Peri-Implant Bone Stability Around Tapered Implant Prosthetic Connection: A Systematic Review and Meta-Analysis Comparing Different Cone Morse and Conometric Implants Angle Contact and Coupling Interface Designs
Abstract
1. Introduction
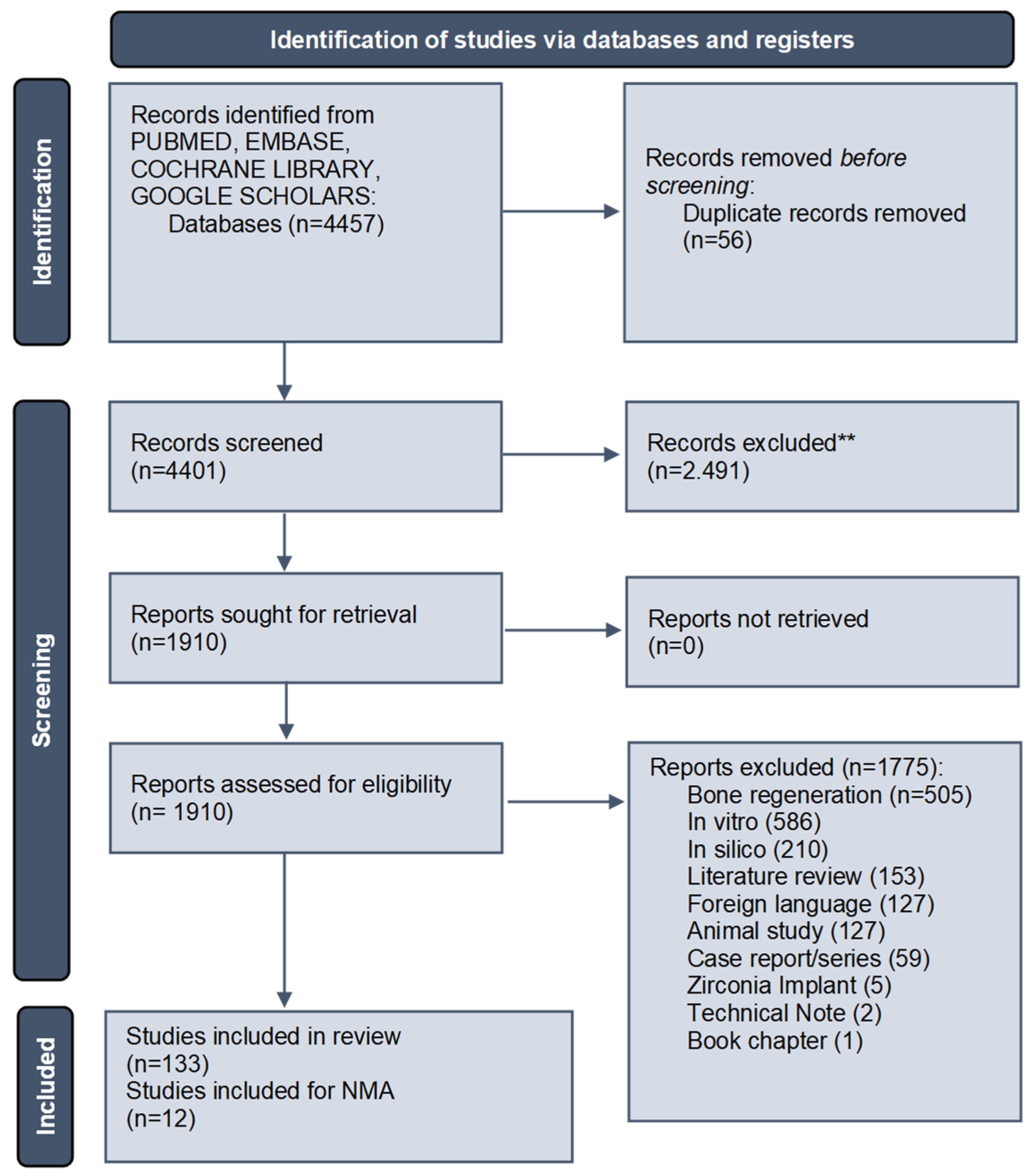
2. Materials and Methods
2.1. Preliminary Screening Strategy
- (1)
- P = population/patient/problem—subjects needing a dental implant for prosthetic rehabilitations;
- (2)
- I = intervention—dental implant treatment positioning and fixed oral rehabilitation;
- (3)
- C = comparison—comparison between different internal, external and conical prosthetic joints;
- (4)
- O = outcome—marginal bone loss; major prosthetic complications.
2.2. Inclusion Criteria
2.3. Study Data Extraction
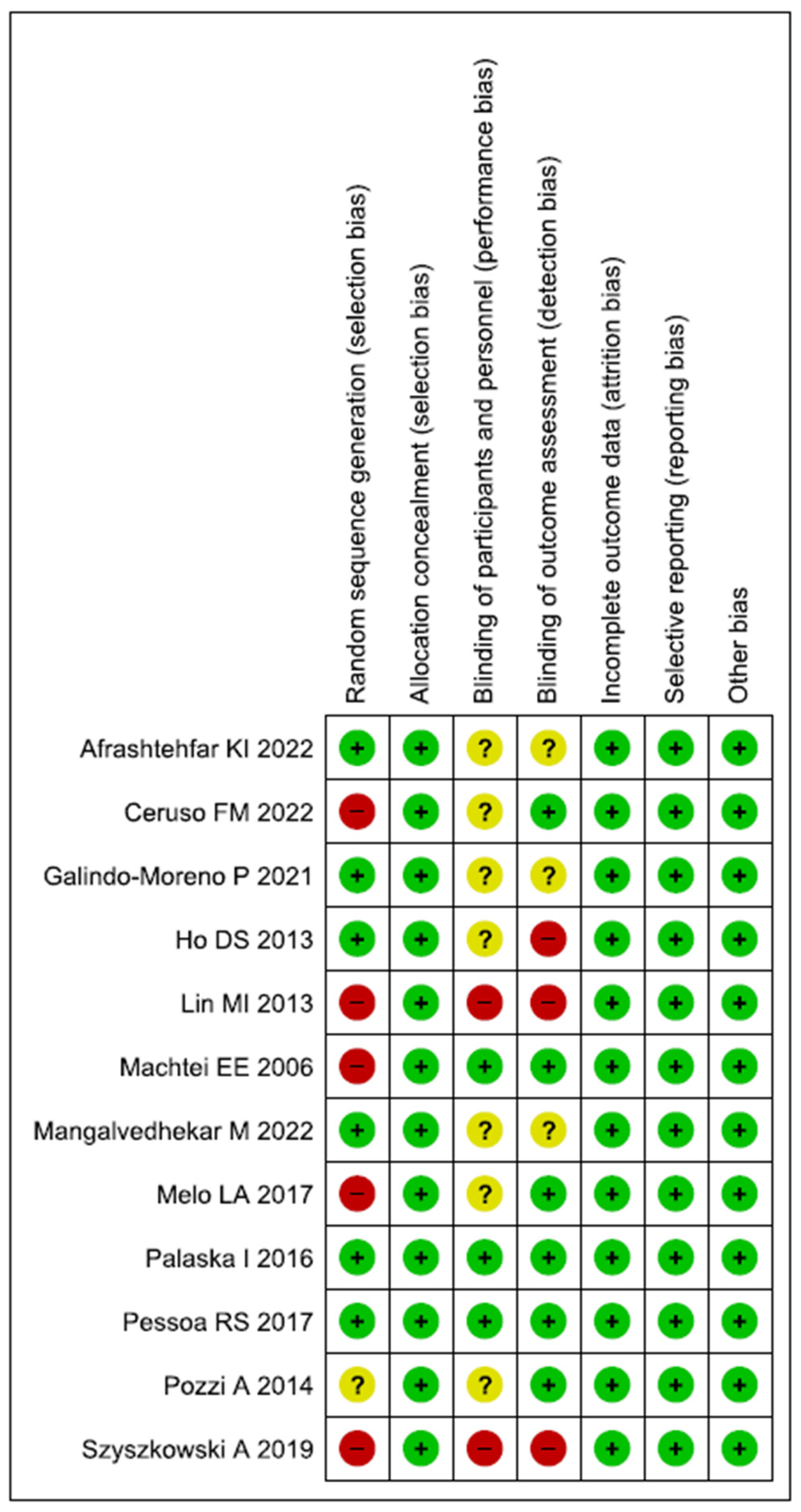
2.4. Risk of Bias Assessment
2.5. Heterogeneity Measurement and Meta-Analysis
3. Results
3.1. Screening Output
3.2. General Characteristics of the Studies Included
3.3. Complications
| Author | Journal | Year | Study Design | Population | Implant | Producer | Cone Morse Angle | Connection | Methods | Prosthetic Complications |
|---|---|---|---|---|---|---|---|---|---|---|
| Canullo L [79] | J. Prosthet. Dent. | 2022 | Retrospective study | 43 participants | 48 implants | Premium Kohno; Sweden & Martina Prama; Sweden & Martina (tissue level) | NA | Cone morse | Clinical and radiographic assessment | __ |
| Degidi M [23] | Int. J. Periodontics Restorative Dent. | 2018 | CT | 76 patients | 156 implants | Ankylos, Dentsply | 5.7° | Cone morse | Clinical and radiographic assessment |
|
| do Vale Souza JP [48] | Eur. J. Dent. | 2021 | CT | 25 patients | 25 implants | DSP Biomedical | NA | Cone morse | Clinical and radiographic assessment Insertion torque—ISQ | __ |
| Hartmann R [139] | J. Oral. Rehabil. | 2020 | RCT | 37 patients | 47 implants | Neodent TI Cortical, Brazil | 11.5° | Conometric | Clinical assessment | __ |
| Sánchez-Torres A [31] | J. Prosthet. Dent. | 2021 | Retrospective study | 56 patients | 288 implants | Replace tapered implants: Nobel Biocare AB Multiunit abutments: Nobel Biocare AB | 6° | Cone morse | Oral Health Impact Profile (OHIP) |
|
| Sato RK [41] | Implant Dent. | 2017 | Cohort prospective study | 16 patients | 16 single implants | Drive cone Morse Acqua, Neodent, Brazil | NA | Cone morse | Clinical and radiographic assessment | __ |
| Abi Rached S [143] | Minerva Dent. Oral. Sci. | 2023 | CT | 7 patients | 18 implants | Straumann® SP cylindrical implants JD Octa® tapered implants | 1:16° 2:15° | Conometric | Clinical and radiographic assessment | |
| Ackermann KL [29] | Int. J. Implant Dent. | 2020 | CT | 94 patients | 130 implants | Conelog Screw-Line; Camlog Biotechnologies | 7.5° | Cone morse |
|
|
| Afrashtehfar KI [75] | Evid Based. Dent. | 2022 | RCT | 24 patients | 48 implants | Conelog, Camlog Biotechnologies, Basel, Switzerland | 7.5° | Cone morse | Clinical and radiographic assessment | __ |
| Al-Fakeh H [92] | J. Stomatol. Oral Maxillofac. Surg. | 2022 | Retrospective study | 65 patients | 102 implants | NA | NA | Cone morse | Clinical and radiographic assessment | __ |
| Apaza-Bedoya K [97] | J Periodontol. | 2023 | Cross-sectional | 99 patients | 266 implants | NA | NA | Cone morse | __ | |
| Baer RA [42] | Clin. Oral. Investig. | 2022 | Cohort prospective study | 67 patients | 81 implants | NA | NA | Cone morse | __ | __ |
| Baldi D [80] | Minerva Stomatol. | 2020 | Retrospective study | __ | 26 implants | NA | NA | Cone morse | __ | |
| Bernard L [70] | J. Prosthet. Dent. | 2019 | RCT | 15 patients | 89 implants | Ankylos; Dentsply Sirona | 5.7° | Cone morse | Clinical and radiographic assessment | __ |
| Cacaci C [45] | Clin. Oral. Investig. | 2019 | CT | 94 patients | 130 implants | Conelog Screw-Line implants; Camlog Biotechnologies AG, Basel, Switzerland | 7.5° | Cone morse | Clinical and radiographic assessment | __ |
| Cannata M [20] | Eur. J. Oral Implantol. | 2017 | RCT | 90 patients | 90 implants | JD Implant, Modena, Italy | 5° | Internal hexagon Cone morse | Clinical and radiographic assessment | Screw loosening (2) [HI group] |
| Canullo L [54] | Clin. Implant Dent. Relat. Res. | 2018 | CT | 22 patients | 22 implants | Premium Kohno, Sweden & Martina, Due Carrare, Padua, Italy | NA | Cone morse | Clinical and radiographic assessment | __ |
| Canullo L [91] | Int. J. Prosthodont. | 2022 | Retrospective study | 85 patients | 133 implants | NA | NA | Cone morse | Clinical and radiographic assessment | __ |
| Cassetta M [34] | J. Oral Sci. | 2016 | Cohort prospective study | 350 patients | 748 implants | NA | NA | Cone morse | __ | 6 were early failures (0.8%) and 28 were late failures (3.7%) |
| Cassetta M [38] | Int. J. Oral. Maxillofac. Surg. | 2016 | CT | 350 patients | 648 implants | NA | NA | Cone morse | Clinical and radiographic assessment | 1 fracture of porcelain surface without metal exposure |
| Cassetta M [34] | J. Oral. Sci. | 2016 | CT | 270 patients | 576 implants | Osseothread; ImplaDent, Formia, Italy | NA | Cone morse | Clinical and radiographic assessment | __ |
| Ceruso FM [133] | Materials | 2022 | CT | 30 patients | 30 Implants | 1: Nobel Parallel, Nobel Biocare, Swiss (12° Conical connection) 2: Prama, Sweden, and Martina, Italy HI | 1: 12° 2:- | Internal hexagon Conometric | Clinical and radiographic assessment | __ |
| Cooper LF [130] | Int. J. Oral Maxillofac. Implants | 2021 | RCT | 141 patients | 141 implants | NA | NA | Conometric Internal hexagon | __ | Six platform-switched interface and eight flat interface implants failed |
| Corvino E [67] | Int. J. Oral. Implantol. (Berl) | 2020 | RCT | 33 patients | 53 implants | NA | NA | Internal hexagon Cone morse | Clinical and radiographic assessment | __ |
| Dagher M. [60] | J. Maxillofac. Oral Surg. | 2022 | CT | 24 patients | 30 implants | UFII, DIOTM, DIO Implant Busan 612–020, Korea | NA | Cone morse | Clinical and radiographic assessment | __ |
| de Melo LA [56] | J. Indian Soc. Periodontol. | 2017 | CT | 23 patients | 46 implants | Neodent, Curitiba, Brazi | 11.5° | External hexagon Cone morse | Clinical and radiographic assessment | __ |
| De Paoli S [62] | Int. J. Periodontics Restorative Dent. | 2023 | CT | 12 patients | 24 implants | NA | NA | Cone morse | __ | __ |
| Degidi M [35] | J. Prosthodont. | 2018 | CT | 65 patients | 134 implants | ANKYLOS; Dentsply Implants, Mannheim, Germany | 5.7° | Cone morse | Clinical and radiographic assessment |
|
| Degidi M [43] | Clin. Oral Implants Res. | 2017 | Cross-sectional | 145 patients | 523 implants | Ankylos®, Dentsply Implants, Mannheim, Germany | 5.7° | Cone morse | Clinical and radiographic assessment | __ |
| Degidi M [61] | Int. J. Periodontics Restorative Dent. | 2016 | CT | 39 patients | 78 implants | Ankylos®, Dentsply Implants, Mannheim, Germany | 5.7° | Cone morse | Clinical and radiographic assessment, ISQ | __ |
| Dev SV [131] | J. Pharm. Bioallied. Sci. | 2021 | CT | 20 patients | 20 implants | NA | NA | Conometric | __ | __ |
| Ding Y [93] | Clin. Implant Dent. Relat. Res. | 2023 | Retrospective study | 33 patients | 218 implants | NA | NA | Cone morse | __ | __ |
| Doornewaard R [64] | Clin. Implant Dent. Relat. Res. | 2021 | RCT | 25 patients | 98 implants | DCC, Southern Implants, Irene, South Africa | NA | Cone morse External hexagon Internal hexagon | Clinical and radiographic assessment | __ |
| Eerdekens L [36] | Clin. Implant Dent. Relat. Res. | 2015 | CT | 10 patients | 60 implants | __ | NA | Cone morse | 2 out of 59 implants failed | |
| Fabbri G [30] | Int. J. Periodontics Restorative Dent. | 2017 | Retrospective study | 601 patients | 965 implants | Nobel Biocare Straumann Biomet 3i | 1:6° 2: 11.5° 3: NA | External hexagon Cone morse Conometric | Clinical assessment | Complication rates of 1.14%, 3.42%, and 0.62% for fractures, chipping, and unscrewing, respectively |
| Farronato D [68] | BMC Oral Health | 2020 | RCT | 104 patients | 188 implants | Group 1: Anyridge®, MegaGen, South Korea Group 2: Core®, Kristal, Italy | 5° | Internal hexagon Cone morse | Clinical, radiographic, and digital assessment | __ |
| Fernández-Figares-Conde I [52] | Dent. J. (Basel) | 2023 | CT | 218 patients | 218 implants | Proclinic S.A.U, Zaragoza, Spain | NA | Cone morse | Clinical and radiographic assessment | __ |
| Galindo-Moreno P [141] | J. Clin. Med. | 2021 | RCT | 30 patients | 30 implants | N35/M12 implant, Oxtein Iberia S.L. | 11° | Conometric | Clinical and radiographic assessment | Ceramic chipping (1) [HI] |
| Gao WM [129] | BMC Oral Health | 2021 | Retrospective study | 392 patients | 541 implants | NA | NA | Conometric | Clinical and radiographic assessment | veneer chipping, with a frequency of 67.53%. The complication-free rate for integrated abutment crowns was significantly greater than for gold porcelain crowns; molar regions were significantly greater than premolar regions, females performed significantly better than males. |
| Ghensi P [44] | J. Craniofac. Surg. | 2019 | Cross-sectional | 120 patients | 261 implants | CLC CONIC | 6° | Cone morse | Clinical and radiographic assessment | __ |
| Guarnieri R [71] | Int. J. Periodontics Restorative Dent. | 2015 | RCT | 77 patients | 78 implants | BioHorizons | NA | Cone morse | Clinical and radiographic assessment | __ |
| Guarnieri R [85] | Implant Dent. | 2014 | Retrospective study | 46 patients | 46 implants | BioHorizons | NA | Cone morse | Clinical and radiographic assessment | __ |
