Abstract
Objectives: To investigate the efficacy of the assessment methods that are used to diagnose posterior tibialis tendon dysfunction (PTTD) and investigate how the results of these assessments can be used to instruct non-surgical treatments. Design: Systematic review. Data sources: Searches were conducted up to January 2023 in the PubMed, Scopus, Science Direct, Embase, Web of Science and Lilacs databases. Study eligibility criteria: Studies which included patients over 18 years of age, diagnosed with PTTD, which describe the assessments used to aid in the non-surgical treatment of PTTD in comparison with another type of assessment. All types of studies apart from protocols, letters to editor and other systematic reviews and meta-analysis were included. Study appraisal and synthesis methods: Two blinded reviewers performed screening, data extraction, and methodological quality assessments using the QUADAS-2. Results: A total of 15 observational studies were included in the review. Assessment methods included were verbal assessments, physical examinations, and imaging (magnetic resonance imaging (MRI), ultrasound (US), and radiographs). The single-heel rise test was a commonly mentioned physical examination, showing reliability in one study but contradicting in another. MRI was frequently described as the “gold standard”. However, US showed both comparable accuracy and advantages compared to MRI, such as cost-effectiveness and real-time examinations. Conclusions: There are many assessment methods described in the literature and, due to the lack of accuracy of the tests, a mixture of tests should be used to assess PTTD. The parameters from the tests can provide a diagnosis of PTTD, but do not offer detail on how they assist the non-surgical treatment of the condition.
1. Introduction
Posterior tibialis tendon dysfunction (PTTD) is a progressive and highly disabling condition, which causes pain, changes in gait, global weakness, and deformity in its later stages [1,2,3]. It is a condition which often goes undiagnosed, even when deformity and pain are present [4]. In some cases, the journey for patients in receiving the correct diagnosis or correct care can take years, leaving patients feeling lost. Moreover, with the progression of the condition, patients are left with treatment burdens and a negative outlook [5]. PTTD is associated with inflammation and/or elongation of the tendon of the tibialis posterior (TP). In the case of elongation, this can cause a flatfoot deformity, arthritis, changes in gait, and pain [3]. PTTD is a condition which mainly affects women and has been shown to have a prevalence of over 3% in women over 40 years of age [4].
Due to the evolving nature of the condition, many authors have divided the condition into stages, to better guide treatment methodology. Johnson and Storm were the first to stage the condition in 1989 [6]. This was later revised by multiple authors, including Myerson in 1996 [7], and further by Bluman et al. in 2007 [8]. In 2012, Raikin et al. developed the Rearfoot Ankle Midfoot (RAM) classification, which has also been modified from the original Johnson and Storm system, and introduces more detail regarding the rearfoot, ankle, and midfoot [9]. Other classifications systems have been suggested, such as the “Grand Rapids Arch Collapse Classification” in 2019 [10] as well as a consensus group classification in 2020 [11]. It has been described in one paper that the most commonly used system is still the original Johnson and Storm classification; this has not been validated [12]. All the described classification systems provide an algorithmic approach and suggest treatment methodologies. However, although the more recent systems provide more detail, they still categorize patient presentations into types and provide generic treatment suggestions such as orthotics and physiotherapy.
All these category systems require an initial assessment of the foot and ankle, to determine the condition of the tendon, function, and deformity of the foot. The aim of this study is to look at the efficacy of the assessment methods used to diagnose PTTD, defined in the research, as well as how the results of these assessments are used to instruct non-surgical treatments. This review holds the idea that, perhaps, individual assessments provide more data than the categorization systems, and can be used for the effective non-surgical treatment of PTTD.
2. Materials and Methods
This systematic review is registered on the International Prospective Register of Systematic Reviews (PROSPERO): CRD42023388190. In order to respond to the aims set out in this present study, a systematic review was carried out, looking for papers which describe the assessments used to aid in non-surgical treatment of PTTD. This was carried out to answer the following hypothesis: the guidance provided from the results of these assessments is not sufficient to provide a specific non-surgical treatment.
The systematic review was conducted following the “Preferred reported items of systematic reviews and meta-analysis” (PRISMA) regulations and following the recommendations of the Cochrane Collaboration [13].
2.1. Selection Criteria
All studies were conducted in accordance with the following PECO structure:
- Types of studies
All types of studies apart from protocols, letters to the editor, and other systematic reviews and meta-analyses were considered.
