Abstract
The clinical management of major depressive disorder remains hampered by a trial-and-error approach to treatment selection, a challenge that current diagnostic and static predictive models have failed to address. While artificial intelligence (AI) applications have focused on classifying a patient’s present state, they lack the ability to forecast the trajectory of their future response. This study addresses this critical gap by proposing a new theoretical framework that conceptualises depression treatment response as a complex dynamic system. Drawing a powerful analogy from the engineering field of structural health monitoring and damage prognosis, which forecasts the remaining useful life of a system, we shift the paradigm from diagnosis to prognosis. We introduce three core constructs: the Patient State Vector (PSV), a multimodal baseline of a patient’s clinical, biological, and digital phenotype; the Therapeutic Impulse Function (TIF), a formal representation of a treatment’s properties; and the Predicted Recovery Trajectory (PRT), the forecasted path of symptom severity over time. The central thesis of the framework is that a patient’s PRT emerges from the dynamic interaction between their initial PSV and a given TIF. We present a series of testable propositions, such as how early fluctuations in PRT can classify patients into distinct “dynamic phenotypes” predictive of long-term outcomes. By integrating mechanisms across neurobiology, behaviour, and pharmacology within an SHM-inspired framework, this prognostic theory aims to provide a new systems-based paradigm for personalised psychiatry, moving beyond static prediction to a mechanistic understanding of recovery. This cross-disciplinary adaptation illustrates how SHM-derived principles of state assessment, load modelling, and prognosis can inform new frontiers in predictive health modelling.
1. Introduction
The clinical management of major depressive disorder (MDD), a condition characterised by a persistent low mood and a loss of interest or pleasure, represents one of the most significant challenges in modern medicine. Despite the availability of numerous antidepressant medications, treatment selection remains a protracted trial-and-error process for a substantial proportion of patients [1,2,3,4,5]. Response rates to first-line pharmacotherapy are modest, with fewer than half of patients achieving a meaningful response and only approximately 30% reaching full remission [6,7]. This heterogeneity in treatment outcomes means that many individuals endure multiple, often unsuccessful, treatment trials—each lasting weeks or months—which prolongs their suffering and increases the socioeconomic burden of the illness [8,9].
A parallel challenge has been extensively addressed in engineering through the field of Structural Health Monitoring (SHM) and damage prognosis, where analogous problems of system heterogeneity, uncertain responses to load, and long-term performance forecasting have been studied for decades [1,2,3,4,10]. In response, a growing body of research has applied machine learning and other computational approaches to predict treatment outcomes, yet these efforts have largely failed to translate into clinical practice [5,11,12,13,14]. We argue that this is due to a fundamental conceptual limitation: the majority of current models are designed for static prediction. They attempt to classify a binary endpoint (e.g., responder vs. non-responder at 8 weeks) based on a snapshot of baseline characteristics [15,16,17,18,19,20,21]. This approach fails to capture the inherently dynamic nature of recovery and does not align with the clinical reality of monitoring patients’ progress over time. Therefore, the critical knowledge gap is not merely in prediction but in prognosis—the ability to forecast the entire future trajectory of a patient’s illness course under a specific treatment [22,23,24,25,26,27,28,29,30].
To address this gap, this study makes a theoretical contribution by proposing a new framework that reframes treatment response as a complex dynamic system. We introduce an interdisciplinary paradigm by drawing a powerful analogy with structural health monitoring (SHM), a field that has evolved from simple damage detection to the more sophisticated challenge of damage prognosis: forecasting the “remaining useful life” of a complex system based on its current state and future operational loads [31,32]. This framework exemplifies how SHM concepts, originally designed for forecasting the remaining useful life of engineered structures, can be generalised to other dynamic systems, including biomedical and clinical contexts. Applying this SHM-inspired prognostic lens to psychiatry, we conceptualise a patient’s mental state as a dynamic system, with treatment conceptualised as a targeted external load or perturbation designed to shift that system from a stable state of illness to a stable state of recovery [23,25,33,34]. This explicit transfer of SHM concepts to psychiatry illustrates the generality of prognosis as a systems problem: whether the system under observation is a bridge, an aircraft, or a human brain, the challenge remains to forecast its future trajectory given its current state and applied inputs.
To formalise this, we introduce three core theoretical constructs.
- Patient State Vector (PSV): A comprehensive, multimodal representation of a patient’s baseline state, integrating static clinical and biological data and high-frequency, real-world behavioural data from digital phenotyping [35,36].
- Therapeutic Impulse Function (TIF): A formal characterisation of a treatment’s properties, including its pharmacodynamic and pharmacokinetic profile, which acts as a specific input or “impulse” to the patient’s system [37].
- Predicted Recovery Trajectory (PRT): The forecasted, continuous path of a patient’s symptom severity over time, which emerges from the dynamic interaction between their unique PSV and a given TIF.
These constructs mirror the key informational components of SHM prognosis: PSV corresponds to the current state assessment, TIF to the future loading conditions, and PRT to the estimation of remaining useful life. By defining these constructs and the causal logic that connects them, this prognostic theory aims to provide a new systems-based paradigm for personalised psychiatry. It moves beyond static classification to a mechanistic understanding of recovery. It seeks to offer a conceptual foundation for developing the next generation of clinical decision support tools, ultimately helping to move the field from a reactive, trial-and-error model to a proactive, predictive science [1,2,3,4].
2. The Limits of the Current Static Prediction Paradigm
The urgent need to move beyond the trial-and-error approach in psychiatry has catalysed a significant body of research on computational models for predicting treatment outcomes in antidepressant therapy [11,12,13,14,38]. Leveraging machine learning (ML) algorithms, these studies have sought to identify individual-level predictors from a wide array of data types, including clinical features, neuroimaging, and genetics [15,17,18,19,20]. While these efforts are a vital step toward personalised medicine, their clinical translation has been minimal [5,11,12,13,14,39,40]. A similar challenge has been recognised in structural health monitoring (SHM), where early models focused on detecting or classifying damage states at single time points, but failed to capture the temporal evolution of degradation. Just as static classifiers in engineering overlooked fatigue progression or crack propagation, static prediction in psychiatry overlooks the dynamic reality of recovery. We argue that this translational gap is not merely a technical limitation but rather a fundamental conceptual issue rooted in the prevailing paradigm of static prediction [15,17,18,19,20]. This paradigm is characterised by several core limitations that prevent it from capturing the dynamic reality of clinical recovery.
First, the vast majority of current models are designed to predict a single, static endpoint, typically by dichotomising a continuous outcome into a binary classification (e.g., “responder” vs. “non-responder”) at a fixed time point, such as 8 or 12 weeks [15,17,18,19,20,21]. Although this approach is computationally convenient, it is a profound oversimplification of the therapeutic process. Recovery from depression is not a singular event but a longitudinal trajectory with significant intraindividual variability over time [41]. By collapsing this rich temporal information into a single binary outcome, static models discard crucial data about the speed of response, fluctuation patterns, and stability of improvement, all of which are clinically vital for treatment planning [42,43,44]. In SHM, an analogous limitation motivated the development of prognosis frameworks centred on remaining useful life (RUL), shifting the focus from binary damage detection to forecasting the full trajectory of structural degradation.
Second, the static paradigm struggles to account for the profound heterogeneity inherent in MDD [45,46,47]. Two patients can meet the diagnostic criteria for MDD with no overlapping symptoms, reflecting distinct underlying etiologies [45,48,49]. Data-driven models that treat MDD as a monolithic category often produce results with limited generalizability and poor predictive accuracy at the individual level [46,47,50]. Indeed, systematic reviews have noted that studies with higher methodological rigour tend to report lower accuracy, suggesting that many promising results are artefacts of small, homogeneous samples that do not generalise to real-world clinical populations [18,20].