| Hamudi N [53] | J. Clin. Med. | 2021 | CT | 21 patients | 42 implants | NA | NA | Cone morse | Clinical and radiographic assessment | __ |
| Heydecke G [51] | Clin. Oral. Investig. | 2019 | CT | 94 patients | 88 implants | NA | NA | Cone morse | __ | __ |
| Horwitz J [59] | J. Oral. Implantol. | 2018 | CT | 60 patients | 117 implants | Branemark implants | NA | Cone morse | Clinical and radiographic assessment | __ |
| Jin X [28] | Clin. Oral Implants Res. | 2022 | Retrospective study | 6823 patients | 12.538 implants | 1: Straumann Bone Level, Straumann AG (contact angle 7.2°) 2: Ankylos, Dentsply Implants (contact angle 5.7°) | 1: 7.2° 2:5.7° | Cone morse | Clinical and radiographical assessment | Implant fracture (9): 4 Straumann; 5 Dentsply Abutment fracture (28): 14 Straumann; 14 Dentsply |
| Koutouzis T [73] | Int. J. Oral Maxillofac. Implants | 2014 | RCT | 30 patients | 30 implants | ANKYLOS CX, DENTSPLY Implant Manufacturing | 5.7° | Cone morse | Clinical and radiographic assessment | __ |
| Koutouzis T [74] | Int. J. Oral Maxillofac. Implants | 2013 | RCT | 30 patients | 30 implants | Dentsply Ankylos System | 5.7° | Cone morse | Clinical and radiographic assessment | __ |
| Koutouzis T [82] | Int. J. Oral Maxillofac. Implants | 2015 | Retrospective study | 25 patients | 30 implants | Ankylos®, Dentsply Implants, Mannheim, Germany | 5.7° | Cone morse | Clinical and radiographic assessment | __ |
| Kruse AB [78] | Int. J. Implant Dent. | 2021 | Retrospective study | 36 patients | 93 implants | 1. Ankylos© 2. Branemark© 3. ITI Bonefit© | 1:5.7° 2:- 3:- | Cone morse Internal hexagon External hexagon | Clinical and radiographic assessment | __ |
| Lin MI [88] | J. Dent. Res. | 2013 | Retrospective study | 63 patients | 103 implants | 1: Brånemark System TMMK 2: IV TiUnite, Nobel Biocare, Sweden, 3: Atlas, Cowellmedi, South Korea 4: Ankylos Plus Implant, Friadent, Germany | 1: NA 2: NA 3: NA 4: 5.7° | Cone morse | Clinical and radiographical assessment | __ |
| Linkevicius T [138] | Clin. Implant Dent. Relat. Res. | 2021 | RCT | 64 patients | 64 implants | MIS Implant Technologies Ltd., Bar-Lev Industrial Park, Israel | 12° | Conometric | Clinical and radiographic assessment | __ |
| Linkevicius T [98] | Clin. Oral Implants Res. | 2015 | CT | __ | 60 implants | (1) BioHorizons, Birmingham, AL, USA (2) Certain Prevail; Biomet/3i, Palm Beach Gardens, FL, USA | NA | Cone morse | __ | |
| Lopez MA [89] | J. Biol. Regul. Homeost. Agents | 2016 | Retrospective study | 66 patients | 66 implants | FMD Falappa Medical Devices, Italy | NA | Cone morse | Clinical and radiographical assessment | __ |
| Lops D [90] | Materials | 2020 | Retrospective study | 93 patients | 410 implants | Anyridge, MegaGen Implant Co., South Korea | 5° | Cone morse | Clinical and radiographical assessment, marginal bone loss | __ |
| Machtei EE [86] | Clin. Oral Implants Res. | 2006 | Retrospective study | 27 patients | 73 implants | Osseotite/Osseotite TG (3I Implant Innovations Inc., USA) | 8° | External hexagon Cone morse | Clinical and radiographical assessmentMarginal bone loss | __ |
| Mangalvedhekar M [120] | J. Pharm. Bioallied. Sci. | 2022 | CT | 50 patients | __ | Nobel Biocare | 12° | Conometric External hexagon | Clinical and radiographical assessment | __ |
| Mangano C [94] | Clin. Oral Implants Res. | 2015 | Retrospective study | 49 patients | 178 implants | Mac System, Milan, Italy | NA | Cone morse | Clinical and radiographic assessment | Prosthetic complications (10.3%) |
| Mangano F [24] | Int. J. Environ. Res. Public Health | 2019 | Retrospective study | 25 Patients | 40 implant | Exacone®, Leone Implants, Florence, Italy | NA | Cone morse | Full-digital Protocol (SCAN-PLAN-MAKE-DONE®) | Occlusal issues (2/40 crowns: 5%), interproximal issues (1/40 crowns: 2.5%), and aesthetic issues (1/40 crowns: 2.5%). Overall incidence of issues at delivery of 10% (4/40 crowns). |
| Mangano F [55] | J. Craniofac. Surg. | 2018 | CT | 578 patients | 612 implants | Leone Implants, Florence, Italy | NA | Cone morse | Clinical and radiographic assessment | __ |
| McGuire MK [72] | Int. J. Periodontics Restorative Dent. | 2015 | RCT | 12 patients | 12 implants | (1) OsseoSpeed, Dentsply Implants (2) NobelSpeedy Replace, Nobel Biocare (3) NanoTite Certain Prevail, Biomet 3i | 1: NA 2: NA 3: NA | Cone morse | Clinical and radiographic assessment | __ |
| Melo LA [57] | Braz. Dent. J. | 2017 | CT | 20 patients | 40 implants | Neodent | 11.5° | External hexagon Cone morse | Clinical and radiographic assessment | __ |
| Meloni SM [76] | Dent. J. (Basel) | 2020 | Retrospective study | 82 patients | 152 implants | NobelReplace CC PMC or NobelReplace Tapered Groovy | 6° | Cone morse | Clinical and radiographic assessment | __ |
| Mihali SG [136] | J. Oral Implantol. | 2021 | RCT | 49 patient | 98 implants | Mis Implant System | 12° | Conometric | Clinical and radiographical assessment | __ |
| Moergel M [22] | Clin. Oral Implants Res. | 2021 | CT | 24 patients | 52 implants | Conelog Screw-Line; Camlog Biotechnologies | 7.5° | Cone morse | Clinical and radiographical assessment, marginal bone loss | Screw fracture (1) |
| Moroi A [69] | Clin. Implant Dent. Relat. Res. | 2020 | RCT | 43 patients | 88 implants | Nobel Biocare, Sweden | 6° | Cone morse | Clinical and radiographic assessment ISQ | __ |
| Naumann M [37] | Clin. Oral Implants Res. | 2023 | RCT | 20 patients | - | NA | NA | Cone morse | 1 restoration failed after 6 months due to the loss of the abutment interface. | |
| Obreja K [25] | Int. J. Periodontics Restorative Dent. | 2022 | Cross-sectional | 44 patients | 57 implants | NA | Cone morse | Clinical and radiographical assessment | None | |
| Oda Y [39] | Clin. Oral Implants Res. | 2021 | Retrospective study | 65 patients | 592 implants | 1: Brånemark system implant 2: Ankylos implant 3: Straumann system tissue-level implant—Zimmer screw-vent | 1: NA 2: 5.7° 3: 7.2° | Internal hexagon External hexagon Cone morse | Clinical and radiographical assessment Marginal bone loss | __ |
| Ogino Y [66] | Int. J. Oral Maxillofac. Implants | 2021 | RCT | 25 patients | 30 implants | GC Aadva implants | NA | Cone morse | Clinical and radiographical assessment, marginal bone loss | __ |
| Paganelli OEB [132] | Gen. Dent. | 2022 | CT | 9 patients | 36 implants | NA | NA | Conometric External hexagon | Clinical evaluation via magnetic transduction resonance frequency analysis | __ |
| Palaska I [148] | Clin. Oral Implants Res. | 2016 | RCT | 81 patients | 105 implants | 1: Osseospeed, Astratech Dental, Sweden 2. Prevail, Biomet 3i, USA | 1: 6° 2:- | Internal polygonal butt-joint Cone morse | Clinical and radiographical assessment Marginal bone loss | __ |
| Pariente L. [150] | J. Oral Implantol. | 2020 | CT | 33 patients | 50 implants | NA | NA | Conometric | Clinical and radiographic assessment | __ |
| Park H [77] | J. Periodontal Implant Sci. | 2021 | Retrospective study | 12 patients | 24 implants | NA | NA | Cone morse | Clinical and radiographic assessment | __ |
| Penitente PA [102] | Clin. Ter. | 2023 | Retrospective study | 319 patients | 1227 implants | NA | NA | External hexagon Cone morse | Clinical and radiographic assessment | |
| Pessoa RS [140] | Clin. Implant Dent. Relat. Res. | 2017 | RCT | 12 patients | 48 implants | UNITITEVR, SIN—Sistema de Implante, Sao Paulo, Brazil | 16° | External hexagon Conometric | Clinical and radiographic assessment | __ |
| Pieri F [65] | Int. J. Oral Maxillofac. Implants | 2011 | RCT | 40 patients | 40 implants | __ | NA | Internal hexagon Cone morse | Clinical and radiographical assessmentMarginal bone loss | __ |
| Radaelli MTB [135] | J. Periodontal Res. | 2020 | CT | 33 patients | 109 implants | Neodent, Curitiba, PR, Brazil | 11.5° | Conometric | Clinical and radiographic assessment | __ |
| Raj HK [134] | J. Contemp. Dent. Pract. | 2022 | CT | 20 patients | 20 implants | Nobel Biocare | 12° | Conometric | Clinical and radiographical assessment | __ |
| Romanos G [83] | Clin. Implant Dent. Relat. Res. | 2016 | Retrospective study | 247 patients | 634 implants | Ankylos®, Dentsply Implants, Mannheim, Germany | 5.7° | Cone morse | Clinical and radiographic assessment | __ |
| Romanos GE [87] | Int. J. Oral Maxillofac. Implants | 2011 | Retrospective study | 122 patients | 488 implants | __ | NA | Cone morse | __ | |
| Saglanmak A [101] | Quintessence Int. | 2021 | Retrospective study | __ | 44 implants | NA | NA | Cone morse | Clinical and radiographic assessment | |
| Scarano A [63] | J. Periodontol. | 2016 | CT | 15 patients | 37 implants | NA | NA | Cone morse Internal hexagon | __ | __ |
| Sharma V [26] | J. Indian. Prosthodont. Soc. | 2022 | CT | 10 patients | 20 implants | NA | NA | Cone morse | Clinical and radiographical assessment | none |
| Simonpieri A [84] | Quintessence Int. | 2017 | Retrospective study | 42 patients | 334 implants | In-Kone Universal System, Global D | 8° | Cone morse | Clinical and radiographic assessment | __ |
| Smojver I [47] | Int. J. Mol. Sci. | 2022 | CT | __ | 100 implants | NA | NA | Cone morse | Clinical and radiographic assessment | __ |
| Spinelli A [40] | Materials (Basel) | 2023 | Cohort prospective study | 36 patients | 41 implants | Tapered Tissue-level Laser-Lok, Biohorizons, Birmingham, AL, USA | NA | Cone morse | Clinical and radiographical assessment | __ |
| Stacchi C [137] | Clin. Implant Dent. Relat. Res. | 2023 | RCT | 102 implants | 51 patients | NA | NA | Conometric | Clinical and radiographical assessment | __ |