- Participants
Studies included in this review were ones focused on adults over 18 years of age diagnosed with PTTD. Studies were excluded if their focus was on patients who presented with a congenital deformity (i.e., accessory bones) or who presented with a systemic disease (i.e., diabetes, rheumatoid arthritis) were excluded. However, studies were included if the study included participants with these conditions as part of the overall cohort.
Cadaver studies (in vitro) were also excluded.
- Type of exposure
Studies which describe the assessments used to aid in non-surgical treatment of PTTD were included. Articles were excluded if they were specifically related to an assessment which would aid surgical treatment only. Studies focused on assessments used for research purposes to describe the condition but not to aid non-surgical treatment or diagnosis were excluded.
Additionally, studies focused purely on complete tendon rupture, dislocation, spring ligament, or trauma to the bone were excluded. However, studies were included if the participants with these conditions were part of the overall cohort.
Papers focused on medication treatment and diagnostics (i.e., oral medication or injections) were also excluded.
- Comparison
Studies that compared the assessment with another type of assessment to explore PTTD or describe the assessment methodology.
- Outcome measure
The outcomes considered were those used to evaluate PTTD accurately, such as precision, sensitivity, or specificity.
2.2. Search Strategy
The search was conducted by two researchers independently (G.B. and G.G.N.) and the following electronic databases were queried: PubMed, Scopus, Science Direct, Embase, Web of Science, and Lilacs. The following medical subject headings (MeSHs) terms were used: “Tibialis Posterior Dysfunction”, “Dysfunction, Tibialis Posterior”, “Tibial Tendon Dysfunction, Posterior”, and “Posterior Tibial Tendon Insufficiency”. There were no restrictions added regarding date or language in this search. A secondary search was also performed analysing the references included in the articles obtained. Unpublished studies were not included. The last search was performed in January 2023.
The following search strategy was used: (((Dysfunction, Tibialis Posterior) OR (Tibialis Posterior Dysfunction)) OR (Tibial Tendon Dysfunction, Posterior)) OR (Posterior Tibial Tendon Insufficiency).
2.3. Study Selection
The selection of the studies was carried out by two researchers (G.B. and L.R.P.), both blinded to each other’s selection; following this, any disagreements were discussed to come to a consensus. After the selection of the papers from the databases, the duplicates were eliminated. After the elimination, a screening of the titles and abstracts was conducted, based on the inclusion and exclusion criteria. Full copies of the selected studies were then analysed to assess compliance with the eligibility criteria. The information on the phases of the selection process was described through a PRISMA flow diagram (Figure 1).
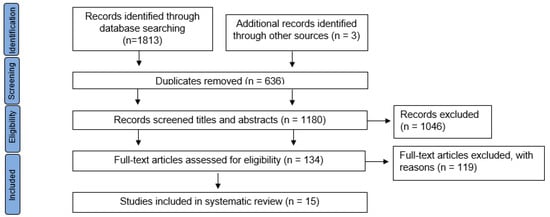
Figure 1.
PRISMA flow diagram for the studies included in this review.
The results were downloaded and imported into the Rayyan QCRI tool to help with the process of duplicates elimination [14].
2.4. Data Extraction and Synthesis
A table was created with the data extracted from the studies. An Excel document was used to structure the data collected. The main researcher (G.B.) extracted all the relevant data from the studies, such as the characteristics of the publication (author, country, year, study design), the PTTD stage, the number and gender of participants, the assessment methodology used, and the presence of a suggestion of non-surgical treatment dependent on the results of the assessment. This was then checked by another researcher (L.R.P.) to ensure that the data were correct.
2.5. Risk of Bias and Quality Assessment
To estimate the methodological quality/risk of bias of each of the included studies, a quality assessment tool was used. An independent peer review was implemented. To resolve cases in which the decisions of two reviewers differed (L.R.P. and E.L.R.), a third reviewer (G.G.N.) evaluated the text and decided upon its inclusion.
QUADAS-2 is the recommended tool for use in systematic reviews to evaluate the risk of bias and the applicability of primary diagnostic accuracy studies. It consists of 4 key domains, including patient selection, index test, reference standard, and flow of patients through the study and timing of the index test(s) and reference standard. Each domain is assessed in terms of the risk of bias and the first three are also assessed in terms of concerns regarding applicability. Those domains can be considered as high, low, or unclear risk. The QUADAS-2 tool is applied in 4 phases: summarize the review question, tailor the tool and produce review-specific guidance, construct a flow diagram for the primary study, and judge bias and applicability. This tool allows for more transparent rating of the bias and applicability of primary diagnostic accuracy studies [15].
