Dynamic, Over-Valgus Correction Without Osteotomy for Nonunion of Subtrochanteric Hip Fractures Using a Dynamic Hip Screw †
Abstract
Featured Application
Abstract
1. Introduction
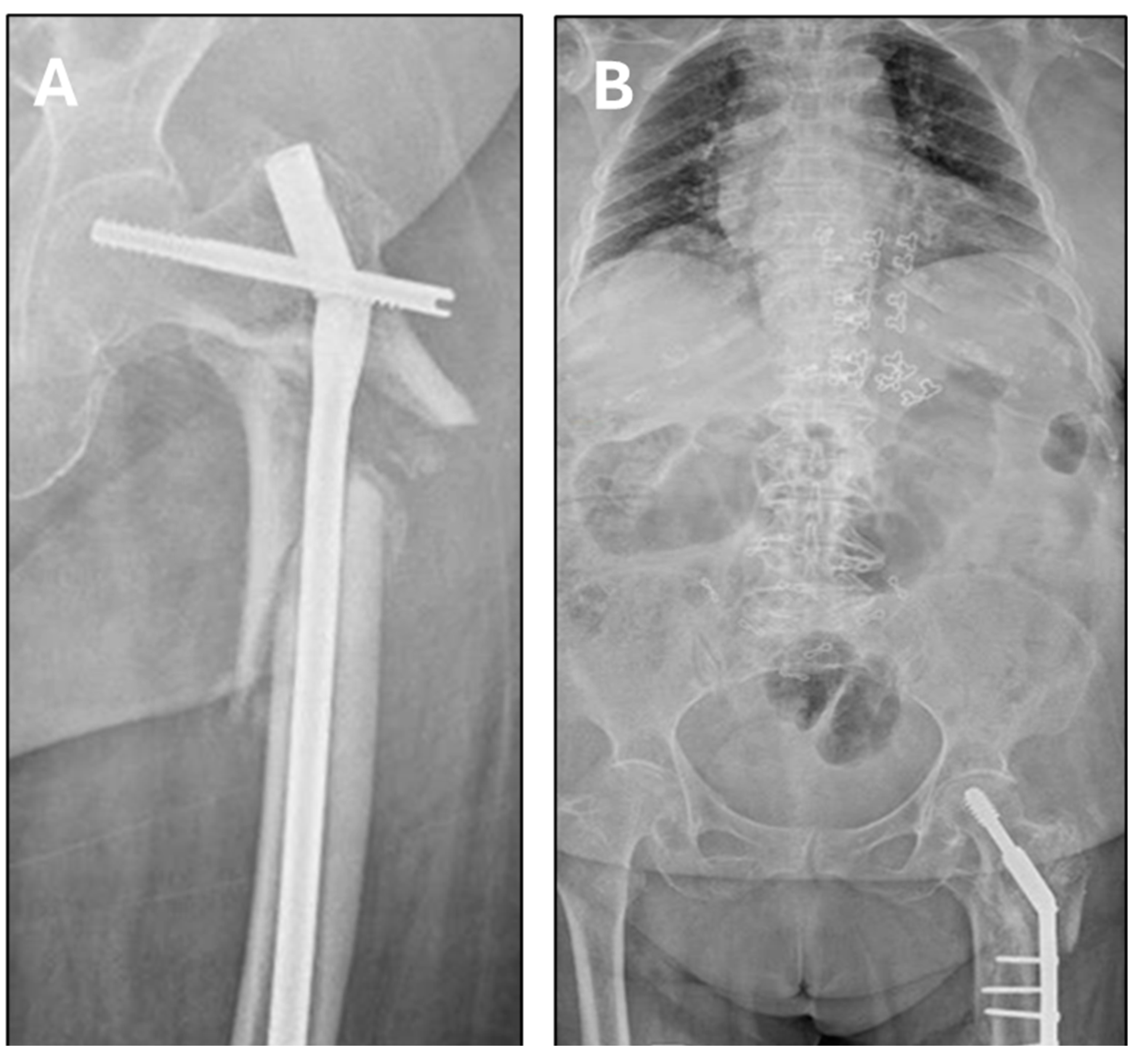
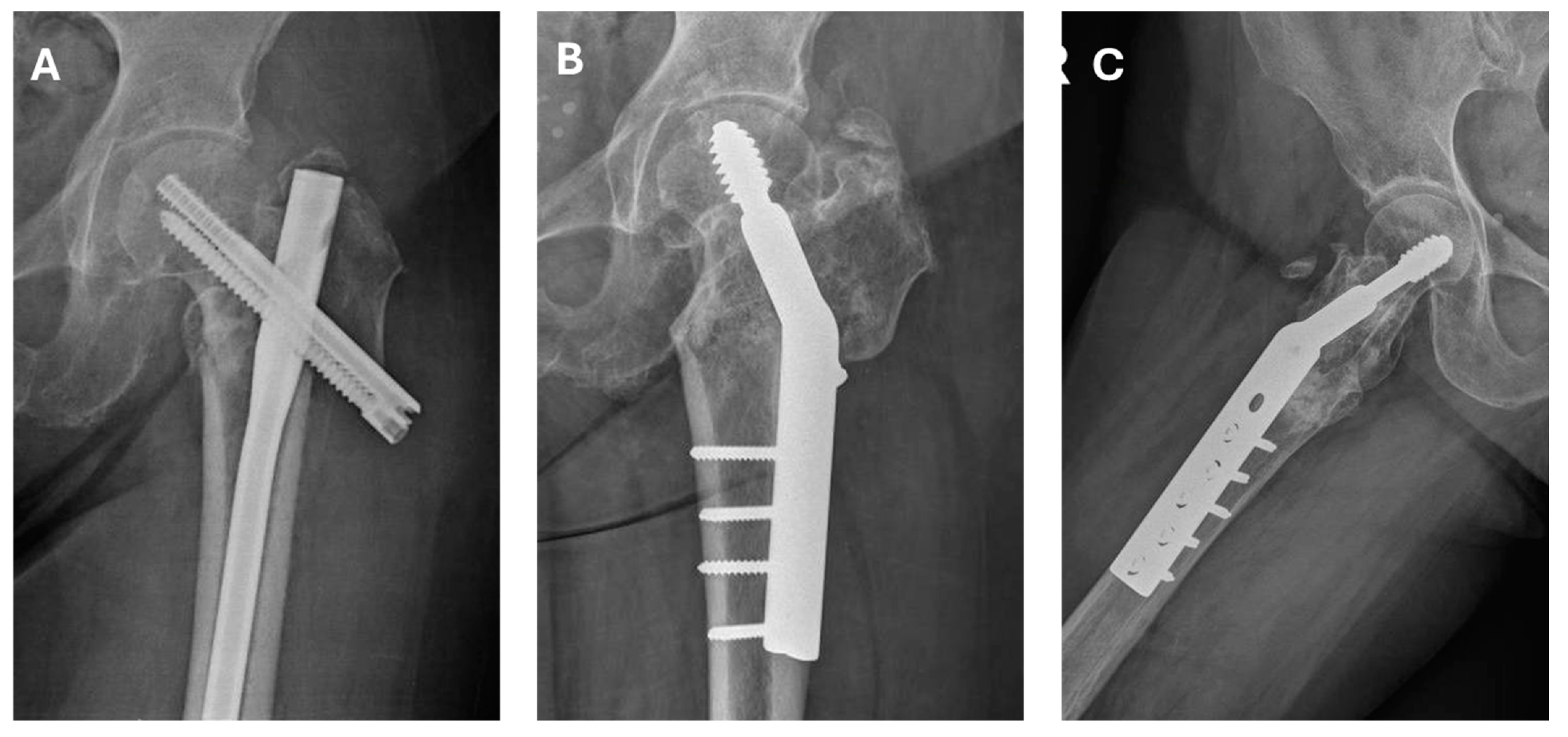
2. Material and Patients
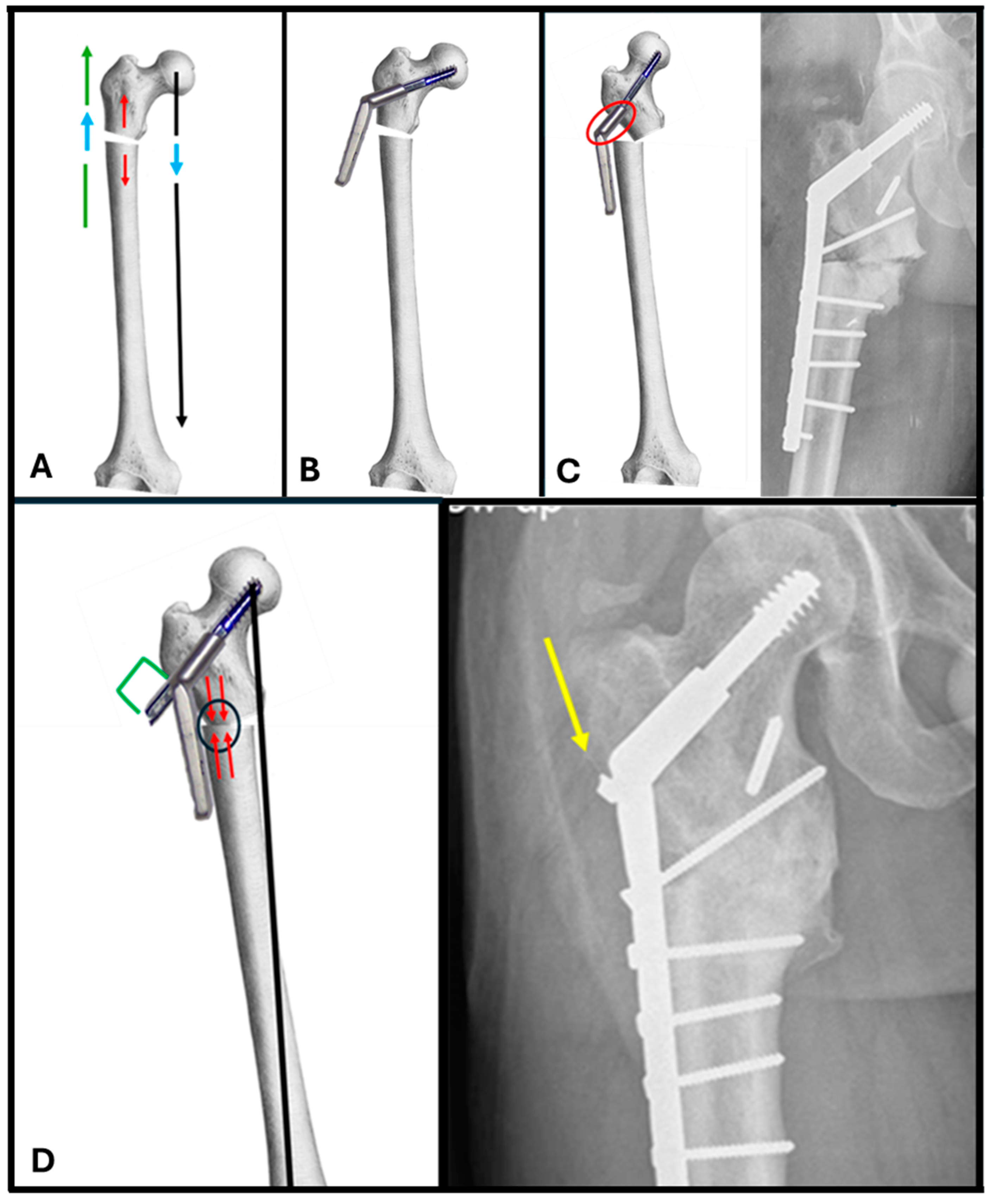
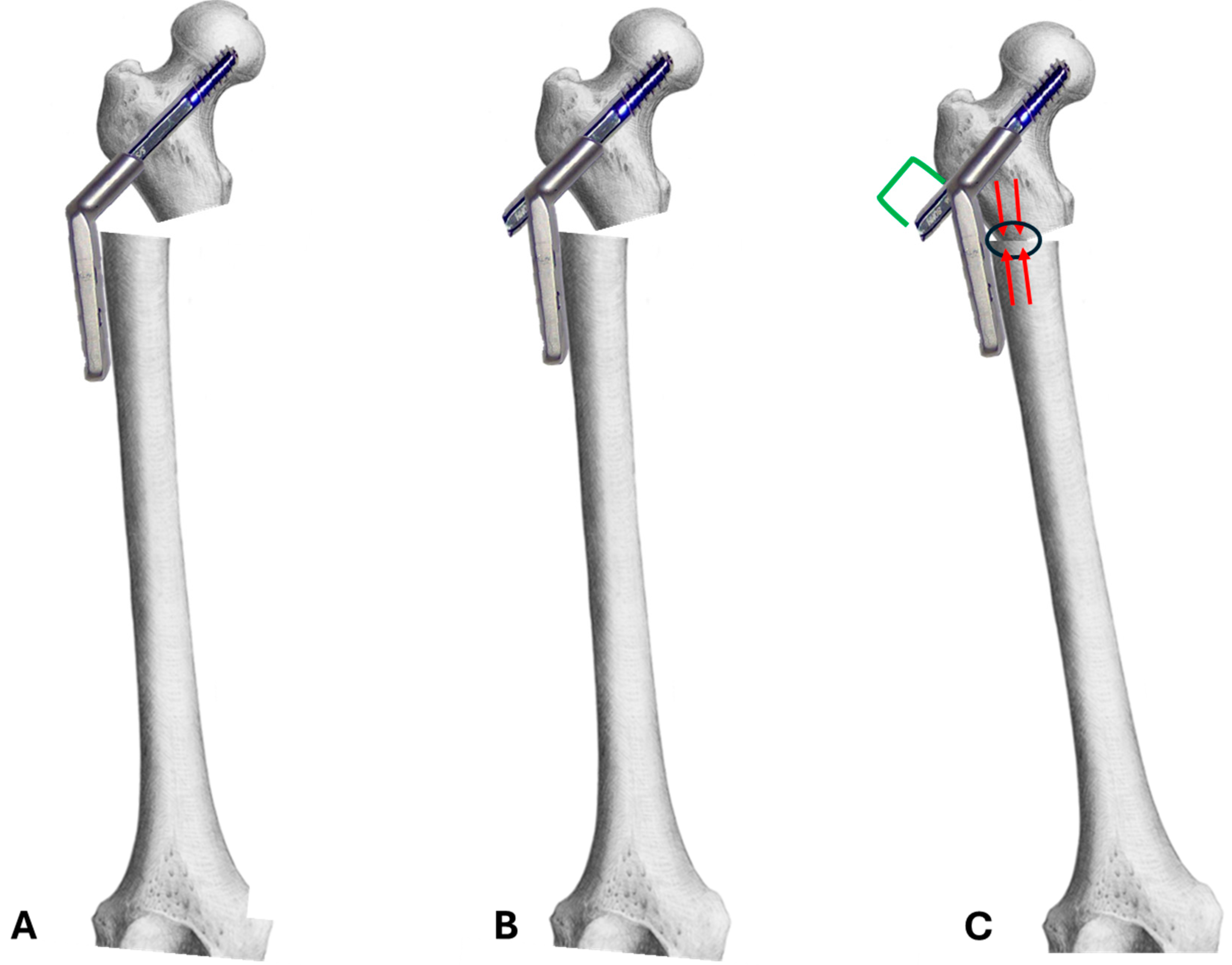
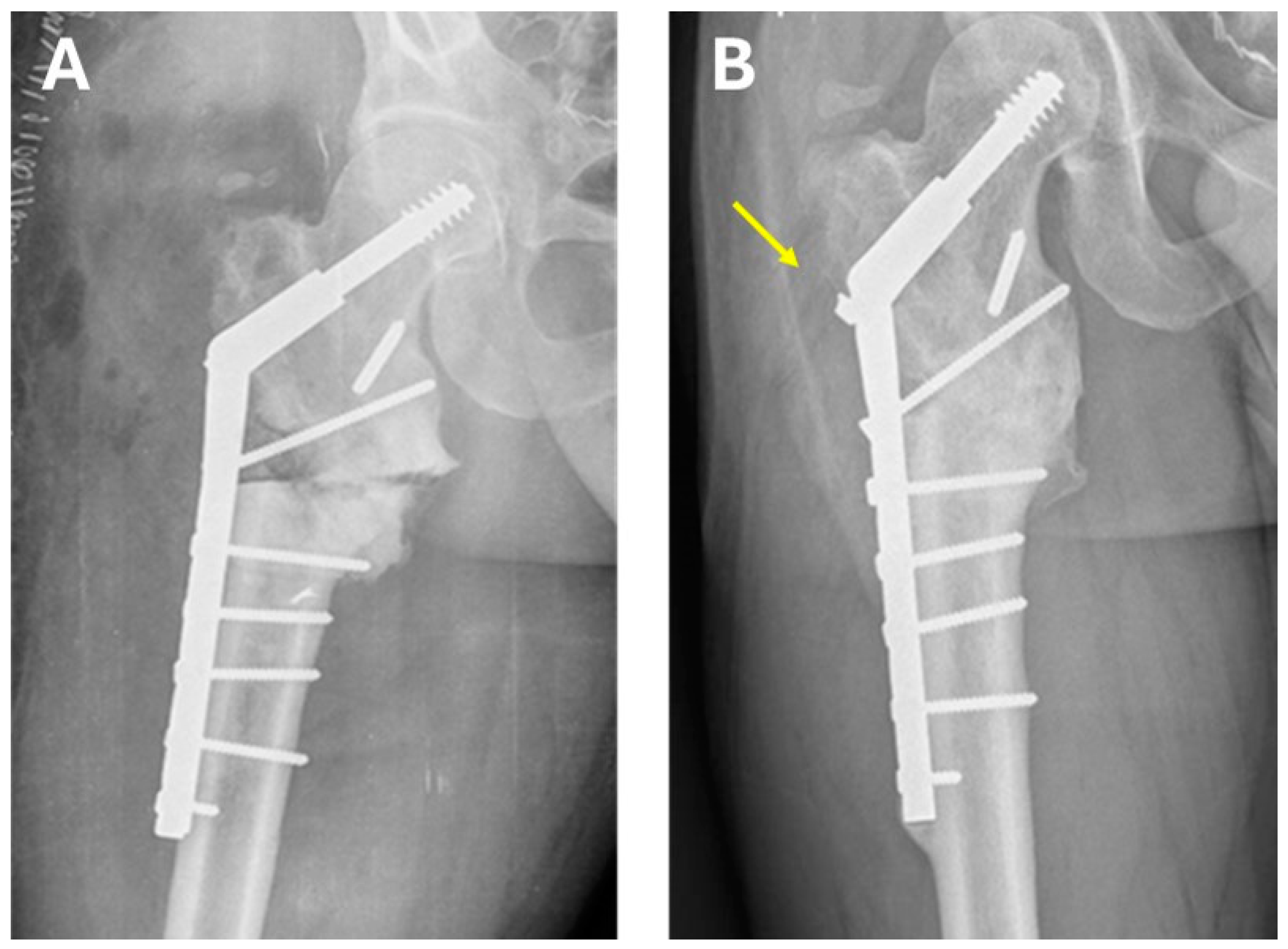