| Studenikin R [142] | Int. J. Dent. | 2021 | CT | 15 patients | 15 implants | Nobel Biocare | 12° | Conometric | ||
| Sun Y [100] | Clin. Implant Dent. Relat. Res. | 2023 | RCT | 19 patients | 42 implants | NA | NA | Cone morse | Clinical and radiographic assessment | |
| Szyszkowski A [58] | Implant Dent. | 2019 | CT | 214 patients | 540 implants | (a) Alpha-Bio Tec, Petach Tikwa, Israel (b) MIS Implant Technologies, Shlomi, Israel | 1: NA 2: 12° | Conometric Internal hexagon | Clinical and radiographic assessment | __ |
| Tallarico M [96] | Eur. J. Dent. | 2022 | Cohort prospective study | 90 patients | 243 implants | Osstem TSIII, Osstem Implant Co. Ltd., Seoul, South Korea | NA | Cone morse | Clinical and radiographic assessment | Four prostheses failed |
| Tetè G [49] | J. Biol. Regul. Homeost. Agents | 2020 | CT | __ | - | NA | NA | Cone morse | Clinical and radiographic assessment | __ |
| Thomé G [81] | Int. J. Oral. Maxillofac. Implants | 2020 | Retrospective study | 101 patients | 453 implants | Helix Acqua GM, Neodent | NA | Cone morse | Clinical and radiographic assessment | __ |
| Toia M [116] | Clin. Oral Implants Res. | 2022 | RCT | 50 patients | 119 implants | OsseoSpeed Astra Tech Implant System | 1: 6° | Cone morse | Clinical and radiographic assessment | (a) Screw loosening (2): [abutment level group (AL) (1); implant level group (IG) (1)] (b) Screw fracture (2): [abutment level group (AL)] |
| van Hooft J [46] | J. Clin. Med. | 2022 | CT | 16 patients | 23 implants | NA | NA | Cone morse | Clinical and radiographic assessment | __ |
| Vervaeke S [50] | J. Clin. Periodontol. | 2018 | CT | 25 patients | 52 implants | Astra Tech Osseospeed TX™, Denstply implants, USA | NA | Cone morse | Clinical and radiographic assessment | __ |
| Weigl P [99] | J. Prosthet. Dent. | 2019 | CT | 23 patients | 91 implants | Ankylos | 5.7° | Cone morse | ||
| Yamada S [27] | Int. J. Implant Dent. | 2023 | CT | 31 patients | 45 implants | 1: NobelActive®/NobelReplace Tapered 2: CC®, Nobel Biocare, Gothenberg, Sweden, 3: Bone Level Implant®/Bone Level Tapered Implant®, Straumann, Basel, Switzerland | 1: 6° 2: 11° 3: 15° | Cone morse Conometric | Clinical and radiographic assessment | none |
| Yang F [32] | Clin. Implant Dent. Relat. Res. | 2022 | Retrospective study | 495 patients | 945 implants | Ankylos; Dentsply Sirona | 5.7° | Cone morse | Clinical and radiographic assessment | Abutment fracture (AF) (13) Abutment screw loosening (ASL) (12) |
| Yi Y [21] | J. Prosthet. Dent. | 2023 | Retrospective study | 428 patients | 898 implants | One-plant FIT; Warantec | 1.5° | Cone morse | Clinical and radiographic assessment | Screw fractures (23) Screw loosening (417) Abutment fracture (102) Implant fracture (31) |
| Frisch E [103] | Clin. Implant. Dent. Relat. Res. | 2015 | Retrospective study | 20 patients | 80 implants | Ankylos, Dentsply Friadent, Mannheim, Germany) | 5.7° | Cone morse | Clinical and radiographic assessment | __ |
| Ho DS [104] | Clin. Oral. Implants Res. | 2013 | RCT | 32 subjects | 64 implants | Test: NobelActive™ Control: Brånemark | 1: 6° 2:NA | Cone morse | Clinical and radiographic assessment | __ |
| Mangano F [105] | Clin. Oral Implants Res. | 2012 | Retrospective study | 26 patients | 26 implants | Leone Implant System(R), Florence, Italy | NA | Cone morse | Clinical and radiographic assessment | __ |
| Bae MS [144] | Implant Dent. | 2011 | Retrospective study | 92 patients | 294 implants | MIS Implants Technologies Ltd., Shlomi, Israel | 12° | Conometric | Clinical and radiographic assessment | |
| Mangano C [106] | Clin. Oral Implants Res. | 2011 | CT | 60 patients | 288 implants | Leone Implant System (®) | NA | Cone morse | Clinical and radiographic assessment | __ |
| Mangano C [107] | J. Periodontal. | 2011 | CT | 893 patients | 2.549 implants | NA | NA | Cone morse | Clinical and radiographic assessment | Few prosthetic complications at the implant–abutment interface reported (0.37%) |
| Moberg LE [108] | Clin. Oral Implants Res. | 1999 | CT | 29 patients | 30 implants | ITI implant system | NA | Cone morse Internal octagonal butt-joint | Clinical and radiographic assessment | __ |
| Palmer RM [145] | Clin. Oral Implants Res. | 1997 | CT | 15 patients | 15 implants | AstraTech, Molndal Sweden | 1: 11.2° | Conometric | Clinical and radiographic assessment |
|
| Levine RA [109] | Int. J. Oral Maxillofac. Implants | 1997 | CT | 129 patients | 174 implants | ITI implant system | NA | Cone morse | Clinical and radiographic assessment |
|
| Chapman RJ [110] | Implant Dent. | 1996 | CT | __ | 1.757 implants | NA | NA | Cone morse | __ | 9 abutment posts fractured for a failure rate of 0.05%. 31 (1.7%) abutments loosened. |
| Morris HF [111] | J. Oral. Implantol. | 2001 | CT | 313 patients | 1.419 implants | Ankylos Implant | 5.7° | Cone morse | Clinical and radiographic assessment | __ |
| Mangano C [112] | Int. J. Oral Maxillofac. Implants | 2001 | Retrospective study | 69 patients | 80 implants | Mac System, Cabon, Milan, Italy | NA | Cone morse | Clinical and radiographic assessment | 2 fractured abutments and 1 loosened abutment |
| Gatti C [113] | Clin. Implant Dent. Relat. Res. | 2002 | CT | 10 patients | 40 implants | Brånemark implants (MK II; Nobel Biocare AB, Gothenburg, Sweden) Nobel Biocare AB | NA | Cone morse | __ | __ |
| Kronström M [114] | J. Prosthet. Dent. | 2003 | CT | 17 patients | 68 implants | Brånemark implants | NA | Cone Morse | ||
| Chou CT [115] | J. Oral Implantol. | 2004 | CT | __ | 1500 implants | Ankylos Implant | 5.7° | Cone morse | Clinical and radiographic assessment | __ |
| Toia M. [116] | Clin. Oral Implants Res. | 2023 | RCT | 50 patients | 119 implants | NA | NA | Cone morse | Clinical and radiographic assessment | __ |
| Galindo-Moreno P [117] | J. Clin. Med. | 2023 | Retrospective study | - | - | NA | NA | |||
| Gehrke SA [118] | Medicina (Kaunas) | 2023 | Retrospective study | 79 patients | 120 implants | NA | NA | Cone morse | C. group: fractured abutments (5%), no abutment loosening T. group: no abutment fracture, loosening screws (11.3%) | |
| Gehrke SA [95] | J. Funct. Biomater. | 2023 | Retrospective study | 65 patients | 26 implants | NA | NA | Cone morse | One patient failed due to an abutment fracture after 25 months of function | |
| Lops D. [119] | J. Clin. Med. | 2022 | Retrospective study | 80 patients | 312 implants | Anyridge; MegaGen Implant | 5° | Cone morse | Clinical and radiographic assessment | - |
| Galindo-Moreno P [149] | Clin. Oral Implants Res. | 2022 | Retrospective study | 19 patients | 160 implants | OsseoSpeed Astra Tech TX implants | 6° | Cone morse | Clinical and radiographic assessment | 14 implants > 2 mm of MBL (8.75%) |
| Mangalvedhekar M [120] | J. Pharm. Bioallied. Sci. | 2022 | CT | 50 patients | 50 implants | 1: Nobel Biocare 2: Nobel Biocare | 1: 6° 2: NA | Cone morse External hexagon (EH) | Clinical and radiographic assessment | __ |
| Pozzi A [146] | Int. J. Periodontics Restorative Dent. | 2021 | Retrospective study | 281 patients | 686 implants | NA | NA | Conometric | __ | |
| Eskan MA [147] | Int. J. Implant Dent. | 2020 | Retrospective study | 42 patients | 171 implants | Straumann | 11.5° | Conometric | Clinical and radiographic assessment | __ |
| Friberg B [121] | Clin. Implant Dent. Relat. Res. | 2019 | CT | 47 patients | 51 implants | NobelParallel CC | 6° | Cone morse | Clinical and radiographic assessment | __ |
| Mundt T [122] | Int. J. Oral Maxillofac. Implants | 2006 | Retrospective study | 159 patients | 663 implants | 1:Ankylos Implant 2: Branemark Systems 3: NP MkIII Ti Unite 4: Frialit CELLplust 5: Replaces 6: Select Tapered Ti Unite 7: XiVE S CELL 8: Osseotite XPt 9: Straumann | 1: 5.7° 2: NA 3: NA 4: NA 5: 6° 6:6° 7: NA 8: 11.5° | Cone morse Conometric Internal hexagonal External hexagonal | Clinical and radiographic assessment | __ |
| Mangano C [123] | Eur. J. Oral Implantol. | 2008 | CT | 302 patients | 314 implants | NA | NA | Cone morse | Clinical and radiographic assessment | 0.6% implant–abutment loosening rate |
| Mangano C [124] | Clin. Oral Implants Res. | 2009 | CT | 689 patients | 1920 implants | Leone Implant System, Florence, Italy | NA | Cone morse | Clinical and radiographic assessment | 0.65% rate of loosening at the implant–abutment interface |
| Mangano C [125] | Int. J. Oral. Maxillofac. Implants | 2010 | CT | 295 patients | 307 implants | NA | NA | Cone morse | Clinical and radiographic assessment | __ |
| Gultekin BA [126] | Int. J. Oral Maxillofac. Implants | 2013 | CT | 25 patients | 93 implants | Ti UNITE, Nobel Biocare | 6° | Cone morse | Clinical and radiographic assessment | __ |
| Pozzi A [127] | Clin. Implant Dent. Relat. Res. | 2014 | RCT | 34 patients | 68 implants | 1: NobelActive, Nobel Biocare AB, Göteborg, Sweden 2: Nobel Speedy Groovy, Nobel Biocare AB, Sweden | 1: 6° 2: 6° | External hexagon Cone morse | Clinical and radiographic assessment | __ |
| Pozzi A [128] | Eur. J. Oral Implantol. | 2015 | CT | 54 patients | 118 implants | Nobel Replace Conical Connection implants, Nobel Biocare, Swiss | 6° | Cone morse | Clinical and radiographic assessment | Crown failure (1) |
3.4. Risk of Bias Assessment (RoB)
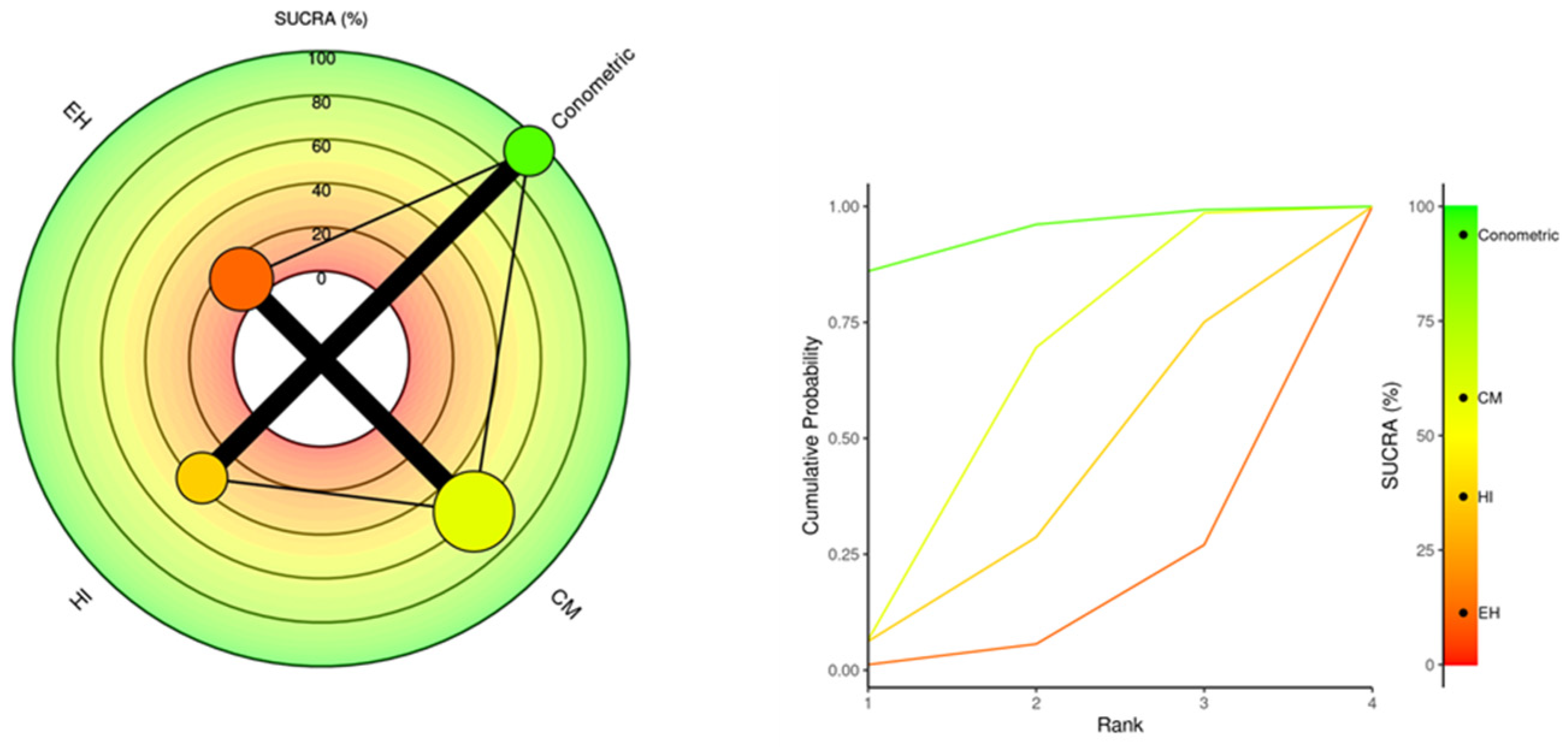
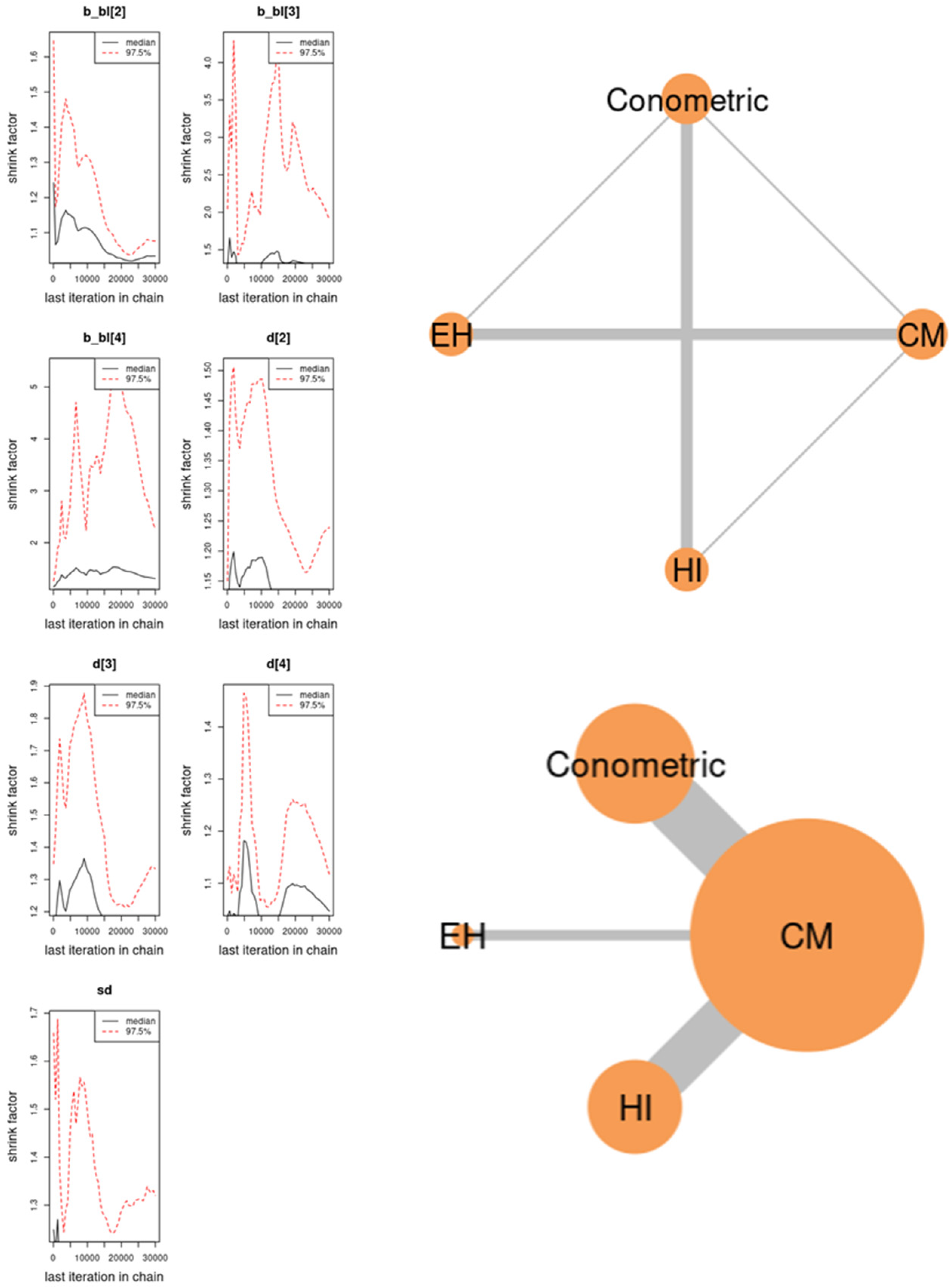
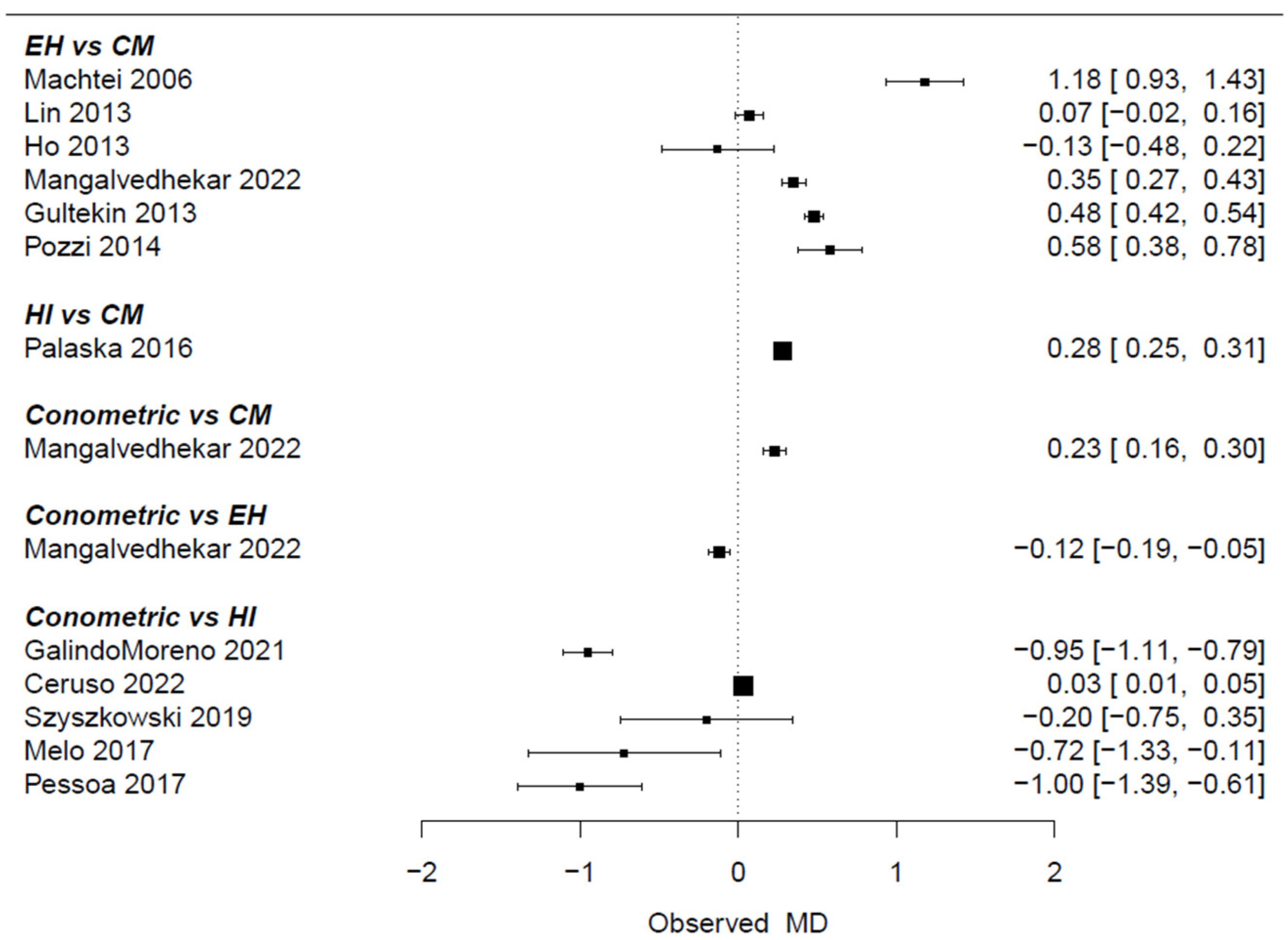
3.5. Meta-Analysis
3.6. Meta-Regression MBL