2.6. Synthesis of Results
Data were extracted and pooled using RevMan 5.0 software [16]. Due to heterogeneity, it was not possible to conduct meta-analysis.
3. Results
Using the search strategy outlined above, we identified a total of 1813 studies in the databases, as well as three additional records identified through other sources, which was via the reference lists of the initial papers that were retrieved. Of these 1816 items, 636 were duplicated records. The remaining 1180 studies were evaluated by title and abstract by two independent reviewers (G.B. and L.R.P.). Of these, 1046 were excluded due to differences in inclusion criteria as they were studies based on surgery, systematic reviews and meta-analyses, cadaver studies, studies focused on the spring ligament, complete tendon rupture, dislocation, or trauma to the bone, and papers focused on medication treatment and diagnostics. After that, 134 full texts were assessed for eligibility and 119 were excluded because they were protocols, letters to editor, participants were under 18 years of age, participants were not diagnosed with PTTD, participants presented with congenital deformity or some systemic disease, studies which describe the assessments used to aid in surgical treatment of PTTD, or studies focused on assessments used for research purposes to describe the condition. Thus, only fifteen papers fully met the inclusion criteria. Figure 1 shows the PRISMA flow diagram for the studies included in this review.
3.1. General Characteristics of the Studies Assessed
A total of 933 (413 with PTTD) participants were included in the 15 studies. Of the 13 studies that specified gender, 67.25% of participants were female and 32.75% of participants were male. Of the 13 that included a mean age, the mean age was 48.96 years. All the studies included were observational studies, published between 1996 and 2021. The studies were conducted in Australia, Italy, Singapore, Austria, Taiwan, Switzerland, New Zealand, Korea, the USA, Slovenia, and the UK. The characteristics of the studies included are described in Table 1.

Table 1.
General characteristics of included studies.
The inclusion criteria varied among the studies, with some studies having strict criteria and others being more generalized. Some participants with a previous PTTD diagnosis or medical history indicating PTTD were included; however, no further examination was undertaken to confirm this [18,19,31]. Other participants were included based on signs and symptoms, such as localized oedema, asymmetric acquired flatfoot deformity, and pain [23]. Other papers described a physical examination, some of which provided details of how this was undertaken [17,20,22,24,25,28,29], and others only defining that an examination took place [26,27,30]. The tests used within the physical examination were a combination of the tests previously described in this review, as well as other measurements of foot posture and/or localized weakness.
In the papers reviewed, none of them provided any detail as to how the results of the tests would aid in classification or to inform the treatment methodology used. Kohls-Gatzoulis et al. indicated that some of the included patients went on to have custom-made shoes or ankle–foot orthoses, but not how these were designed [28]. Lim et al. also described that the included patients went on to have conservative treatment, such as physical therapy, immobilization, or orthotic devices [30]. Perry et al. described that, while the foot is flexible, it can be treated with a corrective orthotic device such as the University of California Biomechanics Laboratory brace, a moulded ankle–foot orthosis, an articulated moulded ankle–foot orthosis, or a Marzano brace. If the deformity is rigid, then the suggested orthosis is something that would accommodate the bony deformity [29]. Gonzalez et al. describe the importance of early detection, so that early conservative treatment such as orthotics and physiotherapy can prevent progression to later stages [20]. Although these papers mention orthotics and physiotherapy and discuss their importance, none of them link the findings of their assessments to specific treatments.
The results include several different methods for the assessment and diagnostics of PTTD; these include a variety of physical and imaging assessments, as well as subjective verbal assessments (Table S1: results of the included studies).
- Verbal Assessment
One paper focused on verbal assessment for the diagnosis of PTTD, which could then later warrant further investigation by a clinician to provide a definitive diagnosis. This was the only non-clinician-based assessment found in the search [28].
- Physical assessments
The physical examinations included as comparisons were the following: posterior tibial oedema sign (PTE) [17,26], first metatarsal rise (FMR) sign [31], first ray mobility test [22], unipedal standing balance test (USBT) [25], pain on palpation TP tendon [17], weakness with contraction [17], single-heel rise test (SHRT) [17,21,25], double-heel rise test (DHRT) [31], and the too-many-toes (TMT) sign [31].
