Encapsulation and Delivery of Mitoxantrone Using Zirconium-Based Metal–Organic Frameworks (MOFs) and Their Cytotoxic Potential in Breast Cancer Cells
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Experimental
2.2.1. UiO-66 Synthesis
2.2.2. UiO-66-NH2 Synthesis
2.3. MTX Loading in MOFs
2.4. Characterisation
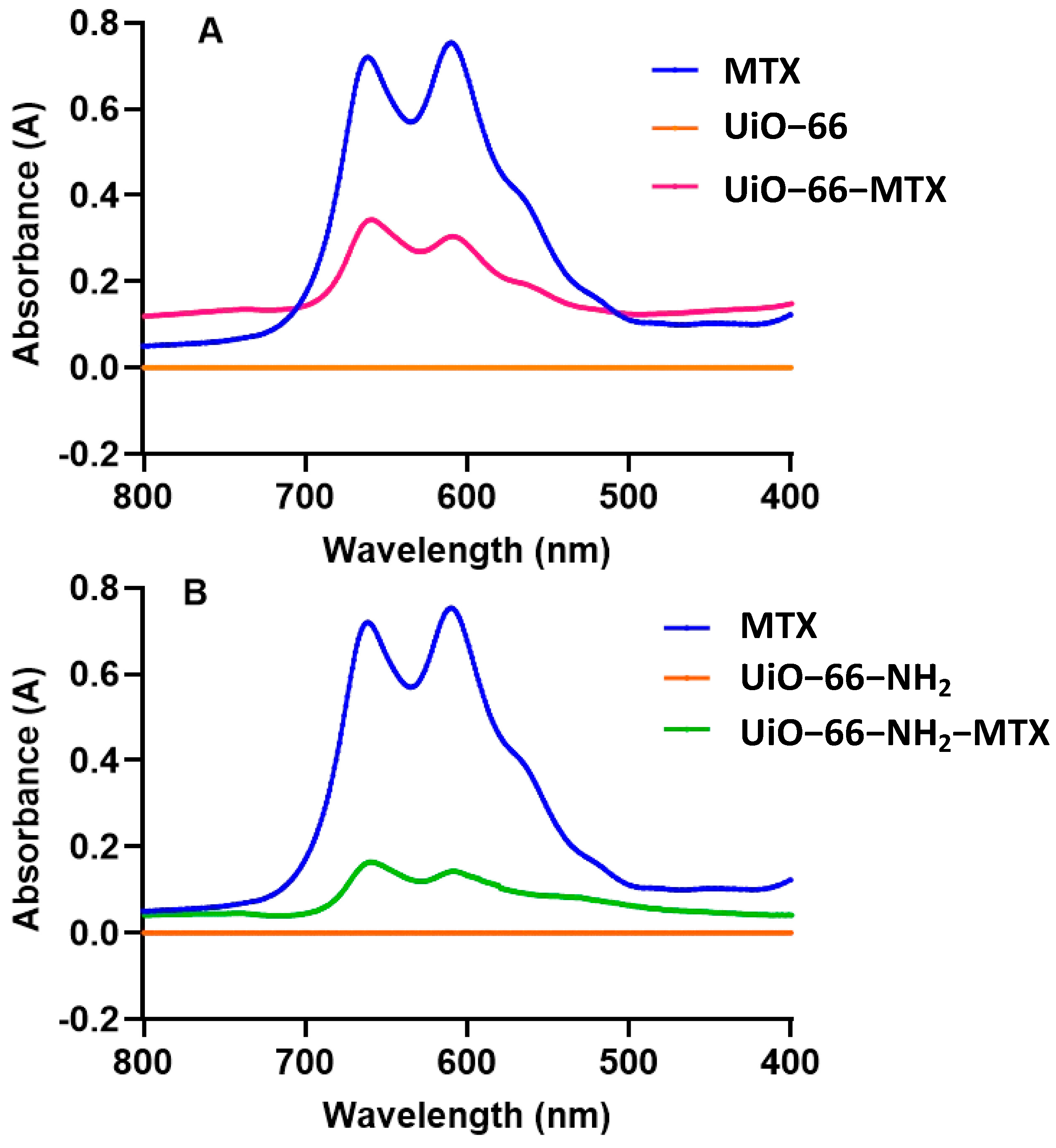
2.4.1. UV–Visible Absorption Behaviour
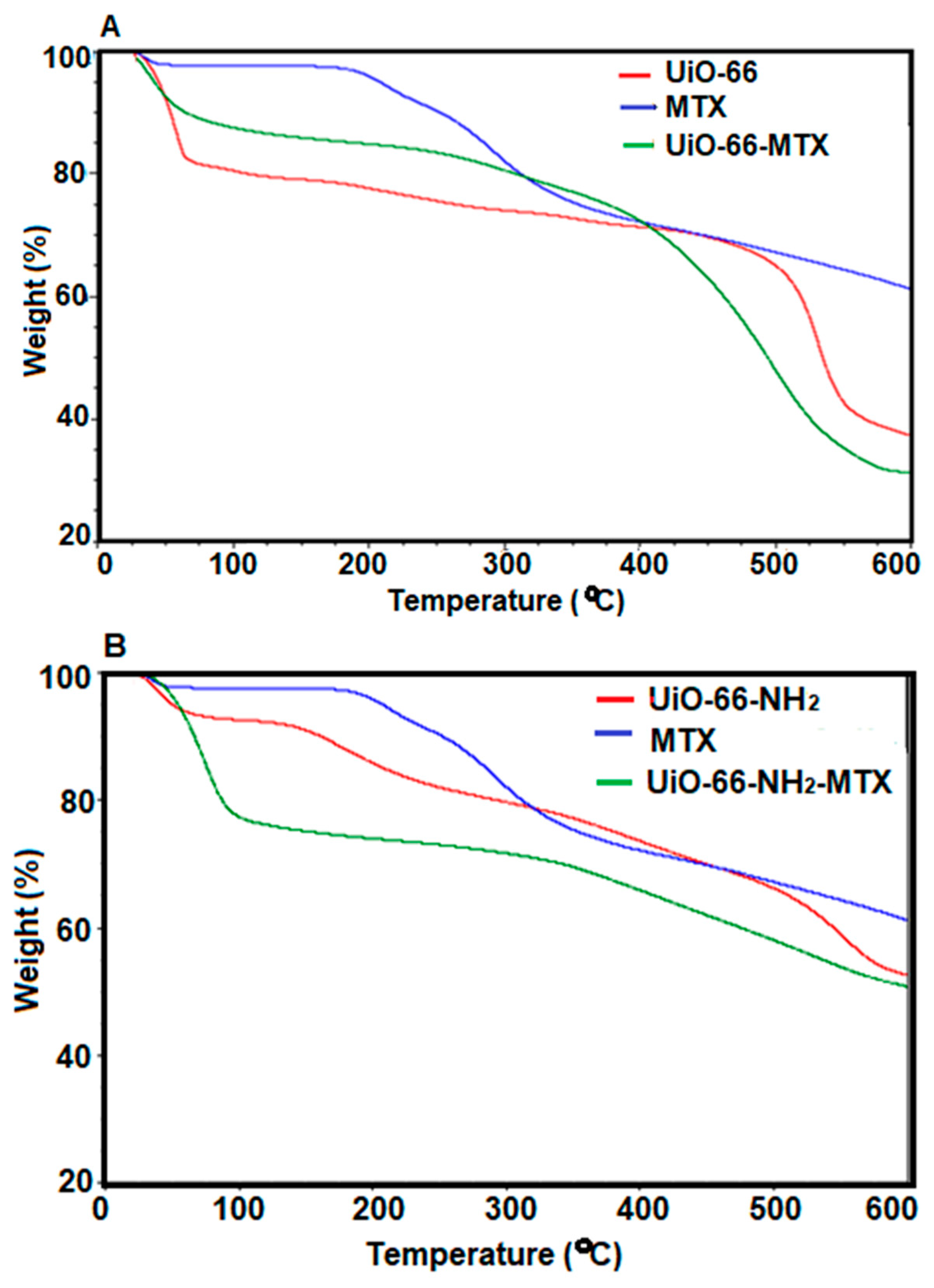
2.4.2. Thermogravimetric Analysis (TGA)
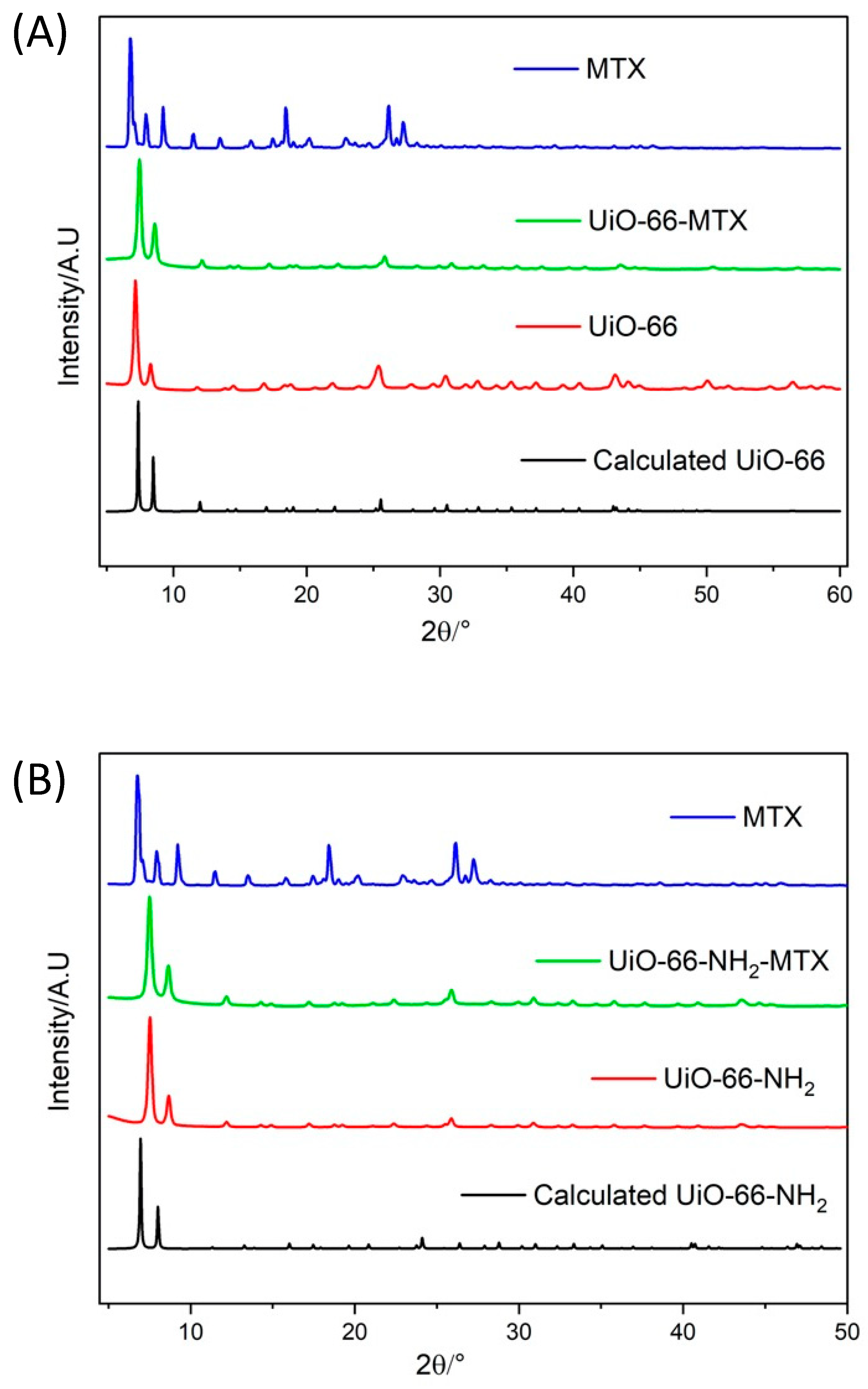
2.4.3. Powdered X-ray Diffraction (PXRD)
2.4.4. Dynamic Light Scattering (DLS)
2.4.5. Fourier Transform Infrared (FTIR) Spectrometry
2.4.6. Scanning Electron Microscopy (SEM) of Crystals
2.5. Drug Release Studies
2.6. Cell Culture
2.7. Cytotoxicity Study
2.8. Statistical Analysis
3. Results and Discussion
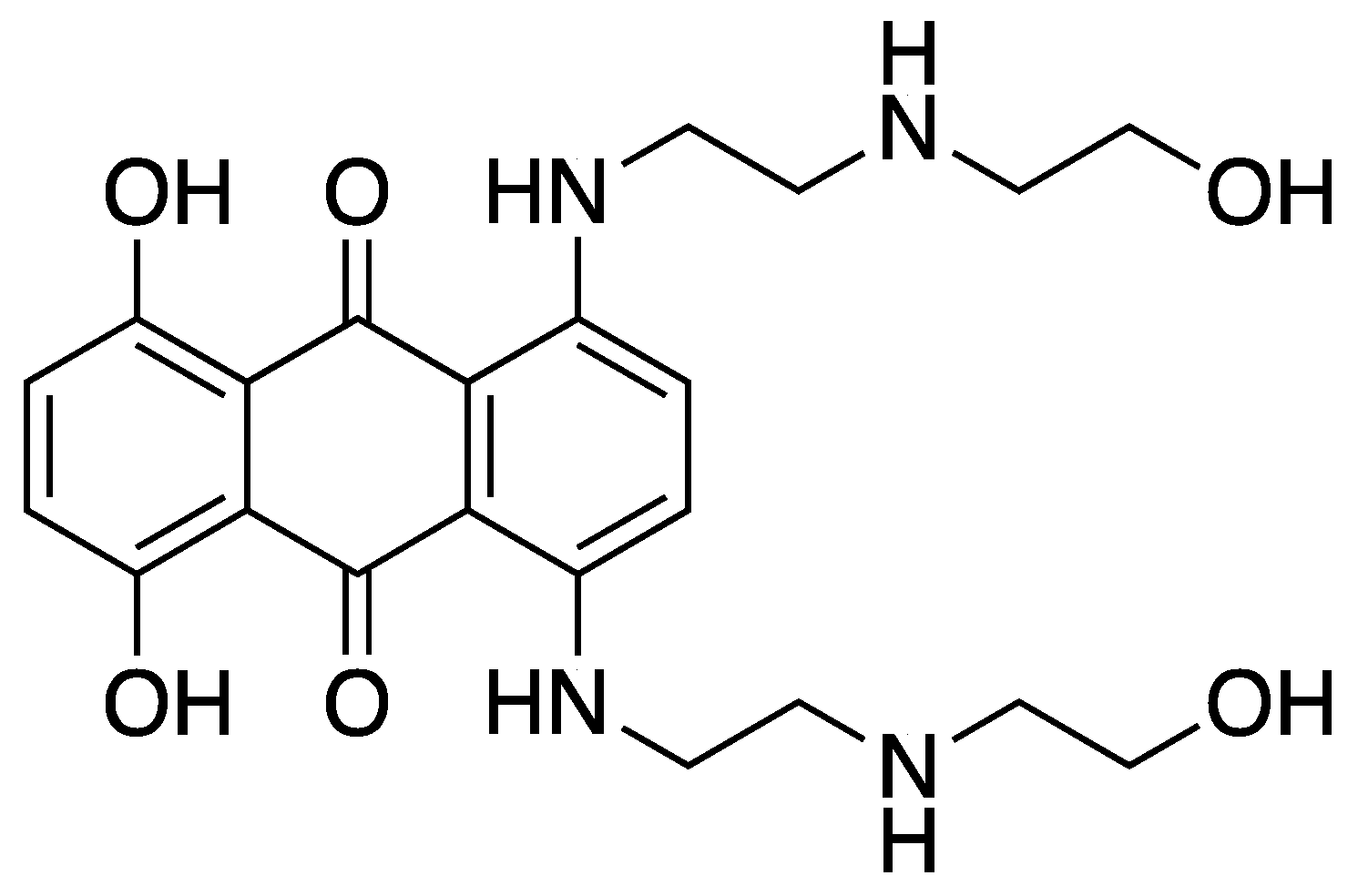
3.1. MTX Loading
3.2. Characterisation
3.2.1. TGA
3.2.2. PXRD
3.2.3. DLS
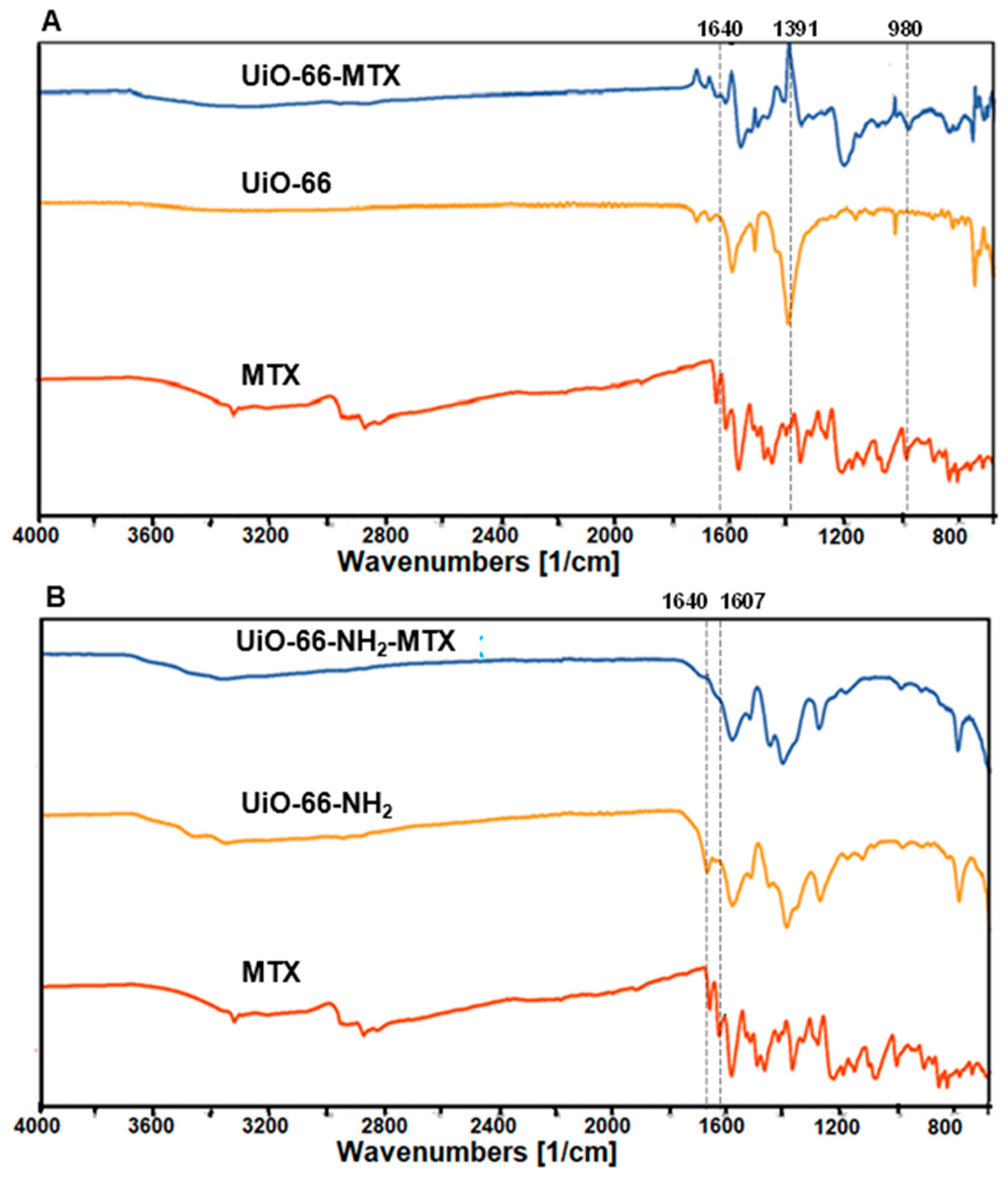
3.2.4. FTIR
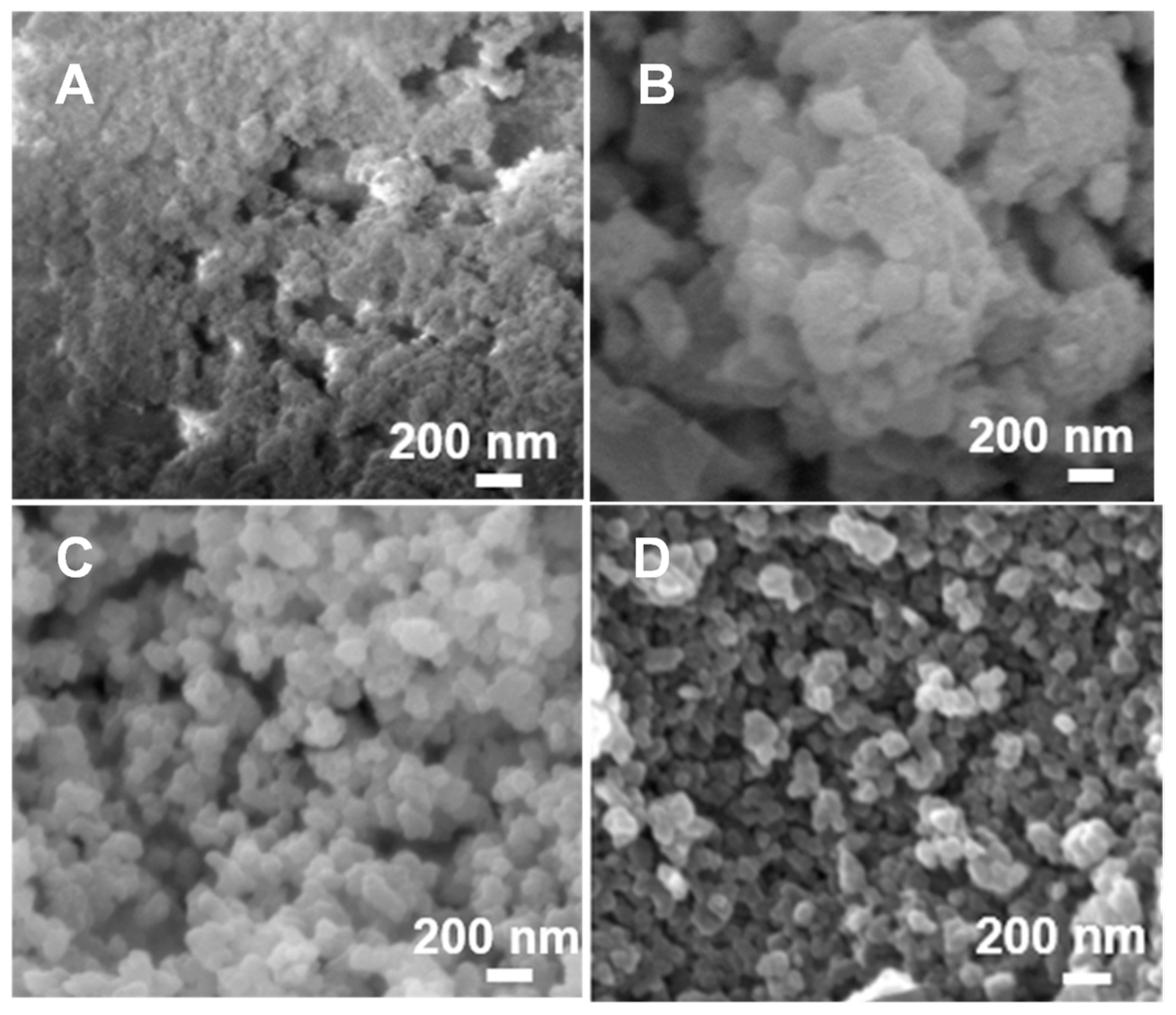
3.2.5. SEM
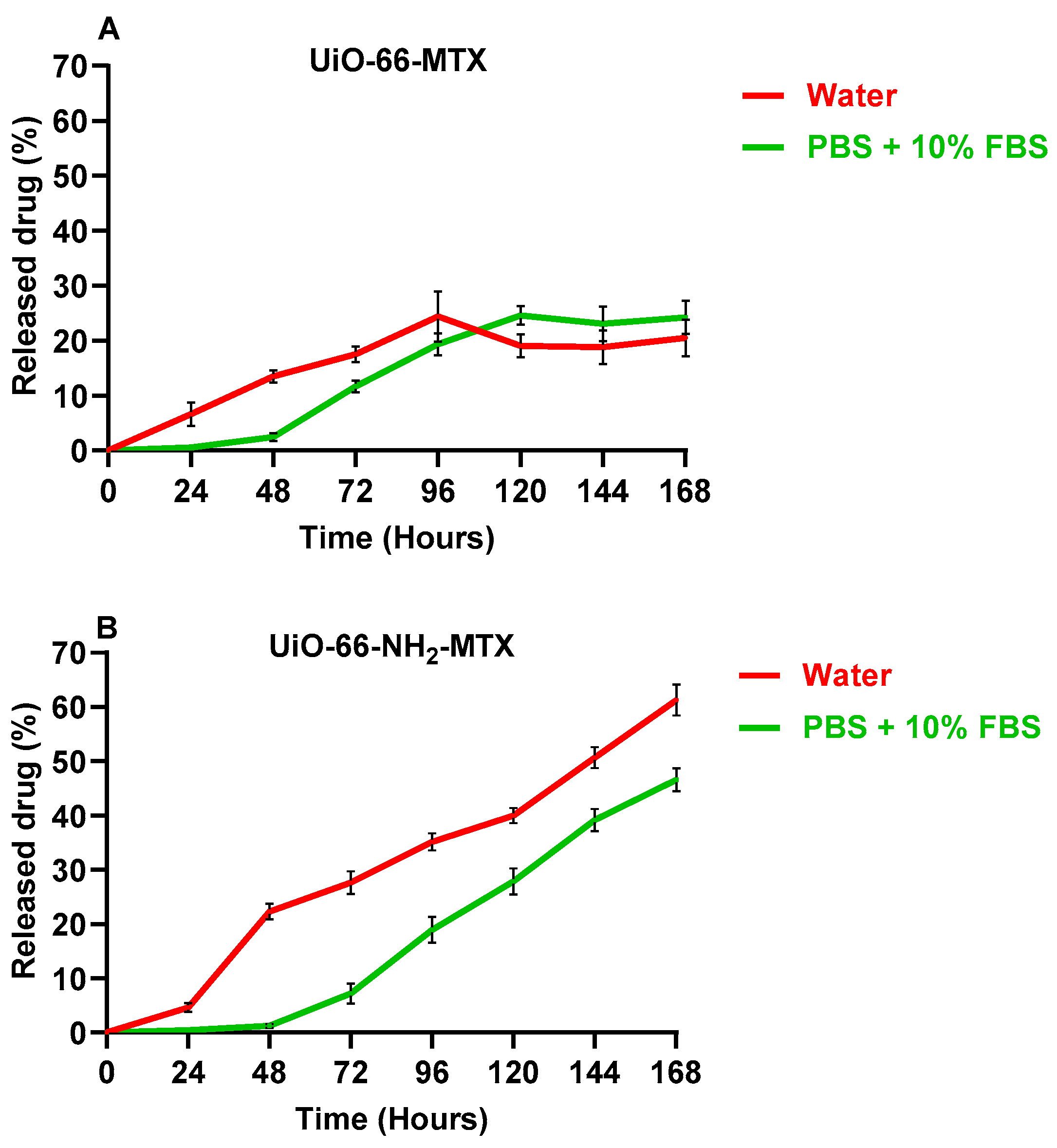
3.3. In Vitro Release Studies
3.4. Biocompatibility of the Nanocarrier
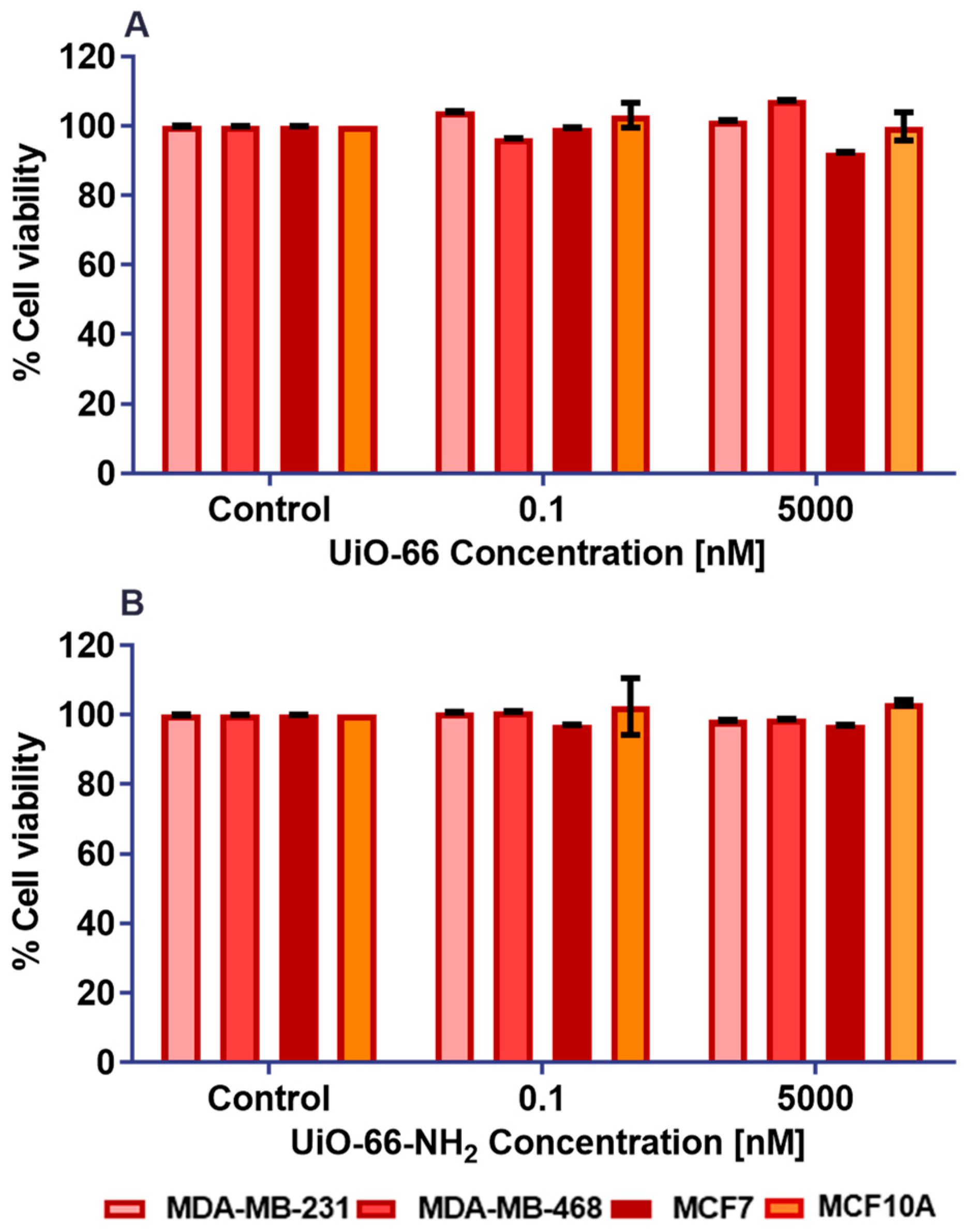
3.4.1. Chemosensitivity Assay in Monolayer Culture of Cell Lines with Pristine MOFs
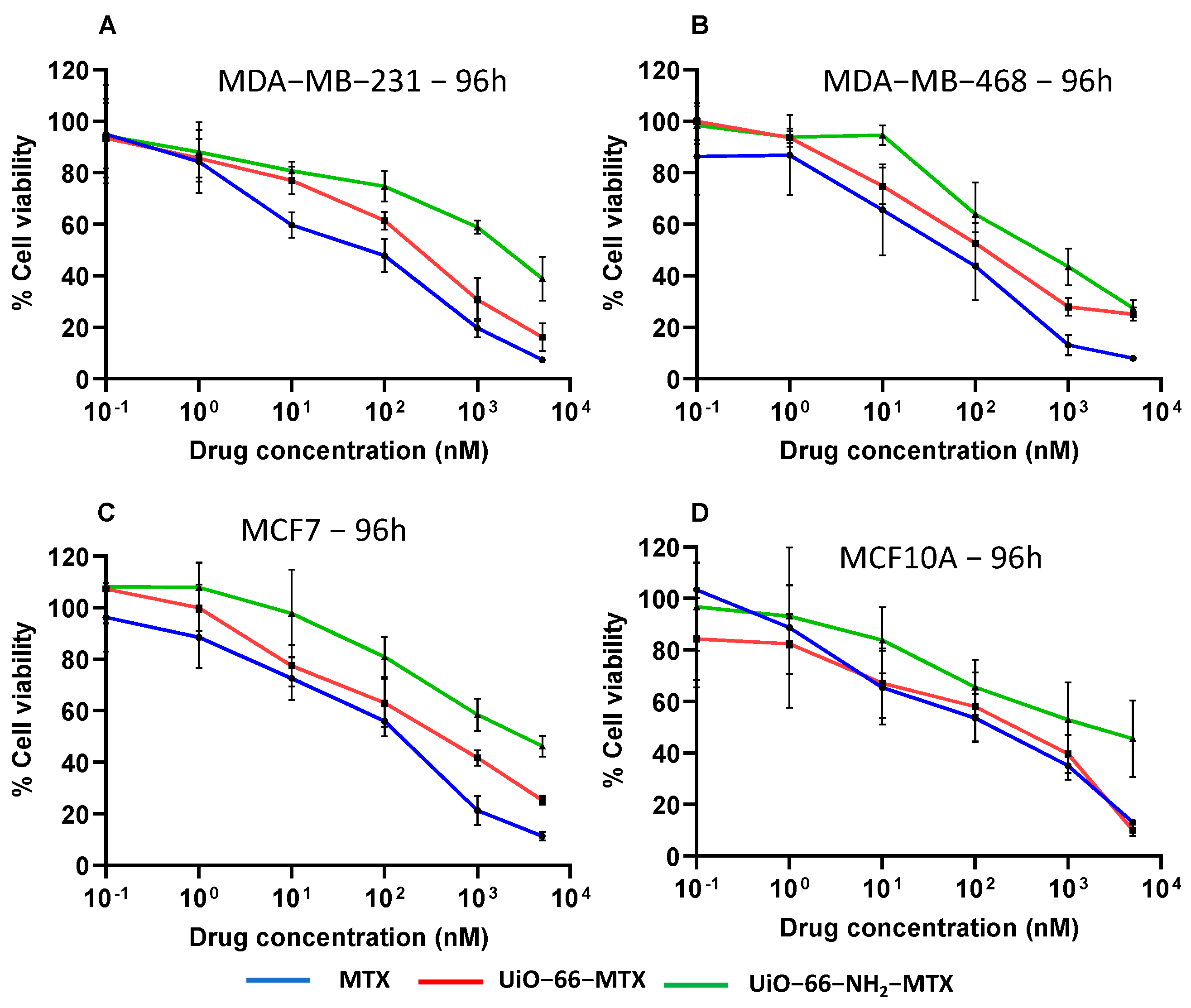
3.4.2. Cytotoxicity Assay in Monolayer Culture of Cell Lines with Free and Loaded MTX
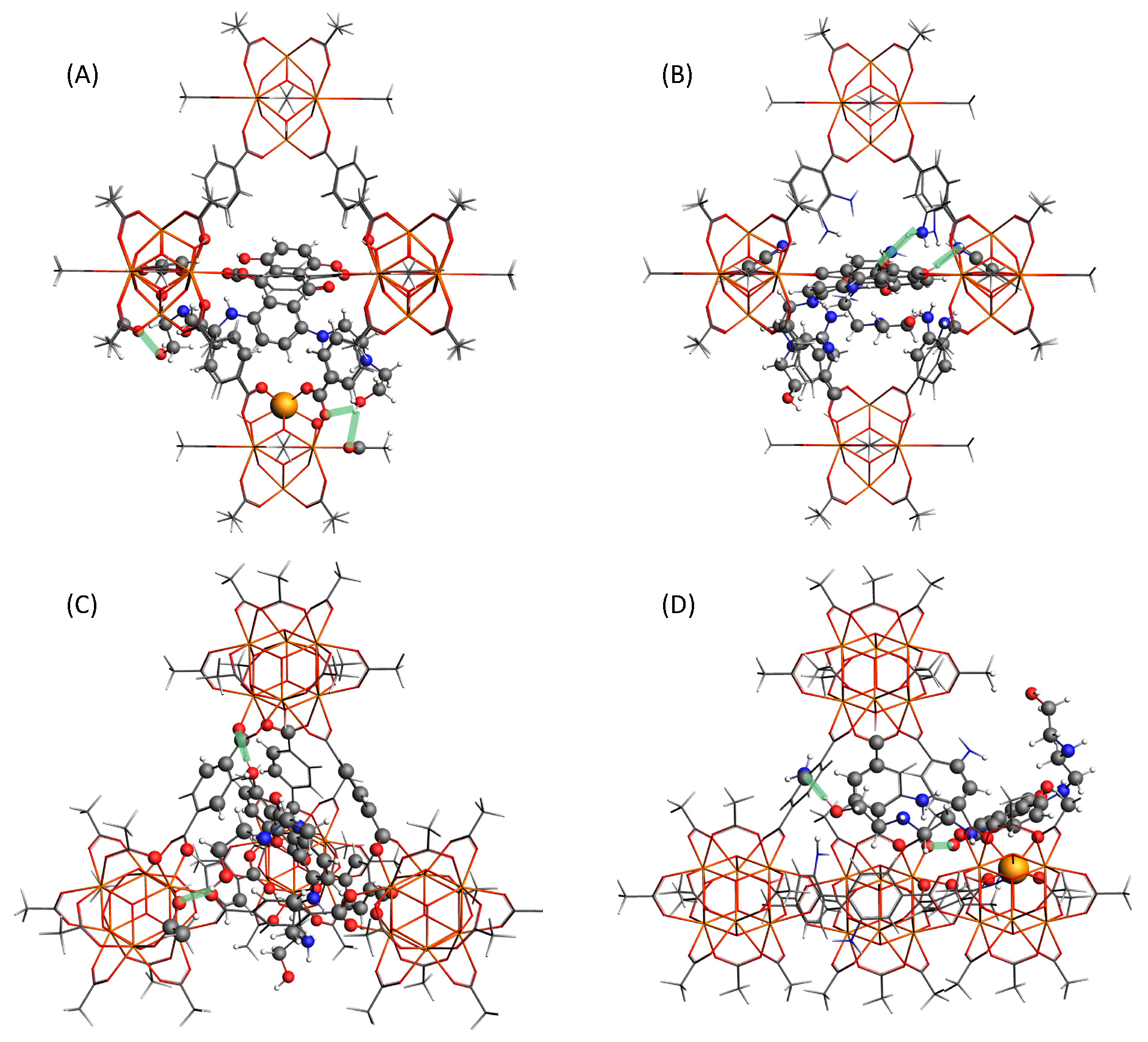
3.5. Computational Modelling
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Trushina, D.B.; Sapach, A.Y.; Burachevskaia, O.A.; Medvedev, P.V.; Khmelenin, D.N.; Borodina, T.N.; Soldatov, M.A.; Butova, V.V. Doxorubicin-Loaded Core–Shell UiO-66@SiO2 Metal–Organic Frameworks for Targeted Cellular Uptake and Cancer Treatment. Pharmaceutics 2022, 14, 1325. [Google Scholar] [CrossRef] [PubMed]