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Albrektsson, T.; Zarb, G.; Worthington, P.; Eriksson, A.R. The Long-Term Efficacy of Currently Used Dental Implants: A Review and Proposed Criteria of Success. Int. J. Oral Maxillofac. Implants 1986, 1, 11–25. [Google Scholar] [PubMed]
- Hamada, Y.; Shin, D.; John, V. Peri-Implant Disease—A Significant Complication of Dental Implant Supported Restorative Treatment. J. Indiana Dent. Assoc. 2016, 95, 31–38. [Google Scholar] [PubMed]
- Koutouzis, T. Implant-abutment Connection as Contributing Factor to Peri-implant Diseases. Periodontol. 2000 2019, 81, 152–166. [Google Scholar] [CrossRef] [PubMed]
- Comuzzi, L.; Tumedei, M.; Romasco, T.; Petrini, M.; Afrashtehfar, K.I.; Inchingolo, F.; Piattelli, A.; Di Pietro, N. Insertion Torque, Removal Torque, and Resonance Frequency Analysis Values of Ultrashort, Short, and Standard Dental Implants: An In Vitro Study on Polyurethane Foam Sheets. J. Funct. Biomater. 2023, 14, 10. [Google Scholar] [CrossRef]
- King, G.N.; Hermann, J.S.; Schoolfield, J.D.; Buser, D.; Cochran, D.L. Influence of the Size of the Microgap on Crestal Bone Levels in Non-Submerged Dental Implants: A Radiographic Study in the Canine Mandible. J. Periodontol. 2002, 73, 1111–1117. [Google Scholar] [CrossRef]
- Daher, F.I.; Abi-Aad, H.L.; Dimassi, H.I.; Cordioli, G.; Majzoub, Z.A.K. Immediate versus Conventional Loading of Variable-Thread Tapered Implants Supporting Three- to Four-Unit Fixed Partial Dentures in the Posterior Maxilla: 3-Year Results of a Split-Mouth Randomised Controlled Trial. Int. J. Oral Implantol. 2019, 12, 449–466. [Google Scholar]
- Bernardes, S.R.; da Gloria Chiarello de Mattos, M.; Hobkirk, J.; Ribeiro, R.F. Loss of Preload in Screwed Implant Joints as a Function of Time and Tightening/Untightening Sequences. Int. J. Oral Maxillofac. Implants 2014, 29, 89–96. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, J. Influences of Microgap and Micromotion of Implant–Abutment Interface on Marginal Bone Loss around Implant Neck. Arch. Oral Biol. 2017, 83, 153–160. [Google Scholar] [CrossRef]
- Romeo, E.; Ghisolfi, M.; Murgolo, N.; Chiapasco, M.; Lops, D.; Vogel, G. Therapy of Peri-Implantitis with Resective Surgery: A 3-Year Clinical Trial on Rough Screw-Shaped Oral Implants. Part I: Clinical Outcome. Clin. Oral Implants Res. 2004, 16, 9–18. [Google Scholar] [CrossRef]
- Kim, D.-H.; Kim, H.J.; Kim, S.; Koo, K.-T.; Kim, T.-I.; Seol, Y.-J.; Lee, Y.-M.; Ku, Y.; Rhyu, I.-C. Comparison of Marginal Bone Loss between Internal- and External-Connection Dental Implants in Posterior Areas without Periodontal or Peri-Implant Disease. J. Periodontal Implant Sci. 2018, 48, 103–113. [Google Scholar] [CrossRef]
- Ellakany, P.; Mahrous, A.; Eraky, D.; Albarrak, A.; AlJindan, R.; Fouda, S. Evaluation of Bacterial Leakage in Platform-Switching Dental Implant with Morse Taper Connection Under Thermocycling and Loading Effects: In Vitro Study. Int. J. Oral Maxillofac. Implants 2021, 36, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Assenza, B.; Tripodi, D.; Scarano, A.; Perrotti, V.; Piattelli, A.; Iezzi, G.; D’Ercole, S. Bacterial Leakage in Implants with Different Implant-Abutment Connections: An in Vitro Study. J. Periodontol. 2012, 83, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, P.F.; Grenho, L.; Fernandes, M.H.; Sampaio-Fernandes, J.C.; Gomes, P.S. Microgap and Bacterial Microleakage during the Osseointegration Period: An in Vitro Assessment of the Cover Screw and Healing Abutment in a Platform-Switched Implant System. J. Prosthet. Dent. 2023, 130, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Larrucea, C.; Conrado, A.; Olivares, D.; Padilla, C.; Barrera, A.; Lobos, O. Bacterial Microleakage at the Abutment-Implant Interface, in Vitro Study. Clin. Implant Dent. Relat. Res. 2018, 20, 360–367. [Google Scholar] [CrossRef]
- Sahin, C.; Ayyildiz, S. Correlation between Microleakage and Screw Loosening at Implant-Abutment Connection. J. Adv. Prosthodont. 2014, 6, 35. [Google Scholar] [CrossRef]
- Norton, M.R. An in Vitro Evaluation of the Strength of an Internal Conical Interface Compared to a Butt Joint Interface in Implant Design. Clin. Oral Implants Res. 1997, 8, 290–298. [Google Scholar] [CrossRef]
- Ohat, N. Handbook for Conducting a Literature-Based Health Assessment Using OHAT Approach for Systematic Review and Evidence Integration; US Department of Health and Human Services: Washington, DC, USA, 2019. [Google Scholar]
- Owen, R.K.; Bradbury, N.; Xin, Y.; Cooper, N.; Sutton, A. MetaInsight: An Interactive Web-Based Tool for Analyzing, Interrogating, and Visualizing Network Meta-Analyses Using R-Shiny and Netmeta. Res. Synth. Methods 2019, 10, 569–581. [Google Scholar] [CrossRef]
- Hutton, B.; Salanti, G.; Caldwell, D.M.; Chaimani, A.; Schmid, C.H.; Cameron, C.; Ioannidis, J.P.A.; Straus, S.; Thorlund, K.; Jansen, J.P.; et al. The PRISMA Extension Statement for Reporting of Systematic Reviews Incorporating Network Meta-Analyses of Health Care Interventions: Checklist and Explanations. Ann. Intern. Med. 2015, 162, 777–784. [Google Scholar] [CrossRef]
- Cannata, M.; Grandi, T.; Samarani, R.; Svezia, L.; Grandi, G. A Comparison of Two Implants with Conical vs. Internal Hex Connections: 1-Year Post-Loading Results from a Multicentre, Randomised Controlled Trial. Eur. J. Oral Implantol. 2017, 10, 161–168. [Google Scholar]
- Yi, Y.; Heo, S.J.; Koak, J.Y.; Kim, S.K. Mechanical Complications of Implant-Supported Restorations with Internal Conical Connection Implants: A 14-Year Retrospective Study. J. Prosthet. Dent. 2023, 129, 732–740. [Google Scholar] [CrossRef]
- Moergel, M.; Rocha, S.; Messias, A.; Nicolau, P.; Guerra, F.; Wagner, W. Clinical and Radiographic Performance of Self-Locking Conical Connection Implants in the Posterior Mandible: Five-Year Results of a Two-Centre Prospective Study. Clin. Oral Implants Res. 2021, 32, 998–1007. [Google Scholar] [CrossRef] [PubMed]
- Degidi, M.; Nardi, D.; Gianluca, S.; Piattelli, A. The Conometric Concept: A 5-Year Follow-up of Fixed Partial Monolithic Zirconia Restorations Supported by Cone-in-Cone Abutments. Int. J. Periodontics Restor. Dent. 2018, 38, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.; Margiani, B.; Admakin, O. A Novel Full-Digital Protocol (SCAN-PLAN-MAKE-DONE(®)) for the Design and Fabrication of Implant-Supported Monolithic Translucent Zirconia Crowns Cemented on Customized Hybrid Abutments: A Retrospective Clinical Study on 25 Patients. Int. J. Environ. Res. Public Health 2019, 16, 317. [Google Scholar] [CrossRef] [PubMed]
- Obreja, K.; Begić, A.; Trimpou, G.; Galarraga-Vinueza, M.E.; Balaban, Ü.; Schwarz, F.; Parvini, P. Clinical and Esthetic Evaluation Following Immediate Implant Placement and Restoration with Platform- Switched Morse Taper Implants in the Esthetic Zone: A Cross-Sectional Study. Int. J. Periodontics Restor. Dent. 2022, 42, 665–673. [Google Scholar] [CrossRef]
- Sharma, V.; Paliwal, J.; Bhansali, S.; Meena, K.K.; Gupta, N.; Dadarwal, A. Evaluation of Clinical and Radiographic Outcome of Friction Fit Conical Abutment System in Implant-Supported Dental Prostheses: An in Vivo Study. J. Indian Prosthodont. Soc. 2022, 22, 29–37. [Google Scholar] [CrossRef]
- Yamada, S.; Nakano, T.; Kobayashi, T.; Ishigaki, S. Maxillary Labial Peri-Implant Hard and Soft Tissue Alteration Observed on Cross-Sectional Dimension: A 2-Year Prospective Observational Study. Int. J. Implant Dent. 2023, 9, 16. [Google Scholar] [CrossRef]
- Jin, X.; Guan, Y.; Ren, J.; Zhao, Y.; Wang, X.; He, F. A Retrospective Study of 12,538 Internal Conical Connection Implants Focused on the Long-Term Integrity of Implant-Abutment Complexes. Clin. Oral Implants Res. 2022, 33, 377–390. [Google Scholar] [CrossRef]
- Ackermann, K.-L.; Barth, T.; Cacaci, C.; Kistler, S.; Schlee, M.; Stiller, M. Clinical and Patient-Reported Outcome of Implant Restorations with Internal Conical Connection in Daily Dental Practices: Prospective Observational Multicenter Trial with up to 7-Year Follow-Up. Int. J. Implant Dent. 2020, 6, 14. [Google Scholar] [CrossRef]
- Fabbri, G.; Fradeani, M.; Dellificorelli, G.; De Lorenzi, M.; Zarone, F.; Sorrentino, R. Clinical Evaluation of the Influence of Connection Type and Restoration Height on the Reliability of Zirconia Abutments: A Retrospective Study on 965 Abutments with a Mean 6-Year Follow-Up. Int. J. Periodontics Restor. Dent. 2017, 37, 19–31. [Google Scholar] [CrossRef]
- Sánchez-Torres, A.; Cercadillo-Ibarguren, I.; Figueiredo, R.; Gay-Escoda, C.; Valmaseda-Castellón, E. Mechanical Complications of Implant-Supported Complete-Arch Restorations and Impact on Patient Quality of Life: A Retrospective Cohort Study. J. Prosthet. Dent. 2021, 125, 279–286. [Google Scholar] [CrossRef]
- Yang, F.; Ruan, Y.; Liu, Y.; Chen, J.; Chen, Y.; Zhang, W.; Ding, Y.; Wang, L. Abutment Mechanical Complications of a Morse Taper Connection Implant System: A 1- to 9-Year Retrospective Study. Clin. Implant Dent. Relat. Res. 2022, 24, 683–695. [Google Scholar] [CrossRef] [PubMed]
- Toia, M.; Stocchero, M.; Galli, S.; Papia, E.; Wennerberg, A.; Becktor, J.P. The Use of Implant-Level Connection in Screw-Retained Fixed Partial Dentures: A 3-Year Randomised Clinical Trial. Clin. Oral Implants Res. 2022, 33, 78–93. [Google Scholar] [CrossRef] [PubMed]
- Cassetta, M.; Di Mambro, A.; Giansanti, M.; Brandetti, G.; Calasso, S. A 36-Month Follow-up Prospective Cohort Study on Peri-Implant Bone Loss of Morse Taper Connection Implants with Platform Switching. J. Oral Sci. 2016, 58, 49–57. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Degidi, M.; Nardi, D.; Sighinolfi, G.; Piattelli, A. The Conometric Concept: Definitive Fixed Lithium Disilicate Restorations Supported by Conical Abutments. J. Prosthodont. 2018, 27, 605–610. [Google Scholar] [CrossRef]