The test which was mentioned the most in the included papers was the SHRT. This was used as a baseline comparison for other tests, such as the USBT, which showed a high success rate compared to controls [25]. One paper looked at the validity of the SHRT, pain on tendon palpation, swelling around the tendon, and pain/weakness with tibialis posterior contraction compared to ultrasound (US) findings. It concluded that the SHRT has good reliability. However, the other tests obtained only moderate reliability. The paper highlighted that, after using clinical findings, a diagnosis can be confirmed with US. However, US and clinical findings on their own are not sufficient [17]. The findings of this paper related to the PTE contradicts the findings of one paper, which found that, compared to magnetic resonance imaging (MRI), PTE had a sensitivity of 86% and a specificity of 100% [26]. Another paper looks at the FMR test, which has been shown to be more reliable than SHRT, DHRT, TMT, MRI, and radiographs, even at early stages. This was confirmed in some cases with surgical exploration [31]. The validity of the FMR test and the SHRT have been further confirmed in another study by MRI using the Movin score. However, when the tests are compared to each other, they show little significance [21]. Another study looked at the link between pain on palpation during a physical exam and PPTD findings using MRI and ultrasound. It concluded that pain on physical exam is strongly linked to tendonitis, but not to tendon tear. It also highlighted that US is less accurate in identifying tendon disruption [29]. The first ray mobility test was the only test found in the review that has been shown not to be correlated with PTTD [22].
- Imaging parameters
Within the literature, the most-described method for assessment was imaging, including MRI, US, and radiographs. MRI has been described by many papers; many of them describe it to be the “gold standard” [20,23,26,27].
Certain parameters using MRI are used to provide a positive diagnosis. One paper compared the cross-sectional area and the TP thickness, finding that TP cross-sectional area is the more sensitive measurement [19]. Another paper highlights that finding the pathology requires looking specifically at tenosynovial fluid rather than just intrasubstance TP pathology. Identifying a fluid width measuring greater than or equal to 9 mm is a predictor of stage 1 PTTD [20]. One study showed TP sheath fluid had modest specificity and fair–moderate sensitivity. The study also found excellent specificity and fair sensitivity for tibial spurring and unroofing of the talus. However, bone-bruise-like lesions were commonly seen both in the PTTD cases and in the control group [30].
US can also be used to assess subcutaneous swelling, which confirms the validity of the previous study, looking at swelling in a physical examination. A significant association between subcutaneous swelling and PTTD findings has been shown through US; therefore, more validation is provided for PTE [18].
- ○
- MRI and Ultrasound comparison
More recent papers have compared MRI to US. US has been shown to be highly efficient in detecting tears and inflammation in the tendon and is slightly more accurate than MRI. However, MRI can detect secondary signs of PTTD, such as bone marrow oedema, which US cannot. Furthermore, compared to surgical findings, both have demonstrated good accuracy [23]. However, another paper also found that US shows more false positives compared to MRI; therefore, it has been deemed to be less accurate [29]. One study found the correlation between surgical findings and MRI to be in 100% agreement with the diagnostics of type 1 PTTD, with 73% agreement in stage 2 and 60% agreement in stage 3; these results highlight that, perhaps, US imaging is more accurate in the earlier stages. The differences noted within these cases are between mixing partial tears and tendinosis [27]. Although some papers have identified US as being less accurate than MRI [29], it has also identified MRI and US to be comparable [27] or more accurate [23]. Furthermore, US has been deemed to have many advantages, as it is more convenient to use in clinics, it is cheaper, and it has the ability to be used to perform real-time examinations [27].
- ○
- Radiographs
One of the included studies compared MRI to radiographs. There was some correlation. However, as radiographs are only able to detect deformity, which is secondary to tendon tear and is neither tendinosis nor tenosynovitis, it is not as accurate as MRI or US [24].
3.2. Risk of Bias
Most of the included studies presented a low risk of bias. However, the study from Arnoldner et al. in 2015 [23] presented a high risk of bias in five of the items, as per the QUADAS assessment. Most of the included studies (13 out of 15) presented a low risk of bias in the flow and timing domains and in the index test from the applicability concerns. On the other hand, eight of the included studies presented a high risk of bias in the patient selection domain (Table 2).

Table 2.
Risk of bias assessment of included studies. QUADAS-2 results.
