1. Introduction
The success of dental implant surgery is closely related to the implant material, surface treatment, thread morphology, bone quality and density, and primary stability. Accuracy is the most crucial indicator which can be controlled and improved by surgeons during implant planning and surgery. An accurate implant position is essential to facilitate subsequent prosthesis fabrication and prevent complications, such as early implant and implant restoration failures, and damage to adjacent teeth and vital structures, such as the mandibular nerve [
1,
2]. Computer-assisted implant surgery (CAIS) is a clinically applied technology where a three-dimensional (3D) printed surgical guide assists surgeons in accurately drilling and placing the dental implant [
3,
4]. Numerous studies have consistently demonstrated that CAIS accuracy and reliability offer superiority compared to freehand implant placement, supporting its widespread application in current clinical practice [
5,
6,
7]. Although CAIS improves the accuracy and reduces the complexity of clinical operations, cone beam computer tomography (CBCT) artefacts still limit its effectiveness in clinical practice [
8]. This review presents an evidence-based perspective on addressing the challenges of CAIS in the presence of CBCT artefacts, evaluating current limitations, proposing strategies to enhance implant alignment management and supporting dental surgeons and technicians in achieving greater accuracy during implant planning and surgical template fabrication.
2. Methods
A search strategy was conducted through PubMed, Web of Science and Scopus databases from 2015 to 2025 using the keywords “Metal artifacts”, “Implant planning”, “Implant placement”, “Accuracy” and “Data alignment”.
The inclusion criteria were accuracy studies related to implant placement and planning, case reports and dental techniques involving cases of partially edentulous patients with metallic artefacts and articles published in English. Studies were excluded based on the following criteria: (i) planning of the implant-supported restoration process, (ii) techniques to reduce artefacts using an algorithm and (iii) review articles.
The titles and abstracts were initially screened by reviewers (C.L.). After identifying articles that met the inclusion criteria, the following data were extracted and tabulated: applicable conditions, operational complexity, visiting times before CAIS, aligning times, accuracy, reasons for deviations, advantages and limitations.
3. Accuracy of CAIS: Theory Versus Practice
Accuracy is a broad concept that encompasses related but distinct components: trueness and precision. These terms are frequently used to evaluate the digital workflow of CBCT scanning, intra-oral scanning, laboratory scanning, dental impressions and plaster cast fabrication [
9]. Trueness refers to the degree of systematic error, agreement and consistency between the means of tests and actual reference values resulting in systematic error or bias [
10]. In implant dentistry, trueness is commonly used as the key outcome measure to assess the accuracy of measurements between digital scans or printed casts and a reference standard in studies evaluating CBCT scans, intra-oral and laboratory scans, and 3D [
9,
11]. Moreover, the mean deviation between the planned implant and the actually placed implant is often applied to assess the CAIS accuracy [
12,
13].
In contrast, precision refers to the agreement of repeated measurements made under specified conditions, recording the random error to reflect the repeatability and reproducibility of independent test results [
10]. In implant dentistry, precision is widely evaluated through CBCT, intra-oral and laboratory scans, as well as the fabrication of 3D-printed surgical templates [
14,
15]. However, assessing precision in implant placement studies is limited due to ethical and practical constraints, as repeated implant placements at the same site in the same patient are not feasible in vivo [
12]. Consequently, most implant accuracy studies emphasise trueness, while precision remains underexplored despite being an essential component of overall accuracy.
An accurate implant position is crucial for facilitating subsequent prosthesis fabrication and preventing damage to adjacent teeth and vital structures. CAIS plays a pivotal role in achieving this optimal outcome by using an implant surgical template to guide the implant placement according to the preoperative plan. However, the risk of inaccurate placement in implant positioning remains high. This unfavourable outcome is often attributed to errors in 3D data alignment during implant planning for designing and fabricating the implant surgical templates in the conventional digital workflow [
3,
6].
4. Critical Steps in CAIS Implant Planning
Image-guided or computer-assisted technology in healthcare utilises medical imaging technology, where reverse engineering is employed for data acquisition, pre-surgical planning and virtual treatment in 3D-modelling software. Compared to freehand surgery, this technique allows for the use of professional software to process and plan more kinds of data, such as CBCT, intra-oral scan, facial scan and virtual occlusion data, before surgery. During surgery, 3D-printed guides or dynamic navigation can assist the surgical process more accurately [
6,
13]. In implant dentistry, CAIS consists of static and dynamic systems, which differ primarily in how the surgical guidance is delivered.
Data acquisition is a crucial step before CAIS, including two types of data, CBCT scans and intra-oral scans. For the parameters of CBCT scanning (
Table 1) in the condition of metal artefacts, the large field of view (FOV) and high-resolution modes are more effective in improving the accuracy of CAIS (tube voltage 90 KV, tube current 12.5 mA, resolution 75 μm and visual field 15 × 13 cm). The metal artefact reduction (MAR) function is also recommended in the condition of existing metal restorations [
16]. Intra-oral scans do not require specific parameter adjustments in clinical practice. However, when the number of consecutive missing teeth exceeds five units (including edentulous jaws), intra-oral scanning is not recommended. In such cases, impression or dental casts scanning by a desktop scanner can be used [
8,
9,
15].
