Increased Functional Mobility in Healthy Elderly Individuals After Six Months of Adapted Taekwondo Practice
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Experimental Protocol
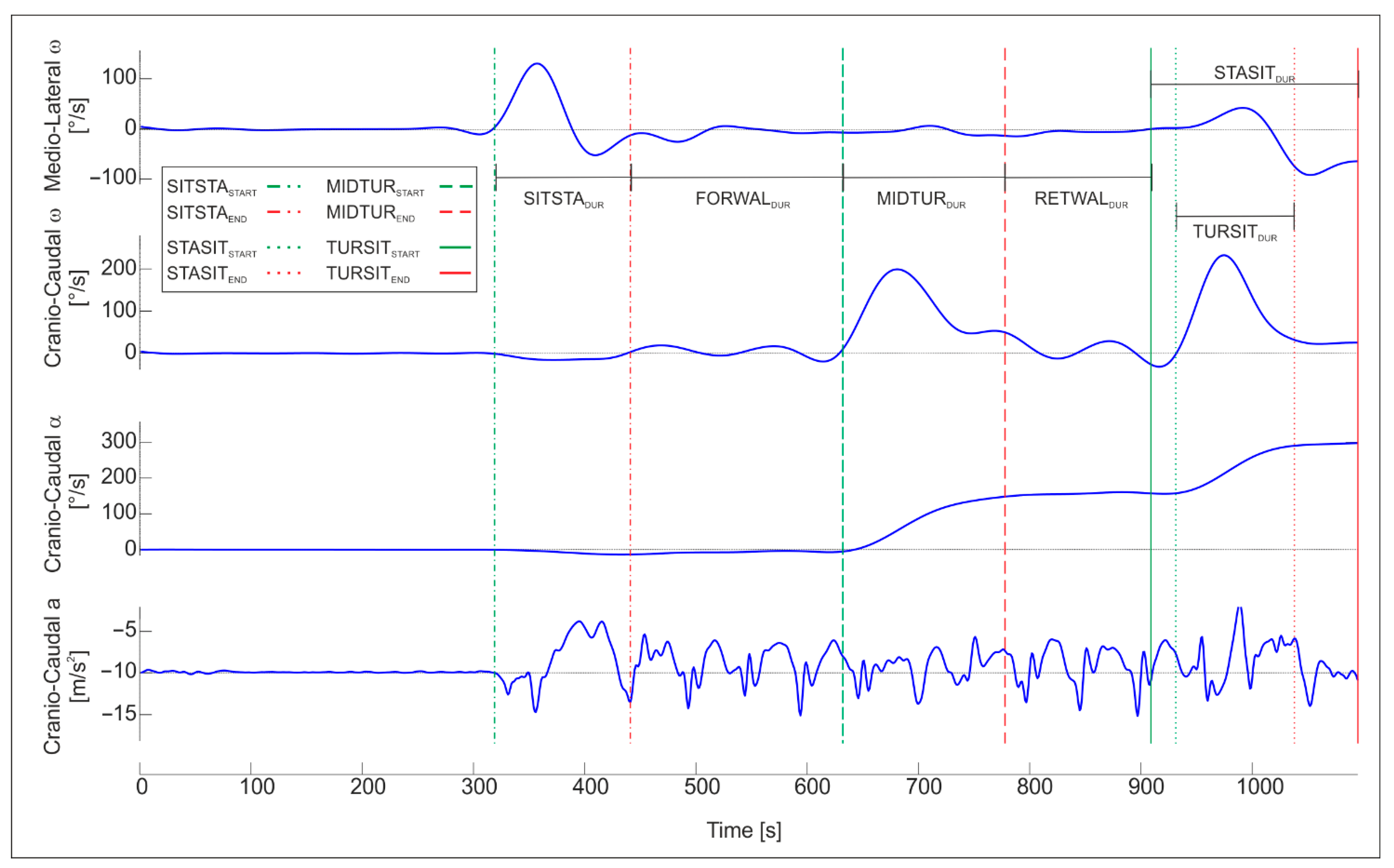
2.4. Data Analysis
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United Nations. World Population Ageing 2019; ST/ESA/SER.A/444; United Nations: Manhattan, NY, USA, 2020. [Google Scholar]
- Taffet, G.E. Physiology of Aging. In Geriatric Medicine; Springer: Cham, Switzerland, 2024; pp. 1555–1565. [Google Scholar]
- Tieland, M.; Trouwborst, I.; Clark, B.C. Skeletal muscle performance and ageing. J. Cachexia Sarcopenia Muscle 2018, 9, 3–19. [Google Scholar] [CrossRef]
- Macaluso, A.; De Vito, G. Muscle strength, power and adaptations to resistance training in older people. Eur. J. Appl. Physiol. 2004, 91, 450–472. [Google Scholar] [CrossRef]
- Rodrigues, F.; Domingos, C.; Monteiro, D.; Morouço, P. A Review on Aging, Sarcopenia, Falls, and Resistance Training in Community-Dwelling Older Adults. Int. J. Environ. Res. Public Health 2022, 19, 874. [Google Scholar] [CrossRef] [PubMed]
- Partridge, L.; Deelen, J.; Slagboom, P.E. Facing up to the global challenges of ageing. Nature 2018, 561, 45–56. [Google Scholar] [CrossRef] [PubMed]
- Candela, F.; Zucchetti, G.; Ortega, E.; Rabaglietti, E.; Magistro, D. Preventing Loss of Basic Activities of Daily Living and Instrumental Activities of Daily Living in Elderly: Identification of Individual Risk Factors in a Holistic Perspective. Holist. Nurs. Pract. 2015, 29, 313–322. [Google Scholar] [CrossRef] [PubMed]
- Salari, N.; Darvishi, N.; Ahmadipanah, M.; Shohaimi, S.; Mohammadi, M. Global prevalence of falls in the older adults: A comprehensive systematic review and meta-analysis. J. Orthop. Surg. Res. 2022, 17, 334. [Google Scholar] [CrossRef]
- Ikegami, S.; Takahashi, J.; Uehara, M.; Tokida, R.; Nishimura, H.; Sakai, A.; Kato, H. Physical performance reflects cognitive function, fall risk, and quality of life in community-dwelling older people. Sci. Rep. 2019, 9, 12242. [Google Scholar] [CrossRef]
- Rubenstein, L.Z. Falls in older people: Epidemiology, risk factors and strategies for prevention. Age Ageing 2006, 35 (Suppl. 2), ii37–ii41. [Google Scholar] [CrossRef]
- Galluzzo, L.; Gandin, C.; Ghirini, S.; Scafato, E. L’invecchiamento della popolazione: Opportunità o sfida. Not. Ist. Super. Sanità 2012, 25, iii–vi. [Google Scholar]