Third, many of the most powerful machine learning models, particularly those based on deep learning, function as “black boxes”, where the internal logic connecting inputs to outputs is opaque to human users [17,18,51,52]. In a safety-critical field such as medicine, a prediction without a clear, interpretable rationale is clinically inert [15,16,17,18,19,20]. For a clinician to trust and act upon a model’s output—for instance, to choose one medication over another—they must be able to understand why the model made its recommendation [51,52]. The lack of model interpretability is a major barrier to clinical adoption and highlights the need for theory-driven approaches that can provide mechanistic insights, not just predictive accuracy [15,16,17,18,19,20]. The limitations of static prediction, therefore, resonate across disciplines: whether in monitoring aircraft structures or forecasting patient trajectories, static endpoints cannot represent the inherently dynamic nature of system evolution. What distinguishes the present work is not only the recognition of these shared limitations but also the proposal of an SHM-inspired theoretical framework that explicitly addresses them, providing a structured path from static prediction to dynamic prognosis.
Finally, the field is beset by methodological challenges, including heterogeneity of methods, small sample sizes, and a pervasive lack of external validation, which collectively limit the clinical utility of published models [17,18,20,53]. The absence of robust, replicable biomarkers means that even models with high reported accuracy often fail to perform well when applied to new and different patient populations [51,52,54,55]. These limitations underscore a fundamental point: simply applying more complex algorithms to the same static prediction problem is unlikely to yield clinically transformative tools in the near future. A true advance may require a conceptual shift away from predicting static endpoints and toward the more ambitious and clinically relevant goal of forecasting dynamic recovery trajectories [41,42,43,44].
This approach fails to capture the inherently dynamic nature of recovery and does not align with the clinical reality of monitoring patients’ progress over time. Our work builds on an emerging body of literature advocating for a dynamic systems view of psychiatric disorders, which conceptualises mental illness as a complex system of causally interacting symptoms and variables over time. Recent reviews have argued that this dynamic perspective is essential for understanding the non-linear transitions between illness and health [23,24,25,26,27,28,29,30], a concept we formalise in our framework as a state transition between “attractor states” (see Section 4.2.4). While network models have focused on the interactions between current symptoms, the prognostic challenge requires forecasting future trajectories—a goal that aligns with computational state-space models and forms the basis of our proposed framework.
3. A New Paradigm from Engineering: Damage Prognosis
Overcoming the limitations of static prediction requires a conceptual shift. We propose that such a shift can be achieved by importing a powerful framework from a seemingly disparate field: the engineering discipline of structural health monitoring (SHM) and, more specifically, its advanced application, damage prognosis (DP) [31,32]. SHM refers to the process of implementing a damage identification strategy for critical infrastructure, such as aircraft and bridges. By embedding a network of sensors within a structure, engineers can continuously monitor its integrity, detect the emergence of damage, such as fatigue cracks or corrosion, and use this real-time data to optimise maintenance and prevent catastrophic failure [31]. The SHM framework has thus become a generalisable paradigm for dynamic system prognosis, providing conceptual tools that can be adapted not only to engineered structures but also to other complex systems.
However, the ultimate goal of modern SHM extends beyond simple damage detection (a diagnostic task) to the more sophisticated challenge of damage prognosis (a forecasting task) [31]. While diagnosis answers the question, “What is the state of the system now?”, prognosis seeks to answer the far more valuable question, “Given the current state, how will the system behave in the future?” [31]. The central aim of DP is to forecast the “remaining useful life” (RUL) of a system, that is, to estimate how long it can continue to perform its intended function before a critical failure occurs. This allows engineers to move from reactive or scheduled maintenance to proactive, condition-based interventions that are both safer and more cost-effective [31].
The successful implementation of a DP framework is contingent on three core informational components [31]:
- Current State Assessment: A precise characterisation of the system’s current condition, including any existing damage. This was achieved using data collected from the SHM sensor network.
- Future Loading Conditions: An estimation of the operational and environmental loads that the system will be subjected to in the future (e.g., flight cycles for an aircraft and traffic patterns for a bridge).
- Damage Evolution Model: A predictive model, often physics-based or data-driven, that simulates the propagation of existing damage under estimated future loads.
By explicitly transferring these three informational components, state assessment, loading conditions, and damage evolution, to psychiatry, we illustrate how SHM principles can serve as a universal template for prognosis in complex, adaptive systems. We can conceptualise an individual patient as a complex system whose mental health state evolves over time. From this perspective, a psychiatric disorder such as MDD can be seen as an undesirable yet stable state of the system. A therapeutic intervention—whether pharmacological or psychological—is not merely a passive treatment but an active “load” or perturbation applied to the system with the goal of shifting it from a state of illness toward a state of sustained recovery [23,25,33,34]. Therefore, the central clinical challenge is not just to diagnose the current state but to make an accurate prognosis: to select the specific intervention that is most likely to induce a favourable trajectory toward remission for that particular individual. This reframing allows us to move beyond the static, cross-sectional view of treatment response and adopt a dynamic, longitudinal perspective that is better aligned with the realities of clinical care and research. Table 1 provides a direct conceptual mapping between the informational components of damage prognosis and the proposed psychiatric framework.

Table 1.
Conceptual Mapping Between Damage Prognosis and the Proposed Psychiatric Framework.
This mapping does not trivialise the differences between engineered and biological systems; instead, it demonstrates that SHM-derived constructs (state, load, prognosis) are sufficiently abstract to provide a common language for forecasting across domains.
4. A Prognostic Theory of Treatment Response
This section explicitly operationalises the analogy with SHM by aligning the three informational components of damage prognosis, state assessment, loading conditions, and remaining useful life, with psychiatric constructs. A theoretical contribution is defined by its ability to introduce new concepts or frameworks that explain phenomena and guide future research directions. Following the established principles of theory building, we articulate our framework through its three essential elements: core constructs (What), their relationships (How), and the underlying causal logic (Why) [56]. Figure 1 provides a visual representation of the framework.
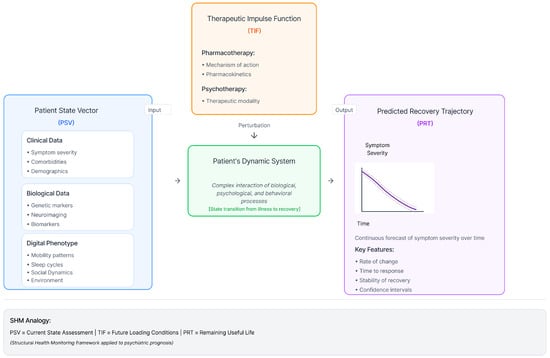
Figure 1.
Conceptual model of the prognostic framework. The Patient State Vector (PSV) and Therapeutic Impulse Function (TIF) serve as inputs to the patient’s dynamic system, which in turn generates a Predicted Recovery Trajectory (PRT) as its output.
4.1. The “What”: Core Theoretical Constructs
We propose three core constructs that serve as the building blocks of the prognostic framework, which are directly analogous to the components of damage prognosis.
Patient State Vector (PSV): The PSV is a comprehensive, multimodal, and time-varying representation of an individual’s state at the initiation of treatment. In SHM, this corresponds to continuous monitoring via embedded sensors; in psychiatry, digital phenotyping serves a comparable role, capturing fluctuations with similar temporal resolution. Critically, the PSV moves beyond traditional baseline measures by integrating data across multiple levels of analysis to create a high-dimensional characterisation of the patient. This includes:
- Clinical Data: Standardised assessments of symptom severity (e.g., PHQ-9 scores), diagnostic history, comorbidities, and demographic information [17,18]. This domain includes information typically collected in clinical trials and practice, captured longitudinally. Data sources include Electronic Health Records (EHRs) and Patient-Reported Outcome Measures (PROMs). Metrics include symptom severity (e.g., PHQ-9, HAM-D, tracked weekly), diagnostic history (e.g., ICD-10 codes for MDD and comorbidities), and demographics.