- Batten, S.R.; Champness, N.R.; Chen, X.M.; Garcia-Martinez, J.; Kitagawa, S.; Öhrström, L.; O’Keeffe, M.; Suh, M.P.; Reedijk, J. Coordination polymers, metal–organic frameworks and the need for terminology guidelines. CrystEngComm 2012, 14, 3001–3004. [Google Scholar] [CrossRef]
- Yaghi, O.M.; Li, H. Hydrothermal Synthesis of a Metal-Organic Framework Containing Large Rectangular Channels. J. Am. Chem. Soc. 1995, 117, 10401–10402. [Google Scholar] [CrossRef]
- Galarda, A.; Goscianska, J. Biocompatible Fe-Based Metal-Organic Frameworks as Diclofenac Sodium Delivery Systems for Migraine Treatment. Appl. Sci. 2023, 13, 12960. [Google Scholar] [CrossRef]
- Li, H.; Eddaoudi, M.; O’Keeffe, M.; Yaghi, O.M. Design and synthesis of an exceptionally stable and highly porous metal-organic framework. Nature 1999, 402, 276–279. [Google Scholar] [CrossRef]
- Ding, S.; Khan, A.I.; Cai, X.; Song, Y.; Lyu, Z.; Du, D.; Dutta, P.; Lin, Y. Overcoming blood–brain barrier transport: Advances in nanoparticle-based drug delivery strategies. Mater. Today 2020, 37, 112–125. [Google Scholar] [CrossRef]
- Rabiee, N.; Bagherzadeh, M.; Haris, M.H.; Ghadiri, A.M.; Moghaddam, F.M.; Fatahi, Y.; Dinarvand, R.; Jarahiyan, A.; Ahmadi, S.; Shokouhimehr, M. Polymer-Coated NH2-UiO-66 for the Codelivery of DOX/pCRISPR. ACS Appl. Mater. Interfaces 2021, 13, 10796–10811. [Google Scholar] [CrossRef]
- Allen, T.M.; Cullis, P.R. Liposomal drug delivery systems: From concept to clinical applications. Adv. Drug Deliv. Rev. 2013, 65, 36–48. [Google Scholar] [CrossRef]
- Arruebo, M. Drug delivery from structured porous inorganic materials. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2012, 4, 16–30. [Google Scholar] [CrossRef]
- Muñoz, B.; Rámila, A.; Pérez-Pariente, J.; Díaz, I.; Vallet-Regí, M. MCM-41 Organic Modification as Drug Delivery Rate Regulator. Chem. Mater. 2003, 15, 500–503. [Google Scholar] [CrossRef]
- Sun, T.; Zhang, Y.S.; Pang, B.; Hyun, D.C.; Yang, M.; Xia, Y. Engineered nanoparticles for drug delivery in cancer therapy. Angew Chem. Int. Ed. Engl. 2014, 53, 12320–12364. [Google Scholar] [CrossRef]
