Hallux Strength Matters: Its Relationship with Physical Performance and Predictive Role in Fall Risk
Abstract
1. Introduction
2. Materials and Methods
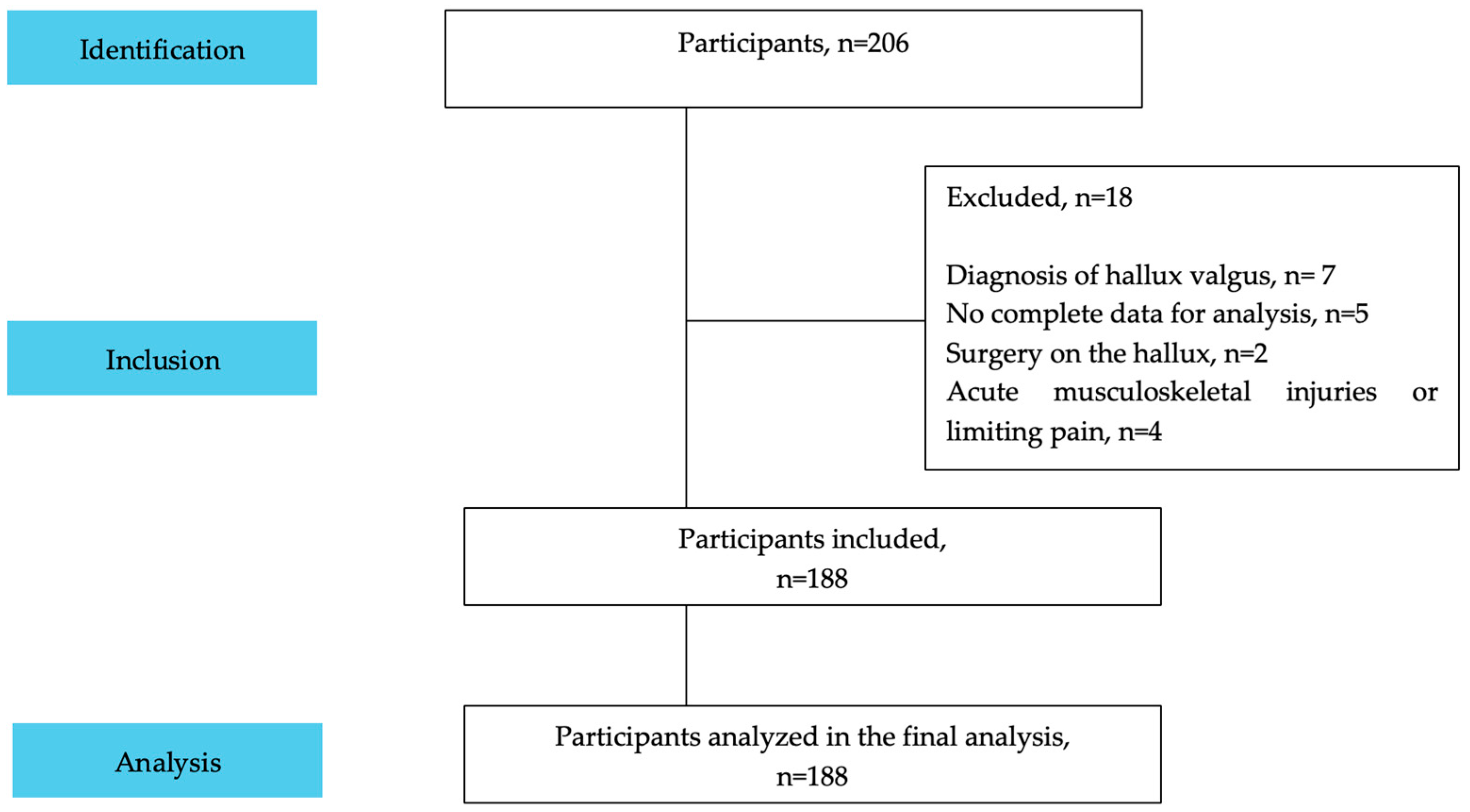
2.1. Design and Participants
2.2. Procedures
2.2.1. Hallux Plantar Flexion Strength
2.2.2. Physical Performance
2.2.3. Fall Risk
2.3. Statistical Analysis
3. Results
4. Discussion
4.1. Limitations and Strengths
4.2. Future Applications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PGT | Paper Grip Test |
| SLS | Single-Leg Stance Test |
| SPPB | Short Physical Performance Battery |
| TUG | Timed Up and Go Test |
| 5-STS | Five times sit-to-stand test |
References
- Alvarado García, A.M.; Maya, S.; María, Á. Análisis del concepto de envejecimiento. Gerokomos 2014, 25, 57–62. [Google Scholar] [CrossRef]
- Concha-Cisternas, Y.; Vargas-Vitoria, R.; Celis-Morales, C. Cambios morfofisiológicos y riesgo de caídas en el adulto mayor: Una revisión. Rev. Científica Salud Uninorte 2020, 36, 450–470. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Zhuang, C.L.; Zhang, F.M.; Li, W.; Wang, K.H.; Xu, H.X.; Song, C.H.; Guo, Z.; Shi, H. Associations of low handgrip strength with cancer mortality: A multicentre observational study. JCSM 2020, 11, 1476–1486. [Google Scholar] [CrossRef] [PubMed]
- Pereira, C.C.; Pagotto, V.; de Oliveira, C.; Silveira, E.A. Sarcopenia and mortality risk in community-dwelling Brazilian older adults. Sci. Rep. 2022, 12, 17531. [Google Scholar] [CrossRef] [PubMed]
- Marincolo, J.C.S.; Aprahamian, I.; Corona, L.P.; Neri, A.L.; Yassuda, M.S.; Borim, F.S.A. Three definitions of probable sarcopenia and associations with falls and functional disability among community-dwelling older adults. Osteoporos. Sarcopenia 2021, 7, 69–74. [Google Scholar] [CrossRef]
- Petermann-Rocha, F.; Balntzi, V.; Gray, S.R.; Lara, J.; Ho, F.K.; Pell, J.P.; Celis-Morales, C. Global prevalence of sarcopenia and severe sarcopenia: A systematic review and meta-analysis. JCSM 2022, 13, 86–99. [Google Scholar] [CrossRef]