- Biological Data: Genotypic information (e.g., pharmacogenetic markers), neuroimaging data (e.g., fMRI, EEG), and other biomarkers (e.g., inflammatory markers, metabolic indices) that may moderate treatment response [46,47,54,55,57]. This domain captures neurobiological and physiological substrates. These data are often static or low-frequency. Data sources include genetic assays, neuroimaging, and blood samples. Metrics include pharmacogenetics (e.g., genotypes for CYP2D6, CYP2C19), neuroimaging (e.g., functional connectivity), and peripheral biomarkers (e.g., inflammatory markers, cortisol).
- Digital Phenotype Data: High-frequency, real-world behavioural data passively collected from personal devices, such as smartphones and wearables. This includes objective measures and feature-engineered metrics reflect behavioural domains such as mobility patterns (e.g., GPS/location entropy, time spent at home), social activity (e.g., call/text frequency, log metadata), and circadian rhythms (e.g., inferred sleep duration from phone usage patterns), sleep cycles, and physical activity, which provide a continuous and ecologically valid window into the behavioural manifestations of depression [35,36]. The integration of these dynamic real-world data streams is a key innovation of the PSV construct. Collecting these data streams, especially from personal devices, presents significant HCI challenges related to ensuring user engagement while minimising the burden [58].
As detailed in Table 2, the PSV can be conceptualised as having a “core” set of variables that are more readily available in clinical practice and an “extended” set for more intensive research contexts. This distinction enhances the perceived feasibility of the concept, allowing for pragmatic implementation, while also outlining a more ambitious scope for research.

Table 2.
Operationalisation of the Patient State Vector (PSV).
Therapeutic Impulse Function (TIF): The TIF is a formal characterisation of a given treatment, analogous to the “future loading conditions” in an engineering system. It conceptualises an intervention not as a static label (e.g., “Drug A”) but as a dynamic “impulse” or perturbation applied to the patient’s system. To move this beyond a simple label and make it computationally testable, we operationalise the TIF as a feature vector describing its quantitative properties. This allows a model to learn why treatments differ, not just that they do. This parallels the concept of future loading conditions in SHM, where the anticipated stresses on a structure are formally modelled to forecast its degradation. The TIF is defined by a set of parameters that describe its properties, such as:
- Pharmacotherapy TIF: A vector representation for a medication would include:
- –
- Mechanism of Action: A multi-hot encoded vector representing primary targets (e.g., for an SSRI, for an SNRI targeting Serotonin and Norepinephrine).
- –
- Half-life Elimination: A numerical feature (in hours) governing time to steady state.
- –
- Metabolism: A categorical feature for the primary CYP450 enzyme (e.g., CYP2D6), enabling direct modelling of gene-drug interactions with the PSV.
- –
- Dose: A normalised numerical feature for the prescribed daily dosage.
- Psychotherapy TIF: A vector representation for a psychotherapy would include:
- –
- Modality: A one-hot encoded vector (e.g., Cognitive Behavioural Therapy, Psychodynamic).
- –
- Dose and Schedule: Numerical features for session duration (minutes) and frequency (sessions per week). This structured TIF serves as a static or dynamic input to the prognostic model, allowing it to learn not only that treatments differ in outcome, but how and why they do so, based on their intrinsic properties.
Predicted Recovery Trajectory (PRT): The PRT is the primary output of the prognostic framework, representing the forecasted, continuous path of a patient’s symptom severity over time. Analogous to remaining useful life (RUL) in SHM, the PRT provides a probabilistic forecast of when a patient may reach recovery thresholds, mirroring the engineering task of estimating time to structural failure. Unlike a binary endpoint, the PRT is a longitudinal curve that characterises the expected course of recovery, including the initial rate of change, time to reach a response or remission threshold, and stability of recovery. The central thesis of this theory posits that PRT is an emergent property of the dynamic interaction between an individual’s unique PSV and a specific TIF.
This mapping illustrates that prognosis, whether for a bridge or a brain, relies on a universal triplet: state, perturbation, and trajectory. The framework is thus presented not a metaphor but an isomorphic transfer of prognostic logic. Taken together, PSV, TIF, and PRT form a direct analogue to the canonical triplet of state assessment, loading conditions, and damage evolution in SHM, thereby embedding psychiatric prognosis within a well-established engineering framework.
4.2. The “How”: Propositions of the Prognostic Framework
These propositions mirror the way in which SHM formalises the interaction between structural state, loading conditions, and damage evolution, thereby illustrating that the proposed psychiatric framework follows the same prognostic logic applied in engineering. We articulate the relationships between them through a series of formal and testable propositions. These propositions force a consideration of the concrete applications of the theory and increase the likelihood that subsequent research will constitute valid tests of its core arguments [56].
4.2.1. Proposition 1: The Patient State Vector (PSV) Predicts an Unperturbed Trajectory
In the absence of a new therapeutic impulse, the initial PSV may contain the necessary information to forecast the likely short-term course of illness. Specifically, components of the PSV reflecting greater biological and behavioural dysregulation (e.g., higher inflammatory markers, more severe sleep disruption, and greater social withdrawal as measured by digital phenotyping) are hypothesised to predict a PRT characterised by non-remission or worsening of symptoms. This is analogous to the current state assessment in SHM, where the system’s baseline damage state can predict its unperturbed degradation trajectory under normal loading.
4.2.2. Proposition 2: The Effect of a Therapeutic Impulse Function (TIF) on the Predicted Recovery Trajectory (PRT) Is Conditional upon the Patient State Vector (PSV)
This proposition posits a direct interaction effect between the patient and treatment. The efficacy of a specific TIF is not uniform across all patients but is moderated by the initial state of the individual. This parallels how in SHM, the response of a structure to a given load is conditional on its current state of integrity; identical loads can yield very different damage propagation depending on baseline defects.
Patients with PSV characterised by high inflammatory markers (e.g., C-reactive protein) will exhibit a more rapidly declining PRT when administered a TIF with known anti-inflammatory properties compared to a standard SSRI [54,55,57].
Patients with a PSV characterised by digital phenotype markers of anhedonia (e.g., low GPS location variance and reduced social communication) will show a more favourable PRT with a dopaminergic TIF than with a purely serotonergic TIF.
4.2.3. Proposition 3: Early Changes in PRT Are Predictive of Long-Term Treatment Outcomes
The initial response dynamics within the first weeks of treatment contain more predictive information for long-term outcomes than static baseline PSV alone. Analogously, in SHM, early indicators of crack propagation or vibration anomalies are often more predictive of remaining useful life than static baseline measurements. Patients can be classified into distinct “dynamic phenotypes” based on their early PRT (e.g., “fast responders”, “slow responders, and ”non-responders”). A rapid early decline in symptom severity, even if modest, is a strong predictor of eventual remission, whereas a flat or worsening initial PRT is a strong predictor of treatment failure.
4.2.4. Proposition 4: Clinical Recovery Represents a Critical State Transition (Bifurcation) in a Patient’s Dynamic System
The state of MDD can be modelled as a stable “attractor state” in a patient’s state space, characterised by self-reinforcing feedback loops between symptoms (e.g., insomnia leads to fatigue, which leads to anhedonia) [23,25,33,34]. An effective TIF acts as a sufficient perturbation to destabilise this illness attractor, pushing the system toward a “tipping point” or bifurcation, after which it can settle into an alternative, stable “recovery attractor” [59]. This corresponds to the way catastrophic failure in structures is modelled as a state transition or bifurcation event, once accumulated loads destabilise the existing equilibrium
A successful state transition from a depressive attractor to a recovery attractor will be preceded by a measurable increase in the variance of high-frequency digital phenotype signals (e.g., sleep duration and mobility) in the early phase of the PRT, a phenomenon known as critical slowing down [34]. An analogous phenomenon has been observed in SHM, where variance increases in vibration or strain signals can serve as early warning indicators of an approaching critical transition.