- Eerdekens, L.; Schols, M.; Coelst, L.; Quirynen, M.; Naert, I. A 5-Year Prospective Study on Cone-Anchored Implants in the Edentulous Maxilla. Clin. Implant Dent. Relat. Res. 2015, 17 (Suppl. S2), e621–e632. [Google Scholar] [CrossRef]
- Naumann, M.; Scholz, P.; Krois, J.; Schwendicke, F.; Sterzenbach, G.; Happe, A. Monolithic Hybrid Abutment Crowns (Screw-Retained) versus Monolithic Hybrid Abutments with Adhesively Cemented Monolithic Crowns. Clin. Oral Implants Res. 2023, 34, 209–220. [Google Scholar] [CrossRef]
- Cassetta, M.; Driver, A.; Brandetti, G.; Calasso, S. Peri-Implant Bone Loss around Platform-Switched Morse Taper Connection Implants: A Prospective 60-Month Follow-up Study. Int. J. Oral Maxillofac. Surg. 2016, 45, 1577–1585. [Google Scholar] [CrossRef]
- Oda, Y.; Mori, G.; Honma, S.; Ito, T.; Iijima, T.; Yajima, Y. Marginal Bone Loss and the Risk Indicators of Fixed Screw-Retained Implant-Supported Prostheses and Fixed Telescopic-Retained Implant-Supported Prostheses in Full Arch: A Retrospective Case-Control Study. Clin. Oral Implants Res. 2021, 32, 818–827. [Google Scholar] [CrossRef]
- Spinelli, A.; Zamparini, F.; Romanos, G.; Gandolfi, M.G.; Prati, C. Tissue-Level Laser-Lok Implants Placed with a Flapless Technique: A 4-Year Clinical Study. Materials 2023, 16, 1293. [Google Scholar] [CrossRef]
- Sato, R.K.; Thomé, G.; Fontão, F.N.G.K.; de Melo Filho, A.; Melo, A.C.M. Morse Taper Implants Immediately Loaded in Fresh Extraction Sockets: A Prospective Cohort Study. Implant Dent. 2017, 26, 345–350. [Google Scholar] [CrossRef]
- Baer, R.A.; Nölken, R.; Colic, S.; Heydecke, G.; Mirzakhanian, C.; Behneke, A.; Behneke, N.; Gottesman, E.; Ottria, L.; Pozzi, A.; et al. Immediately Provisionalized Tapered Conical Connection Implants for Single-Tooth Restorations in the Maxillary Esthetic Zone: A 5-Year Prospective Single-Cohort Multicenter Analysis. Clin. Oral Investig. 2022, 26, 3593–3604. [Google Scholar] [CrossRef] [PubMed]
- Degidi, M.; Daprile, G.; Piattelli, A. Marginal Bone Loss around Implants with Platform-Switched Morse-Cone Connection: A Radiographic Cross-Sectional Study. Clin. Oral Implants Res. 2017, 28, 1108–1112. [Google Scholar] [CrossRef] [PubMed]
- Ghensi, P.; Tonetto, G.; Soldini, C.; Bettio, E.; Mortellaro, C.; Soldini, C. Dental Implants With a Platform-Switched Morse Taper Connection and an Osteo Growth Induction Surface. J. Craniofacial Surg. 2019, 30, 1049–1054. [Google Scholar] [CrossRef] [PubMed]
- Cacaci, C.; Ackermann, K.-L.; Barth, T.; Kistler, S.; Stiller, M.; Schlee, M. A Non-Interventional Multicenter Study to Document the Implants Success and Survival Rates in Daily Dental Practices of the CONELOG Screw-Line Implant. Clin. Oral Investig. 2019, 23, 2609–2616. [Google Scholar] [CrossRef] [PubMed]
- van Hooft, J.; Kielenstijn, G.; Liebregts, J.; Baan, F.; Meijer, G.; D’haese, J.; Bronkhorst, E.; Verhamme, L. Intraoral Scanning as an Alternative to Evaluate the Accuracy of Dental Implant Placements in Partially Edentate Situations: A Prospective Clinical Case Series. J. Clin. Med. 2022, 11, 5876. [Google Scholar] [CrossRef]
- Smojver, I.; Bjelica, R.; Vuletić, M.; Gerbl, D.; Budimir, A.; Gabrić, D. Antimicrobial Efficacy and Permeability of Various Sealing Materials in Two Different Types of Implant–Abutment Connections. Int. J. Mol. Sci. 2022, 23, 8031. [Google Scholar] [CrossRef]
- Do Vale Souza, J.P.; de Moraes Melo Neto, C.L.; Piacenza, L.T.; Freitas da Silva, E.V.; de Melo Moreno, A.L.; Penitente, P.A.; Brunetto, J.L.; Dos Santos, D.M.; Goiato, M.C. Relation Between Insertion Torque and Implant Stability Quotient: A Clinical Study. Eur. J. Dent. 2021, 15, 618–623. [Google Scholar] [CrossRef]
- Tetè, G.; Cisternino, L.; Giorgio, G.; Sacchi, L.; Montemezzi, P.; Sannino, G. Immediate versus Delayed Loading of Post-Extraction Implants in the Aesthetic Zone: A Prospective Longitudinal Study with 4-Year Follow-Up. J. Biol. Regul. Homeost. Agents 2020, 34, 19–25. [Google Scholar]
- Vervaeke, S.; Matthys, C.; Nassar, R.; Christiaens, V.; Cosyn, J.; De Bruyn, H. Adapting the Vertical Position of Implants with a Conical Connection in Relation to Soft Tissue Thickness Prevents Early Implant Surface Exposure: A 2-Year Prospective Intra-Subject Comparison. J. Clin. Periodontol. 2018, 45, 605–612. [Google Scholar] [CrossRef]
- Heydecke, G.; Mirzakhanian, C.; Behneke, A.; Behneke, N.; Fügl, A.; Zechner, W.; Baer, R.A.; Nölken, R.; Gottesman, E.; Colic, S.; et al. A Prospective Multicenter Evaluation of Immediately Functionalized Tapered Conical Connection Implants for Single Restorations in Maxillary Anterior and Premolar Sites: 3-Year Results. Clin. Oral Investig. 2019, 23, 1877–1885. [Google Scholar] [CrossRef]
- Fernández-Figares-Conde, I.; Castellanos-Cosano, L.; Fernandez-Ruiz, J.-A.; Soriano-Santamaria, I.; Hueto-Madrid, J.-A.; Gómez-Lagunas, J.; Romano-Laureato, R.; Torres-Lagares, D. Multicentre Prospective Study Analysing Relevant Factors Related to Marginal Bone Loss: A Two-Year Evolution. Dent. J. 2023, 11, 185. [Google Scholar] [CrossRef] [PubMed]
- Hamudi, N.; Barnea, E.; Weinberg, E.; Laviv, A.; Mijiritsky, E.; Matalon, S.; Chaushu, L.; Kolerman, R. The Association of the One-Abutment at One-Time Concept with Marginal Bone Loss around the SLA and Platform Switch and Conical Abutment Implants. J. Clin. Med. 2021, 11, 74. [Google Scholar] [CrossRef] [PubMed]
- Canullo, L.; Pesce, P.; Tronchi, M.; Fiorellini, J.; Amari, Y.; Penarrocha, D. Marginal Soft Tissue Stability around Conical Abutments Inserted with the One Abutment-One Time Protocol after 5 Years of Prosthetic Loading. Clin. Implant Dent. Relat. Res. 2018, 20, 976–982. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.; Lucchina, A.G.; Brucoli, M.; Migliario, M.; Mortellaro, C.; Mangano, C. Prosthetic Complications Affecting Single-Tooth Morse-Taper Connection Implants. J. Craniofacial Surg. 2018, 29, 2255–2262. [Google Scholar] [CrossRef] [PubMed]
- De Melo, L.A.; de Farias, D.B.; de Medeiros, A.K.B.; Barbosa, G.A.S.; Dantas, E.M.; Carreiro, A. da F.P. Comparative Evaluation of Peri-Implant Tissues in Patients Wearing Mandibular Overdenture with Different Implant Platforms. J. Indian Soc. Periodontol. 2017, 21, 473–477. [Google Scholar] [CrossRef]
- Melo, L.A.d.; de Souza, M.B.C.; Barbosa, G.A.S.; Carreiro, A. da F.P. Peri-Implant Bone Loss of External Hexagon and Morse Taper in Patients Wearing Immediately Loaded Overdentures. Braz. Dent. J. 2017, 28, 694–698. [Google Scholar] [CrossRef]
- Szyszkowski, A.; Kozakiewicz, M. Effect of Implant-Abutment Connection Type on Bone Around Dental Implants in Long-Term Observation: Internal Cone Versus Internal Hex. Implant Dent. 2019, 28, 430–436. [Google Scholar] [CrossRef]
- Horwitz, J.; Machtei, E.E.; Frankental, S.; Gabay, E.; Mayer, Y.; Joseph, L.; Cohen, O. Clinical and Patient-Related Outcomes of a Tapered Implant System With Switched Platform Conical Abutments: A Private Practice Field Trial. J. Oral Implantol. 2018, 44, 326–329. [Google Scholar] [CrossRef]
- Dagher, M.; Mokbel, N.; Aboukhalil, R.; Ghosn, N.; Kassir, A.; Naaman, N. Marginal Bone Level and Bone Thickness Reduction in Delayed and Immediate Implant Placement Protocol 6 Months Post-Loading: An Observational Clinical Prospective Study. J. Maxillofac. Oral Surg. 2022, 21, 571–579. [Google Scholar] [CrossRef]
- Degidi, M.; Nardi, D.; Piattelli, A. The Conometric Concept: Coupling Connection for Immediately Loaded Titanium-Reinforced Provisional Fixed Partial Dentures—A Case Series. Int. J. Periodontics Restor. Dent. 2016, 36, 347–354. [Google Scholar] [CrossRef]
- De Paoli, S.; Benfenati, S.P.; Gobbato, L.; Toia, M.; Chen, C.-Y.; Nevins, M.; Kim, D.M. A Prospective Clinical Assessment of BioHorizons Tissue-Level Implants. Int. J. Periodontics Restor. Dent. 2023, 43, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Lorusso, C.; Di Giulio, C.; Mazzatenta, A. Evaluation of the Sealing Capability of the Implant Healing Screw by Using Real Time Volatile Organic Compounds Analysis: Internal Hexagon Versus Cone Morse. J. Periodontol. 2016, 87, 1492–1498. [Google Scholar] [CrossRef] [PubMed]
- Doornewaard, R.; Sakani, S.; Matthys, C.; Glibert, M.; Bronkhorst, E.; Vandeweghe, S.; Vervaeke, S.; De Bruyn, H. Four-Implant-Supported Overdenture Treatment in the Maxilla. Part I: A Randomized Controlled Split Mouth Trial Assessing the Effect of Microthreads and Abutment Connection Type on 4 Years Peri-Implant Health. Clin. Implant Dent. Relat. Res. 2021, 23, 671–679. [Google Scholar] [CrossRef] [PubMed]
- Pieri, F.; Aldini, N.N.; Marchetti, C.; Corinaldesi, G. Influence of Implant-Abutment Interface Design on Bone and Soft Tissue Levels around Immediately Placed and Restored Single-Tooth Implants: A Randomized Controlled Clinical Trial. Int. J. Oral Maxillofac. Implants 2011, 26, 169–178. [Google Scholar] [PubMed]
- Ogino, Y.; Matsushita, Y.; Sasaki, M.; Ayukawa, Y.; Koyano, K. A 3-Year Prospective Study on Radiographic Marginal Bone Evaluation Around Platform-Shifting Implants with Internal Conical Connections. Int. J. Oral Maxillofac. Implants 2021, 36, 574–580. [Google Scholar] [CrossRef]
- Corvino, E.; Pesce, P.; Camodeca, F.; Moses, O.; Iannello, G.; Canullo, L. Clinical and Radiological Outcomes of Implants with Two Different Connection Configurations: A Randomised Controlled Trial. Int. J. Oral Implantol. 2020, 13, 355–368. [Google Scholar]