4. Discussion
The objective of this systematic review was to identify the assessment methodology used in the diagnosis and classification of PTTD, and to determine the accuracy of the tests and the parameters used to aid in non-surgical treatment decision making. It has been shown that the assessment methodologies used in the diagnosis and classification of PTTD present limitations in terms of accuracy and precision; therefore, it has been deemed necessary to combine the tests. This can then inform practitioners of the most appropriate assessment methodologies for the condition, ensuring that their practice is evidence-based.
Many methodologies are described in the literature to aid in the assessment of PTTD, all of which aim to provide a positive diagnosis of PTTD and inform practitioners about functional weakness, deformity, and damage to the tendon. Although the included papers describe these symptoms, none reported on how the findings from the tests aid in specific non-surgical treatment plans for PTTD.
The SHRT is the most frequently mentioned MSK examination; it has been used both as a test for use a comparison and as a test used for inclusion. However, the way in which the test is performed has been put into question, as it has been shown in a previous study that some patients with type 2 PTTD are able to invert their heel during the examination, giving a false negative result [32]. Although the SHRT has been validated [33], it has not been validated for the diagnostics of PTTD; therefore, the results of this test used for this purpose should be combined with other tests for further confirmation.
The included studies aimed to validate the tests used; one or more of the other tests included in this review had also not been previously validated. For patients who had planned surgeries, this meant surgical exploration could be used as a baseline. However, it was also stated that surgical exploration may be less accurate than MRI or US due to an inability to look within the tendon itself [23]. A combination of tests, such as the SLHR, palpation, swelling, and weakness, have also been compared to MRI and/or US. However, none of the tests have been shown to be 100% effective in the diagnosis of PTTD; therefore, it is advised to use a mixture of MSK assessment and imaging to provide a complete picture of the damage/inflammation present, as well as the functional deficit with which the patient presents [17,29].
There is a conflict between opinions on which imaging modality, i.e., US or MRI, should be used for PTTD diagnoses. MRI has been deemed to be more accurate in some cases; therefore, it is considered to be the gold standard. However, considering the fact that the conservative management of tendinosis and partial tear is similar, the importance of a truly accurate diagnosis of tendinosis and partial tear is low [27]. Furthermore, considering the other benefits of US, such as cost and real-time assessment, US has the potential to replace MRI as the gold standard for PTTD assessment [23]. Although radiography is an accurate way of defining deformity, it is not accurate in defining PTTD; it is unable to look at the structures linked to a flat foot deformity, such as the PTT, deltoid, or the spring ligament [24].
The accuracy of any assessment requires that the execution and interpretation are precise. Some studies have highlighted the use of paratenon fluid in the positive diagnosis of PTTD [34]. However, this has been found in asymptomatic patients; therefore, it could be identified as a normal finding [35]. The location of assessment has also been put into question, as some studies look only at the area below the medial malleolus and not above it. The area above the tendon been shown to be affected; moreover, this is normally the case in more severe presentations of PTTD [18].
Only one included study defines a subjective style assessment, with the patients being asked to provide details about their symptoms and/or medical history [28]. No full subjective assessment has been described where medical history and lifestyle details are considered to aid in treatment decisions.
The papers identified in this review do not describe the plethora of tests which are used to both diagnose and prescribe effective non-surgical treatments for PTTD; additionally, they do not describe how this is/should be followed up to determine the success or failure of said treatment. The research also does not describe how to assess for treatment failure, or what to do if treatment fails; for example, they do not address a bridge between non-surgical and surgical treatments. Gait examination was not found to be presented as a method used for clinical examination of PTTD in the literature search; however, a recent study interviewing podiatrists demonstrated that this is used as a part of their assessment approaches. It also highlighted that there was a lack of continuity in the assessments used and the parameters which were assessed [36]. Many studies describe the differences between the gait of patients with PTTD compared to controls without PTTD [1,2,3]. However, the use of gait systems or a description of visual gait analysis for patients with PTTD has not been described in the literature.
No papers describe a connection between the results of the examinations or how they connect to a detailed treatment plan. Many papers discuss the use of a classification method; therefore, one would assume that these findings would be used in combination with other assessments to guide further diagnostics. However, no papers show findings which can be used to aid in a non-surgical treatment plan, they only suggest a treatment path. This is not representative of a clinical assessment; this, in line with subjective assessments and patient histories, leads to a specific treatment plan.
