2014, 24, 986–993. [Google Scholar]
- Althobaiti, S.; Rushton, A.; Aldahas, A.; Falla, D.; Heneghan, N.R. Practicable performance-based outcome measures of trunk muscle strength and their measurement properties: A systematic review and narrative synthesis. PLoS ONE 2022, 17, e0270101. [Google Scholar]
- De Blaiser, C.; De Ridder, R.; Willems, T.; Danneels, L.; Roosen, P. Reliability and validity of trunk flexor and trunk extensor strength measurements using handheld dynamometry in a healthy athletic population. Phys. Ther. Sport 2018, 34, 180–186. [Google Scholar]
- Bonhof-Jansen, E.D.J.; van Ham, A.; Kroon, G.J.; Winter, R.W.; Brink, S.M. Validity and reliability of a portable handheld dynamometer compared to a fixed isokinetic dynamometer to assess forearm torque strength. Hand Surg. Rehabil. 2023, 42, 147–153. [Google Scholar] [CrossRef]
- Barros, M.; Clemente, N.; Rezende, F.; Cardoso, T.; Thomaz, S.R.T.; Garcia, P.; Ribeiro, A.; Martins, W. Reliability of the handheld dynamometer in the evaluation of the muscle strength of trunk extensors in healthy adults. Motricidade 2021, 17, 235–241. [Google Scholar] [CrossRef]
- Jubany, J.; Busquets, A.; Marina, M.; Cos, F.; Angulo-Barroso, R. Reliability and validity of a custom-made instrument including a hand-held dynamometer for measuring trunk muscle strength. J. Back Musculoskelet. Rehabil. 2015, 28, 317–326. [Google Scholar]
- Martínez-Romero, M.T.; Ayala, F.; De Ste Croix, M.; Vera-Garcia, F.J.; Sainz de Baranda, P.; Santonja-Medina, F.; Sánchez-Meca, J. A Meta-Analysis of the Reliability of Four Field-Based Trunk Extension Endurance Tests. Int. J. Environ. Res. Public Health 2020, 17, 3088. [Google Scholar] [CrossRef]
- Arvanitidis, M.; Falla, D.; Sanderson, A.; Martinez-Valdes, E. Does pain influence control of muscle force? A systematic review and meta-analysis. Eur. J. Pain 2025, 29, e4716. [Google Scholar] [CrossRef]
- ASTM E8/E8M-09; Standard Test Methods for Tension Testing of Metallic Materials. ASTM International: West Conshohocken, PA, USA, 2010. [CrossRef]
- Nawab, S.H.; Chang, S.S.; De Luca, C.J. High-yield decomposition of surface EMG signals. Clin. Neurophysiol. 2010, 121, 1602–1615. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Lipovšek, T.; Kacin, A.; Puh, U. Reliability and validity of hand-held dynamometry for assessing lower limb muscle strength. Isokinet. Exerc. Sci. 2021, 30, 231–240. [Google Scholar] [CrossRef]
- Shrout, P.E.; Fleiss, J.L. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef]