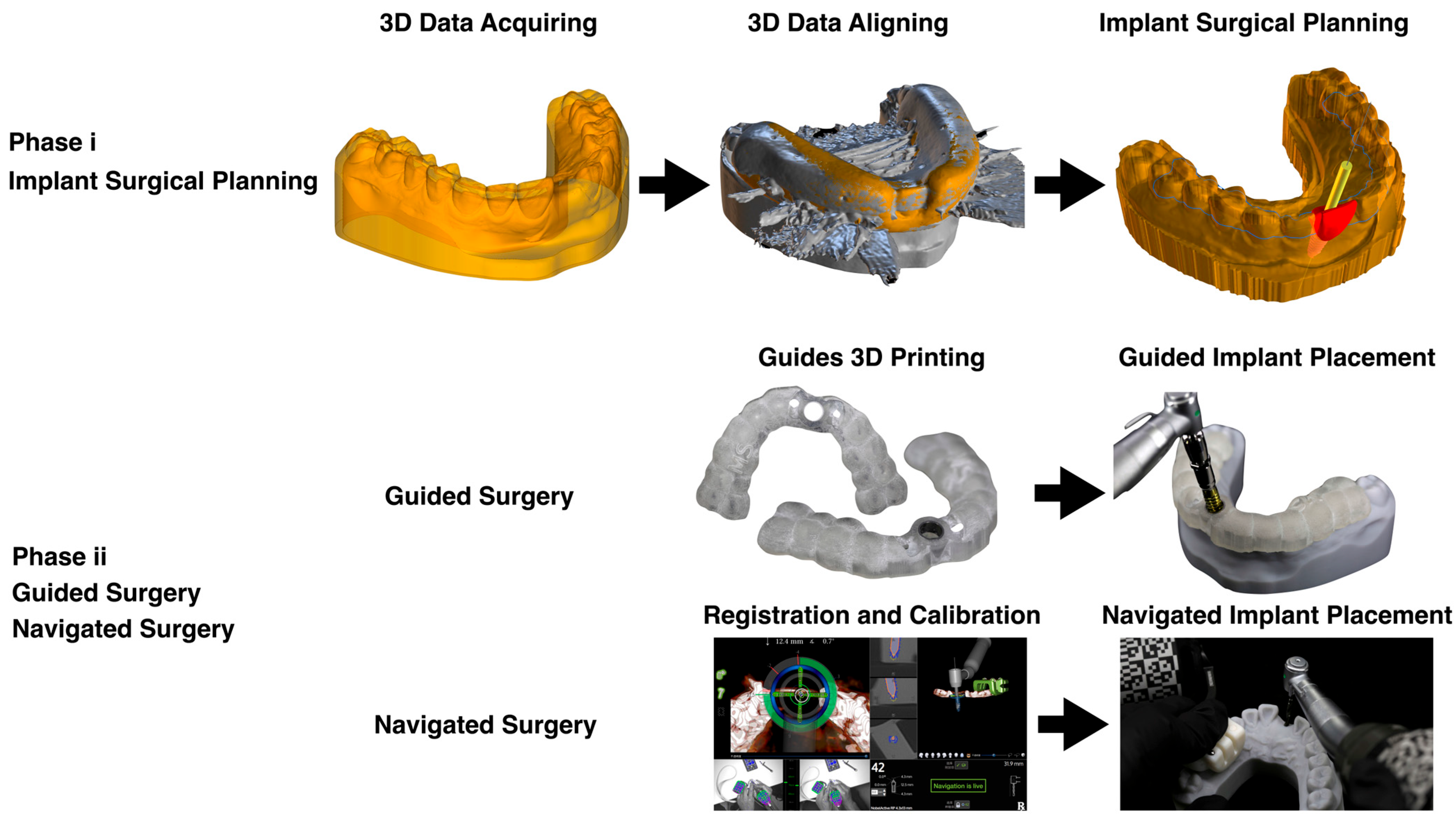
Static CAIS involves pre-surgical planning, designing and 3D printing surgical templates to accurately guide implant screw placement at the desired site and depth for patients using fixed-diameter drills. It consists of step-by-step procedures for selecting an ideal implant position and processes for implant placement before the actual surgical procedure. Essentially, CAIS has two phases: (i) implant surgical planning and (ii) guided or navigated surgery. In the first phase, the patient’s 3D clinical data, such as gingival and mucosal locations and anatomy, as well as the wax-up of the implant prosthesis, are fed into implant planning software using an intra-oral scanner [
17]. The system then organises the clinical data and produces a virtual implant, which is used for the next phase of guided/navigated surgery to plan an accurate implant placement. Subsequently, CBCT data from the patient’s jaw scan is obtained, carrying detailed information on the bone anatomy. The software then combines the earlier scanned intra-oral information and CBCT into a 3D model using the Standard Tessellation Language (STL) method [
9,
18,
19]. Careful alignment in this step is crucial to ensuring the accuracy of the 3D model generated [
20,
21,
22], which serves as a guide for the clinical placement of the implant. A diagrammatic summary is illustrated in
Figure 1.
Dynamic navigation (DN) is a branch of image–CAIS technology that has been gradually applied in dental clinics in recent years. The DN system can identify the drill’s position in real-time and then display the relative positions between the drills and the patients’ CBCT on the monitor to instruct the drilling process and implant placement [
23]. The system requires surgical planning and placement of virtual implants. It uses trackers and cameras to acquire the implant’s real-time position on the patient and the implant handpiece, then transfers the relative position of the implant into the computer and displays it to the surgeon. This display helps the surgeon to clearly observe the position of the drill tip in relation to the maxillary sinus or mandibular neural canal. The DN system also guides the surgeon to drill in the ideal position planned earlier [
12,
23,
24,
25,
26]. Although the dynamic system requires registration and calibration before surgery, aligning the CBCT scan with the intra-oral scan is mandatory, as there is no need for dentition surface mesh for design and 3D printing the guides [
24,
27]. More studies have shown that the accuracy of navigation implant surgery is higher than freehand (non-guided) and guided implant surgeries [
3,
4,
7,
28].
5. Limitations of CAIS
One of the steps to achieve this optimal outcome is to use an implant surgical template to guide the implant placement according to the preoperative plan. However, the risk of inaccurate placement in implant positioning remains high. This unfavourable outcome is often attributed to errors in 3D data alignment with virtual dental models, a critical step in the conventional digital workflow [
3,
6]. Such misalignments can significantly compromise the transfer accuracy of the planned implant position on patients.
Additionally, many studies have shown that although implant surgical guides can improve the accuracy and reduce the difficulty of clinical operations, they still require many pre-surgical preparations to fabricate the surgical template. Especially in fully edentulous cases and metal artefact cases, where an additional radiographic template is needed [
29,
30,
31].
6. Implant Planning Challenges
6.1. Accuracy in Aligning 3D Data
Two essential datasets are prerequisites for surgical planning, i.e., bone data from CBCT and dentition data, including abutment teeth, mucosa topography and implant site. These data provide the basis for designing the digital tooth- or mucosal-supported implant. Aligning these two datasets is a critical step in implant planning that directly influences the accuracy of implant placement [
3,
32]. Usually, there are two approaches to reduce errors: increasing the selection of landmarks or artificially creating markers [
6,
33]. In cases of a single missing tooth, data alignment commonly relates to the enamel landmarks of adjacent natural teeth. However, data alignment may be challenging in cases of multiple missing teeth [
32,
33]. To resolve this problem, the double-scan method (DS) using a radiographic template with markers, currently considered the gold standard in the implant planning stage, is recommended [
34,
35,
36,
37].
In the past years, several studies have explored optimised methods based on the DS approach. However, these methods only aimed to reduce clinical operations and not improve accuracy [
37,
38,
39,
40]. On the other hand, the DS method requires not only additional clinical operations but also exhibits lower accuracy in the presence of metal artefacts [
41].