5. Causal Mechanisms and Multi-Level Integration
The propositions outlined above describe the expected relationships within this framework. A complete theoretical contribution should also provide a plausible causal rationale for the existence of these relationships [56]. Our framework is grounded in a multilevel integration of mechanisms spanning neurobiology, behavioural science, and dynamic systems theory. We posit that Dynamic Systems Theory provides the conceptual language to unify these different levels of analysis, allowing us to connect the biological and pharmacological drivers of change with their real-world behavioural manifestations into a single, coherent explanation. This multi-level integration mirrors the way SHM combines physical models of material degradation, sensor data, and load histories into a unified explanation of structural prognosis.
5.1. Neurobiological and Pharmacological Mechanisms
The delayed onset of action for most antidepressants provides strong evidence for adopting a dynamic systems view. TIF, such as the administration of a selective serotonin reuptake inhibitor (SSRI), does not produce an immediate therapeutic effect. Instead, it initiates a cascade of adaptive neurobiological changes over several weeks [54,55,57]. The initial TIF, which inhibits the serotonin transporter, perturbs the system, but therapeutic PRT emerges from the brain’s gradual adaptation to this change. This includes the downregulation of postsynaptic serotonin receptors, alterations in the hypothalamic–pituitary–adrenal (HPA) axis, and promotion of neurogenesis and synaptic plasticity, particularly in regions such as the hippocampus [37,54,55,57]. This is conceptually analogous to how, in SHM, an external load perturbs the system, and prognosis emerges not from the load alone but from the system’s adaptive response to it, such as crack-tip plasticity or redistribution of stress.
The PSV moderates this process. For instance, a patient with a PSV indicating high baseline HPA axis dysregulation (e.g., elevated cortisol) may be more sensitive to a TIF that effectively normalises this system [54,55,57]. Similarly, genetic polymorphisms included in the PSV, such as those affecting cytochrome P450 enzymes, directly alter the pharmacokinetics of a TIF, influencing drug metabolism and bioavailability, and thus shaping the PRT [37].
5.2. Behavioural and Psychological Mechanisms
These neurobiological changes do not occur in a vacuum; they manifest as observable behavioural and psychological change. The digital phenotype components of the PSV could provide a high-resolution, real-world readout of the behavioural expression of a patient’s internal state [35]. These are not merely correlates but direct manifestations of depressive symptomatology. For example, psychomotor retardation and anhedonia, which are core features of depression, are objectively captured by reduced mobility (lower step count, less location variance) and decreased social communication (fewer calls and texts) [36]. These passive data streams offer a continuous measure of the state of the system, allowing for the detection of subtle changes that precede shifts in self-reported mood.
Psychotherapeutic interventions can be conceptualised as TIF that directly target these behavioural and cognitive patterns. Cognitive Behavioural Therapy (CBT), for instance, perturbs the system by challenging maladaptive thought patterns and encouraging behavioural activation [34]. The “dose-response” relationship observed in psychotherapy, where most change occurs in early sessions, aligns with the concept of an early PRT being highly predictive of the final outcome [60]. This parallels SHM, where early anomalies in vibration or strain patterns often provide disproportionately strong information about the long-term prognosis of the structure.
5.3. Integration via Dynamic Systems Theory
Dynamic systems theory (DST) provides a mathematical and conceptual language to unify these multilevel mechanisms [23,25,33,59]. In DST, a system’s behaviour is described by its trajectory through a “state space” defined by its key variables (e.g., mood, stress, social activity). Stable patterns of behaviour, such as persistent depression or sustained wellness, are represented as “attractor states”—regions in the state space toward which the system naturally gravitates. A depressive attractor is “deep”, meaning that the system is resilient to minor positive events and tends to return to a depressed state.
From this perspective, an effective TIF is a perturbation strong enough to induce a “bifurcation”—a qualitative shift in the system’s dynamics that allows it to escape the depressive attractor and transition to a healthy one [59]. The PSV defines the initial “energy” required to escape the depressive attractor; a patient with a more resilient biological and behavioural profile (a “shallower” attractor) may require a less potent TIF to achieve this transition. Early PRT serves as an empirical indicator of the system’s stability; a trajectory that shows rapid change and increased variance may signal that the depressive attractor has been destabilised, presaging a successful transition to recovery [34]. This DST lens provides a mechanistic, non-linear explanation for the heterogeneity of treatment response and the often abrupt shifts between illness and health observed in clinical practice. Such bifurcations are also well recognised in engineering systems, where a structure under repeated loading may remain stable until reaching a critical threshold, at which point a sudden transition (e.g., crack propagation leading to fracture) occurs. This cross-domain convergence underscores that prognosis in both psychiatry and SHM can be understood through a common dynamical systems lens. Future work will formalise this DST framework mathematically using non-linear state–space or differential equation models, analogous to those applied in SHM damage evolution.
Specifically, this could involve adapting formulations commonly used in SHM, such as stochastic differential equations for damage evolution, state–space Kalman filtering, or probabilistic prognosis models, to represent transitions between depressive and recovery attractors in the patient’s dynamic system.
6. Implications, Future Directions, and a Research Agenda
The formulation of a prognostic theory of treatment response is not merely an academic exercise; it is a call for a fundamental shift in how we conceptualise, investigate, and ultimately practice personalised psychiatry. By moving beyond the prevailing paradigm of static prediction, this framework offers a new lens through which to view the challenge of treatment heterogeneity and provides a structured path toward a more dynamic, predictive, and mechanistic approach to mental healthcare. These implications are not confined to psychiatry. By showing how SHM concepts can be translated into a new clinical domain, this work highlights the generalisability of prognosis paradigms across fields and opens opportunities for reciprocal learning between biomedical and engineering sciences.
6.1. Clinical and Human-Computer Interaction (HCI) Implications
The primary goal of this prognostic framework was to enhance clinical decision-making. In a clinical setting, a validated prognostic model could function as a sophisticated decision-support tool. Rather than selecting a treatment based on population-level guidelines and trial-and-error, a clinician could input a patient’s unique PSV and simulate the likely PRTs for several different TIFs (e.g., various antidepressants or psychotherapies). This would allow for a collaborative discussion with the patient about the potential speed of recovery, likelihood of remission, and specific trajectory of improvement, thereby setting more realistic expectations and fostering a stronger therapeutic alliance [11,12,13,14].
However, the translation of such a tool into practice is fundamentally an HCI challenge that requires further research. The design of the interface through which clinicians and patients interact with prognostic forecasts is critical. The system must present complex probabilistic information in an intuitive and transparent manner, avoiding deterministic oversimplification [58]. For example, visualising multiple potential PRTs with confidence intervals could help communicate uncertainty effectively, which is a key design challenge in human-centred AI for mental health. Furthermore, the integration of such tools into existing clinical workflows, such as electronic health records (EHRs), must be seamless to avoid creating additional burdens for practitioners [19,21]. Human-centred design principles are essential to ensure that these prognostic tools are not only accurate but also usable, trustworthy, and genuinely supportive of the clinical relationship.
Illustrative Use Case
To illustrate the envisioned clinical application, consider a follow-up consultation in which a clinician uses the prognostic decision support interface with a patient. The model, having been fed the patient’s PSV, forecasts a flattening in the predicted recovery trajectory (PRT) over the next four weeks and, using XAI methods (see Section 6.2.1), highlights disrupted sleep regularity and reduced mobility (from the digital phenotype) as primary contributing factors.
Guided by this insight, the clinician and patient review the recent behavioural data together. The tool functions as a shared visual aid, facilitating a collaborative conversation. The clinician might say, “You can see here how your sleep patterns have become more irregular in the last week, which the model suggests is a strong predictor of this ’flattening’ curve. Let’s discuss what might be contributing to this.” This interaction exemplifies how the proposed system can function as an interpretive, collaborative aid—reframing the tool from a top-down predictor to a bottom-up facilitator of shared understanding, empowering the patient, and supporting clinical reasoning rather than replacing human judgement.