- Podsiadlo, D.; Richardson, S. The timed "Up & Go": A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar]
- Beauchet, O.; Fantino, B.; Allali, G.; Muir, S.W.; Montero-Odasso, M.; Annweiler, C. Timed Up and Go test and risk of falls in older adults: A systematic review. J. Nutr. Health Aging 2011, 15, 933–938. [Google Scholar] [CrossRef]
- Kang, L.; Han, P.; Wang, J.; Ma, Y.; Jia, L.; Fu, L.; Yu, H.; Chen, X.; Niu, K.; Guo, Q. Timed Up and Go Test can predict recurrent falls: A longitudinal study of the community-dwelling elderly in China. Clin. Interv. Aging 2017, 12, 2009–2016. [Google Scholar] [CrossRef] [PubMed]
- Ortega-Bastidas, P.; Gómez, B.; Aqueveque, P.; Luarte-Martínez, S.; Cano-de-la-Cuerda, R. Instrumented Timed Up and Go Test (iTUG)-More Than Assessing Time to Predict Falls: A Systematic Review. Sensors 2023, 23, 3426. [Google Scholar] [CrossRef] [PubMed]
- Dierick, F.; Stoffel, P.; Schütz, G.; Buisseret, F. High Specificity of Single Inertial Sensor-Supplemented Timed Up and Go Test for Assessing Fall Risk in Elderly Nursing Home Residents. Sensors 2022, 22, 2339. [Google Scholar] [CrossRef] [PubMed]
- Close, J.C.T.; Lord, S.R. Fall prevention in older people: Past, present and future. Age Ageing 2022, 51, afac105. [Google Scholar] [CrossRef]
- Landi, F.; Abbatecola, A.M.; Provinciali, M.; Corsonello, A.; Bustacchini, S.; Manigrasso, L.; Cherubini, A.; Bernabei, R.; Lattanzio, F. Moving against frailty: Does physical activity matter? Biogerontology 2010, 11, 537–545. [Google Scholar] [CrossRef]
- Feng, F.; Xu, H.; Sun, Y.; Zhang, X.; Li, N.; Sun, X.; Tian, X.; Zhao, R. Exercise for prevention of falls and fall-related injuries in neurodegenerative diseases and aging-related risk conditions: A meta-analysis. Front. Endocrinol. 2023, 14, 1187325. [Google Scholar] [CrossRef]
- DelCastillo-Andrés, Ó.; Toronjo-Hornillo, L.; Toronjo-Urquiza, M.T.; Cachón Zagalaz, J.; Campos-Mesa, M.D.C. Adapted Utilitarian Judo: The Adaptation of a Traditional Martial Art as a Program for the Improvement of the Quality of Life in Older Adult Populations. Societies 2018, 8, 57. [Google Scholar] [CrossRef]
- Huang, Z.; Feng, Y.; Li, Y.; Lv, C. Systematic review and meta-analysis: Tai Chi for preventing falls in older adults. BMJ Open 2017, 7, e013661. [Google Scholar] [CrossRef]
- Kim, C.Y.; Jeong, H.W.; Baek, C.Y.; Kim, S.W.; Kim, H.D. Effects of Taekkyon-based exercise program on balance, lower extremity strength, and gait parameters in community-dwelling older women: Randomized controlled trial. Medicine 2024, 103, e37463. [Google Scholar] [CrossRef]