Accuracy in data acquisition and alignment during the surgical planning stage is a critical prerequisite for ensuring the accuracy of CAIS, particularly in the design and fabrication of implant surgical templates. Virtual implant placement relies on CBCT data, while the surgical guide is constructed based on intra-oral scan data; therefore, precise alignment between these datasets is essential for producing an accurate and clinically practical implant guide [
3,
4,
6]. The accuracy is typically assessed by comparing the STL data from intra-oral scans with the original CBCT or STL data post-alignment, a method commonly employed in evaluating intra-oral and facial scanning accuracy [
42,
43]. Despite its importance, limited research has been conducted on assessing data alignment accuracy, particularly in dental implant planning. To address this gap, a standard approach has been proposed for aligning experiments involving 3D mesh data to compare the accuracy of the widely used DS protocol [
44].
6.2. Accuracy of Radiographic Templates in Implant Planning
During implant placement surgery, CAIS can be performed using either static CAIS (also known as guided implant surgery) or dynamic CAIS (also known as navigated implant surgery). Static CAIS is more commonly used than dynamic CAIS, which is relatively new [
45]. Current evidence suggests that radiographically guided implant templates offer significantly higher accuracy than freehand techniques, with deviations ranging from 0.5 mm to 1 mm using the former protocol. In contrast, the latter often exceeds 1 mm in deviation [
3,
4,
6]. Moreover, studies comparing the DN technology with a static navigation-assisted protocol can achieve accuracy up to 1.5 times greater than the conventional guided method [
25,
27].
Implant placement accuracy is commonly assessed by calculating the linear and angular deviations between the preoperative virtual implant planning and the actual postoperative implant position [
3,
4,
6,
28]. Postoperative implant positionings can be determined either through CBCT-based 3D reconstruction [
13,
26,
41] or via dental cast scanning of the scan bodies [
46]. Accuracy evaluation typically consists of four parameters: the deviation at the implant neck, the deviation at the implant apex, the implant depth discrepancy and the implant angle discrepancy [
46].
6.3. Metal Artefacts in Implant Planning
CBCT artefacts are distortions in 3D images, often caused by metal-containing restorations or prostheses, such as crowns, amalgam fillings, implants and radiographic implant templates. These artefacts arise primarily due to the beam hardening and scattering effects when the X-ray passes through dense materials, which inevitably disrupts the uniformity of the reconstructed images [
47]. As a result, the image is profoundly distorted, appearing as streaks, shadows, or ‘noises’ in the CBCT image and compromising the clarity of anatomical structures. Furthermore, CAIS cannot be performed accurately [
37,
39]. Based on existing research, metal artefacts mainly reduce the accuracy of CAIS by increasing the deviation in 3D data alignment. The study of implant placement accuracy comparing with and without metal artefacts conditions by Kim et al. showed that metal artefacts lead to an increased deviation of approximately 0.32 mm at the implant neck, 0.27 mm at the implant apex, 0.36 mm at depth and 0.79 degrees of the angular deviation [
41]. Another study compared the registration deviation in implant planning, and the results showed that the metal artefacts increased the alignment deviation by approximately 0.5 mm [
8].
In CAIS, CBCT artefacts critically affect the implant planning stage. Because the implant guide’s design depends on accurate alignment between CBCT data and intra-oral scans, distorted CBCT images containing noise make it difficult to identify landmarks for 3D mesh reconstruction alignment [
37,
41]. This malalignment can lead to reduced accuracy of the surgical template and implant position. Although research in this area remains limited, several studies confirm that the metal artefact decreases the accuracy of static CAIS [
8,
41].
CBCT artefacts often necessitate additional clinical steps and appointment visits to fabricate conventional radiographic templates using the DS technique. This situation can be time-consuming, costly and not always feasible, especially in cases of single-unit implant surgery. Eventually, this prompts surgeons and patients to abandon CIAS in favour of freehand surgery. However, this preference results in expected reduced implant placement accuracy.
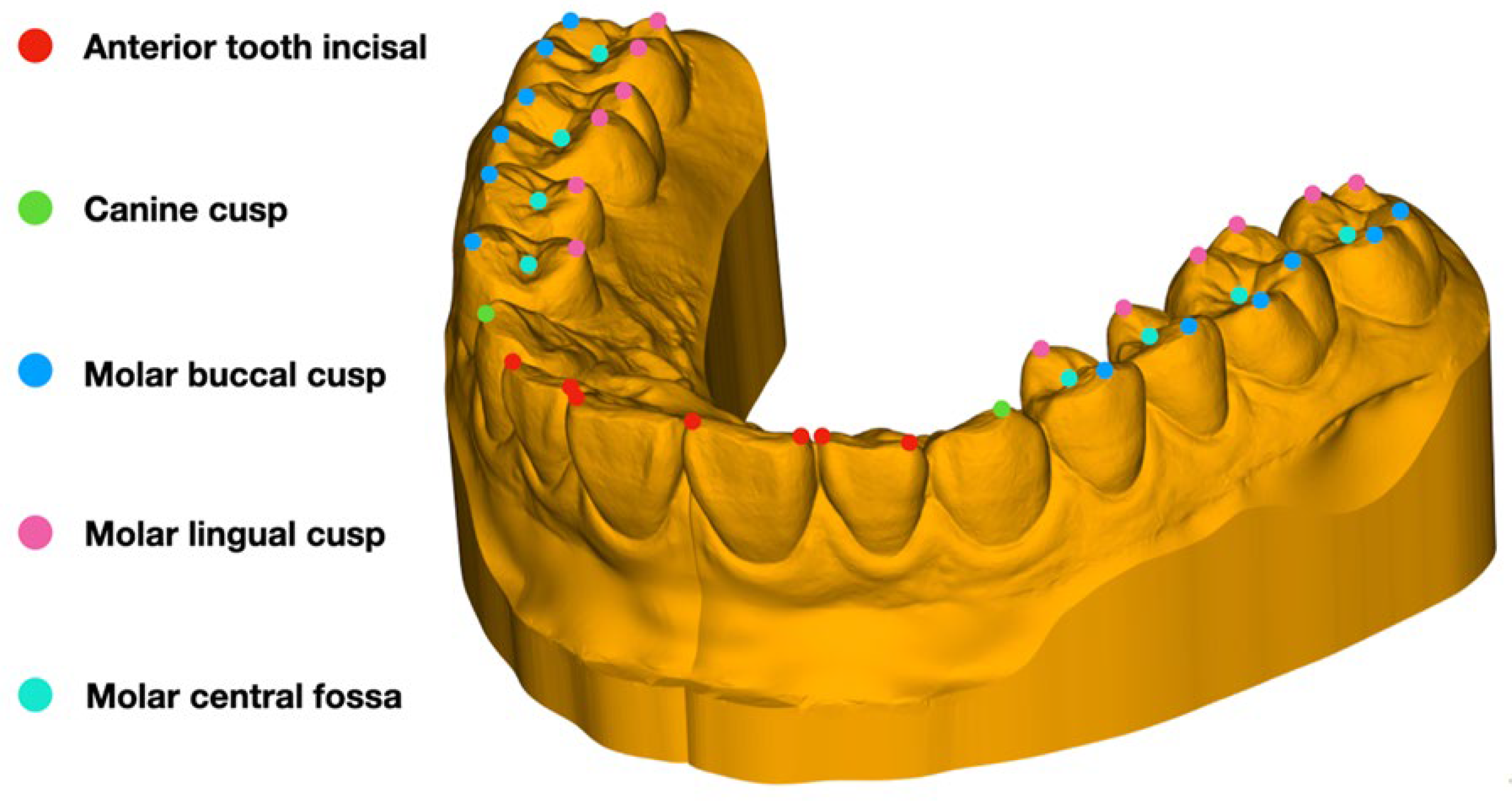
The landmarks play a crucial role in data alignment. The most commonly used landmarks include the adjacent tooth inward, canine cushion, molar buccal cushion, molar lingual cushion and molar central focus (
Figure 2). Usually, six to eight of the above landmarks are selected separately using CBCT data, and intra-oral scanning data are chosen independently. The two datasets are aligned in the same coordinate system by point-to-point match. However, metal artefacts also complicate the transfer of STL data to CBCT alignment by obscuring surfaces and distorting key anatomical structures, as shown in an example in
Figure 2, required for precise overlaying of virtual models [
41]. Despite the use of advanced software for artefact reduction, the accuracy of surgical templates remains below the clinically acceptable level. There is a need for a more straightforward and robust method to effectively achieve accurate alignment of the CBCT data and virtual dental models, even in the presence of metal artefacts.