In addition to this, although all the classification systems describe the necessity of orthotics with some detail, there is a lack of specificity in the method of manufacture, prescription, or type of orthoses to be used. Regarding the detail provided by the classification systems, Johnson and Storm describe the use of medial shoe wedges or orthotics [6]. Bluman et al. describe orthoses with medial posting and a custom brace [37]. Rankin describes medial rearfoot posted orthotic inserts and moulded ankle–foot orthoses [9]; finally, Myerson et al. provide the most detail, describing the use of an ankle stirrup brace, a medial heel-and-sole shoe wedge, a hinged ankle–foot orthosis, an orthotic arch-support, a stiff orthotic support, and a rigid ankle–foot orthosis [7]. However, the relationship between the assessments used, the classification systems, and detailed treatment plans is lacking.
There is a clear lack of awareness of PTTD, leading to poor referrals and delayed treatment [28]. In addition to this, this paper has identified that there is no assessment and treatment protocol defined when a patient has arrived at the correct practitioner. Due to the progressive nature of this condition, there is a need for a standardized assessment and treatment protocol, agreed upon by expert consensus. This protocol should include all assessments used within a clinical environment to aid in decision making, and the presentation of the plethora of treatment options available to the patient. More research is needed to develop assessment tools which provide data to help with non-surgical clinical decision making for PTTD.
The present study shows some strengths, one of them being that it is the first to define all the assessments described in the literature; additionally, it identifies a clear lack of evidence in support of the use of these assessments. This has clinical implications and can help to guide future clinical guidelines for assessment. However, some limitations are also present in this review. The main weakness of this systematic review is the lack of high quality and homogeneity in the included studies. Excluding papers which focused on surgical assessment and methodology linked to research may have excluded methods that could also be used in non-surgical approaches. However, the authors decided that the methods described in these papers were not realistic for use in an MSK clinic. Most papers have poor design, with few included subjects, no control group, or a control group including patients with other pathologies. Some studies are outdated, using parameters such as paratendon fluid, and looking only at the location below the medial malleolus; these approaches have since been deemed to be insufficient due to the pathology also being present superior to the malleolus.
5. Conclusions
The current assessment methods for posterior tibial tendon dysfunction (PTTD) exhibit limitations in terms of accuracy and precision. To improve the diagnosis of this condition, a combination of tests, including clinical evaluations, imaging studies, and laboratory testing, should be explored. This approach increases the validity and reliability of PTTD assessment, enabling healthcare providers to make more informed decisions regarding treatment. Further research is needed to validate this approach and explore the potential for developing more accurate assessment methods for PTTD.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/app14062362/s1, Table S1: Results of the included studies.
Author Contributions