- Concha-Cisternas, Y.; Lobos, J.; Retamal, C.; Bastías, D.; Lanuza, F.; Nuñez-Espinosa, C.; Pizarro-Mena, R.; Guede-Rojas, F. Adiposity and mediterranean diet adherence: A Comparison between older women with and without sarcopenia. Retos 2025, 68, 1784–1795. [Google Scholar] [CrossRef]
- Lee, S.Y.; Choo, P.L.; Pang, B.W.J.; Lau, L.K.; Jabbar, K.A.; Seah, W.T.; Chen, K.K.; Ng, T.P.; Wee, S.-L. SPPB reference values and performance in assessing sarcopenia in community-dwelling Singaporeans–Yishun study. BMC Geriatr. 2021, 21, 213. [Google Scholar]
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985, 100, 126. [Google Scholar]
- Concha-Cisternas, Y.; Castro-Piñero, J.; Vásquez-Muñoz, M.; Molina-Márquez, I.; Vásquez-Gómez, J.; Guzmán-Muñoz, E. Effects of Neuromuscular Training on Postural Balance and Physical Performance in Older Women: Randomized Controlled Trial. J. Funct. Morphol. 2024, 9, 195. [Google Scholar] [CrossRef]
- Yang, H.; Jiang, Y.; Liang, D.; Yang, C.; Qin, K.; Xie, Y.; Zhang, L.; Tang, P.; Cui, X.; Lyu, H. Sarcopenia-related traits and risk of falls in older adults: Results from meta-analysis of cohort studies and Mendelian randomization analyses. Aging Clin. Exp. Res. 2025, 37, 106. [Google Scholar] [CrossRef]
- Salari, N.; Darvishi, N.; Ahmadipanah, M.; Shohaimi, S.; Mohammadi, M. Global prevalence of falls in the older adults: A comprehensive systematic review and meta-analysis. J. Orthop. Surg. Res. 2022, 17, 334. [Google Scholar] [CrossRef]
- Monteiro, Y.C.M.; Vieira, M.A.d.S.; Vitorino, P.V.d.O.; Queiroz SJd Policena, G.M.; Souza, A.C.S.E. Trend of fall-related mortality among the elderly. Rev. Esc. Enferm. USP 2021, 55, e20200069. [Google Scholar] [CrossRef]
- World Health Organization. Falls: Key Facts; World Health Organization: Geneva, Switzerland, 2023; Available online: https://www.who.int/news-room/fact-sheets/detail/falls (accessed on 10 September 2025).