Efforts to manage CBCT artefacts include patients wearing registration devices and trackers during CBCT scans. These devices are then repositioned at the same sites during the surgery to enable alignment between the virtual and actual patient. The method unifies data within the same spatial coordinate system [
24,
40]. However, artefact noises can still be present in the CBCT and affect the registration algorithm in the 3D reconstruction mesh, especially in compromised implant placement accuracy, particularly in the DS protocol [
41]. Although studies in this aspect are scarce, the outcome may lead to a possible registration failure or reduced surgical accuracy. Therefore, further studies are needed to develop simplified, cost-effective and robust protocols to ensure accurate implant planning and guide fabrication in the presence of CBCT artefacts.
7. Constraints of DS Implant Surgery
Technically, the DS technique requires at least two visits before the implant placement guided surgery. These visits are essential for taking jaw impressions for radiographic template fabrication and double-scan (CBCT) procedures, ensuring data alignment. Additional patient visits, longer waiting times, increased material usage and complex dentists’ operational procedures are additional constraints that burden surgeons [
35,
36,
48]. Nevertheless, surgeons need to consider these efforts to ensure accuracy in outcomes when opting for conventional DS techniques.
A radiographic template, usually made of poly-methyl methacrylate (PMMA) resin in cases of removable partial or complete dentures, often uses gutta-percha as radiopaque markers for identifying critical anatomical landmarks. For the DS implant placement workflow, two CBCT scans can be performed: first, a scan of the jaw is taken, followed by a second scan with the radiographic template in a stable position. The two scans are fitted into the implant planning software and aligned with the anatomical landmarks and markers [
49]. Through this, the radiographic template provides prosthetic information, particularly the position and dimension, for virtual implant placement in partial and complete edentulous cases [
29,
50]. In the presence of metal artefacts, a radiographic template is mainly beneficial for data alignment [
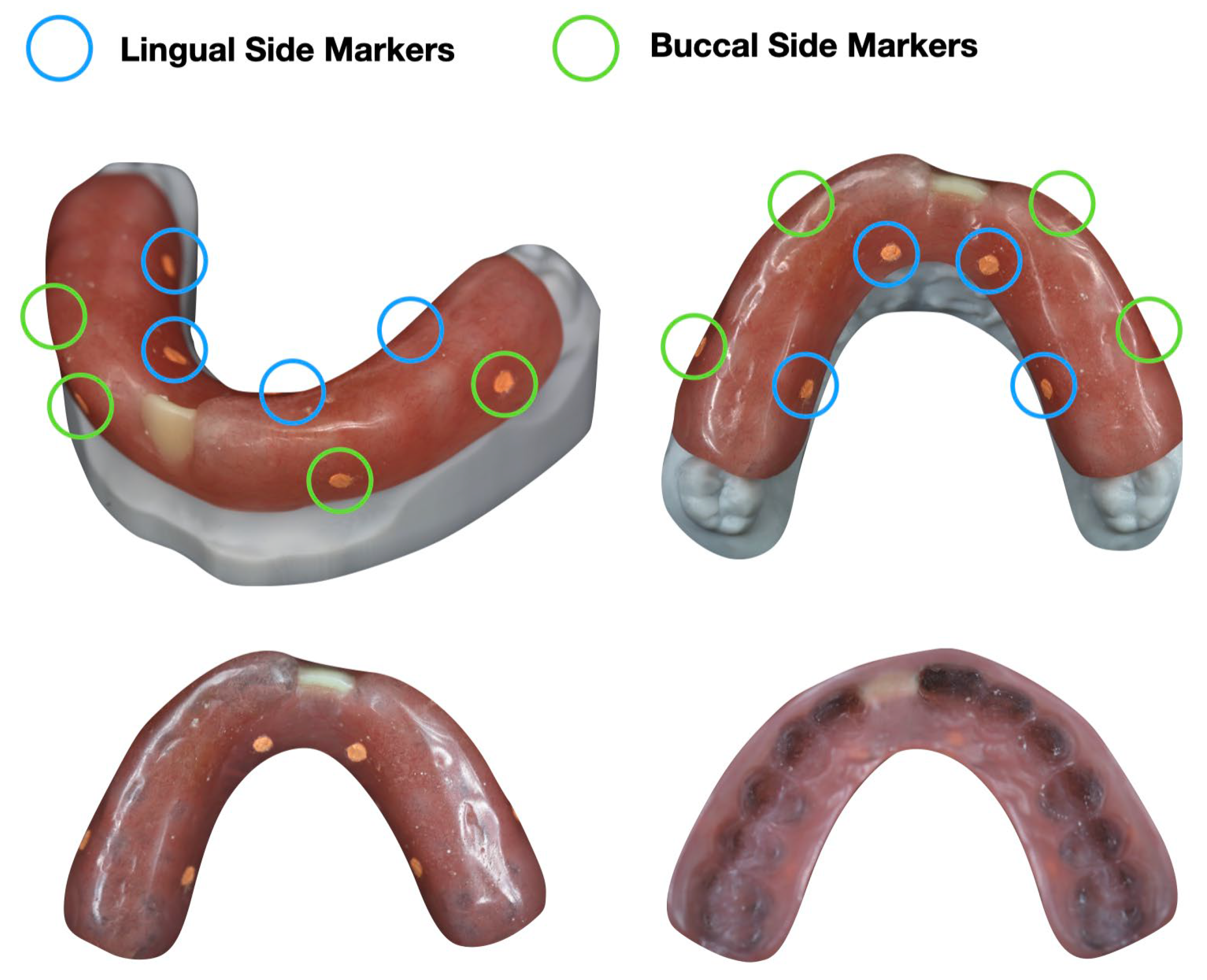
51]. Due to the noise in the scans, it does not provide valuable information for implant and implant–prosthetic planning. The selection of the conventional point-to-point method or the double-scan method in various clinical situations is shown in
Figure 3.