- Farronato, D.; Manfredini, M.; Stocchero, M.; Caccia, M.; Azzi, L.; Farronato, M. Influence of Bone Quality, Drilling Protocol, Implant Diameter/Length on Primary Stability: An In Vitro Comparative Study on Insertion Torque and Resonance Frequency Analysis. J. Oral Implantol. 2020, 46, 182–189. [Google Scholar] [CrossRef]
- Moroi, A.; Saito, Y.; Takayama, A.; Ueki, K. Comparison of Nonself-Tapping Tapered Implant and Self-Tapping Hybrid Implant in Terms of Implant Stability at Initial and Second Fixation: A Prospective Randomized Clinical Trial. Clin. Implant Dent. Relat. Res. 2020, 22, 679–688. [Google Scholar] [CrossRef]
- Bernard, L.; Vercruyssen, M.; Vanderveken, J.; Coucke, W.; Quirynen, M.; Naert, I. Randomized Controlled Trial Comparing Immediate Loading with Conventional Loading Using Cone-Anchored Implant-Supported Screw-Retained Removable Prostheses: A 2-Year Follow-up Clinical Trial. J. Prosthet. Dent. 2019, 121, 258–264. [Google Scholar] [CrossRef]
- Guarnieri, R.; Grande, M.; Ippoliti, S.; Iorio-Siciliano, V.; Riccitiello, F.; Farronato, D. Influence of a Laser-Lok Surface on Immediate Functional Loading of Implants in Single-Tooth Replacement: Three-Year Results of a Prospective Randomized Clinical Study on Soft Tissue Response and Esthetics. Int. J. Periodontics Restor. Dent. 2015, 35, 865–875. [Google Scholar] [CrossRef]
- McGuire, M.K.; Scheyer, T.; Ho, D.K.; Stanford, C.M.; Feine, J.S.; Cooper, L.F. Esthetic Outcomes in Relation to Implant-Abutment Interface Design Following a Standardized Treatment Protocol in a Multicenter Randomized Controlled Trial--a Cohort of 12 Cases at 1-Year Follow-Up. Int. J. Periodontics Restor. Dent. 2015, 35, 149–159. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Koutouzis, T.; Mesia, R.; Calderon, N.; Wong, F.; Wallet, S. The Effect of Dynamic Loading on Bacterial Colonization of the Dental Implant Fixture–Abutment Interface: An In Vitro Study. J. Oral Implantol. 2014, 40, 432–437. [Google Scholar] [CrossRef] [PubMed]
- Koutouzis, T.; Neiva, R.; Nonhoff, J.; Lundgren, T. Placement of Implants with Platform-Switched Morse Taper Connections with the Implant-Abutment Interface at Different Levels in Relation to the Alveolar Crest: A Short-Term (1-Year) Randomized Prospective Controlled Clinical Trial. Int. J. Oral Maxillofac. Implants 2013, 28, 1553–1563. [Google Scholar] [CrossRef] [PubMed]
- Afrashtehfar, K.I.; Weber, A.; Abou-Ayash, S. Titanium-Base Abutments May Have Similar Long-Term Peri-Implant Effects as Non-Bonded One-Piece Abutments. Evid. Based Dent. 2022, 23, 134–135. [Google Scholar] [CrossRef]
- Meloni, S.M.; Melis, L.; Xhanari, E.; Tallarico, M.; Spano, G.; Pisano, M.; Baldoni, E.; Cervino, G.; Tullio, A.; Lumbau, A.I. Three-Year Retrospective Comparative Study between Implants with Same Body-Design but Different Crest Module Configurations. Dent. J. 2020, 8, 135. [Google Scholar] [CrossRef]
- Park, H.; Moon, I.-S.; Chung, C.; Shin, S.-J.; Huh, J.-K.; Yun, J.-H.; Lee, D.-W. Comparison of Peri-Implant Marginal Bone Level Changes between Tapered and Straight Implant Designs: 5-Year Follow-up Results. J. Periodontal Implant Sci. 2021, 51, 422–432. [Google Scholar] [CrossRef]
- Kruse, A.B.; Wild, V.; Ratka-Krüger, P.; Vach, K.; Frisch, E. Peri-Implant Bone-Level Changes in the Second Decade of Loading with Regard to the Implant-Abutment Connection: A Retrospective Study on Implants under Systematic Aftercare. Int. J. Implant Dent. 2021, 7, 104. [Google Scholar] [CrossRef]
- Canullo, L.; Menini, M.; Bagnasco, F.; Di Tullio, N.; Pesce, P. Tissue-Level versus Bone-Level Single Implants in the Anterior Area Rehabilitated with Feather-Edge Crowns on Conical Implant Abutments: An up to 5-Year Retrospective Study. J. Prosthet. Dent. 2022, 128, 936–941. [Google Scholar] [CrossRef]
- Baldi, D.; Colombo, J.; Verardi, S.; Rebaudi, A.; Rebaudi, F.; Makary, C. Clinical Osseointegration of Bone Level Implants with Conical Shape and Textured Surface with Low Primary Stability. Minerva Stomatol. 2020, 69, 8–13. [Google Scholar] [CrossRef]
- Thomé, G.; Cartelli, C.A.; Vianna, C.P.; Trojan, L.C. Retrospective Clinical Study of 453 Novel Tapered Implants Placed in All Bone Types: Survival Rate Analysis Up to 2 Years of Follow-Up. Int. J. Oral Maxillofac. Implants 2020, 35, 757–761. [Google Scholar] [CrossRef]
- Koutouzis, T.; Podaru, A.; Neiva, R. Facial Peri-Implant Soft Tissue Topography of Posterior Single Implant-Supported Restorations and Relationship to Adjacent Teeth: A Retrospective Analysis. Int. J. Oral Maxillofac. Implants 2015, 30, 681–687. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Romanos, G.; Grizas, E.; Laukart, E.; Nentwig, G.-H. Effects of Early Moderate Loading on Implant Stability: A Retrospective Investigation of 634 Implants with Platform Switching and Morse-Tapered Connections. Clin. Implant Dent. Relat. Res. 2016, 18, 301–309. [Google Scholar] [CrossRef] [PubMed]
- Simonpieri, A.; Gasparro, R.; Pantaleo, G.; Mignogna, J.; Riccitiello, F.; Sammartino, G. Four-Year Post-Loading Results of Full-Arch Rehabilitation with Immediate Placement and Immediate Loading Implants: A Retrospective Controlled Study. Quintessence Int. 2017, 48, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Guarnieri, R.; Placella, R.; Testarelli, L.; Iorio-Siciliano, V.; Grande, M. Clinical, Radiographic, and Esthetic Evaluation of Immediately Loaded Laser Microtextured Implants Placed into Fresh Extraction Sockets in the Anterior Maxilla: A 2-Year Retrospective Multicentric Study. Implant Dent. 2014, 23, 144–154. [Google Scholar] [CrossRef]
- Machtei, E.E.; Oved-Peleg, E.; Peled, M. Comparison of Clinical, Radiographic and Immunological Parameters of Teeth and Different Dental Implant Platforms. Clin. Oral Implants Res. 2006, 17, 658–665. [Google Scholar] [CrossRef]
- Romanos, G.E.; May, S.; May, D. Treatment Concept of the Edentulous Mandible with Prefabricated Telescopic Abutments and Immediate Functional Loading. Int. J. Oral Maxillofac. Implants 2011, 26, 593–597. [Google Scholar]
- Lin, M.I.; Shen, Y.W.; Huang, H.L.; Hsu, J.T.; Fuh, L.J. A Retrospective Study of Implant-Abutment Connections on Crestal Bone Level. J. Dent. Res. 2013, 92, 202S–207S. [Google Scholar] [CrossRef]
- Lopez, M.A.; Andreasi Bassi, M.; Confalone, L.; Gaudio, R.M.; Lombardo, L.; Lauritano, D. Clinical Outcome of 215 Transmucosal Implants with a Conical Connection: A Retrospective Study after 5-Year Follow-Up. J. Biol. Regul. Homeost. Agents 2016, 30, 55–60. [Google Scholar]
- Lops, D.; Stocchero, M.; Motta Jones, J.; Freni, A.; Palazzolo, A.; Romeo, E. Five Degree Internal Conical Connection and Marginal Bone Stability around Subcrestal Implants: A Retrospective Analysis. Materials 2020, 13, 3123. [Google Scholar] [CrossRef]
- Canullo, L.; Hjerppe, J.; Menini, M.; Bagnasco, F.; Petazzi, G.M.; Pesce, P. Zirconia Crowns and FDPs with Feather-Edge Margins on Conical Implant Abutments-Up-To-5-Year Clinical Retrospective Study. Int. J. Prosthodont. 2022, 35, 380–386. [Google Scholar] [CrossRef]
- Al-Fakeh, H.; Sharhan, H.M.; Ziyad, T.A.; Abdulghani, E.A.; Al-Moraissi, E.; Al-Sosowa, A.A.; Liu, B.; Zhang, K. Three-Dimensional Radiographic Assessment of Bone Changes around Posterior Dental Implants at Native Bone Site in Gansu Province, Northwest of China: A Retrospective Cohort Study. J. Stomatol. Oral Maxillofac. Surg. 2022, 123, e186–e191. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.; Zhou, H.; Zhang, W.; Chen, J.; Zheng, Y.; Wang, L.; Yang, F. Evaluation of a Platform-Switched Morse Taper Connection for All-on-Four or Six Treatment in Edentulous or Terminal Dentition Treatment: A Retrospective Study with 1-8 Years of Follow-Up. Clin. Implant Dent. Relat. Res. 2023, 25, 815–828. [Google Scholar] [CrossRef] [PubMed]
- Mangano, C.; Iaculli, F.; Piattelli, A.; Mangano, F. Fixed Restorations Supported by Morse-Taper Connection Implants: A Retrospective Clinical Study with 10-20 Years of Follow-Up. Clin. Oral Implants Res. 2015, 26, 1229–1236. [Google Scholar] [CrossRef] [PubMed]
- Gehrke, S.A.; Scarano, A.; Cortellari, G.C.; Fernandes, G.V.O.; Mesquita, A.M.M.; Bianchini, M.A. Marginal Bone Level and Biomechanical Behavior of Titanium-Indexed Abutment Base of Conical Connection Used for Single Ceramic Crowns on Morse-Taper Implant: A Clinical Retrospective Study. J. Funct. Biomater. 2023, 14, 128. [Google Scholar] [CrossRef]
- Tallarico, M.; Lumbau, A.M.I.; Meloni, S.M.; Ieria, I.; Park, C.-J.; Zadrożny, L.; Xhanari, E.; Pisano, M. Five-Year Prospective Study on Implant Failure and Marginal Bone Remodeling Expected Using Bone Level Implants with Sandblasted/Acid-Etched Surface and Conical Connection. Eur. J. Dent. 2022, 16, 787–795. [Google Scholar] [CrossRef]
- Apaza-Bedoya, K.; Galarraga-Vinueza, M.E.; Correa, B.B.; Schwarz, F.; Bianchini, M.A.; Magalhães Benfatti, C.A. Prevalence, Risk Indicators, and Clinical Characteristics of Peri-Implant Mucositis and Peri-Implantitis for an Internal Conical Connection Implant System: A Multicenter Cross-Sectional Study. J. Periodontol. 2024, 95, 582–593. [Google Scholar] [CrossRef]
- Linkevicius, T.; Puisys, A.; Svediene, O.; Linkevicius, R.; Linkeviciene, L. Radiological Comparison of Laser-Microtextured and Platform-Switched Implants in Thin Mucosal Biotype. Clin. Oral Implants Res. 2015, 26, 599–605. [Google Scholar] [CrossRef]