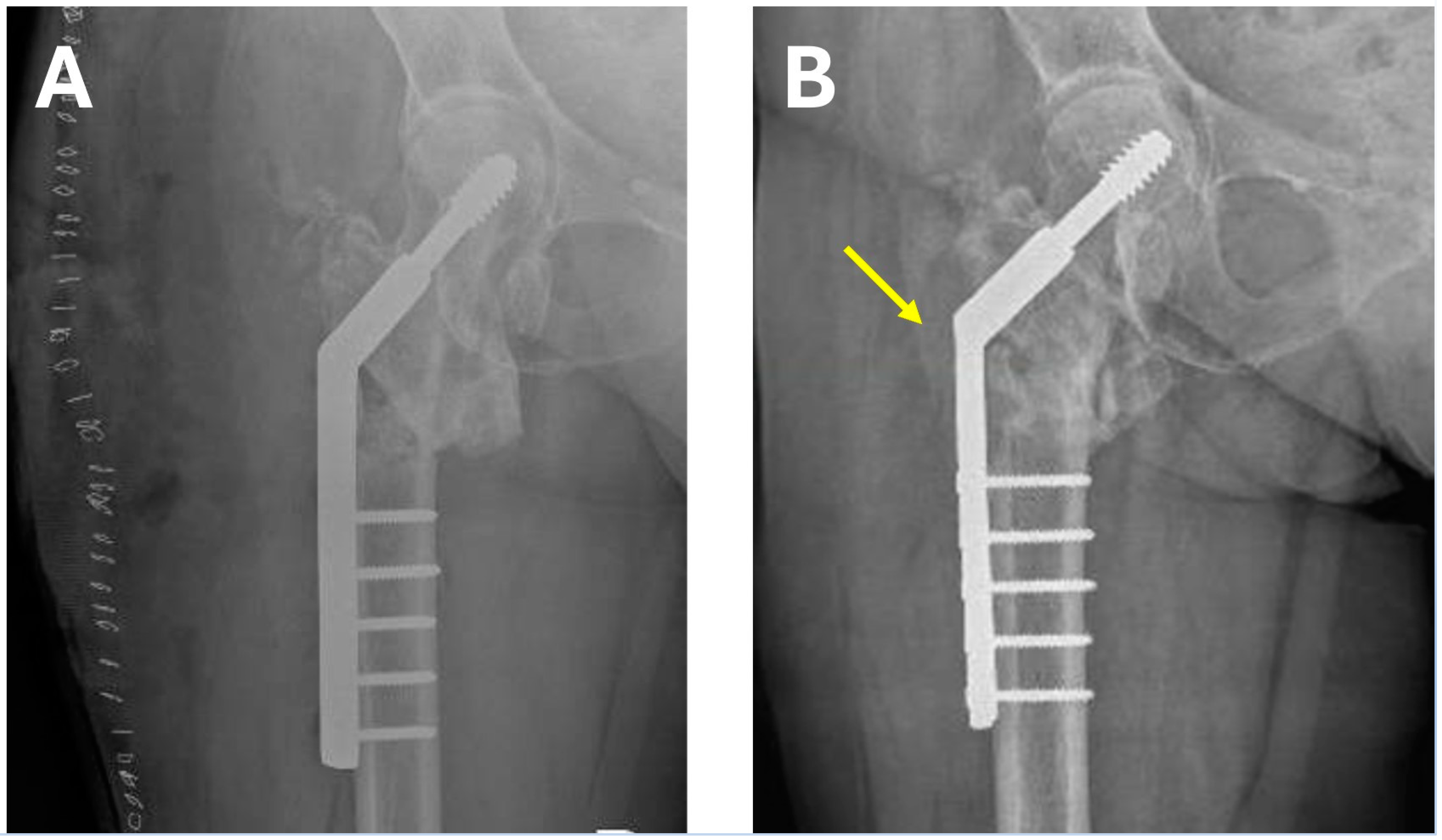
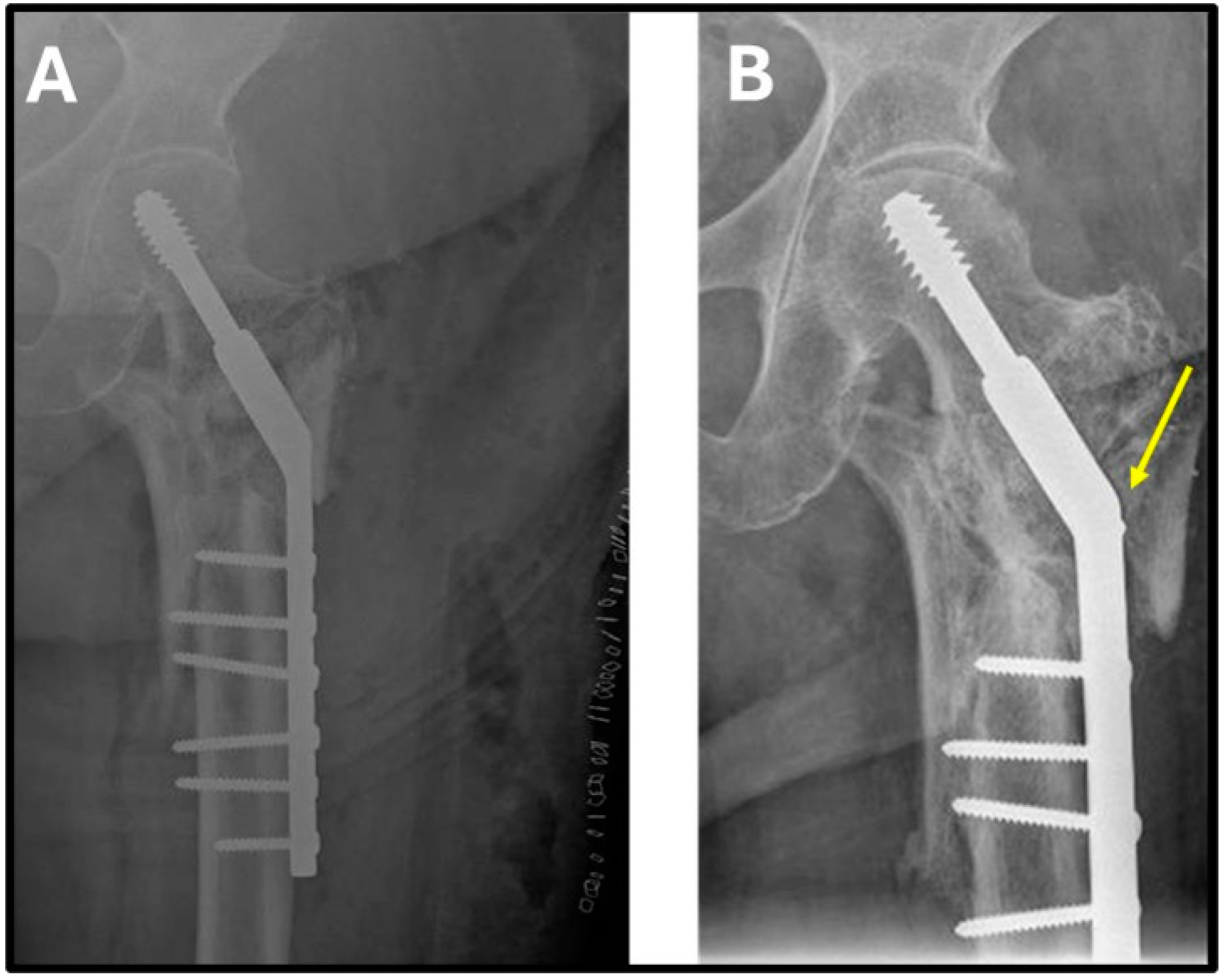
3. Key Points of the Surgical Technique
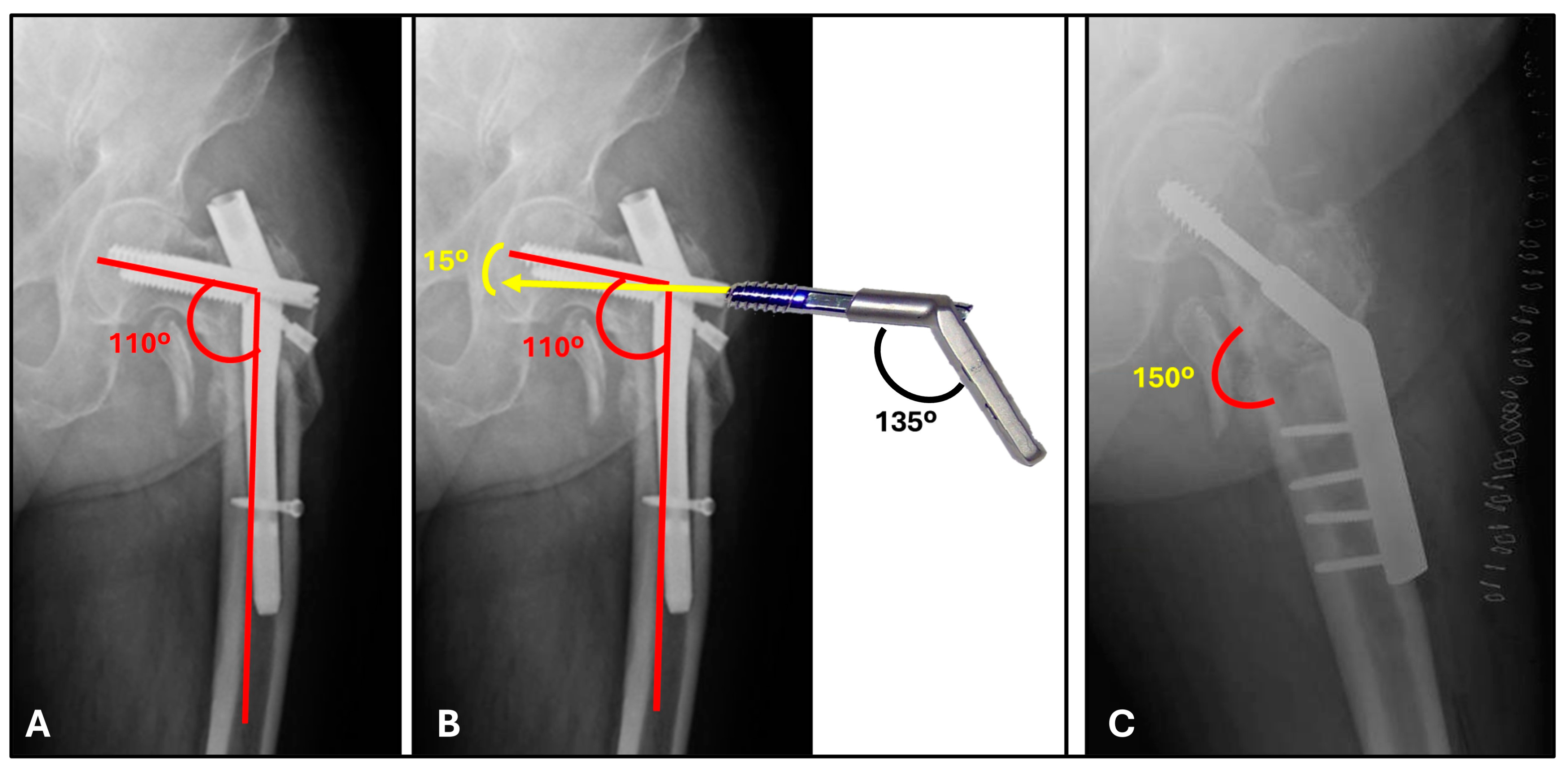
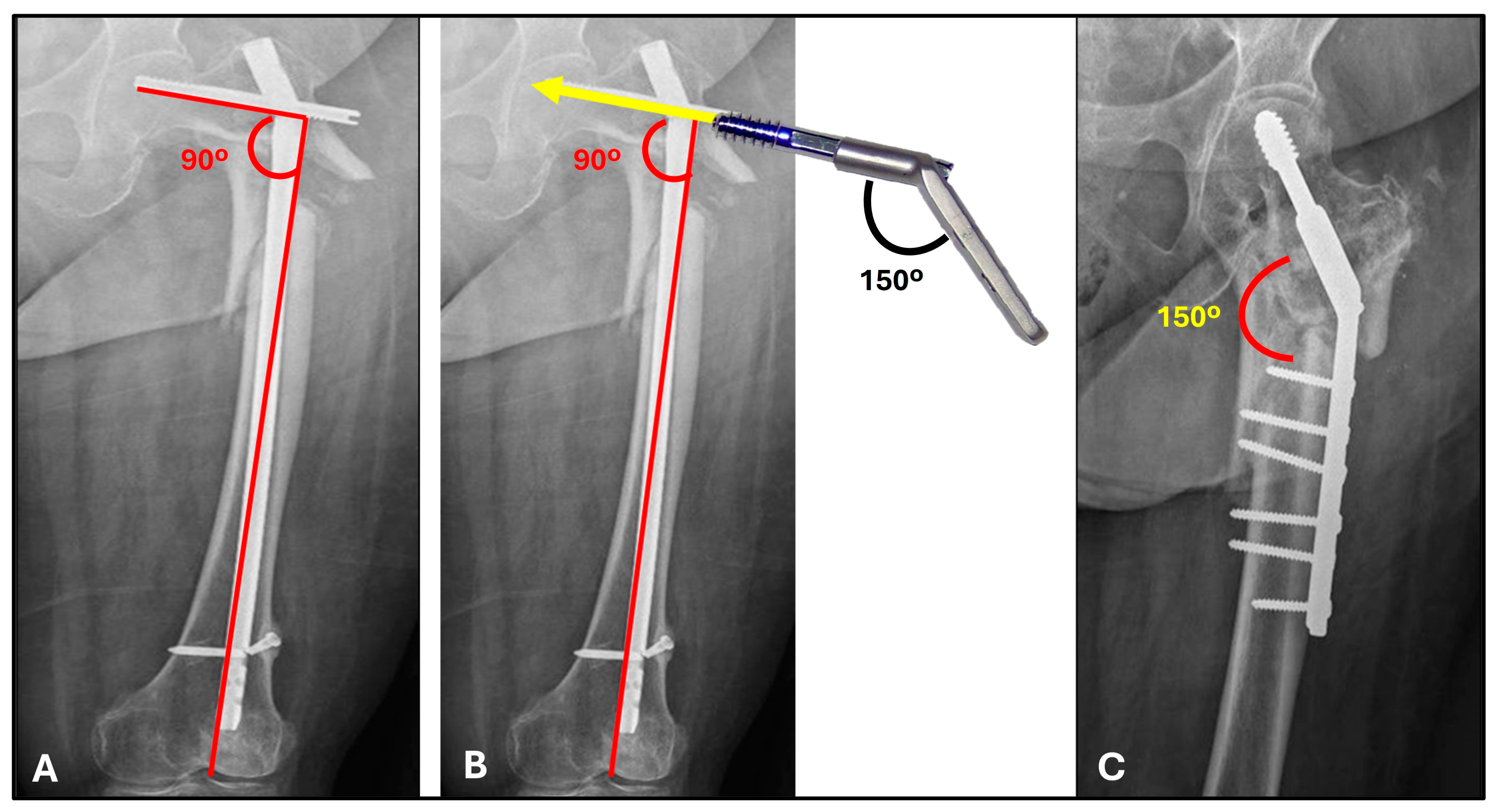
4. Preoperative Planning
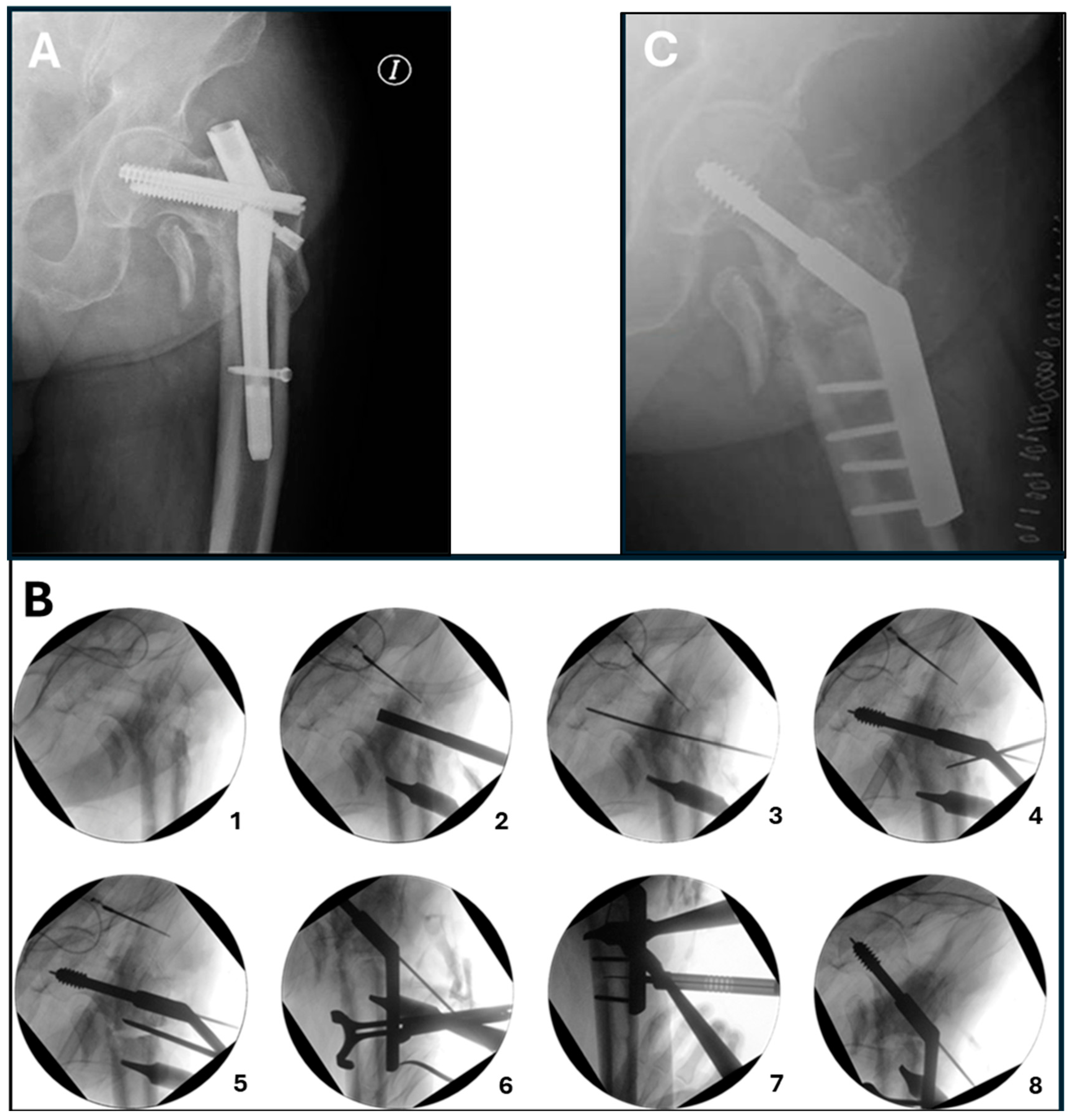
5. Surgical Procedure
6. Results
7. Discussion
- (a)
- The stability of the nonunion site is primarily achieved through the bone, avoiding stress on the device. If the bone does not achieve union in a timely manner, there is more time before its breakage. Conventional techniques have reported up to 13% implant failures [13]. Also, using additional plates is a widespread practice and aims to increase the stability of the nonunion site [13,19]. Although our number of patients is small, no implant failures have occurred in our study. Dynamic fixation secures robust stability between the fragments. In addition, it is implemented by improving load transmission (over valgus correction), making the implementation of the DHS with other devices unnecessary.
- (b)
- Immediate full weight bearing is allowed from the first postoperative day. In previous procedures, full weight bearing is often limited to weeks, along with the limitations this entails, especially for the elderly population.
- (c)
- Grafting of the nonunion site is never required. Bone grafting is necessary in most procedures to promote bone union, which adds comorbidity for the patient. A bone union rate of up to 100% using extramedullary devices that involve bone grafting has been reported [15]. The same 100% bone union rate was obtained in our series. Even expensive, non-risk-free therapies, such as teriparatide or recombinant human bone morphogenetic protein (BMP), have also been used to aid fixation, with promising results [22,23]. Dynamic compression offers an excellent biomechanical environment that promotes quick and significant callus formation, making them unnecessary.