- Stark, T.; Walker, B.; Phillips, J.K.; Fejer, R.; Beck, R. Hand-held dynamometry correlation with the gold standard isokinetic dynamometry: A systematic review. PMR 2011, 3, 472–479. [Google Scholar] [CrossRef]
- Park, H.W.; Baek, S.; Kim, H.Y.; Park, J.G.; Kang, E.K. Reliability and Validity of a New Method for Isometric Back Extensor Strength Evaluation Using A Hand-Held Dynamometer. Ann. Rehabil. Med. 2017, 41, 793–800. [Google Scholar] [CrossRef]
- Silva, M.F.; Dias, J.M.; Pereira, L.M.; Mazuquin, B.F.; Lindley, S.; Richards, J.; Cardoso, J.R. Determination of the motor unit behavior of lumbar erector spinae muscles through surface EMG decomposition technology in healthy female subjects. Muscle Nerve 2017, 55, 28–34. [Google Scholar] [CrossRef]
- Hodges, P.W.; Tucker, K. Moving differently in pain: A new theory to explain the adaptation to pain. Pain 2011, 152, S90–S98. [Google Scholar] [CrossRef] [PubMed]
- Bouisset, S.; Zattara, M. Biomechanical study of the programming of anticipatory postural adjustments associated with voluntary movement. J. Biomech. 1987, 20, 735–742. [Google Scholar] [CrossRef] [PubMed]
- Hunt, A. A Guide to the Measurement of Force; Institute of Measurement and Control: London, UK, 1998. [Google Scholar]
- Juan-Recio, C.; Barbado, D.; Vaquero, M.P.; López-Plaza, D. Reliability assessment and correlation analysis of three protocols to measure trunk muscle strength and endurance. J. Sports Sci. 2017, 36, 357–364. [Google Scholar] [CrossRef]
- Zemková, E.; Zapletalová, L. The Role of Neuromuscular Control of Postural and Core Stability in Functional Movement and Athlete Performance. Front. Physiol. 2022, 13, 796097. [Google Scholar] [CrossRef]
- Hamed, A.; Hamed, A.; Bohm, S.; Mersmann, F.; Arampatzis, A. Exercises of dynamic stability under unstable conditions increase muscle strength and balance ability in the elderly. Scand. J. Med. Sci. Sports 2018, 28, 961–971. [Google Scholar] [CrossRef]
- Kollmitzer, J.; Ebenbichler, G.; Sabo, A.; Kerschan, K.; Bochdansky, T. Effects of back extensor strength training versus balance training on postural control. Med. Sci. Sports Exerc. 2000, 32, 1770–1776. [Google Scholar] [CrossRef] [PubMed]
- McGill, S.M. Low back stability: From formal description to issues for performance and rehabilitation. Exerc. Sport Sci. Rev. 2001, 29, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Soares, A.; Júnior, J.; Silva, L.; Domenech, S.; Gomes, N. Valores Normativos Da Dinamometria Lombar: Um Teste Funcional Para O Tronco. In Proceedings of the IV Simpósio em Neuromecânica Aplicada, Florianópolis, Brasil, 28 November 2013. [Google Scholar]