- Li, Y.; Lu, A.; Long, M.; Cui, L.; Chen, Z.; Zhu, L. Nitroimidazole derivative incorporated liposomes for hypoxia-triggered drug delivery and enhanced therapeutic efficacy in patient-derived tumor xenografts. Acta Biomater. 2019, 83, 334–348. [Google Scholar] [CrossRef] [PubMed]
- Bai, Y.; Liu, C.P.; Song, X.; Zhuo, L.; Bu, H.; Tian, W. Photo- and pH- Dual-Responsive β-Cyclodextrin-Based Supramolecular Prodrug Complex Self-Assemblies for Programmed Drug Delivery. Chem. Asian J. 2018, 13, 3903–3911. [Google Scholar] [CrossRef] [PubMed]
- Fytory, M.; Arafa, K.K.; El Rouby, W.M.A.; Farghali, A.A.; Abdel-Hafiez, M.; El-Sherbiny, I.M. Dual-ligated metal organic framework as novel multifunctional nanovehicle for targeted drug delivery for hepatic cancer treatment. Sci. Rep. 2021, 11, 19808. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.; Karami, A.; Sabouni, R.; Husseini, G.A.; Paul, V. pH and ultrasound dual-responsive drug delivery system based on PEG–folate-functionalized Iron-based metal–organic framework for targeted doxorubicin delivery. Colloids Surfaces A Physicochem. Eng. Asp. 2021, 626, 127062. [Google Scholar] [CrossRef]
- Freund, R.; Zaremba, O.; Arnauts, G.; Ameloot, R.; Skorupskii, G.; Dincă, M.; Bavykina, A.; Gascon, J.; Ejsmont, A.; Goscianska, J.; et al. The Current Status of MOF and COF Applications. Angew. Chem. Int. Ed. 2021, 60, 23975–24001. [Google Scholar] [CrossRef] [PubMed]
- Samanidou, V.F.; Deliyanni, E.A. Metal Organic Frameworks: Synthesis and Application. Molecules 2020, 25, 960. [Google Scholar] [CrossRef]
- Yadav, P.; Kumari, S.; Yadav, A.; Bhardwaj, P.; Maruthi, M.; Chakraborty, A.; Kanoo, P. Biocompatible Drug Delivery System Based on a MOF Platform for a Sustained and Controlled Release of the Poorly Soluble Drug Norfloxacin. ACS Omega 2023, 8, 28367–28375. [Google Scholar] [CrossRef]