- Miller, I.; Climstein, M.; Vecchio, L.D. Functional Benefits of Hard Martial Arts for Older Adults: A Scoping Review. Int. J. Exerc. Sci. 2022, 15, 1430–1443. [Google Scholar] [CrossRef]
- Bubela, D.; Sacharko, L.; Chan, J.; Brady, M. Balance and Functional Outcomes for Older Community-Dwelling Adults Who Practice Tai Chi and Those Who Do Not: A Comparative Study. J. Geriatr. Phys. Ther. 2019, 42, 209. [Google Scholar] [CrossRef]
- Li, X.; Bae, J.; Lim, B.; Seo, J.; Sung, Y.; Jiang, S.; Jamrasi, P.; Ahn, S.; Shin, C.; Pan, M.; et al. Impact of Taekwondo training on cognitive and physical function in elderly individuals: A comprehensive review of randomized controlled trials. Complement. Ther. Clin. Pract. 2024, 57, 101878. [Google Scholar] [CrossRef]
- Park, J.; Kim, B.; Jeong, M.; Jung, H.; Hong, G.; Park, S.K. Effects of Taekwondo training on thigh muscle cross-sectional area, health-related physical fitness, HbA1c, and GLP-1 in sedentary older women. Front. Sports Act. Living 2025, 7, 1553202. [Google Scholar] [CrossRef]
- Cromwell, R.L.; Meyers, P.M.; Meyers, P.E.; Newton, R.A. Tae Kwon Do: An effective exercise for improving balance and walking ability in older adults. J. Gerontology. Ser. A Biol. Sci. Med. Sci. 2007, 62, 641–646. [Google Scholar] [CrossRef]
- Linhares, D.G.; dos Santos, A.O.B.; dos Santos, L.L.; Marcos-Pardo, P.J.; de Souza Cordeiro, L.; de Castro, J.B.P.; de Souza Vale, R.G. Effects of taekwondo on health in older people: A systematic review. Retos 2022, 46, 36–42. [Google Scholar] [CrossRef]
- Weiss, A.; Herman, T.; Plotnik, M.; Brozgol, M.; Giladi, N.; Hausdorff, J.M. An instrumented timed up and go: The added value of an accelerometer for identifying fall risk in idiopathic fallers. Physiol. Meas. 2011, 32, 2003–2018. [Google Scholar] [CrossRef]
- Bergamini, E.; Ligorio, G.; Summa, A.; Vannozzi, G.; Cappozzo, A.; Sabatini, A.M. Estimating orientation using magnetic and inertial sensors and different sensor fusion approaches: Accuracy assessment in manual and locomotion tasks. Sensors 2014, 14, 18625–18649. [Google Scholar] [CrossRef] [PubMed]
- Quinzi, F.; Camomilla, V.; Bratta, C.; Piacentini, M.F.; Sbriccoli, P.; Vannozzi, G. Hopping skill in individuals with Down syndrome: A qualitative and quantitative assessment. Hum. Mov. Sci. 2021, 78, 102821. [Google Scholar] [CrossRef] [PubMed]