6.2. Methodological Implications
Operationalising this theory requires a significant evolution in research methodology, moving from static classification to dynamic time-series forecasting. The theory is incomplete without a concrete and testable empirical framework. We provide such a framework here, moving the concept from an “architectural blueprint” to an actionable plan.
6.2.1. A Computational Architecture for Prognosis
The task of forecasting a PRT from a multi-modal, asynchronous, and irregularly-sampled PSV is computationally non-trivial. The appropriate model must be (a) sequence-aware, to handle time-series data, and (b) time-aware, to learn from irregular time gaps (e.g., a 7-day gap between clinical visits is different from a 10-day gap).
Therefore, we propose that the theoretical propositions are best tested using a time-aware Long Short-Term Memory (LSTM) network. LSTMs, a type of Recurrent Neural Network (RNN), are designed to learn long-range temporal dependencies by maintaining an internal “memory state”, making them ideally suited for modelling the path-dependent nature of recovery. A “time-aware” variant (e.g., using time-decay gates) explicitly models the time elapsed between observations, allowing the model to learn that a symptom score from yesterday is more relevant than one from three weeks ago. This architecture can be implemented with separate input pathways to fuse the static features (e.g., genetics, TIF vector) with the dynamic time-series (e.g., weekly PHQ-9, daily mobility). This model can be paired with Explainable AI (XAI) techniques (e.g., SHAP, attention-based saliency) to move beyond a “black box” and identify which PSV features and which time-points are driving a given PRT forecast.
6.2.2. A Protocol for Empirical Validation
A rigorous and transparent protocol is essential for testing the theory’s propositions and ensuring model reliability. This protocol provides the explicit pathway to falsifiability for the theory.
- Data Preprocessing: All continuous input features (e.g., step count, symptom scores) will be standardised (e.g., z-score normalisation). High-frequency digital phenotype data will be aggregated to a consistent temporal resolution (e.g., daily summaries).
- Validation: To prevent information leakage and ensure the model generalises to unseen patients, a patient-level, nested cross-validation (CV) scheme must be employed. The outer loop splits patients into training and test sets; the inner loop performs hyperparameter tuning on a validation set carved from the training set.
- Evaluation Metrics: The evaluation must reflect the prognostic goal of forecasting the entire trajectory. This provides the direct mechanism for falsifiability; the theory’s propositions (e.g., Proposition 3) are supported only if a dynamic model (like the LSTM) significantly outperforms static benchmarks. Key metrics include:
- –
- Trajectory-wise Root Mean Squared Error (RMSE) or Mean Absolute Error (MAE): The average error across all forecasted time points. This is the primary measure of path accuracy.
- –
- Endpoint MAE: The error at the final time point only (e.g., week 12). This allows for direct comparison with traditional static models.
- –
- Dynamic Time Warping (DTW): A metric that measures the similarity between two temporal sequences, even if they are out of phase. This assesses if the model correctly predicted the shape of recovery (e.g., “fast-responder”) even if its timing was slightly off.
- Benchmarks: To prove its value, the proposed model must be benchmarked against simpler alternatives, as outlined in Table 3.
 Table 3. Model Evaluation Benchmarks.
Table 3. Model Evaluation Benchmarks.
6.3. Ethical Considerations
A prognostic framework, by its nature, raises profound ethical questions that must be addressed proactively. The collection of continuous multimodal data for the PSV requires stringent privacy and data security protocols to protect highly sensitive personal information [61]. The principles of informed consent must be adapted for a world of continuous data collection, ensuring that patients have ongoing control and understanding of how their data are used [62,63,64].
Moreover, AI-built prognostic models are susceptible to algorithmic bias, potentially learning and amplifying existing societal inequities present in the training data. Models trained on demographically limited datasets may be less accurate for underrepresented populations, exacerbating health disparities. Therefore, ensuring fairness, accountability, and transparency is not an optional add-on but a core requirement for the ethical development and deployment of these technologies, as emphasised by global health organisations [65].
A prognostic framework, by its nature, raises profound ethical questions that must be addressed proactively. A brief discussion is insufficient for a framework that relies on such sensitive, continuous data. We therefore propose a practical, multi-part governance framework as a core component of the methodology.
- Data Privacy and Informed Consent: The continuous, passive nature of digital phenotyping is incompatible with traditional, one-time consent models.
- Methodological Solution: We propose implementing a dynamic consent interface within any data collection application. This would allow patients granular control to view, pause, or withdraw specific data streams at any time. This must be paired with privacy-preserving machine learning techniques, such as federated learning, where the model is trained on the user’s device, and only anonymised model weights—not raw personal data—are sent to a central server.
- Algorithmic Bias and Fairness: AI models trained on historical data risk learning and amplifying existing societal biases and health disparities, which can lead to poor performance in underrepresented populations.
- Methodological Solution: A mandatory algorithmic bias audit must be part of the validation protocol (Section 6.2.2). This involves disaggregating all key performance metrics (e.g., Trajectory RMSE) across demographic subgroups (e.g., race, gender, socioeconomic status). If significant performance disparities are identified, mitigation strategies (e.g., data reweighting, fairness constraints) must be employed and reported transparently.
- Accountability and Responsibility: If a model’s forecast contributes to an adverse outcome, who is responsible?
- Methodological Solution: The framework must establish clear lines of accountability. The model must be legally and ethically framed as a Clinical Decision Support (CDS) tool, not an autonomous medical device. The final clinical judgement and responsibility must always reside with the human clinician. The system’s interface and documentation must clearly state its probabilistic nature, its limitations, and its role as an assistive tool to augment, rather than replace, professional expertise.
6.4. Limitations of the Prognostic Framework
While this prognostic theory offers a new paradigm, it is essential to acknowledge its inherent challenges and limitations that must be addressed in future research. The primary weakness is the immense practical difficulty of collecting the complete multimodal data required to fully operationalise the Patient State Vector (PSV). Integrating genetic, neuroimaging, clinical, and high-frequency digital phenotyping data for a single individual is a resource-intensive task that is currently only feasible in well-funded research settings and not in routine clinical practice [17,18].
Furthermore, the complexity of the framework is a double-edged sword. Although it aims to capture the intricate reality of treatment response, this complexity increases computational demands and may reduce interpretability. There is a significant risk that the resulting models could become “black boxes”, which would undermine the goal of providing clinicians with transparent and trustworthy decision support [51,52]. Therefore, the development of explainable AI (XAI) methods is not an optional addition but a core necessity for the successful translation of this framework.
Finally, this framework is, by design, a high-level conceptual framework. It does not specify the precise mathematical forms of the interactions between the PSV and TIF or the exact algorithms best suited for forecasting the PRT. These crucial details must be determined through the iterative process of empirical testing outlined in our research agenda. This paper provides an architectural blueprint, but significant engineering and construction work remains to be done. This situation is analogous to SHM, where comprehensive sensing and modelling of all possible degradation mechanisms is rarely feasible in practice. Both fields, therefore, face a balance between complexity, interpretability, and practical applicability. However, this shared challenge also presents a unique opportunity. Reciprocally, testing SHM-inspired prognosis frameworks in highly complex biological systems may feed back into SHM by stress-testing models under extreme heterogeneity and uncertainty.
6.5. Boundary Conditions and Scope of the Theory
A robust theory must also acknowledge its boundaries—the “Who, Where, and When” that define its scope of applicability [56]. This prognostic framework was initially conceptualised for Major Depressive Disorder (MDD) in outpatient settings, given the high rates of treatment heterogeneity and the availability of longitudinal data in this population. However, its applicability is likely to be broader. The core principles: characterising an initial state, applying a perturbation, and forecasting a trajectory could potentially be adapted for other relapsing–remitting conditions, such as bipolar disorder or anxiety disorders. Furthermore, although developed with pharmacotherapy and psychotherapy in mind, the TIF construct is flexible enough to model other interventions, such as neuromodulation. The precise boundary conditions of this theory are ultimately an empirical question, representing a key avenue for future research, as outlined below. More broadly, this suggests that prognosis, whether in psychiatry or SHM, is best understood as a transferable systems problem defined by three universal elements: state assessment, applied perturbations, and forecast trajectories.