- Xue, J.; Liu, J.; Yong, J.; Liang, K. Biomedical Applications of Metal–Organic Frameworks at the Subcellular Level. Adv. NanoBiomed Res. 2021, 1, 2100034. [Google Scholar] [CrossRef]
- DeCoste, J.B.; Peterson, G.W.; Jasuja, H.; Glover, T.G.; Huang, Y.-G.; Walton, K.S. Stability and degradation mechanisms of metal–organic frameworks containing the Zr6O4(OH)4 secondary building unit. J. Mater. Chem. A 2013, 1, 5642–5650. [Google Scholar] [CrossRef]
- Zhang, C.; Xin, L.; Li, J.; Cao, J.; Sun, Y.; Wang, X.; Luo, J.; Zeng, Y.; Li, Q.; Zhang, Y.; et al. Metal–Organic Framework (MOF)-Based Ultrasound-Responsive Dual-Sonosensitizer Nanoplatform for Hypoxic Cancer Therapy. Adv. Healthc. Mater. 2022, 11, 2101946. [Google Scholar] [CrossRef] [PubMed]
- Dijkers, E.C.; Kosterink, J.G.; Rademaker, A.P.; Perk, L.R.; van Dongen, G.A.; Bart, J.; de Jong, J.R.; de Vries, E.G.; Lub-de Hooge, M.N. Development and characterization of clinical-grade 89Zr-trastuzumab for HER2/neu immunoPET imaging. J. Nucl. Med. 2009, 50, 974–981. [Google Scholar] [CrossRef] [PubMed]
- Tinianow, J.N.; Gill, H.S.; Ogasawara, A.; Flores, J.E.; Vanderbilt, A.N.; Luis, E.; Vandlen, R.; Darwish, M.; Junutula, J.R.; Williams, S.-P.; et al. Site-specifically 89Zr-labeled monoclonal antibodies for ImmunoPET. Nucl. Med. Biol. 2010, 37, 289–297. [Google Scholar] [CrossRef] [PubMed]
- Dijkers, E.C.; Oude Munnink, T.H.; Kosterink, J.G.; Brouwers, A.H.; Jager, P.L.; De Jong, J.R.; Van Dongen, G.A.; Schroder, C.P.; Lub-de Hooge, M.N.; de Vries, E.G. Biodistribution of 89Zr-trastuzumab and PET Imaging of HER2-Positive Lesions in Patients With Metastatic Breast Cancer. Clin. Pharmacol. Ther. 2010, 87, 586–592. [Google Scholar] [CrossRef]
- Liu, W.; Wang, Y.-M.; Li, Y.-H.; Cai, S.-J.; Yin, X.-B.; He, X.-W.; Zhang, Y.-K. Fluorescent Imaging-Guided Chemotherapy-and-Photodynamic Dual Therapy with Nanoscale Porphyrin Metal-Organic Framework. Small 2017, 13, 1603459. [Google Scholar] [CrossRef]