- Quinzi, F.; Camomilla, V.; Sbriccoli, P.; Piacentini, M.F.; Vannozzi, G. Assessing motor competence in kicking in individuals with Down syndrome through wearable motion sensors. J. Intellect. Disabil. Res. JIDR 2022, 66, 558–567. [Google Scholar] [CrossRef] [PubMed]
- Weiss, A.; Mirelman, A.; Buchman, A.S.; Bennett, D.A.; Hausdorff, J.M. Using a body-fixed sensor to identify subclinical gait difficulties in older adults with IADL disability: Maximizing the output of the timed up and go. PLoS ONE 2013, 8, e68885. [Google Scholar] [CrossRef]
- Bohannon, R.W. Reference values for the timed up and go test: A descriptive meta-analysis. J. Geriatr. Phys. Ther. 2006, 29, 64–68. [Google Scholar] [CrossRef] [PubMed]
- Long, J.; Cai, T.; Huang, X.; Zhou, Y.; Kuang, J.; Wu, L. Reference value for the TUGT in healthy older people: A systematic review and meta-analysis. Geriatr. Nurs. 2020, 41, 325–330. [Google Scholar] [CrossRef] [PubMed]
- Lopez, P.; Pinto, R.S.; Radaelli, R.; Rech, A.; Grazioli, R.; Izquierdo, M.; Cadore, E.L. Benefits of resistance training in physically frail elderly: A systematic review. Aging Clin. Exp. Res. 2018, 30, 889–899. [Google Scholar] [CrossRef]
- Chen, W.; Li, M.; Li, H.; Lin, Y.; Feng, Z. Tai Chi for fall prevention and balance improvement in older adults: A systematic review and meta-analysis of randomized controlled trials. Front. Public Health 2023, 11, 1236050. [Google Scholar] [CrossRef] [PubMed]
- Mortaza, N.; Abu Osman, N.A.; Mehdikhani, N. Are the spatio-temporal parameters of gait capable of distinguishing a faller from a non-faller elderly? Eur. J. Phys. Rehabil. Med. 2014, 50, 677–691. [Google Scholar]
- Lee, S.H.; Scott, S.D.; Pekas, E.J.; Lee, S.; Lee, S.H.; Park, S.Y. Taekwondo training reduces blood catecholamine levels and arterial stiffness in postmenopausal women with stage-2 hypertension: Randomized clinical trial. Clin. Exp. Hypertens. 2019, 41, 675–681. [Google Scholar] [CrossRef]
- Çiftçi, R.; Kurtoğlu, A.; Çar, B.; Karavaş, E.; Eken, Ö.; Söyler, M.; Ardigò, L.P.; Nobari, H. Exploring the quadriceps muscle architecture variations in various sports disciplines: A comparative analysis of football, taekwondo, and athletics. J. Sports Med. Phys. Fit. 2024, 64, 728–736. [Google Scholar] [CrossRef]
- Van Hooren, B.; Aagaard, P.; Monte, A.; Blazevich, A.J. The role of pennation angle and architectural gearing to rate of force development in dynamic and isometric muscle contractions. Scand. J. Med. Sci. Sports 2024, 34, e14639. [Google Scholar] [CrossRef]