8. Modified Techniques and Solutions for Metal Artefacts
The recent publications of dental techniques and clinical case reports are shown in
Table 2.
8.1. Conventional Radiographic Template Method
The conventional radiographic template method utilises the patient’s existing denture, typically a complete denture, as the basic framework for creating a radiographic template filled with gutta-percha on its polished surface. The advantage of this technique is that it can be completed during the first visit, thereby reducing the need for additional visits for template fabrication and the treatment time and cost. The denture is initially relined to ensure that the fitting surface fully adapts to the patient’s mucosa and has an appropriate occlusal height. A double scan is then performed using the relined denture in the patient’s mouth [
31].
The same principle applies to patients with removable partial dentures, in which the existing dentures are modified to serve as radiographic templates. A study injected silicone rubber onto the outer surface of the denture before performing the double scan [
30]. Similarly, another case reported using a denture containing metal components as a radiographic template. After a double scan, a metal mesh was incorporated as a reference base for alignment [
29].
8.2. Modified 3D-Printed Radiographic Templates
With recent advances in dental scanning and 3D-printing technology, surgical and radiographic templates can now be produced in the clinic. Virtual radiographic templates can be designed digitally after scanning of dental casts and then made using 3D printers. Retention spaces filled with markers are incorporated into the design to facilitate the filling of markers, which are essential in the data alignment process [
30,
52], as shown in
Figure 4. There are usually eight markers distributed on the polished surface (outer surface), with four markers on the buccal side and four on the lingual side, symmetrically distributed.
8.3. Alternative Radiopaque Markers in Templates
Case studies have investigated the use of resin drops as radiopaque markers to enhance data alignment and reduce the number of dental visits for the implant planning workflow. In these studies, intra-oral scans were taken after placing four resin ‘drops’ on patients’ hard palates to serve as landmarks in intra-oral impression scanning. The CBCT data were then aligned with the former, connecting essential landmarks and references [
40,
55]. However, the resin was found to obstruct X-rays, resulting in poor visibility during the scan.
Previous studies have attempted to use resin markers on both complete and partial edentulous patients, including cases with metal artefacts [
15,
46]. However, this approach faced several limitations. One of the key drawbacks was the potential for data alignment error due to the placement of markers on movable mucosa, which compromised the identification of landmarks and reproducibility between CBCT and intra-oral scans. Additionally, conventional dental impressions could not be used, as the impression material might dislodge the resin markers. The risk of misalignment errors also increases with the length of the edentulous span.
Zirconia has recently been introduced as a template marker for implant planning [
53]. Other materials used for similar purposes include light-cure resin fillings [
41,
53], silicone rubber [
30] and gutta-percha [
30,
52,
56]. Among these, gutta-percha and zirconia have demonstrated the highest radiopacity, followed by resin fillings, with silicone being the least radiopaque [
57]. However, gutta-percha materials are difficult to shape and cannot consistently maintain uniform density, which limits their practical use as markers. Therefore, zirconia beads were chosen as the preferred marker material.
8.4. Modified Impression Scanning Technique
The impression scanning method is used in conjunction with the cross-aligning method. Two case reports on metal artefacts using a special tray with markers have been completed, taking an impression [
37,
39]. The impression did not need to cover all parts of the teeth thoroughly; only the middle parts were required. The report took a CBCT scan of a patient with the impression in place and then took another impression afterwards for the fabrication of a plaster model to be used for the dentition data scan. Then, the model’s first impression was reset as the intermediate data for cross-alignment [
37,
39]. It is essential that the impression scanning method is used together with the cross-aligning method. According to the current study, this method is mainly used for individual tooth loss artefact cases [
53]. The impression tray in this method is a specially designed finished tray with radiopaque markers, making the clinical operation more straightforward than other methods, which require additional impression-making. However, the disadvantage of this method is the same as that of the cross-aligning method in that error superposition may occur, and the design is complex.
8.5. Cross-Aligning Method
The cross-aligning, or two-alignment steps, method requires three types of datasets: (1) one CBCT dataset and (2) two STL datasets, i.e., (a) the original dentition scan and (b) an intermediate dataset that combines dentition and a characterised marker or an impression. After acquiring the CBCT and STL scans, the intermediate STL dataset is aligned separately with both the CBCT and dentition scans. This method enables the fusion of more accurate bone and dentition data [
38,
53].
Cross-aligning methods are often integrated with other approaches to improve data acquisition, particularly when direct alignment between CBCT and non-marked dentition scan is not feasible. Using an intermediate dataset containing both dentition and a marker, the method enables the indirect yet effective fusion of bone and dentition data. However, the process involves two steps; each alignment leads to systematic error, and multiple alignments may lead to error superposition. While specific studies on alignment accuracy in implant surgery planning are limited, research in the field of virtual patient construction highlights that data matching errors significantly impact overall accuracy [
22]. Furthermore, the complexity of this method limits its compatibility with conventional design software and workflows. It requires the expertise of dental technicians for precise surgical planning.
8.6. Modified-Scan Technique
A modified-scan technique was recently introduced using customised 3D-printed impression trays to eliminate the need for radiographic templates and reduce patients’ visits [
54]. This approach generally follows the conventional DS protocol to minimise alignment time and improve cross-aligning accuracy. In the reported workflow, 3D-printed radiographic trays were fabricated with eight zirconia markers bonded on the outer surfaces. A CBCT scan was then taken with the tray positioned intraorally, followed by a second CBCT scan of the tray alone. The high radiodensity of the zirconia markers allowed precise alignment of the two CBCT scan datasets. Subsequently, a 3D Boolean subtraction operation was applied to produce the dentition mesh from the scanned impression data. The aligned datasets, comprising the dentition mesh and the maxillary or mandibular bone, provided a reliable foundation for subsequent implant planning.