- Cavka, J.H.; Jakobsen, S.; Olsbye, U.; Guillou, N.; Lamberti, C.; Bordiga, S.; Lillerud, K.P. A New Zirconium Inorganic Building Brick Forming Metal Organic Frameworks with Exceptional Stability. J. Am. Chem. Soc. 2008, 130, 13850–13851. [Google Scholar] [CrossRef] [PubMed]
- DeStefano, M.R.; Islamoglu, T.; Garibay, S.J.; Hupp, J.T.; Farha, O.K. Room-Temperature Synthesis of UiO-66 and Thermal Modulation of Densities of Defect Sites. Chem. Mater. 2017, 29, 1357–1361. [Google Scholar] [CrossRef]
- Wu, H.; Yildirim, T.; Zhou, W. Exceptional Mechanical Stability of Highly Porous Zirconium Metal–Organic Framework UiO-66 and Its Important Implications. J. Phys. Chem. Lett. 2013, 4, 925–930. [Google Scholar] [CrossRef]
- Ibrahim, A.H.; El-Mehalmey, W.A.; Haikal, R.R.; Safy, M.E.A.; Amin, M.; Shatla, H.R.; Karakalos, S.G.; Alkordi, M.H. Tuning the Chemical Environment within the UiO-66-NH2 Nanocages for Charge-Dependent Contaminant Uptake and Selectivity. Inorg. Chem. 2019, 58, 15078–15087. [Google Scholar] [CrossRef]
- Mocniak, K.A.; Kubajewska, I.; Spillane, D.E.M.; Williams, G.R.; Morris, R.E. Incorporation of cisplatin into the metal–organic frameworks UiO66-NH2 and UiO66—Encapsulation vs. conjugation. RSC Adv. 2015, 5, 83648–83656. [Google Scholar] [CrossRef]
- Bazzazan, S.; Moeinabadi-Bidgoli, K.; Lalami, Z.A.; Bazzazan, S.; Mehrarya, M.; Yeganeh, F.E.; Hejabi, F.; Akbarzadeh, I.; Noorbazargan, H.; Jahanbakhshi, M.; et al. Engineered UIO-66 metal-organic framework for delivery of curcumin against breast cancer cells: An in vitro evaluation. J. Drug Deliv. Sci. Technol. 2023, 79, 104009. [Google Scholar] [CrossRef]
- Gholami, M.; Hekmat, A.; Khazaei, M.; Darroudi, M. OXA-CuS@UiO-66-NH2 as a drug delivery system for Oxaliplatin to colorectal cancer cells. J. Mater.Sci. Mater. Med. 2022, 33, 26. [Google Scholar] [CrossRef] [PubMed]