- Jeon, W.; Whitall, J.; Griffin, L.; Westlake, K.P. Trunk kinematics and muscle activation patterns during stand-to-sit movement and the relationship with postural stability in aging. Gait Posture 2021, 86, 292–298. [Google Scholar] [CrossRef]
- Sbriccoli, P.; Camomilla, V.; Di Mario, A.; Quinzi, F.; Figura, F.; Felici, F. Neuromuscular control adaptations in elite athletes: The case of top level karateka. Eur. J. Appl. Physiol. 2010, 108, 1269–1280. [Google Scholar] [CrossRef]
- Quinzi, F.; Camomilla, V.; Felici, F.; Di Mario, A.; Sbriccoli, P. Differences in neuromuscular control between impact and no impact roundhouse kick in athletes of different skill levels. J. Electromyogr. Kinesiol. 2013, 23, 140–150. [Google Scholar] [CrossRef]
- Quinzi, F.; Camomilla, V.; Felici, F.; Di Mario, A.; Sbriccoli, P. Agonist and antagonist muscle activation in elite athletes: Influence of age. Eur. J. Appl. Physiol. 2015, 115, 47–56. [Google Scholar] [CrossRef]
- Quinzi, F.; Camomilla, V.; Di Mario, A.; Felici, F.; Sbriccoli, P. Repeated Kicking Actions in Karate: Effect on Technical Execution in Elite Practitioners. Int. J. Sports Physiol. Perform. 2016, 11, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.; Roh, H. Taekwondo Enhances Cognitive Function as a Result of Increased Neurotrophic Growth Factors in Elderly Women. Int. J. Environ. Res. Public Health 2019, 16, 962. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Lee, H. Comparison of the Lower Extremity Kinematics and Center of Mass Variations in Sit-to-Stand and Stand-to-Sit Movements of Older Fallers and Nonfallers. Arch. Rehabil. Res. Clin. Transl. 2022, 4, 100181. [Google Scholar] [CrossRef]
- Schlüter-Brust, K.; Leistenschneider, P.; Dargel, J.; Springorum, H.P.; Eysel, P.; Michael, J.W. Acute Injuries in Taekwondo. Int. J. Sports Med. 2011, 32, 629–634. [Google Scholar] [CrossRef] [PubMed]
| Participant Characteristics | ||
|---|---|---|
| F (n = 9) | M (n = 11) | |
| Age (years) | 67 ± 3.3 | 62.5 ± 3.9 |
| Stature (m) | 1.53 ± 0.02 | 1.71 ± 0.06 |
| Body Mass (kg) | 66.3 ± 7.4 | 84 ± 15.1 |
| Acronyms | Variable Definitions | Unit |
|---|---|---|
| TUGDUR | Overall TUG duration = Δt (Stasitend − Sitstastart) | s |
| SITSTADUR | Sit-to-stand phase duration = Δt (Sitstaend − Sitstastart) | s |
| FORWALDUR | Stand-to-sit phase duration = Δt (Stasitend − Stasitstart) | s |
| MIDTURDUR | Mid-turn phase duration = Δt (Midturend − Midturstart) | s |
| RETWALDUR | Turn-to-sit phase duration= Δt (Tursitend − Tursitstart) | s |