Conceptualization, L.R.-P., G.B. and G.G.-N.; Formal analysis, L.R.-P. and E.L.-R.; Methodology, G.G.-N., A.G. and L.R.-P.; Writing—original draft, G.B. and L.R.-P.; Writing—review and editing, L.R.-P., G.B., E.L.-R., A.G. and G.G.-N. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Neville, C.; Flemister, A.S.; Houck, J. Total and distributed plantar loading in subjects with stage II tibialis posterior tendon dysfunction during terminal stance. Foot Ankle Int. 2013, 34, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Simonsen, M.B.; Yurtsever, A.; Næsborg-Andersen, K.; Leutscher, P.D.C.; Hørslev-Petersen, K.; Andersen, M.S.; Hirata, R.P. Tibialis posterior muscle pain effects on hip, knee and ankle gait mechanics. Hum. Mov. Sci. 2019, 66, 98–108. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Latt, L.D.; Martin, R.D.; Mannen, E.M. Postural Control Differences between Patients with Posterior Tibial Tendon Dysfunction and Healthy People during Gait. Int. J. Environ. Res. Public Health 2022, 19, 1301. [Google Scholar] [CrossRef] [PubMed]
- Kohls-Gatzoulis, J.; Woods, B.; Angel, J.C.; Singh, D. The prevalence of symptomatic posterior tibialis tendon dysfunction in women over the age of 40 in England. Foot Ankle Surg. 2009, 15, 75–81. [Google Scholar] [CrossRef]
- Campbell, R.F.; Morriss-Roberts, C.; Durrant, B.; Cahill, S. “I need somebody who knows about feet” a qualitative study investigating the lived experiences of conservative treatment for patients with posterior tibial tendon dysfunction. J. Foot Ankle Res. 2019, 12, 51. [Google Scholar] [CrossRef]
- Johnson, K.A.; Strom, D.E. Tibialis posterior tendon dysfunction. Clin. Orthop. Relat. Res. 1989, 239, 196–206. [Google Scholar] [CrossRef]
- Myerson, M.S. Adult acquired flatfoot deformity: Treatment of dysfunction of the posterior tibial tendon. Instr. Course Lect. 1997, 46, 393–405. [Google Scholar]
- Bluman, E.M.; Title, C.I.; Myerson, M.S. Posterior Tibial Tendon Rupture: A Refined Classification System. Foot Ankle Clin. 2007, 12, 233–249. [Google Scholar] [CrossRef]
- Raikin, S.M.; Winters, B.S.; Daniel, J.N. The RAM Classification. A Novel, Systematic Approach to the Adult-Acquired Flatfoot. Foot Ankle Clin. 2012, 17, 169–181. [Google Scholar] [CrossRef]
- Burkard, D.; Patton, D.; Padley, M.; Maskill, J.D.; Bohay, D.R.; Anderson, J.G. Statistical Validation of the Grand Rapids Arch Collapse Classification. Foot Ankle Orthop. 2019, 4, 2473011419834531. [Google Scholar] [CrossRef]
- Myerson, M.S.; Thordarson, D.B.; Johnson, J.E.; Hintermann, B.; Sangeorzan, B.J.; Deland, J.T.; Schon, L.C.; Ellis, S.J.; Netto, C.D.C. Classification and Nomenclature: Progressive Collapsing Foot Deformity. Foot Ankle Int. 2020, 41, 1271–1276. [Google Scholar] [CrossRef] [PubMed]
- Abousayed, M.M.; Tartaglione, J.P.; Rosenbaum, A.J.; Dipreta, J.A. Classifications in Brief: Johnson and Strom Classification of Adult-acquired Flatfoot Deformity. Clin. Orthop. Relat. Res. 2016, 474, 588–593. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 88, 105906. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- Whiting, P.F. QUADAS-2: A Revised Tool for the Quality Assessment of Diagnostic Accuracy Studies. Ann. Intern. Med. 2011, 155, 529. [Google Scholar] [CrossRef] [PubMed]
- The Nordic Cochrane Centre. The Cochrane Collaboration. Review Manager (RevMan); The Nordic Cochrane Centre: Lund, Sweden, 2014. [Google Scholar]
- Ross, M.H.; Smith, M.D.; Mellor, R.; Durbridge, G.; Vicenzino, B. Clinical tests of tibialis posterior tendinopathy: Are they reliable, and how well are they reflected in structural changes on imaging? J. Orthop. Sports Phys. Ther. 2021, 51, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Dammeyer, K.; Klochko, C.; Soliman, S. Sonographic finding of medial ankle subcutaneous edema and its association with posterior tibial tenosynovitis. J. Med. Ultrasound 2022, 30, 20–25. [Google Scholar] [CrossRef]
- Park, S.; Lee, J.; Cho, H.R.; Kim, K.; Bang, Y.-S.; Kim, Y.U. The predictive role of the posterior tibial tendon cross-sectional area in early diagnosing posterior tibial tendon dysfunction. Medicine 2020, 99, e21823. [Google Scholar] [CrossRef]
- Gonzalez, F.M.; Harmouche, E.; Robertson, D.D.; Umpierrez, M.; Singer, A.D.; Younan, Y.; Bariteau, J. Tenosynovial fluid as an indication of early posterior tibial tendon dysfunction in patients with normal tendon appearance. Skelet. Radiol. 2019, 48, 1377–1383. [Google Scholar] [CrossRef]