9. Research Limitations and Future Research Directions
It should be noted, however, that much of the available evidence is from in vitro studies, case reports or small clinical studies, and therefore lacks large-sample or long-term clinical verification. Moving forward, clinicians should select template fabrication strategies tailored to cases with artefacts, while researchers continue to develop simplified, cost-effective and robust protocols. Future studies should prioritise multicentre clinical trials to confirm the reliability and longevity of these modified techniques. Such innovations have the potential to enhance the precision of computer-assisted implant surgery, ensuring predictable outcomes even in challenging cases.
At present, there is still limited research on the impact of metal artefacts on CAIS. Currently, there is only one article on dynamic CAIS, which has shown that metal artefacts do not affect implant placement accuracy [
16]. Additionally, no relevant research on robotic CAIS has been found yet. As metal artefacts exist, more research is needed to support the clinical technical choices of different CAIS techniques.
With the widespread usage of implant surgical guides, new alignment methods for static CAIS have gradually emerged in the past five years. However, the publication of these is limited to novel dental techniques or clinical case reports and still lacks basic experiments and accuracy comparison research. So, comparing the accuracy of different alignment methods will also be a future research direction.
10. Conclusions
Accuracy is fundamental to the success of implant planning and placement, but metal artefacts from CBCT imaging remains a major source of error in 3D data alignment. Such distortions compromise the reliability of surgical templates and can lead to deviations in implant positioning. Considerations for modifications in treatment planning, particularly the fabrication of an implant template for data alignment acquisition in the presence of metal artefacts, are vital. Conventional approaches, such as the double-scan method and radiographic templates, partly address this limitation but add complexity, additional visits and risk of error. Innovative solutions, including 3D-printed radiographic templates, zirconia markers, impression scanning techniques and modified-scan protocols, show promise in improving alignment accuracy despite artefact interference.
Author Contributions
Conceptualisation, C.L.; methodology, all authors; writing—original draft preparation, C.L.; writing—reviewing and editing, I.M.T., X.F.L. and S.M.-S.; validation, X.G. and S.M.-S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors would like to thank the Faculty of Dentistry, Universiti Kebangsaan Malaysia, for its support in this study, which is part of a candidate’s PhD thesis (project registered as DD-2023-046, ethics approval JEP-2022-649).
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Chen, S.T.; Buser, D.; Sculean, A.; Belser, U.C. Complications and Treatment Errors in Implant Positioning in the Aesthetic Zone: Diagnosis and Possible Solutions. Periodontol. 2000 2023, 92, 220–234. [Google Scholar] [CrossRef] [PubMed]
- Hanif, A.; Qureshi, S.; Sheikh, Z.; Rashid, H. Complications in Implant Dentistry. Eur. J. Dent. 2017, 11, 135–140. [Google Scholar] [CrossRef]
- Bell, C.; Sahl, E.; Kim, Y.; Rice, D.D. Accuracy of Implants Placed with Surgical Guides: Thermoplastic Versus 3D Printed. Int. J. Periodontics Restor. Dent. 2018, 38, 113–119.4. [Google Scholar] [CrossRef] [PubMed]
- Cristache, C.M.; Gurbanescu, S. Accuracy Evaluation of a Stereolithographic Surgical Template for Dental Implant Insertion Using 3D Superimposition Protocol. Int. J. Dent. 2017. [Google Scholar] [CrossRef]
- Shen, P.; Zhao, J.; Fan, L.; Qiu, H.; Xu, W.; Wang, Y.; Zhang, S.; Kim, Y.J. Accuracy Evaluation of Computer-Designed Surgical Guide Template in Oral Implantology. J. Craniomaxillofac. Surg. 2015, 43, 2189–2194. [Google Scholar] [CrossRef] [PubMed]
- Pyo, S.W.; Lim, Y.J.; Koo, K.T.; Lee, J. Methods Used to Assess the 3D Accuracy of Dental Implant Positions in Computer-Guided Implant Placement: A Review. J. Clin. Med. 2019, 8, 54. [Google Scholar] [CrossRef]
- D’Souza, K.M.; Aras, M.A. Types of Implant Surgical Guides in Dentistry: A Review. J. Oral Implantol. 2012, 38, 643–652. [Google Scholar] [CrossRef]
- Biun, J.; Dudhia, R.; Arora, H. The Influence of Metal Artifact Reduction on the Trueness of Registration of a Cone-Beam Computed Tomography Scan with an Intraoral Scan in the Presence of Severe Restoration Artifact. J. Prosthodont. 2024, 33, 700–705. [Google Scholar] [CrossRef]
- Baldi, A.; Comba, A.; Rozzi, D.; Kalil, G.; Pereira, R.; Valandro, F.; Michelotto Tempesta, R.; Scotti, N. Does Partial Adhesive Preparation Design and Finish Line Depth Influence Trueness and Precision of Intraoral Scanners? J. Prosthet. Dent. 2023, 129, 637.e1–637.e9. [Google Scholar] [CrossRef]
- Menditto, A.; Patriarca, M.; Magnusson, B. Understanding the Meaning of Accuracy, Trueness and Precision. Accredit. Qual. Assur. 2007, 12, 45–47. [Google Scholar] [CrossRef]
- Mehl, A.; Reich, S.; Beuer, F.; Güth, J.-F. Accuracy, Trueness, and Precision—A Guideline for the Evaluation of these Basic Values in Digital Dentistry. Int. J. Comput. Dent. 2021, 24, 341–352. [Google Scholar] [PubMed]
- Mauer, R.; Shadrav, A.; Dashti, M. Static Surgical Guides and Dynamic Navigation in Implant Surgery. Navig. Oral Maxillofac. Surg. 2022, 1, 135–150. [Google Scholar]