- Henderson, I.C.; Allegra, J.C.; Woodcock, T.; Wolff, S.; Bryan, S.; Cartwright, K.; Dukart, G.; Henry, D. Randomized clinical trial comparing mitoxantrone with doxorubicin in previously treated patients with metastatic breast cancer. J. Clin. Oncol. 1989, 7, 560–571. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Cao, J.; Li, C.; Wang, X.; Zhao, Y.; Li, T.; Du, Y.; Tao, Z.; Peng, W.; Wang, B.; et al. Efficacy and safety of mitoxantrone hydrochloride liposome injection in Chinese patients with advanced breast cancer: A randomized, open-label, active-controlled, single-center, phase II clinical trial. Investig. New Drugs 2022, 40, 330–339. [Google Scholar] [CrossRef] [PubMed]
- Brück, T.B.; Brück, D.W. Oxidative metabolism of the anti-cancer agent mitoxantrone by horseradish, lacto-and lignin peroxidase. Biochimie 2011, 93, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Seiter, K. Toxicity of the topoisomerase II inhibitors. Expert Opin. Drug Saf. 2005, 4, 219–234. [Google Scholar] [CrossRef]
- Lian, X.; Zhang, Y.; Wang, J.; Yan, B. Antineoplastic Mitoxantrone Monitor: A Sandwiched Mixed Matrix Membrane (MMM) Based on a Luminescent MOF–Hydrogel Hybrid. Inorg. Chem. 2020, 59, 10304–10310. [Google Scholar] [CrossRef]
- Wang, J.; Gao, R.; Li, Q.; Xie, S.; Zhao, J.; Wang, C. Synthesis, Cytotoxicity, and Cell Death Profile of Polyaminoanthraquinones as Antitumor Agents. Chem. Biol. Drug Des. 2012, 80, 909–917. [Google Scholar] [CrossRef]
- Seifrtova, M.; Havelek, R.; Chmelarova, M.; Cmielova, J.; Muthna, D.; Stoklasova, A.; Zemankova, S.; Rezacova, M. The effect of ATM and ERK1/2 inhibition on mitoxantrone-induced cell death of leukaemic cells. Folia Biol. Praha 2011, 57, 74–81. [Google Scholar] [PubMed]
- Huang, S.; Yuan, J.; Xie, Y.; Qing, K.; Shi, Z.; Chen, G.; Gao, J.; Tan, H.; Zhou, W. Targeting nano-regulator based on metal–organic frameworks for enhanced immunotherapy of bone metastatic prostate cancer. Cancer Nanotechnol. 2023, 14, 43. [Google Scholar] [CrossRef]