- Albano, D.; Martinelli, N.; Bianchi, A.; Romeo, G.; Bulfamante, G.; Galia, M.; Sconfienza, L.M. Posterior tibial tendon dysfunction: Clinical and magnetic resonance imaging findings having histology as reference standard. Eur. J. Radiol. 2018, 99, 55–61. [Google Scholar] [CrossRef]
- Heng, M.L.; Krishnasamy, P.; Kong, P.W. First ray mobility and posterior tibial tendon dysfunction (PTTD) in persons with flat foot: A case control study. Foot 2018, 37, 57–60. [Google Scholar] [CrossRef] [PubMed]
- Arnoldner, M.A.; Gruber, M.; Syré, S.; Kristen, K.-H.; Trnka, H.-J.; Kainberger, F.; Bodner, G. Imaging of posterior tibial tendon dysfunction—Comparison of high-resolution ultrasound and 3 T MRI. Eur. J. Radiol. 2015, 84, 1777–1781. [Google Scholar] [CrossRef]
- Lin, Y.-C.; Mhuircheartaigh, J.N.; Lamb, J.; Kung, J.W.; Yablon, C.M.; Wu, J.S. Imaging of adult flatfoot: Correlation of radiographic measurements with MRI. Am. J. Roentgenol. 2015, 204, 354–359. [Google Scholar] [CrossRef]
- Kulig, K.; Lee, S.-P.; Reischl, S.F.; Noceti-DeWit, L. Effect of posterior tibial tendon dysfunction on unipedal standing balance test. Foot Ankle Int. 2015, 36, 83–89. [Google Scholar] [CrossRef] [PubMed]
- DeOrio, J.K.; Shapiro, S.A.; McNeil, R.B.; Stansel, J. Validity of the posterior tibial edema sign in posterior tibial tendon dysfunction. Foot Ankle Int. 2011, 32, 189–192. [Google Scholar] [CrossRef]
- Nallamshetty, L.; Nazarian, L.N.; Schweitzer, M.E.; Morrison, W.B.; Parellada, J.A.; Articolo, G.A.; Rawool, N.M.; Abidi, N.A. Evaluation of posterior tibial pathology: Comparison of sonography and MR imaging. Skelet. Radiol. 2005, 34, 375–380. [Google Scholar] [CrossRef] [PubMed]
- Kohls-Gatzoulis, J.; Angel, J.; Singh, D. Tibialis posterior dysfunction as a cause of flatfeet in elderly patients. Foot 2004, 14, 207–209. [Google Scholar] [CrossRef]
- Perry, M.B.; Premkumar, A.; Venzon, D.J.; Shawker, T.H.; Gerber, L.H. Ultrasound, Magnetic Resonance Imaging, and Posterior Tibialis Dysfunction. Clin. Orthop. Relat. Res. 2003, 408, 225–231. [Google Scholar] [CrossRef]
- Lim, P.S.; Schweitzer, M.E.; Deely, D.M.; Wapner, K.L.; Hecht, P.J.; Treadwell, J.R.; Ross, M.S.; Kahn, M.D. Posterior Tibial Tendon Dysfunction: Secondary MR Signs. Foot Ankle Int. 1997, 18, 658–663. [Google Scholar] [CrossRef]
- Hintermann, B.; Gächter, A. The first metatarsal rise sign: A simple, sensitive sign of tibialis posterior tendon dysfunction. Foot Ankle Int. 1996, 17, 236–241. [Google Scholar] [CrossRef]
- Houck, J.; Neville, C.G.; Tome, J.; Flemister, A. Foot kinematics during a bilateral heel rise test in participants with stage II posterior tibial tendon dysfunction. J. Orthop. Sports Phys. Ther. 2009, 39, 593–603. [Google Scholar] [CrossRef] [PubMed]
- Hébert-Losier, K.; Wessman, C.; Alricsson, M.; Svantesson, U. Updated reliability and normative values for the standing heel-rise test in healthy adults. Physiotherapy 2017, 103, 446–452. [Google Scholar] [CrossRef] [PubMed]
- Wainwright, A.M.; Kelly, A.J.; Glew, D.; Mitchelmore, A.E.; Winson, I.G. Classification and management of tibialis posterior tendon injuries according to magnetic resonance imaging findings. Foot 1996, 6, 66–70. [Google Scholar] [CrossRef]
- Lee, S.; Oliveira, I.; Li, Y.; Welck, M.; Saifuddin, A. Fluid around the distal tibialis posterior tendon on ankle MRI: Prevalence and clinical relevance. Br. J. Radiol. 2019, 92, 20190722. [Google Scholar] [CrossRef]
- Harradine, P.; Gates, L.; Metcalf, C.; Bowen, C. Podiatrists’ views and experiences of using real time clinical gait analysis in the assessment and treatment of posterior tibial tendon dysfunction. J. Foot Ankle Res. 2021, 14, 42. [Google Scholar] [CrossRef]
- Bluman, E.M.; Myerson, M.S. Stage IV Posterior Tibial Tendon Rupture. Foot Ankle Clin. 2007, 12, 341–362. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).