- Rodriguez-Fortis, A.O.; Montanero-Pazmiño, C.; Intriago-Briones, J.; Ponce-Alencastro, J.A. Sarcopenia asociada a Síndrome de inestabilidad y caídas: Revisión actualizada para la práctica clínica. Multidiscip. Health Educ. J. 2023, 5, 265–278. [Google Scholar]
- McKeon, P.O.; Hertel, J.; Bramble, D.; Davis, I. The foot core system: A new paradigm for understanding intrinsic foot muscle function. Br. J. Sports Med. 2015, 49, 290. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.; Ye, Y.; Huang, D.; Zhang, X. Age-related differences in the capacity and neuromuscular control of the foot core system during quiet standing. Scand. J. Med. Sci. Sports. 2024, 34, e14522. [Google Scholar] [CrossRef] [PubMed]
- Futrell, E.E.; Roberts, D.; Toole, E. The effects of intrinsic foot muscle strengthening on functional mobility in older adults: A systematic review. J. Am. Geriatr. Soc. 2022, 70, 531–540. [Google Scholar] [CrossRef] [PubMed]
- Mansi, M.K.; Chockalingam, N.; Chatzistergos, P.E. The enhanced paper grip test can substantially improve community screening for the risk of falling. Gait Posture 2024, 108, 157–163. [Google Scholar] [CrossRef]
- Tsekoura, M.; Pantou, M.; Fousekis, K.; Billis, E.; Gliatis, J.; Tsepis, E. Reliability and clinical applicability of lower limp strength using an enhanced paper grip strength. Eur. J. Transl. Myol. 2023, 33, 11841. [Google Scholar] [CrossRef]
- Mansi, M.K.; Chockalingam, N.; Chatzistergos, P.E. An exploration of the mechanistic link between the enhanced paper grip test and the risk of falling. Foot 2023, 57, 102059. [Google Scholar] [CrossRef]
- Chatzistergos, P.E.; Healy, A.; Balasubramanian, G.; Sundar, L.; Ramachandran, A.; Chockalingam, N. Reliability and validity of an enhanced paper grip test; a simple clinical test for assessing lower limb strength. Gait Posture 2020, 81, 120–125. [Google Scholar] [CrossRef]
- Guzmán-Muñoz, E.M.-R.G.; Concha-Cisternas, Y.; Faúndez-Casanova, C. Diseños de investigación cuantitativa en ciencias de la actividad física y la salud. Rev. Cienc. Act. Física UCM 2025, 26, 63–85. [Google Scholar] [CrossRef]
- Jiménez, D.; Lavados, M.; Rojas, P.; Henríquez, C.; Silva, F.; Guillón, M. Evaluación del minimental abreviado de la evaluación funcional del adulto mayor (EFAM) como screening para la detección de demencia en la atención primaria. Rev. Med. Chile. 2017, 145, 862–868. [Google Scholar] [CrossRef]
- Ministerio de Salud (MINSAL). Ministerio de Salud. Manual de Aplicación del Examen de Medicina Preventiva del Adulto mayor, Programa de Salud del Adulto Mayor (2008). Available online: https://diprece.minsal.cl/wrdprss_minsal/wp-content/uploads/2015/05/instructivo-de-control-de-salud-empam.pdf (accessed on 10 September 2025).