- Weigl, P.; Trimpou, G.; Lorenz, J.; Nentwig, G.-H.; Lauer, H.-C. Prefabricated Taper Crowns for the Retention of Implant Superstructures: Three-Year Results of a Prospective Clinical Trial. J. Prosthet. Dent. 2019, 121, 618–622. [Google Scholar] [CrossRef]
- Sun, Y.; Yang, J.; Chen, K.; Li, Z.; Chen, Z.; Huang, B. Clinical and Radiographic Results of Crestal vs. Subcrestal Placement of Implants in Posterior Areas: A Split-Mouth Randomized Controlled Clinical Trial. Clin. Implant Dent. Relat. Res. 2023, 25, 948–959. [Google Scholar] [CrossRef]
- Saglanmak, A.; Gultekin, A.; Cinar, C.; Szmukler-Moncler, S.; Karabuda, C. Effect of Soft Tissue Thickness on Crestal Bone Loss of Early Loaded Implants with Platform Switching: 1- and 5-Year Data. Quintessence Int. 2021, 52, 426–433. [Google Scholar] [CrossRef]
- Penitente, P.A.; do Vale Souza, J.P.; Dos Santos, D.M.; Brunetto, J.L.; de Moraes Melo Neto, C.L.; Bueno Carlini Bittencourt, A.B.; de Sousa Ervolino, I.C.; Goiato, M.C. Survival of Osseointegrated Implants: A 10-Year Retrospective Study. Clin. Ter. 2023, 174, 180–184. [Google Scholar] [CrossRef] [PubMed]
- Frisch, E.; Ziebolz, D.; Ratka-Krüger, P.; Rinke, S. Double Crown-Retained Maxillary Overdentures: 5-Year Follow-Up. Clin. Implant Dent. Relat. Res. 2015, 17, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Ho, D.S.W.; Yeung, S.C.H.; Zee, K.Y.; Curtis, B.; Hell, P.; Tumuluri, V. Clinical and Radiographic Evaluation of NobelActive(TM) Dental Implants. Clin. Oral Implants Res. 2013, 24, 297–304. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.; Mangano, C.; Ricci, M.; Sammons, R.L.; Shibli, J.A.; Piattelli, A. Single-Tooth Morse Taper Connection Implants Placed in Fresh Extraction Sockets of the Anterior Maxilla: An Aesthetic Evaluation. Clin. Oral Implants Res. 2012, 23, 1302–1307. [Google Scholar] [CrossRef]
- Mangano, C.; Mangano, F.; Shibli, J.A.; Ricci, M.; Sammons, R.L.; Figliuzzi, M. Morse Taper Connection Implants Supporting “Planned” Maxillary and Mandibular Bar-Retained Overdentures: A 5-Year Prospective Multicenter Study. Clin. Oral Implants Res. 2011, 22, 1117–1124. [Google Scholar] [CrossRef]
- Mangano, C.; Mangano, F.; Shibli, J.A.; Tettamanti, L.; Figliuzzi, M.; d’Avila, S.; Sammons, R.L.; Piattelli, A. Prospective Evaluation of 2,549 Morse Taper Connection Implants: 1- to 6-Year Data. J. Periodontol. 2011, 82, 52–61. [Google Scholar] [CrossRef]
- Moberg, L.E.; Köndell, P.A.; Kullman, L.; Heimdahl, A.; Gynther, G.W. Evaluation of Single-Tooth Restorations on ITI Dental Implants. A Prospective Study of 29 Patients. Clin. Oral Implants Res. 1999, 10, 45–53. [Google Scholar] [CrossRef]
- Levine, R.A.; Clem, D.S., 3rd; Wilson, T.G.J.; Higginbottom, F.; Saunders, S.L. A Multicenter Retrospective Analysis of the ITI Implant System Used for Single-Tooth Replacements: Preliminary Results at 6 or More Months of Loading. Int. J. Oral Maxillofac. Implants 1997, 12, 237–242. [Google Scholar]
- Chapman, R.J.; Grippo, W. The Locking Taper Attachment for Implant Abutments: Use and Reliability. Implant Dent. 1996, 5, 257–261. [Google Scholar] [CrossRef]
- Morris, H.F.; Winkler, S.; Ochi, S.; Kanaan, A. A New Implant Designed to Maximize Contact with Trabecular Bone: Survival to 18 Months. J. Oral Implantol. 2001, 27, 164–173. [Google Scholar] [CrossRef]
- Mangano, C.; Bartolucci, E.G. Single Tooth Replacement by Morse Taper Connection Implants: A Retrospective Study of 80 Implants. Int. J. Oral Maxillofac. Implants 2001, 16, 675–680. [Google Scholar] [PubMed]
- Gatti, C.; Chiapasco, M. Immediate Loading of Brånemark Implants: A 24-Month Follow-up of a Comparative Prospective Pilot Study between Mandibular Overdentures Supported by Conical Transmucosal and Standard MK II Implants. Clin. Implant Dent. Relat. Res. 2002, 4, 190–199. [Google Scholar] [CrossRef] [PubMed]
- Kronström, M.; Widbom, T.; Löfquist, L.E.; Henningson, C.; Widbom, C.; Lundberg, T. Early Functional Loading of Conical Brånemark Implants in the Edentulous Mandible: A 12-Month Follow-up Clinical Report. J. Prosthet. Dent. 2003, 89, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Chou, C.-T.; Morris, H.F.; Ochi, S.; Walker, L.; DesRosiers, D. AICRG, Part II: Crestal Bone Loss Associated with the Ankylos Implant: Loading to 36 Months. J. Oral Implantol. 2004, 30, 134–143. [Google Scholar] [CrossRef]
- Toia, M.; Parpaiola, A.; Stevanello, N.; Tattan, M.; Saleh, M.H.A.; Ravidà, A. Clinical Outcomes of Implant- versus Abutment-Level Connection in Screw-Retained Fixed Dental Prostheses: A 5-Year Randomized Controlled Trial. Clin. Oral Implants Res. 2024, 35, 230–241. [Google Scholar] [CrossRef]
- Galindo-Moreno, P.; Catena, A.; Lopez-Chaichio, L.; Borges, T.; O’Valle, F.; Torrecillas-Martínez, L.; Padial-Molina, M. The Influence of History of Severe Periodontitis on Estimated Long-Term Marginal Bone Loss around Implants Restored with Fixed Segmented Full-Arch Rehabilitation. J. Clin. Med. 2023, 12, 6665. [Google Scholar] [CrossRef]
- Gehrke, S.A.; Cortellari, G.C.; De Oliveira Fernandes, G.V.; Scarano, A.; Martins, R.G.; Cançado, R.M.; Mesquita, A.M.M. Randomized Clinical Trial Comparing Insertion Torque and Implant Stability of Two Different Implant Macrogeometries in the Initial Periods of Osseointegration. Medicina 2023, 59, 168. [Google Scholar] [CrossRef]
- Lops, D.; Romeo, E.; Stocchero, M.; Palazzolo, A.; Manfredi, B.; Sbricoli, L. Marginal Bone Maintenance and Different Prosthetic Emergence Angles: A 3-Year Retrospective Study. J. Clin. Med. 2022, 11, 2014. [Google Scholar] [CrossRef]
- Mangalvedhekar, M.; Manas, A.; Jyothirmayee, K.; Richashreev; Tenglikar, P.; Das, A.C. Assessment of Clinical and Radiological Outcome of Implant with Two Different Connections Con Iguration: A Controlled Trial. J. Pharm. Bioallied Sci. 2022, 14, S974–S976. [Google Scholar] [CrossRef]
- Friberg, B.; Ahmadzai, M. A Prospective Study on Single Tooth Reconstructions Using Parallel Walled Implants with Internal Connection (NobelParallel CC) and Abutments with Angulated Screw Channels (ASC). Clin. Implant Dent. Relat. Res. 2019, 21, 226–231. [Google Scholar] [CrossRef]
- Mundt, T.; Mack, F.; Schwahn, C.; Biffar, R. Private Practice Results of Screw-Type Tapered Implants: Survival and Evaluation of Risk Factors. Int. J. Oral Maxillofac. Implants 2006, 21, 607–614. [Google Scholar] [PubMed]
- Mangano, C.; Mangano, F.; Piatelli, A.; Lezzi, G.; Mangano, A.; La Colla, L.; Mangano, A. Single-Tooth Morse Taper Connection Implants after 1 Year of Functional Loading: A Multicentre Study on 302 Patients. Eur. J. Oral Implantol. 2008, 1, 305–315. [Google Scholar] [PubMed]
- Mangano, C.; Mangano, F.; Piattelli, A.; Iezzi, G.; Mangano, A.; La Colla, L. Prospective Clinical Evaluation of 1920 Morse Taper Connection Implants: Results after 4 Years of Functional Loading. Clin. Oral Implants Res. 2009, 20, 254–261. [Google Scholar] [CrossRef] [PubMed]
- Mangano, C.; Mangano, F.; Piattelli, A.; Iezzi, G.; Mangano, A.; La Colla, L. Prospective Clinical Evaluation of 307 Single-Tooth Morse Taper-Connection Implants: A Multicenter Study. Int. J. Oral Maxillofac. Implants 2010, 25, 394–400. [Google Scholar]
- Gultekin, B.A.; Gultekin, P.; Leblebicioglu, B.; Basegmez, C.; Yalcin, S. Clinical Evaluation of Marginal Bone Loss and Stability in Two Types of Submerged Dental Implants. Int. J. Oral Maxillofac. Implants 2013, 28, 815–823. [Google Scholar] [CrossRef]
- Pozzi, A.; Agliardi, E.; Tallarico, M.; Barlattani, A. Clinical and Radiological Outcomes of Two Implants with Different Prosthetic Interfaces and Neck Configurations: Randomized, Controlled, Split-Mouth Clinical Trial. Clin. Implant Dent. Relat. Res. 2014, 16, 96–106. [Google Scholar] [CrossRef]
- Pozzi, A.; Tallarico, M.; Moy, P.K. Immediate Loading with a Novel Implant Featured by Variable-Threaded Geometry, Internal Conical Connection and Platform Shifting: Three-Year Results from a Prospective Cohort Study. Eur. J. Oral Implantol. 2015, 8, 51–63. [Google Scholar]
- Gao, W.M.; Geng, W.; Luo, C.C. Prosthetic Complications of Fixed Dental Prostheses Supported by Locking-Taper Implants: A Retrospective Study with a Mean Follow-up of 5 Years. BMC Oral Health 2021, 21, 476. [Google Scholar] [CrossRef]
- Cooper, L.F.; Reside, G.; DeKok, I.; Stanford, C.; Barwacz, C.; Feine, J.; Nader, S.A.; Scheyer, T.; McGuire, M. A 5-Year Esthetic RCT Assessment of Anterior Maxillary Single-Tooth Implants with Different Abutment Interfaces. Int. J. Oral Maxillofac. Implants 2021, 36, 165–176. [Google Scholar] [CrossRef]
- Dev, S.V.; Perti, S.; Sahoo, K.K.; Mohanty, A.; Pati, S.K.; Sri, A.N. A Comprehensive Assessment of Bone Losses in the Postoperative Phase of Single Implant Placed in Mandibular First Molar Regions: A Cone-Beam Computed Tomography-Based Clinical Study. J. Pharm. Bioallied Sci. 2021, 13, S1530–S1534. [Google Scholar] [CrossRef]
- Paganelli, O.E.B.; Santos, P.L.; Spin-Neto, R.; Pereira-Filho, V.A.; Margonar, R. Stability of Mandibular Implants with Morse Taper and External Hexagon Connections Placed under Immediate Loading: A Longitudinal Clinical Study. Gen. Dent. 2022, 70, 50–54. [Google Scholar] [PubMed]
- Ceruso, F.M.; Ieria, I.; Tallarico, M.; Meloni, S.M.; Lumbau, A.I.; Mastroianni, A.; Zotti, A.; Gargari, M. Comparison between Early Loaded Single Implants with Internal Conical Connection or Implants with Transmucosal Neck Design: A Non-Randomized Controlled Trial with 1-Year Clinical, Aesthetics, and Radiographic Evaluation. Materials 2022, 15, 511. [Google Scholar] [CrossRef] [PubMed]