To be explicit, while this framework was conceptualised for Major Depressive Disorder (MDD), its applicability is likely broader, but not universal. The core principles—charac- terising an initial state (PSV), applying a perturbation (TIF), and forecasting a trajectory (PRT)—may be adapted for other relapsing-remitting conditions that share key features with MDD, such as: (1) high treatment heterogeneity, (2) a longitudinal course where the trajectory of recovery is clinically meaningful, and (3) the availability of high-frequency behavioural data (e.g., digital phenotyping). Conditions such as bipolar disorder, post-traumatic stress disorder, and anxiety disorders are strong candidates.
However, the framework may be less applicable to acute, non-relapsing conditions. The generalisability of the specific PSV features and TIF parameters is an empirical question; a PSV for MDD will likely differ significantly from a PSV for bipolar disorder (which would need to prioritise different features, such as those related to mania). The framework’s core contribution is the prognostic logic (PSV + TIF = PRT), which we posit is generalisable, even if the specific variables are not.
6.6. A Research Agenda for a Prognostic Psychiatry
This theoretical framework is not an endpoint but rather a starting point. Its value will be determined by the empirical research it inspires in the future. We conclude by proposing a concrete, multistage research agenda to test, refine, and ultimately translate this theory into practice.
- Establishment of Longitudinal, Multi-Modal Cohorts: The primary focus should be on creating large-scale, openly shared datasets. These studies must collect longitudinal data from patients with MDD, capturing the full PSV (clinical, biological, and high-frequency digital phenotype data) before, during, and after various treatment interventions (TIFs).
- Development and Validation of Prognostic Models: Using these new datasets, the next step is to develop and rigorously validate computational models that can forecast individual PRTs. This work (which will be the subject of our subsequent paper) should focus on time-series models (e.g., LSTMs) and benchmark their prognostic accuracy against the current static prediction methods.
- Testing of Causal Propositions: The propositions of the theory should be empirically tested. For example, studies should investigate whether early changes in the PRT (Proposition 3) are indeed more predictive than baseline data alone and whether specific PSV-TIF interactions (Proposition 2) can be identified that lead to differential treatment outcomes.
- Human-Centred Design and Implementation Studies: Parallel to model development, HCI research is required to co-design and evaluate clinical decision support tools based on this framework. Usability studies, qualitative interviews with clinicians and patients, and pilot implementation trials are necessary to understand how to ethically and effectively integrate prognostic information into clinical care.
By pursuing this agenda, the field can begin to build an empirical and methodological foundation for a truly personalised and prognostic psychiatry, moving one step closer to ensuring that every patient receives the right treatment at the right time. Conversely, applying SHM-derived prognosis frameworks to complex human systems can provide valuable feedback to SHM itself, offering new insights into modelling uncertainty, non-linearity, and heterogeneity in real-world data and, in turn, inform the refinement of SHM methodologies.
Author Contributions
Conceptualisation, H.N.-W.; methodology, H.N.-W., L.D. and I.S.V.; validation, H.N.-W., L.D. and I.S.V.; formal analysis, H.N.-W., L.D. and I.S.V.; investigation, H.N.-W., L.D. and I.S.V.; resources, H.N.-W., L.D. and I.S.V.; writing—original draft preparation, H.N.-W., L.D. and I.S.V.; writing—review and editing, H.N.-W., L.D. and I.S.V.; supervision, L.D. and I.S.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable. This study is a theoretical contribution that does not involve research on human or animal participants.
Informed Consent Statement
Not applicable. No participants were involved in this theoretical study.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Acknowledgments
The authors acknowledge the partial use of generative AI and/or LLM tools (Paperpal by Editage) for copy-editing to improve language and readability in accordance with emerging best practices in academic publishing. The authors are fully responsible for the content, accuracy, and integrity of this study.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| AI | Artificial Intelligence |
| CBT | Cognitive Behavioural Therapy |
| CRP | C-reactive Protein |
| CYP2D6 | Cytochrome P450 2D6 |
| DP | Damage Prognosis |
| DST | Dynamic Systems Theory |
| EEG | Electroencephalography |
| EHR | Electronic Health Record |
| fMRI | Functional Magnetic Resonance Imaging |
| GPS | Global Positioning System |
| HAM-D | Hamilton Depression Rating Scale |
| HCI | Human-Computer Interaction |
| HPA | Hypothalamic-Pituitary-Adrenal (axis) |
| LSTM | Long Short-Term Memory (networks) |
| MDD | Major Depressive Disorder |
| ML | Machine Learning |
| PHQ-9 | Patient Health Questionnaire-9 |
| PRT | Predicted Recovery Trajectory |
| PSV | Patient State Vector |
| RNNs | Recurrent Neural Networks |
| RULs | Remaining Useful Life |
| SHM | Structural Health Monitoring |
| SSRI | Selective Serotonin Reuptake Inhibitor |
| TIF | Therapeutic Impulse Function |
| WHO | World Health Organization |
| XAI | Explainable AI |
References
- Abrahams, A.B.; Beckenstrom, A.; Browning, M.; Dias, R.; Goodwin, G.M.; Gorwood, P.; Kingslake, J.; Morriss, R.; Reif, A.; Ruhe, H.G.; et al. Exploring the incidence of inadequate response to antidepressants in the primary care of depression. Eur. Neuropsychopharmacol. 2024, 83, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Penn, E.M.; Tracy, D.K. The drugs don’t work? Antidepressants and the current and future pharmacological management of depression. Ther. Adv. Psychopharmacol. 2012, 2, 179–188. [Google Scholar] [CrossRef]
- Alharbi, A. Treatment-resistant depression: Therapeutic trends, challenges, and future directions. Patient Prefer. Adherence 2012, 6, 369. [Google Scholar] [CrossRef] [PubMed]
- Zelek-Molik, A.; Litwa, E. Trends in research on novel antidepressant treatments. Front. Pharmacol. 2025, 16, 1544795. [Google Scholar] [CrossRef]
- Voineskos, D.; Daskalakis, Z.J.; Blumberger, D.M. Management of treatment-resistant depression: Challenges and opportunities. Neuropsychiatr. Dis. Treat. 2020, 16, 221–234. [Google Scholar] [CrossRef]
- Rush, A.J.; Trivedi, M.H.; Wisniewski, S.R.; Nierenberg, A.A.; Stewart, J.W.; Warden, D.; Niederehe, G.; Thase, M.E.; Lavori, P.W.; Lebowitz, B.D.; et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: A STAR* D report. Am. J. Psychiatry 2006, 163, 1905–1917. [Google Scholar] [CrossRef]