- Ross, R.; Neeland, I.J.; Yamashita, S.; Shai, I.; Seidell, J.; Magni, P.; Santos, R.D.; Arsenault, B.; Cuevas, A.; Hu, F.B.; et al. Waist circumference as a vital sign in clinical practice: A Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat. Rev. Endocrinol. 2020, 16, 177–189. [Google Scholar] [CrossRef] [PubMed]
- Menz, H.B.; Morris, M.E.; Lord, S.R. Foot and ankle characteristics associated with impaired balance and functional ability in older people. J. Gerontol. A Biol. Sci. Med. Sci. 2005, 60, 1546–1552. [Google Scholar] [CrossRef]
- Bergland, A.; Strand, B.H. Norwegian reference values for the short physical performance battery (SPPB): The Tromsø study. BMC Geriatr. 2019, 19, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Vélez, R.; Pérez-Sousa, M.A.; Venegas-Sanabria, L.C.; Cano-Gutierrez, C.A.; Hernández-Quiñonez, P.A.; Rincón-Pabón, D.; García-Hermoso, A.; Zambom-Ferraresi, F.; de Asteasu, M.L.S.; Izquierdo, M. Normative values for the short physical performance battery (SPPB) and their association with anthropometric variables in older Colombian adults. The SABE study, 2015. Front. Med. 2020, 7, 52. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Monje, F.; Cortés-Gálvez, J.M.; Cartagena-Perez, Y.; Leal-Hernández, M. Valoración funcional del anciano en atención primaria mediante el test «SPPB». Rev. Española Geriatría Gerontol. 2018, 53, 59–60. [Google Scholar] [CrossRef]
- Guralnik, J.M.; Simonsick, E.M.; Ferrucci, L.; Glynn, R.J.; Berkman, L.F.; Blazer, D.G.; Scherr, P.A.; Wallace, R.B. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J. Gerontol. 1994, 49, M85–M94. [Google Scholar] [CrossRef] [PubMed]
- Omaña, H.; Bezaire, K.; Brady, K.; Davies, J.; Louwagie, N.; Power, S.; Santin, S.; Hunter, S.W. Functional reach test, single-leg stance test, and tinetti performance-oriented mobility assessment for the prediction of falls in older adults: A systematic review. Phys. Ther. 2021, 101, pzab173. [Google Scholar] [CrossRef]
- Błaszczyk, J.W.; Fredyk, A.; Błaszczyk, P.M. Transition from double-leg to single-leg stance in the assessment of postural stability. J. Biomech. 2020, 110, 109982. [Google Scholar] [CrossRef] [PubMed]
- Concha- Cisternas, Y.C.; Marzuca-Nassr, G.N. Criterios de valoración geriátrica integral en adultos mayores autovalentes y en riesgo de dependencia en centros de atención primaria en Chile. REEM 2016, 3, 31–41. [Google Scholar]
- Bolgla, L.A.; Malone, T.R. Plantar fasciitis and the windlass mechanism: A biomechanical link to clinical practice. IJATT 2004, 39, 77. [Google Scholar]
- Manfredi-Márquez, M.J.; Tavara-Vidalón, S.P.; Tavaruela-Carrión, N.; Gómez Benítez, M.Á.; Fernandez-Seguín, L.M.; Ramos-Ortega, J. Study of Windlass Mechanism in the lower limb using inertial sensors. Int. J. Environ. Res. Public Health 2023, 20, 3220. [Google Scholar] [CrossRef] [PubMed]