| TURSITDUR | Forward walk phase duration= Δt (Midturstart − Sitstaend) | s |
| STASITDUR | Return walk phase duration =Δt (Stasitend − Midturend) | s |
| MIDTURωCC-PEAK | Peak angular velocity about the cranio-caudal axis of the mid-turn phase | °/s |
| TURSITωCC-PEAK | Peak angular velocity about the cranio-caudal axis of the turn-to-sit phase | °/s |
| APRMSFW | Root mean square of linear acceleration signal on antero-posterior axis during forward walk | m/s2 |
| CCRMSFW | Root mean square of linear acceleration signal on cranio-caudal axis during forward walk | m/s2 |
| MLRMSFW | Root mean square of linear acceleration signal on medio-lateral axis during forward walk | m/s2 |
| APRMSRW | Root mean square of linear acceleration signal on antero-posterior axis during return walk | m/s2 |
| CCRMSRW | Root mean square of linear acceleration signal on cranio-caudal axis during return walk | m/s2 |
| MLRMSRW | Root mean square of linear acceleration signal on medio-lateral axis during return walk | m/s2 |
| SITSTAαFLEX | Peak trunk flexion angle during sit to stand | ° |
| STASITαFLEX | Peak trunk flexion angle during stand to sit | ° |
| SITSTAωFLEX | Peak angular velocity during trunk flexion of sit to stand | °/s |
| STASITωFLEX | Peak angular velocity during trunk flexion of stand to sit | °/s |
| SITSTAωEXT | Peak angular velocity during trunk extension of sit to stand | °/s |
| STASITωEXT | Peak angular velocity during trunk extension of stand to sit | °/s |
| Variables | T0 | T6 | p-Value | ||||
|---|---|---|---|---|---|---|---|
| T1 | T2 | T1 | T2 | Time | Trial | Time × Trial | |
| TUGDUR (s) | 9.45 ± 1.10 | 9.36 ± 1.10 | 8.77 ± 1.00 | 8.44 ± 0.96 | * 0.002 | † 0.016 | 0.107 |
| SITSTADUR (s) | 1.45 ± 0.23 | 1.48 ± 0.26 | 1.46 ± 0.32 | 1.49 ± 0.28 | 0.930 | 0.455 | 0.995 |
| FORWALDUR (s) | 1.92 ± 0.36 | 1.80 ± 0.41 | 1.55 ± 0.38 | 1.57 ± 0.50 | * 0.002 | 0.486 | 0.369 |
| MIDTURDUR (s) | 1.82 ± 0.27 | 1.90 ± 0.31 | 2.00 ± 0.37 | 1.85 ± 0.30 | 0.289 | 0.396 | ‡ 0.023 |
| RETWALDUR (s) | 1.68 ± 0.37 | 1.67 ± 0.37 | 1.41 ± 0.35 | 1.36 ± 0.35 | * 0.001 | 0.421 | 0.842 |
| TURSITDUR (s) | 1.36 ± 0.24 | 1.44 ± 0.27 | 1.34 ± 0.23 | 1.40 ± 0.23 | 0.532 | † 0.007 | 0.781 |
| STASITDUR (s) | 2.13 ± 0.44 | 2.12 ± 0.34 | 1.93 ± 0.39 | 1.80 ± 0.51 | * 0.043 | 0.376 | 0.457 |
| MIDTURωCC-PEAK (°/s) | 162.2 ± 29.1 | 154.9 ± 32.2 | 149.6 ± 25.2 | 164.1 ± 35.4 | 0.807 | 0.427 | ‡ 0.001 |
| TURSITωCC-PEAK (°/s) | 197.5 ± 40.0 | 197.5 ± 40.1 | 197.3 ± 34.5 | 198.9 ± 35.2 | 0.895 | 0.867 | 0.864 |