- Raj, H.K.; Mohan, T.K.; Kattimani, V.; Sreerama, R.; Ramya, Y.; Inampudi, C.K. Evaluation of Immediately Loaded Parallel Conical Connection Implants with Platform Switch in the Maxillary Esthetic Zone: A Prospective Clinical Study. J. Contemp. Dent. Pract. 2022, 23, 405–414. [Google Scholar] [CrossRef] [PubMed]
- Radaelli, M.T.B.; Federizzi, L.; Nascimento, G.G.; Leite, F.R.M.; Boscato, N. Early-Predictors of Marginal Bone Loss around Morse Taper Connection Implants Loaded with Single Crowns: A Prospective Longitudinal Study. J. Periodontal Res. 2020, 55, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Mihali, S.G.; Wang, H.-L.; Karancsi, O.; Bratu, E.A. Internal Hexagon vs. Conical Implant-Abutment Connections: Evaluation of 3-Year Postloading Outcomes. J. Oral Implantol. 2021, 47, 485–490. [Google Scholar] [CrossRef]
- Stacchi, C.; Lamazza, L.; Rapani, A.; Troiano, G.; Messina, M.; Antonelli, A.; Giudice, A.; Lombardi, T. Marginal Bone Changes around Platform-Switched Conical Connection Implants Placed 1 or 2 Mm Subcrestally: A Multicenter Crossover Randomized Controlled Trial. Clin. Implant Dent. Relat. Res. 2023, 25, 398–408. [Google Scholar] [CrossRef]
- Linkevicius, T.; Linkevicius, R.; Gineviciute, E.; Alkimavicius, J.; Mazeikiene, A.; Linkeviciene, L. The Influence of New Immediate Tissue Level Abutment on Crestal Bone Stability of Subcrestally Placed Implants: A 1-Year Randomized Controlled Clinical Trial. Clin. Implant Dent. Relat. Res. 2021, 23, 259–269. [Google Scholar] [CrossRef]
- Hartmann, R.; Bandeira, A.C.F.d.M.; de Araújo, S.C.; Brägger, U.; Schimmel, M.; Leles, C.R. A Parallel 3-Group Randomised Clinical Trial Comparing Different Implant Treatment Options for the Edentulous Mandible: 1-Year Effects on Dental Patient-Reported Outcomes and Chewing Function. J. Oral Rehabil. 2020, 47, 1264–1277. [Google Scholar] [CrossRef]
- Pessoa, R.S.; Sousa, R.M.; Pereira, L.M.; Neves, F.D.; Bezerra, F.J.B.; Jaecques, S.V.N.; Sloten, J.V.; Quirynen, M.; Teughels, W.; Spin-Neto, R. Bone Remodeling Around Implants with External Hexagon and Morse-Taper Connections: A Randomized, Controlled, Split-Mouth, Clinical Trial. Clin. Implant Dent. Relat. Res. 2017, 19, 97–110. [Google Scholar] [CrossRef]
- Galindo-Moreno, P.; Concha-Jeronimo, A.; Lopez-Chaichio, L.; Rodriguez-Alvarez, R.; Sanchez-Fernandez, E.; Padial-Molina, M. Marginal Bone Loss around Implants with Internal Hexagonal and Internal Conical Connections: A 12-Month Randomized Pilot Study. J. Clin. Med. 2021, 10, 5427. [Google Scholar] [CrossRef]
- Studenikin, R. Prosthodontics Using Removable Platform Switching Technologies (Multiunit, On1) as Exemplified by Conical Connection Implant Systems for Early and Immediate Loading. Int. J. Dent. 2021, 2021, 6633804. [Google Scholar] [CrossRef] [PubMed]
- Abi Rached, S.; Chakar, C.; Samarani, R.; Menassa, G.; Sembronio, S.; Pucci, R.; Calabrese, L.; Cantore, S.; Malcangi, A.; Spirito, F.; et al. Radiographic Marginal Bone Level Evaluation around Two Different Tissue-Level Implant Systems: A One-Year Prospective Study. Minerva Dent. Oral Sci. 2023, 72, 298–311. [Google Scholar] [CrossRef] [PubMed]
- Bae, M.-S.; Sohn, D.-S.; Ahn, M.-R.; Lee, H.-W.; Jung, H.-S.; Shin, I.-H. Retrospective Multicenter Evaluation of Tapered Implant with a Sandblasted and Acid-Etched Surface at 1 to 4 Years of Function. Implant Dent. 2011, 20, 280–284. [Google Scholar] [CrossRef]
- Palmer, R.M.; Smith, B.J.; Palmer, P.J.; Floyd, P.D. A Prospective Study of Astra Single Tooth Implants. Clin. Oral Implants Res. 1997, 8, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Pozzi, A.; Tabanella, G.; Guida, A.; Hugo, O.; Authelain, C.; Scheyer, E.T.; McGuire, M.K.; Lipton, D. A Novel Parallel-Walled Dental Implant with a Self-Tapping Apex, Conical Connection, and Platform Shifting: Short-Term Results from a Retrospective Multicenter Clinical Study. Int. J. Periodontics Restor. Dent. 2021, 41, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Eskan, M.A.; Uzel, G.; Yilmaz, S. A Fixed Reconstruction of Fully Edentulous Patients with Immediate Function Using an Apically Tapered Implant Design: A Retrospective Clinical Study. Int. J. Implant Dent. 2020, 6, 77. [Google Scholar] [CrossRef]
- Palaska, I.; Tsaousoglou, P.; Vouros, I.; Konstantinidis, A.; Menexes, G. Influence of Placement Depth and Abutment Connection Pattern on Bone Remodeling around 1-Stage Implants: A Prospective Randomized Controlled Clinical Trial. Clin. Oral Implants Res. 2016, 27, e47–e56. [Google Scholar] [CrossRef]
- Galindo-Moreno, P.; Ravidà, A.; Catena, A.; O’Valle, F.; Padial-Molina, M.; Wang, H.-L. Limited Marginal Bone Loss in Implant-Supported Fixed Full-Arch Rehabilitations after 5 Years of Follow-Up. Clin. Oral Implants Res. 2022, 33, 1224–1232. [Google Scholar] [CrossRef]
- Pariente, L.; Dada, K.; Daas, M.; Linder, S.; Dard, M. Evaluation of the Treatment of Partially Edentulous Patients With Bone Level Tapered Implants: 24-Month Clinical and Radiographic Follow-Up. J. Oral Implantol. 2020, 46, 407–413. [Google Scholar] [CrossRef]
- Scarano, A.; Khater, A.G.A.; Gehrke, S.A.; Serra, P.; Francesco, I.; Di Carmine, M.; Tari, S.R.; Leo, L.; Lorusso, F. Current Status of Peri-Implant Diseases: A Clinical Review for Evidence-Based Decision Making. J. Funct. Biomater. 2023, 14, 210. [Google Scholar] [CrossRef]
- Scarano, A.; Valbonetti, L.; Degidi, M.; Pecci, R.; Piattelli, A.; de Oliveira, P.S.; Perrotti, V. Implant-Abutment Contact Surfaces and Microgap Measurements of Different Implant Connections Under 3-Dimensional X-Ray Microtomography. Implant Dent. 2016, 25, 656–662. [Google Scholar] [CrossRef] [PubMed]
- Prithviraj, D.; Muley, N. Evolution of External and Internal Implant to Abutment Connection. Int. J. Oral Implantol. Clin. Res. 2012, 3, 122–129. [Google Scholar] [CrossRef]
- Baj, A.; Bolzoni, A.; Russillo, A.; Lauritano, D.; Palmieri, A.; Cura, F.; Silvestre, F.J.; Giannì, A.B. Cone-Morse Implant Connection System Significantly Reduces Bacterial Leakage between Implant and Abutment: An in Vitro Study. J. Biol. Regul. Homeost. Agents 2017, 31, 203–208. [Google Scholar] [PubMed]
- Bittencourt, A.B.B.C.; Neto, C.L.d.M.M.; Penitente, P.A.; Pellizzer, E.P.; Dos Santos, D.M.; Goiato, M.C. Comparison of the Morse Cone Connection with the Internal Hexagon and External Hexagon Connections Based on Microleakage—Review. Prague Med. Rep. 2021, 122, 181–190. [Google Scholar] [CrossRef]
- Gil, F.J.; Herrero-Climent, M.; Lázaro, P.; Rios, J.V. Implant–Abutment Connections: Influence of the Design on the Microgap and Their Fatigue and Fracture Behavior of Dental Implants. J. Mater. Sci. Mater. Med. 2014, 25, 1825–1830. [Google Scholar] [CrossRef]
- Scarano, A.; Bartolomeo, A.; Piattelli, M.; Iezzi, G.; Alessandro, Q.; Pietro, T.; Piattelli, A. Retrospective Evaluation of the Microgap between Implants and Abutments in 272 Titanium Implants Retrieved from Man: A 16 Years Experience (1989–2004). J. Oral Implantol. 2005, 31, 269–275. [Google Scholar] [CrossRef]
- Lorusso, F.; Greco Lucchina, A.; Romano, F.; Falisi, G.; Di Carmine, M.S.; Bugea, C.; Scarano, A. Microleakage and Mechanical Behavior of Conical vs. Internal Hexagon Implant-Abutment Connection under a Cyclic Load Fatigue Test. Eur. Rev. Med. Pharmacol. Sci. 2023, 27, 122–127. [Google Scholar] [CrossRef]
- Babaji, P.; Parihar, A.S.; Parihar, A.S.; Jagadeesh, K.N.; Alduwayhi, S.; Annapoorneshwari, S.; Khalid, F.M. Evaluation of Microleakage and Microgap of Two Different Internal Implant-Abutment Connections: An In Vitro Study. J. Contemp. Dent. Pract. 2020, 21, 683–685. [Google Scholar] [CrossRef]
- Tsuruta, K.; Ayukawa, Y.; Matsuzaki, T.; Kihara, M.; Koyano, K. The Influence of Implant–Abutment Connection on the Screw Loosening and Microleakage. Int. J. Implant Dent. 2018, 4, 11. [Google Scholar] [CrossRef]


| Search Strategies | |
|---|---|
| Keywords search: | (taper OR cone OR conical OR Cone morse) AND dental implant |
| Timespan | No limitations (1995–2023) |
| Electronic Databases | Pubmed/Medline, EMBASE, Google Scholar |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alla, I.; Scarano, A.; Sinjari, B.; Xhajanka, E.; Lorusso, F. Peri-Implant Bone Stability Around Tapered Implant Prosthetic Connection: A Systematic Review and Meta-Analysis Comparing Different Cone Morse and Conometric Implants Angle Contact and Coupling Interface Designs. Appl. Sci. 2025, 15, 1237. https://doi.org/10.3390/app15031237
Alla I, Scarano A, Sinjari B, Xhajanka E, Lorusso F. Peri-Implant Bone Stability Around Tapered Implant Prosthetic Connection: A Systematic Review and Meta-Analysis Comparing Different Cone Morse and Conometric Implants Angle Contact and Coupling Interface Designs. Applied Sciences. 2025; 15(3):1237. https://doi.org/10.3390/app15031237
Chicago/Turabian StyleAlla, Iris, Antonio Scarano, Bruna Sinjari, Edit Xhajanka, and Felice Lorusso. 2025. "Peri-Implant Bone Stability Around Tapered Implant Prosthetic Connection: A Systematic Review and Meta-Analysis Comparing Different Cone Morse and Conometric Implants Angle Contact and Coupling Interface Designs" Applied Sciences 15, no. 3: 1237. https://doi.org/10.3390/app15031237
APA StyleAlla, I., Scarano, A., Sinjari, B., Xhajanka, E., & Lorusso, F. (2025). Peri-Implant Bone Stability Around Tapered Implant Prosthetic Connection: A Systematic Review and Meta-Analysis Comparing Different Cone Morse and Conometric Implants Angle Contact and Coupling Interface Designs. Applied Sciences, 15(3), 1237. https://doi.org/10.3390/app15031237