- Parolini, F.; Goethel, M.; Becker, K.; Fernandes, C.; Fernandes, R.J.; Ervilha, U.F.; Santos, R.; Vilas-Boas, J.P. Breaking Barriers: Artificial Intelligence Interpreting the Interplay between Mental Illness and Pain as Defined by the International Association for the Study of Pain. Biomedicines 2023, 11, 2042. [Google Scholar] [CrossRef] [PubMed]
- Burton, N.W.; Turrell, G.; Oldenburg, B.; Sallis, J.F. The relative contributions of psychological, social, and environmental variables to explain participation in walking, moderate-, and vigorous-intensity leisure-time physical activity. J. Phys. Act. Health 2005, 2, 181–196. [Google Scholar]
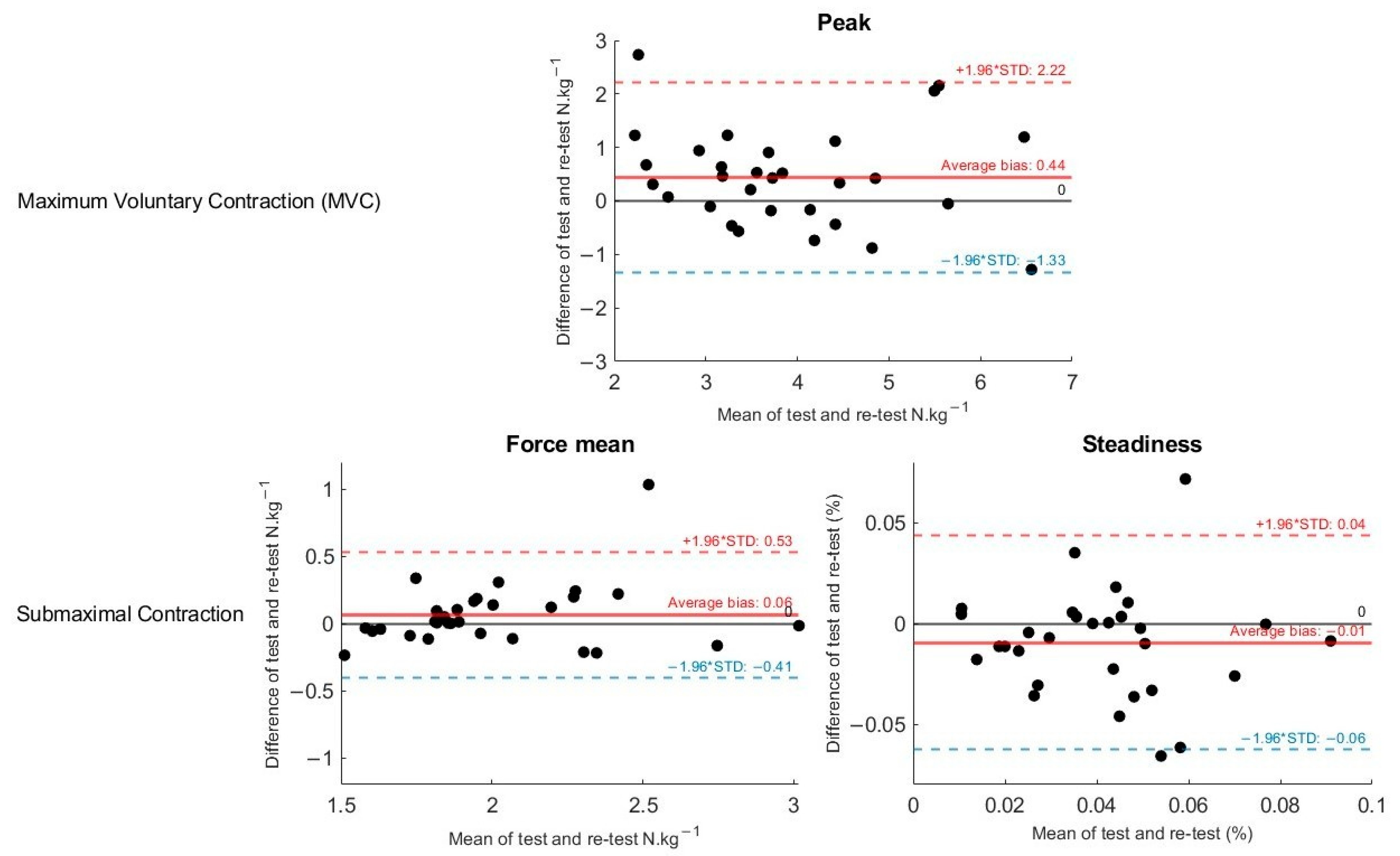
| Test/Retest | Day 1 | Day 2 | p | Cohen’s d | MDC | SEM | ICC (95% CI) | R2 |
|---|---|---|---|---|---|---|---|---|
| Maximal voluntary contractions (MVC) | ||||||||
| Peak force (N·kg−1) | 4.07 (1.18) | 3.88 (1.23) | 0.22 | 0.58 | 1.39 | 0.5 | 0.81 (0.62, 0.91) | 0.71 |
| Submaximal voluntary contraction (SMVC) | ||||||||
| Mean Force (N·kg−1) | 1.88 (0.39) | 2.07 (0.34) | 0.24 | 0.45 | 1.08 | 0.17 | 0.93 (0.84, 0.97) | 0.88 |
| Steadiness (%) | 1.88 (1.22) | 2.46 (1.37) | 0.83 | 0.44 | 2.36 | 0.85 | 0.87 (0.78, 0.90) | 0.40 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Parolini, F.; Goethel, M.; Robalino, J.; Becker, K.; Sousa, M.; Pulcineli, B.C.; Ervilha, U.F.; Vilas-Boas, J.P.; Santos, R. Precision and Reliability of a Dynamometer for Trunk Extension Strength and Steadiness Assessment. Appl. Sci. 2025, 15, 4081. https://doi.org/10.3390/app15084081
Parolini F, Goethel M, Robalino J, Becker K, Sousa M, Pulcineli BC, Ervilha UF, Vilas-Boas JP, Santos R. Precision and Reliability of a Dynamometer for Trunk Extension Strength and Steadiness Assessment. Applied Sciences. 2025; 15(8):4081. https://doi.org/10.3390/app15084081
Chicago/Turabian StyleParolini, Franciele, Márcio Goethel, Johan Robalino, Klaus Becker, Manoela Sousa, Barbara C. Pulcineli, Ulysses F. Ervilha, João Paulo Vilas-Boas, and Rubim Santos. 2025. "Precision and Reliability of a Dynamometer for Trunk Extension Strength and Steadiness Assessment" Applied Sciences 15, no. 8: 4081. https://doi.org/10.3390/app15084081
APA StyleParolini, F., Goethel, M., Robalino, J., Becker, K., Sousa, M., Pulcineli, B. C., Ervilha, U. F., Vilas-Boas, J. P., & Santos, R. (2025). Precision and Reliability of a Dynamometer for Trunk Extension Strength and Steadiness Assessment. Applied Sciences, 15(8), 4081. https://doi.org/10.3390/app15084081