- Bhunia, S.; Saha, P.; Moitra, P.; Addicoat, M.A.; Bhattacharya, S. Efficacious and sustained release of an anticancer drug mitoxantrone from new covalent organic frameworks using protein corona. Chem. Sci. 2022, 13, 7920–7932. [Google Scholar] [CrossRef]
- Li, Z.; Liu, J.; Hu, Y.; Howard, K.A.; Li, Z.; Fan, X.; Chang, M.; Sun, Y.; Besenbacher, F.; Chen, C.; et al. Multimodal Imaging-Guided Antitumor Photothermal Therapy and Drug Delivery Using Bismuth Selenide Spherical Sponge. ACS Nano 2016, 10, 9646–9658. [Google Scholar] [CrossRef]
- Moitra, P.; Kumar, K.; Sarkar, S.; Kondaiah, P.; Duan, W.; Bhattacharya, S. New pH-responsive gemini lipid derived co-liposomes for efficacious doxorubicin delivery to drug resistant cancer cells. Chem. Commun. 2017, 53, 8184–8187. [Google Scholar] [CrossRef] [PubMed]
- Rojas, S.; Carmona, F.J.; Maldonado, C.R.; Horcajada, P.; Hidalgo, T.; Serre, C.; Navarro, J.A.R.; Barea, E. Nanoscaled Zinc Pyrazolate Metal–Organic Frameworks as Drug-Delivery Systems. Inorg. Chem. 2016, 55, 2650–2663. [Google Scholar] [CrossRef]
- Taddei, M.; Dümbgen, K.C.; van Bokhoven, J.A.; Ranocchiari, M. Aging of the reaction mixture as a tool to modulate the crystallite size of UiO-66 into the low nanometer range. Chem. Commun. 2016, 52, 6411–6414. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Zhang, H.; Song, F.; Huang, T.; Ji, J.; Zhong, Q.; Chu, W.; Xu, Q. UiO-66-NH2/GO Composite: Synthesis, Characterization and CO2 Adsorption Performance. Materials 2018, 11, 589. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.S.; Dutta, P.K. Optical spectroscopic studies of the antitumor drug 1,4-dihydroxy-5,8-bis[[2-[(2-hydroxyethyl)amino]ethyl]amino]-9,10-anthracenedione(mitoxantrone). J. Phys. Chem. 1989, 93, 5665–5672. [Google Scholar] [CrossRef]
- Wan, C.; Guo, X.; Song, F.; Liu, Z.; Liu, S. Interactions of mitoxantrone with duplex and triplex DNA studied by electrospray ionization mass spectrometry. Rapid Commun. Mass Spectrom. 2008, 22, 4043–4048. [Google Scholar] [CrossRef]