- Otaghsara, S.S.T.; Joda, T.; Thieringer, F.M. Accuracy of Dental Implant Placement Using Static versus Dynamic Computer-assisted Implant Surgery: An In Vitro Study. J. Dent. 2023, 132, 104487. [Google Scholar] [CrossRef]
- Tahir, N.; Abduo, J. An In Vitro Evaluation of the Effect of 3D Printing Orientation on the Accuracy of Implant Surgical Templates Fabricated by Desktop Printer. J. Prosthodont. 2022, 31, 791–798. [Google Scholar] [CrossRef]
- Pereira, A.L.C.; Medeiros, V.R.; Carreiro, A.F.P. Influence of Implant Position on the Accuracy of Intraoral Scanning in Fully Edentulous Arches: A Systematic Review. J. Prosthet. Dent. 2021, 126, 749–755. [Google Scholar] [CrossRef]
- Liu, C.; Mohd-Said, S.; Leong, X.F.; Tew, I.M. Effect of Metal Artifacts in Cone-beam Computed Tomography on Accuracy of Implant Placement by Static and Dynamic Computer-Assisted Implant Surgery: An In Vitro Study. Int. J. Oral Maxillofac. Implants. 2025, 1–29. [Google Scholar] [CrossRef]
- Al Yafi, F.; Camenisch, B.; Al-Sabbagh, M. Is Digital Guided Implant Surgery Accurate and Reliable? Dent. Clin. North Am. 2019, 63, 381–397. [Google Scholar] [CrossRef]
- Pieralli, S.; Beyer, C.; Wesemann, C.; Vach, K.; Russe, M.F.; Kernen, F.; Nelson, K.; Spies, B.C. Impact of Radiographic Field-of-View Volume on Alignment Accuracy during Virtual Implant Planning: A Noninterventional Retrospective Pilot Study. Clin. Oral Implant. Res. 2022, 33, 1021–1029. [Google Scholar] [CrossRef]
- Ritter, L.; Reiz, S.D.; Rothamel, D.; Dreiseidler, T.; Karapetian, V.; Scheer, M.; Zöller, J.E. Registration Accuracy of Three-Dimensional Surface and Cone Beam Computed Tomography Data for Virtual Implant Planning. Clin. Oral Implant. Res. 2012, 23, 447–452. [Google Scholar] [CrossRef]
- Liu, X.; Yu, J.; Zhou, J.; Tan, J. A Digitally Guided Dual Technique for Both Gingival and Bone Resection during Crown Lengthening Surgery. J. Prosthet. Dent. 2018, 119, 345–349. [Google Scholar] [CrossRef] [PubMed]
- Aldilha Yudha, S.F.; Yulkifli; Yohandri. Validity of Student Worksheet Based on Guided Inquiry Learning Model Assisted by Digital Practicum Tool. J. Phys. Conf. Ser. 2019, 1185, 012058. [Google Scholar] [CrossRef]
- Li, J.; Sommer, C.; Wang, H.-L.; Lepidi, L.; Joda, T.; Mendonca, G. Creating a Virtual Patient for Completely Edentulous Computer-Aided Implant Surgery: A Dental Technique. J. Prosthet. Dent. 2021, 125, 564–568. [Google Scholar] [CrossRef]
- Dianat, O.; Nosrat, A.; Tordik, P.A.; Aldahmash, S.A.; Romberg, E.; Price, J.B.; Mostoufi, B. Accuracy and Efficiency of a Dynamic Navigation System for Locating Calcified Canals. J. Endod. 2020, 46, 1719–1725. [Google Scholar] [CrossRef]
- Lopes, A.; Nobre, M.A.; Santos, D. The Workflow of a New Dynamic Navigation System for the Insertion of Dental Implants in the Rehabilitation of Edentulous Jaws: Report of Two Cases. J. Clin. Med. 2020, 9, 421. [Google Scholar] [CrossRef]
- Block, M.S.; Emery, R.W.; Cullum, D.R.; Sheikh, A. Implant Placement is More Accurate Using Dynamic Navigation. J. Oral Maxillofac. Surg. 2017, 75, 1377–1386. [Google Scholar] [CrossRef]
- Edelmann, C.; Wetzel, M.; Knipper, A.; Luthardt, R.G.; Schnutenhaus, S. Accuracy of Computer-Assisted Dynamic Navigation in Implant Placement with a Fully Digital Approach: A Prospective Clinical Trial. J. Clin. Med. 2021, 10, 1808. [Google Scholar] [CrossRef] [PubMed]
- Emery, R.W.; Merritt, S.A.; Lank, K.; Gibbs, J.D. Accuracy of Dynamic Navigation for Dental Implant Placement—Model-Based Evaluation. J. Oral Implantol. 2016, 42, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Naziri, E.; Schramm, A.; Wilde, F. Accuracy of Computer-Assisted Implant Placement with Insertion Templates. GMS Interdiscip. Plast. Reconstr. Surg. DGPW 2016, 5, Doc15. [Google Scholar]
- An, X.; Yang, H.W.; Choi, B.H. Digital Workflow for Computer-Guided Implant Surgery in Edentulous Patients with an Intraoral Scanner and Old Complete Denture. J. Prosthodont. 2019, 28, 715–718. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, J.M.; Caramês, G.B.; Gill, G.G.; Caramês, J. Adaptation of an Interim Partial Removable Dental Prosthesis as a Radiographic Template for Implant Placement. J. Prosthet. Dent. 2016, 116, 147–148. [Google Scholar] [CrossRef][Green Version]
- Scherer, M.D.; Roh, H.K. Radiopaque Dental Impression Method for Radiographic Interpretation, Digital Alignment, and Surgical Guide Fabrication for Dental Implant Placement. J. Prosthet. Dent. 2015, 113, 343–346. [Google Scholar] [CrossRef]
- Wu, J.; Shui, Y.; Xie, C.; Wu, Q.; Yu, M.; Luo, T.; Zhao, Y.; Yu, H. Effect of Fabrication Methods and Number of Supporting Teeth on the Surface Accuracy and Dimensional Stability of Implant Surgical Guides. J. Prosthet. Dent. 2025, 133, 530.e1–530.e9. [Google Scholar] [CrossRef]
- Raico Gallardo, Y.N.; da Silva-Olivio, I.R.T.; Mukai, E.; Morimoto, S.; Sesma, N.; Cordaro, L. Accuracy Comparison of Guided Surgery for Dental Implants According to the Tissue of Support: A Systematic Review and Meta-Analysis. Clin. Oral Implant. Res. 2017, 28, 602–612. [Google Scholar] [CrossRef]
- Lal, K.; White, G.S.; Morea, D.N.; Wright, R.F. Use of Stereolithographic Templates for Surgical and Prosthodontic Implant Planning and Placement. Part I. The concept. J. Prosthodont. 2006, 15, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Ramasamy, M.; Giri, R.R.; Subramonian, K.; Narendrakumar, R. Implant Surgical Guides: From the Past to the Present. J. Pharm. Bioallied Sci. 2013, 5 (Suppl. S1), 98–102. [Google Scholar] [CrossRef]