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- DeRogatis, M.J.; Kanakamedala, A.C.; Egol, K.A. Management of Subtrochanteric Femoral Fracture Nonunions. JBJS Rev. 2020, 8, e1900143. [Google Scholar] [CrossRef]
- Gargallo Verge, E.J.; Villalon Ogallar, J.; Perez-Nuñez, M.I. Fracturas subtrocantéreas y diafisarias del femur. In Cirugia Ortopédica y Traumatologia, 6th ed.; Delgado-Martinez, A.D., Ed.; Editorial Médica Panamericana: Madrid, Spain, 2024; pp. 809–818. ISBN 9788411063296. [Google Scholar]
- Sims, S.H. Subtrochanteric Femoral Fractures. Orthop. Clin. 2002, 33, 113–126. [Google Scholar] [CrossRef]
- Kainth, G.S.; Nebhani, N.; Shah, B.; Kumar, G.; Kapoor, B. Varus mal-alignment and residual displacement are associated with delayed union in subtrochanteric femur fracture—A retrospective observational study. J. Orthop. 2023, 46, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Prasarn, M.L.; Ahn, J.; Helfet, D.L.; Lane, J.M.; Lorich, D.G. Bisphosphonate-associated femur fractures have high complication rates with operative fixation. Clin. Orthop. 2012, 470, 2295–2301. [Google Scholar] [CrossRef] [PubMed]
- de Vries, J.S.; Kloen, P.; Borens, O.; Marti, R.K.; Helfet, D.L. Treatment of subtrochanteric nonunions. Injury 2006, 37, 203–211. [Google Scholar] [CrossRef]
- Vicenti, G.; Solarino, G.; Bizzoca, D.; Simone, F.; Maccagnano, G.; Zavattini, G.; Ottaviani, G.; Carrozzo, M.; Buono, C.; Zaccari, D.; et al. Use of the 95-degree angled blade plate with biological and mechanical augmentation to treat proximal femur non-unions: A case series. BMC Musculoskelet. Disord. 2022, 22, 1067. [Google Scholar] [CrossRef] [PubMed]
- Haidukewych, G.J.; Berry, D.J. Nonunion of fractures of the subtrochanteric region of the femur. Clin. Orthop. 2004, 419, 185–188. [Google Scholar] [CrossRef]
- Giannoudis, P.V.; Ahmad, M.A.; Mineo, G.V.; Tosounidis, T.I.; Calori, G.M.; Kanakaris, N.K. Subtrochanteric fracture non-unions with implant failure managed with the “Diamond” concept. Injury 2013, 44 (Suppl. 1), S76–S81. [Google Scholar] [CrossRef] [PubMed]
- Rehme-Röhrl, J.; Brand, A.; Dolt, A.; Grünewald, D.; Hoffmann, R.; Stuby, F.; Schweigkofler, U.; von Rüden, C. Functional and Radiological Results Following Revision Blade Plating and Cephalomedullary Nailing in Aseptic Trochanteric and Subtrochanteric Nonunion. J. Clin. Med. 2024, 13, 3591. [Google Scholar] [CrossRef] [PubMed]
- Dietze, C.; Brand, A.; Friederichs, J.; Stuby, F.; Schneidmueller, D.; von Rüden, C. Results of revision intramedullary nailing with and without auxillary plate in aseptic trochanteric and subtrochanteric nonunion. Eur. J. Trauma Emerg. Surg. Off. Publ. Eur. Trauma Soc. 2022, 48, 1905–1911. [Google Scholar] [CrossRef] [PubMed]
- Barquet, A.; Mayora, G.; Fregeiro, J.; López, L.; Rienzi, D.; Francescoli, L. The treatment of subtrochanteric nonunions with the long gamma nail: Twenty-six patients with a minimum 2-year follow-up. J. Orthop. Trauma 2004, 18, 346–353. [Google Scholar] [CrossRef] [PubMed]
- Lotzien, S.; Rausch, V.; Schildhauer, T.A.; Gessmann, J. Revision of subtrochanteric femoral nonunions after intramedullary nailing with dynamic condylar screw. BMC Musculoskelet. Disord. 2018, 19, 448. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.M.; Rhyu, K.H.; Lim, S.J. Salvage of failed osteosynthesis for an atypical subtrochanteric femoral fracture associated with long-term bisphosphonate treatment using a 95° angled blade plate. Bone Jt. J. 2018, 100, 1511–1517. [Google Scholar] [CrossRef]
- Dumbre Patil, S.S.; Karkamkar, S.S.; Patil, V.S.D.; Patil, S.S.; Ranaware, A.S. Reverse distal femoral locking compression plate a salvage option in nonunion of proximal femoral fractures. Indian J. Orthop. 2016, 50, 374–378. [Google Scholar] [CrossRef] [PubMed]
- Balasubramanian, N.; Babu, G.; Prakasam, S. Treatment of Non Unions of Subtrochanteric Fractures Using an Anatomical Proximal Femur Locked Compression Plate—A Prospective Study of 13 Patients. J. Orthop. Case Rep. 2016, 6, 65–68. [Google Scholar] [CrossRef]
- Vaishya, R.; Agarwal, A.K.; Gupta, N.; Vijay, V. Reversed distal femoral locking plate for failed proximal femoral nail with non-union of proximal femoral fractures. Int. Orthop. 2016, 40, 1709–1715. [Google Scholar] [CrossRef]
- Elliott, D.S.; Newman, K.J.H.; Forward, D.P.; Hahn, D.M.; Ollivere, B.; Kojima, K.; Handley, R.; Rossiter, N.D.; Wixted, J.J.; Smith, R.M.; et al. A unified theory of bone healing and nonunion: BHN theory. Bone Jt. J. 2016, 98, 884–891. [Google Scholar] [CrossRef] [PubMed]
- Matre, K.; Havelin, L.I.; Gjertsen, J.-E.; Vinje, T.; Espehaug, B.; Fevang, J.M. Sliding hip screw versus IM nail in reverse oblique trochanteric and subtrochanteric fractures. A study of 2716 patients in the Norwegian Hip Fracture Register. Injury 2013, 44, 735–742. [Google Scholar] [CrossRef]
- Perren, S.M. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: Choosing a new balance between stability and biology. J. Bone Joint Surg. Br. 2002, 84, 1093–1110. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.-C. Locked nailing for shortened subtrochanteric nonunions: A one-stage treatment. Clin. Orthop. 2009, 467, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.T.; Jeong, H.J.; Lee, S.J.; Kim, H.J.; Yoo, J.J. Adjuvant Teriparatide Therapy for Surgical Treatment of Femoral Fractures; Does It Work? Hip Pelvis 2016, 28, 148–156. [Google Scholar] [CrossRef] [PubMed]
- Haubruck, P.; Kammerer, A.; Korff, S.; Apitz, P.; Xiao, K.; Büchler, A.; Biglari, B.; Zimmermann, G.; Daniel, V.; Schmidmaier, G.; et al. The treatment of nonunions with application of BMP-7 increases the expression pattern for angiogenic and inflammable cytokines: A matched pair analysis. J. Inflamm. Res. 2016, 9, 155–165. [Google Scholar] [CrossRef] [PubMed]