| APRMSFW (m/s2) | 2.97 ± 0.74 | 2.93 ± 0.63 | 3.36 ± 0.83 | 3.37 ± 0.85 | * 0.031 | 0.823 | 0.683 |
| CCRMSFW (m/s2) | 9.65 ± 0.20 | 9.70 ± 0.22 | 9.52 ± 0.36 | 9.57 ± 0.35 | 0.105 | † 0.024 | 0.883 |
| MLRMSFW (m/s2) | 1.40 ± 0.27 | 1.45 ± 0.28 | 1.54 ± 0.32 | 1.58 ± 0.34 | 0.090 | 0.096 | 0.838 |
| APRMSRW (m/s2) | 2.44 ± 0.94 | 2.32 ± 0.82 | 2.95 ± 1.17 | 2.94 ± 1.16 | * 0.034 | 0.333 | 0.416 |
| CCRMSRW (m/s2) | 9.89 ± 0.26 | 9.93 ± 0.29 | 9.73 ± 0.61 | 9.80 ± 0.46 | 0.145 | † 0.026 | 0.364 |
| MLRMSRW (m/s2) | 1.54 ± 0.35 | 1.69 ± 0.50 | 1.67 ±0.48 | 1.54 ± 0.38 | 0.748 | 0.685 | 0.176 |
| SITSTAαFLEX (°) | 0.40 ± 0.80 | 0.37 ± 0.84 | 0.10 ± 0.28 | 0.24 ± 0.42 | 0.329 | 1.00 | 0.835 |
| STASITαFLEX (°) | 6.95 ± 9.82 | 12.0 ± 15.6 | 8.97 ± 10.7 | 10.5 ± 11.0 | 0.932 | 0.147 | 0.380 |
| SITSTAωFLEX (°/s) | 99.4 ± 20.5 | 94.9 ± 21.5 | 100.4 ± 21.9 | 102.7 ± 23.2 | 0.328 | 0.342 | 0.149 |
| STASITωFLEX (°/s) | 54.5 ± 13.6 | 53.3 ± 13.3 | 59.4 ± 13.7 | 51.7 ± 32.9 | 0.721 | 0.268 | 0.349 |
| SITSTAωEXT (°/s) | −57.8 ± 17.0 | −55.3 ± 11.8 | −52.9 ± 15.1 | −54.5 ± 18.0 | 0.387 | 0.743 | 0.295 |
| STASITωEXT (°/s) | −80.0 ± 19.0 | −85.5 ± 16.7 | −85.6 ± 20.6 | −85.0 ± 20.8 | 0.530 | 0.123 | 0.089 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lia, C.G.; Greco, F.; Muscari, M.A.; Spadafora, M.; Chiodo, S.; Emerenziani, G.P.; Quinzi, F. Increased Functional Mobility in Healthy Elderly Individuals After Six Months of Adapted Taekwondo Practice. Appl. Sci. 2025, 15, 8932. https://doi.org/10.3390/app15168932
Lia CG, Greco F, Muscari MA, Spadafora M, Chiodo S, Emerenziani GP, Quinzi F. Increased Functional Mobility in Healthy Elderly Individuals After Six Months of Adapted Taekwondo Practice. Applied Sciences. 2025; 15(16):8932. https://doi.org/10.3390/app15168932
Chicago/Turabian StyleLia, Carmen Giulia, Francesca Greco, Mario Antonio Muscari, Marco Spadafora, Salvatore Chiodo, Gian Pietro Emerenziani, and Federico Quinzi. 2025. "Increased Functional Mobility in Healthy Elderly Individuals After Six Months of Adapted Taekwondo Practice" Applied Sciences 15, no. 16: 8932. https://doi.org/10.3390/app15168932
APA StyleLia, C. G., Greco, F., Muscari, M. A., Spadafora, M., Chiodo, S., Emerenziani, G. P., & Quinzi, F. (2025). Increased Functional Mobility in Healthy Elderly Individuals After Six Months of Adapted Taekwondo Practice. Applied Sciences, 15(16), 8932. https://doi.org/10.3390/app15168932