- Yan, Y.; Ou, J.; Shi, H.; Sun, C.; Shen, L.; Song, Z.; Shu, L.; Chen, Z. Plantar pressure and falling risk in older individuals: A cross-sectional study. J. Foot Ankle Res. 2023, 16, 14. [Google Scholar] [CrossRef]
- Kamasaki, T.; Otao, H.; Tanaka, S.; Hachiya, M.; Kubo, A.; Okawa, H.; Sakamoto, A.; Fujiwara, K.; Suenaga, T.; Kichize, Y.; et al. Age-specific comparisons in the rate of force development of toe pressure strength and its association with the timed up and go test. Eur. Geriatr. Med. 2024, 15, 689–698. [Google Scholar] [CrossRef]
- Quinlan, S.; Sinclair, P.; Hunt, A. The evidence for improving balance by strengthening the toe flexor muscles: A systematic review. Gait Posture 2020, 81, 56–66. [Google Scholar] [CrossRef]
- Ridge, S.T.; Rowley, K.M.; Kurihara, T.; McClung, M.; Tang, J.; Reischl, S.; Kulig, K.; Ignasiak, Z. Contributions of intrinsic and extrinsic foot muscles during functional standing postures. Biomed Res. Int. 2022, 7708077. [Google Scholar] [CrossRef]
- Okamura, K.; Egawa, K.; Okii, A.; Oki, S.; Kanai, S. Intrinsic foot muscle strengthening exercises with electromyographic biofeedback achieve increased toe flexor strength in older adults: A pilot randomized controlled trial. Clin. Biomech. 2020, 80, 105187. [Google Scholar] [CrossRef]

| Females (n = 168) | Males (n = 20) | Total (n = 188) | |
|---|---|---|---|
| Age (years) | 72.03 ± 13.6 | 69.95 ± 5.77 | 71.81 ± 6.78 |
| Body weight (kg) | 71.00 ± 13.5 | 79.32 ± 17.68 | 71.00 ± 13.52 |
| Height (m) | 1.55 ± 0.09 | 1.68 ± 0.10 | 1.55 ± 0.09 |
| BMI (kg/m2) | 29.44 ± 4.81 | 28.05 ± 4.04 | 29.44 ± 4.81 |
| Females (n = 168) | Males (n = 20) | Total (n = 188) | |
|---|---|---|---|
| PGT RF (kg) | 6.58 ± 3.05 | 7.95 ± 3.68 | 6.76 ± 3.11 |
| PGT LF (kg) | 6.30 ± 2.88 | 7.39 ± 3.28 | 6.45 ± 2.91 |
| Total score SPPB | 9.63 ± 2.02 | 10.25 ± 2.07 | 9.70 ± 2.02 |
| Balance (points) | 3.88 ± 0.45 | 3.98 ± 0.11 | 3.89 ± 0.43 |
| 5-STS (points) | 2.69 ± 1.17 | 2.80 ± 1.32 | 2.70 ± 1.18 |
| Gait speed (points) | 3.22 ± 0.93 | 3.50 ± 0.95 | 3.26 ± 0.94 |
| TUG (s) | 8.43 ± 2.50 | 9.02 ± 5.54 | 8.55 ± 2.97 |
| SLS-R (s) | 10.20 ± 6.28 | 10.52 ± 7.22 | 10.18 ± 6.37 |
| SLS-L (s) | 10.38 ± 6.30 | 11.08 ± 6.48 | 10.56 ± 6.30 |
| Females (n = 168) | Males (n = 20) | Total (n = 188) | |
|---|---|---|---|
| Total score SPPB | p = 0.040; r = 0.142 | p = 0.048; r = 0.372 | p = 0.008; r = 0.178 |
| Balance (points) | p = 0.130; r = 0.089 | p = 0.140; r = 0.259 | p = 0.110; r = 0.093 |
| 5-STS (points) | p = 0.350; r = −0.030 | p = 0.130; r = 0.267 | p = 0.420; r = 0.015 |
| Gait speed (points) | p = 0.010; r = 0.177 | p = 0.040; r = 0.397 | p = 0.002; r = 0.214 |
| TUG (s) | p =< 0.001; r = −0.351 | p = 0.005; r = −0.559 | p =< 0.001; r = −0.372 |
| SLS-R (s) | p =< 0.001; r = 0.309 | p = 0.030; r = 0.425 | p =< 0.001; r = 0.316 |