- Dhammi, I.; Jain, A.; Singh, A.; Rehan-Ul-Haq; Mishra, P.; Jain, S. Primary nonunion of intertrochanteric fractures of femur: An analysis of results of valgization and bone grafting. Indian J. Orthop. 2011, 45, 514–519. [Google Scholar] [CrossRef] [PubMed]
- Silva, P.; Coelho, D.L.; Curi, C.; de Oliveira, L.A.; de Moraes, F.B.; do Amaral, R.A.; Rebello, P.R. Proximal femural valgus subtrochanteric osteotomy for non union of trochanteric fractures. Rev. Bras. Ortop. 2012, 47, 37–42. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Vidyadhara, S.; Rao, S.K.; Pandian, S.; Gnanadoss, J. Closing lateral wedge valgus osteotomy with dynamic hip screw for the treatment of varus nonunion of pertrochanteric fracture: Can restoration of biomechanics and stabilization alone heal? Arch. Orthop. Trauma Surg. 2009, 129, 827–832. [Google Scholar] [CrossRef]
- El-Alfy, B.; Abououf, A.; Darweash, A.; Fawzy, S. The effect of valgus reduction on resistant subtrochanteric femoral non-unions: A single-centre report of twenty six cases. Int. Orthop. 2024, 48, 1105–1111. [Google Scholar] [CrossRef]
- Kang, S.H.; Han, S.K.; Kim, Y.S.; Kim, M.J. Treatment of subtrochanteric nonunion of the femur: Whether to leave or to exchange the previous hardware. Acta Orthop. Traumatol. Turc. 2013, 47, 91–95. [Google Scholar] [CrossRef]
| PATIENTS | 1 | 2 | 3 | 4 | 5 | Mean |
|---|---|---|---|---|---|---|
| Age * | 34 | 54 | 85 | 69 | 78 | 64 (34–85) |
| Sex | Male | Female | Female | Female | Female | -- |
| Time from fracture to nonunion diagnosis (months) * | 40 | 12 | 12 | 10 | 13 | 17.4 (40–10) |
| Affected hip | Left | Left | Right | Right | Right | -- |
| Injury mechanism | Vehicle accident | Simple fall | Simple fall | Simple fall | Simple fall | -- |
| Previous implant | Long intramedullary nail $ | Short intramedullary nail | Short intramedullary nail | Short intramedullary nail | Long intramedullary nail & | -- |
| Femoral neck angle pre-surgery * | 122° | 128° | 125° | 110° | 115° | 120° (110–122) |
| Pre-surgery offset (mm) * | 59 | 42 | 50 | 54 | 47 | 50.4 (42–59) |
| Vertical distance nonunion-head pre-surgery (mm) * | 57 | 43 | 32 | 46 | 40 | 43.6 (32–57) |
| Limb length discrepancy (mm) * | 12 | 8 | 9 | 4 | 7 | 8 (4–12) |
| Harris Hip Score pre-surgery * | 30 | 42 | 40 | 44 | 34 | 38 (30–44) |
| Patients | 1 | 2 | 3 | 4 | 5 | Mean/Median |
|---|---|---|---|---|---|---|
| DHS degrees used $ | 135° | 150° | 150° | 135° | 150° | 150° |
| Duration of surgery (min) * | 120 | 63 | 123 | 102 | 156 | 112.8 (63–153) |
| Femoral neck angle post-surgery * | 142° | 150° | 150° | 147° | 145° | 146.8 (142–150) |
| Post-surgery offset (mm) * | 24 | 19 | 18 | 20 | 17 | 19.6 (17–24) |
| Vertical distance nonunion–head post-surgery (mm) * | 65 | 55 | 38 | 52 | 48 | 51.6 (38–65) |
| Postoperative leg lengthening (mm) * | 8 | 12 | 6 | 6 | 8 | 8 (6–12) |
| Time to union (months) | 4 | 6 | 6 | 5 | 4 | 5 (4–6) |
| Harris Hip Score post-surgery * | 96 | 96 | 88 | 90 | 88 | 90 (88–96) |
| Study | N° of Patients | Design | Device Used | Follow Up | Results |
|---|---|---|---|---|---|
| Vaishya et al. [17] | 12 | Retrospective | A reversed DF-LCP with bone grafting | 13 months | 100% bone union rate at a mean of 9.5 months. No major complications. |
| Lotzien et al. [13] | 40 | Retrospective | Dynamic condylar screw plating along with bone grafting | 26 months | 93% bone union rate at 26 months. Thirteen patients required a second surgical procedure due to persistent nonunion (n: 1), persistent nonunion leading to implant failure (n: 9), deep infection (n: 2), and periprosthetic fracture (n: 1). Ultimately, 93% (n: 37) achieved union at a mean of 12 months. |
| De vries et al. [6] | 33 | Retrospective | A blade plate, along with cancellous bone grafting | 31 months | 97% bone union rate at a mean of 5 months. Complications included osteonecrosis of the femoral head (3%), refracture (3%), blade plate protrusion (3%), deep infection (3%), femoral neck fracture with fracture of blade plate (3%). |
| Giannoudis et al. [9] | 11 | Retrospective | A blade plate, along with cancellous bone grafting | 26 months | 100% bone union rate at 7 months (5 to 12). The blade plate failure was 7%. |
| Alfy et al. [27] | 26 | Prospective | 95° dynamic condylar screw | 36 months | There was only one nonunion (1/26). The mean HHS was 40 (range 25 to 65), which improved to 85 (range 55 to 95). All the results were excellent or good, and only one was poor. |
| Present Study | 5 | Prospective | 135°/150° dynamic hip screw. No bone grafting. | 12 months | 100% bone union rate (5/5). All excellent and good results. There were no major complications (it was a very small series). |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Delgado-Martínez, A.D.; Cañada-Oya, H.; Zarzuela-Jiménez, C. Dynamic, Over-Valgus Correction Without Osteotomy for Nonunion of Subtrochanteric Hip Fractures Using a Dynamic Hip Screw. Appl. Sci. 2025, 15, 1236. https://doi.org/10.3390/app15031236
Delgado-Martínez AD, Cañada-Oya H, Zarzuela-Jiménez C. Dynamic, Over-Valgus Correction Without Osteotomy for Nonunion of Subtrochanteric Hip Fractures Using a Dynamic Hip Screw. Applied Sciences. 2025; 15(3):1236. https://doi.org/10.3390/app15031236
Chicago/Turabian StyleDelgado-Martínez, Alberto D., Hermenegildo Cañada-Oya, and Cristina Zarzuela-Jiménez. 2025. "Dynamic, Over-Valgus Correction Without Osteotomy for Nonunion of Subtrochanteric Hip Fractures Using a Dynamic Hip Screw" Applied Sciences 15, no. 3: 1236. https://doi.org/10.3390/app15031236
APA StyleDelgado-Martínez, A. D., Cañada-Oya, H., & Zarzuela-Jiménez, C. (2025). Dynamic, Over-Valgus Correction Without Osteotomy for Nonunion of Subtrochanteric Hip Fractures Using a Dynamic Hip Screw. Applied Sciences, 15(3), 1236. https://doi.org/10.3390/app15031236