- Trivedi, M.H.; Rush, A.J.; Wisniewski, S.R.; Nierenberg, A.A.; Warden, D.; Ritz, L.; Norquist, G.; Howland, R.H.; Lebowitz, B.; McGrath, P.J.; et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR* D: Implications for clinical practice. Am. J. Psychiatry 2006, 163, 28–40. [Google Scholar] [CrossRef]
- Crown, W.H.; Finkelstein, S.; Berndt, E.R.; Ling, D.; Poret, A.W.; Rush, A.J.; Russell, J.M. The impact of treatment-resistant depression on health care utilization and costs. J. Clin. Psychiatry 2002, 63, 963–971. [Google Scholar] [CrossRef]
- Lépine, J.P.; Briley, M. The increasing burden of depression. Neuropsychiatr. Dis. Treat. 2011, 7, 3. [Google Scholar] [CrossRef] [PubMed]
- Ozomaro, U.; Wahlestedt, C.; Nemeroff, C.B. Personalized medicine in psychiatry: Problems and promises. BMC Med. 2013, 11, 132. [Google Scholar] [CrossRef]
- Baminiwatta, A. Global trends of machine learning applications in psychiatric research over 30 years: A bibliometric analysis. Asian J. Psychiatry 2022, 69, 102986. [Google Scholar] [CrossRef]
- Iyortsuun, N.K.; Kim, S.; Jhon, M.; Yang, H.; Pant, S. A review of machine learning and deep learning approaches on mental health diagnosis. Healthcare 2023, 11, 285. [Google Scholar] [CrossRef]
- Sun, J.; Lu, T.; Shao, X.; Han, Y.; Xia, Y.; Zheng, Y.; Wang, Y.; Li, X.; Ravindran, A.; Fan, L.; et al. Practical AI application in psychiatry: Historical review and future directions. Mol. Psychiatry 2025, 30, 4399–4408. [Google Scholar] [CrossRef]
- Shatte, A.; Hutchinson, D.; Teague, S. Machine learning in mental health: A scoping review of methods and applications. Psychol. Med. 2019, 49, 1426–1448. [Google Scholar] [CrossRef] [PubMed]
- Karvelis, P.; Charlton, C.E.; Allohverdi, S.G.; Bedford, P.; Hauke, D.J.; Diaconescu, A.O. Computational approaches to treatment response prediction in major depression using brain activity and behavioral data: A systematic review. Netw. Neurosci. 2022, 6, 1066–1103. [Google Scholar] [CrossRef]
- Li, H.; Song, S.; Wang, D.; Zhang, D.; Tan, Z.; Lian, Z.; Wang, Y.; Zhou, X.; Pan, C.; Wu, Y. Treatment response prediction for major depressive disorder patients via multivariate pattern analysis of thalamic features. Front. Comput. Neurosci. 2022, 16, 837093. [Google Scholar] [CrossRef]
- Ntam, V.A.; Huebner, T.; Steffens, M.; Scholl, C. Machine learning approaches in the therapeutic outcome prediction in major depressive disorder: A systematic review. Front. Psychiatry 2025, 16, 1588963. [Google Scholar] [CrossRef]
- Curtiss, J.; DiPietro, C.P. Machine learning in the prediction of treatment response for emotional disorders: A systematic review and meta-analysis. Clin. Psychol. Rev. 2025, 120, 102593. [Google Scholar] [CrossRef] [PubMed]
- Sheu, Y.; Magdamo, C.; Miller, M.; Das, S.; Blacker, D.; Smoller, J.W. Ai-assisted prediction of differential response to antidepressant classes using electronic health records. npj Digit. Med. 2023, 6, 73. [Google Scholar] [CrossRef]
- Sajjadian, M.; Lam, R.W.; Milev, R.; Rotzinger, S.; Frey, B.N.; Soares, C.N.; Parikh, S.V.; Foster, J.A.; Turecki, G.; Müller, D.J.; et al. Machine learning in the prediction of depression treatment outcomes: A systematic review and meta-analysis. Psychol. Med. 2021, 51, 2742–2751. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Vekaria, V.; Wang, F.; Cukor, J.; Su, C.; Adekkanattu, P.; Brandt, P.; Jiang, G.; Kiefer, R.C.; Luo, Y.; et al. Using machine learning to predict antidepressant treatment outcome from electronic health records. Psychiatr. Res. Clin. Pract. 2023, 5, 118–125. [Google Scholar] [CrossRef]
- Stephan, K.E.; Bach, D.R.; Fletcher, P.C.; Flint, J.; Frank, M.J.; Friston, K.J.; Heinz, A.; Huys, J.M.; Owen, M.J.; Binder, E.B.; et al. Charting the landscape of computational psychiatry. Lancet Psychiatry 2017, 4, 324–334. [Google Scholar] [CrossRef]
- Scheffer, M.; Bockting, C.; Borsboom, D.; Cools, R.; Delecroix, C.; Hartmann, J.; Kendler, K.S.; Leemput, I.v.d.; Maas, H.L.J.v.d.; Nes, E.H.v.; et al. A dynamical systems view of psychiatric disorders—Theory. JAMA Psychiatry 2024, 81, 618. [Google Scholar] [CrossRef]
- Gauld, C.; Depannemaecker, D. Dynamical systems in computational psychiatry: A toy-model to apprehend the dynamics of psychiatric symptoms. Front. Psychol. 2023, 14, 1099257. [Google Scholar] [CrossRef]
- Bosl, W.J.; Enlow, M.B.; Nelson, C.A. A dynamical systems framework for precision psychiatry. npj Digit. Med. 2025, 8, 586. [Google Scholar] [CrossRef]
- Öngür, D.; Paulus, M.P. Embracing complexity in psychiatry—From reductionistic to systems approaches. Lancet Psychiatry 2025, 12, 220–227. [Google Scholar] [CrossRef]
- Voerman, S.A.; Strijbos, D.; Staring, A.B.P.; Boer, F.d.; Dijk, M.v.; Driessen, J.; Glas, G.; Goekoop, R.; Mulder, A.; Tromp, N.; et al. Problem-sustaining patterns: Redesigning the concept of mental disorder. Front. Psychiatry 2025, 16, 1382915. [Google Scholar] [CrossRef]
- Friston, K.; Redish, A.D.; Gordon, J.A. Computational nosology and precision psychiatry. Comput. Psychiatry 2017, 1, 2. [Google Scholar] [CrossRef] [PubMed]
- Nelson, B.; McGorry, P.D.; Wichers, M.; Wigman, J.T.W.; Hartmann, J. Moving from static to dynamic models of the onset of mental disorder. JAMA Psychiatry 2017, 74, 528. [Google Scholar] [CrossRef] [PubMed]
- Does, F.H.S.v.d.; Nagamine, M.; Kitano, M.; Saito, T.; Wee, N.J.v.d.; Vermetten, E.; Giltay, E.J. The potential of personalized post-traumatic stress disorder networks. Psychiatry Clin. Psychopharmacol. 2025, 35, S141–S151. [Google Scholar] [CrossRef] [PubMed]
- Farrar, C.R.; Lieven, N.A.J. Damage prognosis: The future of structural health monitoring. Philos. Trans. R. Soc. A Math. Phys. Eng. Sci. 2007, 365, 623–632. [Google Scholar] [CrossRef]
- Worden, K.; Dulieu-Barton, J.M. An overview of intelligent fault detection in systems and structures. Struct. Health Monit. 2004, 3, 85–98. [Google Scholar] [CrossRef]
- Durstewitz, D.; Huys, Q.J.M.; Koppe, G. Psychiatric illnesses as disorders of network dynamics. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 2021, 6, 865–876. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.M.; Andrews, L.A. A complex systems approach to the study of change in psychotherapy. BMC Med. 2020, 18, 197. [Google Scholar] [CrossRef]
- Insel, T.R. Digital phenotyping: An overarching framework to capture our extended mental states. Lancet Psychiatry 2018, 5, 194–195. [Google Scholar] [CrossRef]
- Torous, J.; Onnela, J.; Keshavan, M.S. New dimensions and new tools to realize the potential of rdoc: Digital phenotyping via smartphones and connected devices. Transl. Psychiatry 2017, 7, e1053. [Google Scholar] [CrossRef]