| SLS-L (s) | p =< 0.001; r = 0.376 | p = 0.010; r = 0.505 | p =< 0.001; r = 0.397 |
| Females (n = 168) | Males (n = 20) | Total (n = 188) | |
|---|---|---|---|
| Total score SPPB | p = 0.047; r = 0.125 | p = 0.004; r = 0.577 | p = 0.009; r = 0.175 |
| Balance (points) | p = 0.110; r = 0.096 | p = 0.060; r = 0.351 | p = 0.090; r = 0.099 |
| 5-STS (points) | p = 0.470; r = −0.006 | p = 0.120; r = 0.263 | p = 0.210; r = 0.059 |
| Gait speed (points) | p = 0.020; r = 0.156 | p = 0.006; r = 0.555 | p = 0.002; r = 0.212 |
| TUG (s) | p =< 0.001; r = −0.347 | p =< 0.001; r = −0.696 | p =< 0.001; r = −0.393 |
| SLS-R (s) | p =< 0.001; r = 0.282 | p = 0.003; r = 0.587 | p =< 0.001; r = 0.317 |
| SLS-L (s) | p =< 0.001; r = 0.333 | p =< 0.001; r = 0.658 | p =< 0.001; r = 0.351 |
| Test | R2 | Coefficient β | p-Value | 95% CI | |
|---|---|---|---|---|---|
| PGT RF | 0.17 | <0.001 | |||
| Intercept | 9.51 | <0.001 | 7.43 to 11.58 | ||
| TUG (s) | −0.36 | <0.001 | −0.54 to −0.17 | ||
| SLS-R (s) | 0.10 | 0.013 | 0.02 to 0.18 | ||
| PGT LF | 0.20 | <0.001 | |||
| Intercept | 8.74 | <0.001 | 6.97 to 10.52 | ||
| TUG (s) | −0.34 | <0.001 | −0.50 to −0.18 | ||
| SLS-L (s) | 0.11 | 0.001 | 0.05 to 0.18 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Concha-Cisternas, Y.; Guzmán-Muñoz, E.; Vásquez-Muñoz, M.; Farías-Reyes, V.; Caniulef-Contreras, A.; Pizarro-Mena, R.; Ibarra-Mora, J.; Sepúlveda-Loyola, W.; Cigarroa, I.; Molina-Márquez, I.; et al. Hallux Strength Matters: Its Relationship with Physical Performance and Predictive Role in Fall Risk. Appl. Sci. 2025, 15, 10168. https://doi.org/10.3390/app151810168
Concha-Cisternas Y, Guzmán-Muñoz E, Vásquez-Muñoz M, Farías-Reyes V, Caniulef-Contreras A, Pizarro-Mena R, Ibarra-Mora J, Sepúlveda-Loyola W, Cigarroa I, Molina-Márquez I, et al. Hallux Strength Matters: Its Relationship with Physical Performance and Predictive Role in Fall Risk. Applied Sciences. 2025; 15(18):10168. https://doi.org/10.3390/app151810168
Chicago/Turabian StyleConcha-Cisternas, Yeny, Eduardo Guzmán-Muñoz, Manuel Vásquez-Muñoz, Valentina Farías-Reyes, Almendra Caniulef-Contreras, Rafael Pizarro-Mena, Jessica Ibarra-Mora, Walter Sepúlveda-Loyola, Igor Cigarroa, Iván Molina-Márquez, and et al. 2025. "Hallux Strength Matters: Its Relationship with Physical Performance and Predictive Role in Fall Risk" Applied Sciences 15, no. 18: 10168. https://doi.org/10.3390/app151810168
APA StyleConcha-Cisternas, Y., Guzmán-Muñoz, E., Vásquez-Muñoz, M., Farías-Reyes, V., Caniulef-Contreras, A., Pizarro-Mena, R., Ibarra-Mora, J., Sepúlveda-Loyola, W., Cigarroa, I., Molina-Márquez, I., & Yáñez-Sepúlveda, R. (2025). Hallux Strength Matters: Its Relationship with Physical Performance and Predictive Role in Fall Risk. Applied Sciences, 15(18), 10168. https://doi.org/10.3390/app151810168