- Sykaras, N.; Woody, R.D. Conversion of an Implant Radiographic Template into a Surgical Template. J. Prosthodont. 2001, 10, 108–112. [Google Scholar] [CrossRef] [PubMed]
- Loo, C.A.; Azpiazu-Flores, F.X. Radiographic Template Used to Facilitate the Alignment of Digital Scans to Computed Tomography Scans with Extensive Beam Hardening Artifacts. J. Prosthet. Dent. 2023, 129, 520–522. [Google Scholar] [CrossRef]
- Hamilton, A.; Jamjoom, F.; Doliveux, S.; Gallucci, G.O.; Friedland, B. Radiographic Markers for Merging Virtual Data Sets. J. Prosthet. Dent. 2019, 122, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Yuan, C.; Wei, L.; Li, X.; Wang, P. A Technique for Registering Digital Dental Casts onto Cone Beam Computed Tomography Scans with Excessive Metallic Artifacts. J. Prosthet. Dent. 2021, 125, 29–33. [Google Scholar] [CrossRef]
- Lv, H.X.; Rong, R.; Sa, Y. Radiopaque Fiducial Markers as an Aid to Fabrication of an Implant Surgical Guide for a Patient with Orthodontic Brackets: A Dental Technique. J. Prosthet. Dent. 2023, 129, 835–839. [Google Scholar] [CrossRef]
- Kim, J.-E.; Park, Y.-B.; Shim, J.-S.; Moon, H.-S. The Impact of Metal Artifacts within Cone Beam Computed Tomography Data on the Accuracy of Computer-Based Implant Surgery: An In Vitro Study. Int. J. Oral Maxillofac. Implant. 2019, 34, 585–594. [Google Scholar] [CrossRef]
- Kihara, H.; Hatakeyama, W.; Komine, F.; Takafuji, K.; Takahashi, T.; Yokota, J.; Oriso, K.; Kondo, H. Accuracy and Practicality of Intraoral Scanner in Dentistry: A Literature Review. J. Prosthodont. Res. 2020, 64, 109–113. [Google Scholar] [CrossRef]
- Bohner, L.; Gamba, D.D.; Hanisch, M.; Marcio, B.S.; Tortamano Neto, P.; Laganá, D.C.; Sesma, N. Accuracy of Digital Technologies for the Scanning of Facial, Skeletal, and Intraoral Tissues: A Systematic Review. J. Prosthet. Dent. 2019, 121, 246–251. [Google Scholar] [CrossRef]
- Nada, R.M.; Maal, T.J.J.; Breuning, K.H.; Bergé, S.J.; Mostafa, Y.A.; Kuijpers-Jagtman, A.M. Accuracy and Reproducibility of Voxel Based Superimposition of Cone Beam Computed Tomography Models on the Anterior Cranial Base and the Zygomatic Arches. PLoS ONE 2011, 6, e16520. [Google Scholar] [CrossRef]
- Vercruyssen, M.; Fortin, T.; Widmann, G.; Jacobs, R.; Quirynen, M. Different Techniques of Static/Dynamic Guided Implant Surgery: Modalities and Indications. Periodontol. 2000 2014, 66, 214–227. [Google Scholar] [CrossRef]
- Abduo, J.; Lau, D. Accuracy of Static Computer-Assisted Implant Placement in Long Span Edentulous Area by Novice Implant Clinicians: A Cross-Sectional In Vitro Study Comparing Fully-Guided, Pilot-Guided, and Freehand Implant Placement Protocols. Clin. Implant Dent. Relat. Res. 2021, 23, 561–568. [Google Scholar] [CrossRef]
- Demirturk Kocasarac, H.; Ustaoglu, G.; Bayrak, S.; Katkar, R.; Geha, H.; Deahl, S.T.; Mealey, B.L.; Danaci, M.; Noujeim, M. Evaluation of Artifacts Generated by Titanium, Zirconium, and Titanium–Zirconium Alloy Dental Implants on MRI, CT, and CBCT Images: A Phantom Study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2019, 127, 535–544. [Google Scholar] [CrossRef]
- Zahran, M.H.; Fenton, A. A Radiopaque Implant Template for Partially Edentulous Patients. J. Prosthet. Dent. 2010, 103, 390–392. [Google Scholar] [CrossRef] [PubMed]
- Balshi, S.F.; Wolfinger, G.J.; Balshi, T.J. Surgical Planning and Prosthesis Construction Using Computed Tomography, CAD/CAM Technology, and the Internet for Immediate Loading of Dental Implants. J. Esthet. Restor. Dent. 2006, 18, 312–323. [Google Scholar] [CrossRef] [PubMed]
- Kopp, K.C.; Koslow, A.H.; Abdo, O.S. Predictable Implant Placement with a Diagnostic/Surgical Template and Advanced Radiographic Imaging. J. Prosthet. Dent. 2003, 89, 611–615. [Google Scholar] [CrossRef] [PubMed]
- Wu, Q.; Wu, J.; Tan, Y.; Sun, J.; Yu, H. A Chairside Digital Radiographic Guide for Registering Digital Casts to Cone Beam Computed Tomography Scans with Strong Metallic Artifacts. J. Prosthet. Dent. 2024, 132, 1104–1111. [Google Scholar] [CrossRef]
- De Vico, G.; Ferraris, F.; Arcuri, L.; Guzzo, F.; Spinelli, D. A Novel Workflow for Computer Guided Implant Surgery Matching Digital Dental Casts and CBCT Scan. Oral Implantol. 2016, 9, 33–48. [Google Scholar]
- Shimizu, H.; Arakawa, H.; Mino, T.; Kurosaki, Y.; Tokumoto, K.; Kuboki, T. Newly Developed Data-Matching Methodology for Oral Implant Surgery Allowing the Automatic Deletion of Metal Artifacts in 3D-CT Images Using New Reference Markers: A Case Report. J. Prosthodont. Res. 2021, 65, 125–129. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Tew, I.M.; Leong, X.F.; Mohd-Said, S. Radiopaque Marker Impression and 3D Boolean Inversion for Metal Artifact-Distorted Same-Day Implant Planning: A Digital Workflow. Int. J. Comput. Dent. 2025, 28, 283–294. [Google Scholar]
- Oh, J.H.; An, X.; Jeong, S.M.; Choi, B.H. Digital Workflow for Computer-Guided Implant Surgery in Edentulous Patients: A Case Report. J. Oral Maxillofac. Surg. 2017, 75, 2541–2549. [Google Scholar] [CrossRef] [PubMed]
- Sutare, A.; Parihar, A.; Reddy, P.; Singh, R.; Ac, V. Influence of Windowing and Evaluation of Metal Artifact Reduction Algorithm on Five Different Restorative Materials by Using Different Cone Beam Computed Tomography (CBCT) Scanners: A CBCT Study. Cureus 2023, 15, e41742. [Google Scholar] [CrossRef]
- Pekkan, G. Radiopacity of Dental Materials: An Overview. Avicenna J. Dent. Res. 2016, 8, e36847. [Google Scholar] [CrossRef]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).