- Hiemke, C.; Baumann, P.; Bergemann, N.; Conca, A.; Dietmaier, O.; Egberts, K.; Fric, M.; Gerlach, M.; Greiner, C.; Gründer, G.; et al. AGNP consensus guidelines for therapeutic drug monitoring in psychiatry: Update 2011. Pharmacopsychiatry 2011, 44, 195–235. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Ragguett, R.M.; Mansur, R.B.; Boutilier, J.J.; Rosenblat, J.D.; Trevizol, A.P.; McIntyre, R.S. Applications of machine learning algorithms to predict antidepressant treatment response in patients with major depressive disorder: A systematic review and meta-analysis. J. Affect. Disord. 2018, 241, 573–584. [Google Scholar] [CrossRef]
- Rost, N.; Binder, E.B.; Brückl, T. Predicting treatment outcome in depression: An introduction into current concepts and challenges. Eur. Arch. Psychiatry Clin. Neurosci. 2022, 273, 113–127. [Google Scholar] [CrossRef]
- Uyar, A.; Gönül, A.S. New and emerging pharmacologic treatments for mdd. Front. Psychiatry 2025, 16, 1621887. [Google Scholar] [CrossRef] [PubMed]
- Elsaesser, M.; Feige, B.; Kriston, L.; Schumacher, L.; Peifer, J.; Hautzinger, M.; Härter, M.; Schramm, E. Longitudinal clusters of long-term trajectories in patients with early-onset chronic depression: 2 years of naturalistic follow-up after extensive psychological treatment. Psychother. Psychosom. 2023, 93, 65–74. [Google Scholar] [CrossRef]
- Frässle, S.; Marquand, A.F.; Schmaal, L.; Dinga, R.; Veltman, D.J.; Wee, N.J.v.d.; Tol, M.v.; Schöbi, D.; Penninx, B.W.; Stephan, K.E. Predicting individual clinical trajectories of depression with generative embedding. NeuroImage Clin. 2020, 26, 102213. [Google Scholar] [CrossRef]
- Lai, W.; Liao, Y.; Zhang, H.; Zhao, H.; Li, Y.; Chen, R.; Shi, G.; Liu, Y.; Hao, J.; Li, Z.; et al. The trajectory of depressive symptoms and the association with quality of life and suicidal ideation in patients with major depressive disorder. BMC Psychiatry 2025, 25, 310. [Google Scholar] [CrossRef] [PubMed]
- Schmaal, L.; Marquand, A.F.; Rhebergen, D.; Tol, M.v.; Ruhé, H.G.; Wee, N.J.v.d.; Veltman, D.J.; Penninx, B.W. Predicting the naturalistic course of major depressive disorder using clinical and multimodal neuroimaging information: A multivariate pattern recognition study. Biol. Psychiatry 2015, 78, 278–286. [Google Scholar] [CrossRef]
- Fried, E.I. The 52-symptom challenge: The measurement of depression. Lancet Psychiatry 2017, 4, 181–183. [Google Scholar] [CrossRef]
- Kang, S.; Cho, S. Neuroimaging biomarkers for predicting treatment response and recurrence of major depressive disorder. Int. J. Mol. Sci. 2020, 21, 2148. [Google Scholar] [CrossRef]
- Liu, R.; Hou, X.; Liu, S.; Zhou, Y.; Zhou, J.; Qiao, K.; Qi, H.; Li, R.; Yang, Z.; Zhang, L.; et al. Predicting antidepressant response via local-global graph neural network and neuroimaging biomarkers. npj Digit. Med. 2025, 8, 515. [Google Scholar] [CrossRef] [PubMed]
- Athira, K.V.; Bandopadhyay, S.; Samudrala, P.K.; Naidu, V.; Lahkar, M.; Chakravarty, S. An overview of the heterogeneity of major depressive disorder: Current knowledge and future prospective. Curr. Neuropharmacol. 2020, 18, 168–187. [Google Scholar] [CrossRef]
- Lynall, M.; McIntosh, A.M. The heterogeneity of depression. Am. J. Psychiatry 2023, 180, 703–704. [Google Scholar] [CrossRef]
- Li, X.; Pei, C.; Wang, X.; Wang, H.; Tian, S.; Yao, Z.; Lü, Q. Predicting neuroimaging biomarkers for antidepressant selection in early treatment of depression. J. Magn. Reson. Imaging 2021, 54, 551–559. [Google Scholar] [CrossRef]
- Joyce, D.W.; Kormilitzin, A.; Smith, K.; Cipriani, A. Explainable artificial intelligence for mental health through transparency and interpretability for understandability. npj Digit. Med. 2023, 6, 6. [Google Scholar] [CrossRef]
- Probierz, B.; Straś, A.; Rodek, P.; Kozak, J. Explainable ai in psychiatry. In Explainable Artificial Intelligence for Sustainable Development; Routledge: London, UK, 2025; pp. 245–262. [Google Scholar] [CrossRef]
- Yadav, P.; Kumar, Y.; Kumar, S. Evaluating the impact of machine learning models on adult major depressive disorder using conventional treatment strategies: A systematic review approach. Discov. Public Health 2025, 22, 410. [Google Scholar] [CrossRef]
- Cai, H.; Song, H.; Yang, Y.; Xiao, Z.; Zhang, X.; Jiang, F.; Liu, H.; Tang, Y. Big-five personality traits and depression: Chain mediation of self-efficacy and walking. Front. Psychiatry 2024, 15. [Google Scholar] [CrossRef]
- Chen, J.; Huang, H. The influence of big five personality traits on depression and suicidal behavior. In The Association Between Depression and Suicidal Behavior; InTechOpen: Rijeka, Croatia, 2024. [Google Scholar] [CrossRef]
- Whetten, D.A. What constitutes a theoretical contribution? Acad. Manag. Rev. 1989, 14, 490–495. [Google Scholar] [CrossRef]
- Watson, M.; Protzner, A.B.; McGirr, A. Five-factor personality and antidepressant response to intermittent theta burst stimulation for major depressive disorder. Transcranial Magn. Stimul. 2025, 5, 100196. [Google Scholar] [CrossRef]
- Thieme, A.; Hanratty, M.; Lyons, M.; Palacios, J.; Marques, R.F.; Morrison, C.; Doherty, G. Designing human-centered AI for mental health: Developing clinically relevant applications for online CBT treatment. ACM Trans. Comput.-Hum. Interact. 2022, 29, 1–44. [Google Scholar] [CrossRef]
- Salvi, J.D.; Rauch, S.L.; Baker, J.T. Behavior as physiology: How dynamical-systems theory could advance psychiatry. Am. J. Psychiatry 2021, 178, 791–792. [Google Scholar] [CrossRef]
- Delgadillo, J.; de Jong, K.; Lucock, M.; Lutz, W.; Rubel, J.; Gilbody, S.; Ali, S.; Aguirre, E.; Appleton, M.; Nevin, J.; et al. Feedback-informed treatment versus usual psychological treatment for depression and anxiety: A multisite, pragmatic, cluster-randomised controlled trial. Lancet Psychiatry 2018, 5, 564–572. [Google Scholar] [CrossRef]
- Alowais, S.A.; Alghamdi, S.S.; Alsuhebany, N.; Alqahtani, T.; Alshaya, A.I.; Almoaiqel, M. Revolutionizing healthcare: The role of artificial intelligence in clinical practice. BMC Med Educ. 2023, 23, 689. [Google Scholar] [CrossRef] [PubMed]
- Bauer, M.; Glenn, T.; Monteith, S.; Bauer, R.; Whybrow, P.C.; Geddes, J. Ethical perspectives on recommending digital technology for patients with mental illness. Int. J. Bipolar Disord. 2017, 5, 6. [Google Scholar] [CrossRef]
- Tilala, M.H.; Chenchala, P.K.; Choppadandi, A.; Kaur, J.; Naguri, S.; Saoji, R.; Devaguptapu, B. Ethical considerations in the use of artificial intelligence and machine learning in health care: A comprehensive review. Cureus 2024, 16, e62443. [Google Scholar] [CrossRef] [PubMed]
- Ratti, E.; Morrison, M.; Jakab, I. Ethical and social considerations of applying artificial intelligence in healthcare—A two-pronged scoping review. BMC Med Ethics 2025, 26, 68. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Calls for Safe and Ethical AI for Health. 2023. Available online: https://www.who.int/news/item/16-05-2023-who-calls-for-safe-and-ethical-ai-for-health (accessed on 13 August 2024).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).