- Valenzano, L.; Civalleri, B.; Chavan, S.; Bordiga, S.; Nilsen, M.H.; Jakobsen, S.; Lillerud, K.P.; Lamberti, C. Disclosing the Complex Structure of UiO-66 Metal Organic Framework: A Synergic Combination of Experiment and Theory. Chem. Mater. 2011, 23, 1700–1718. [Google Scholar] [CrossRef]
- Merli, D.; Pivi, F.; Profumo, A.; Quadrelli, P.; Milanese, C.; Risi, G.; Visai, L. Carboxymethylinulin–Chitosan Nanoparticles for the Delivery of Antineoplastic Mitoxantrone. ChemMedChem 2016, 11, 2436–2444. [Google Scholar] [CrossRef]
- Nik, O.G.; Chen, X.Y.; Kaliaguine, S. Functionalized metal organic framework-polyimide mixed matrix membranes for CO2/CH4 separation. J. Membr. Sci. 2012, 413–414, 48–61. [Google Scholar] [CrossRef]
- Huang, Y.; Qin, W.; Li, Z.; Li, Y. Enhanced stability and CO2 affinity of a UiO-66 type metal–organic framework decorated with dimethyl groups. Dalton Trans. 2012, 41, 9283–9285. [Google Scholar] [CrossRef]
- Chavan, S.; Vitillo, J.G.; Gianolio, D.; Zavorotynska, O.; Civalleri, B.; Jakobsen, S.; Nilsen, M.H.; Valenzano, L.; Lamberti, C.; Lillerud, K.P.; et al. H2storage in isostructural UiO-67 and UiO-66 MOFs. Phys. Chem. Chem. Phys. 2012, 14, 1614–1626. [Google Scholar] [CrossRef]
- Pirzadeh, K.; Esfandiari, K.; Ghoreyshi, A.A.; Rahimnejad, M. CO2 and N2 adsorption and separation using aminated UiO-66 and Cu3(BTC)2: A comparative study. Korean J. Chem. Eng. 2020, 37, 513–524. [Google Scholar] [CrossRef]
- Rodrigues, M.O.; de Paula, M.V.; Wanderley, K.A.; Vasconcelos, I.B.; Alves, S., Jr.; Soares, T.A. Metal organic frameworks for drug delivery and environmental remediation: A molecular docking approach. Int. J. Quantum Chem. 2012, 112, 3346–3355. [Google Scholar] [CrossRef]
- Cao, Y.; Zhao, Y.; Lv, Z.; Song, F.; Zhong, Q. Preparation and enhanced CO2 adsorption capacity of UiO-66/graphene oxide composites. J. Ind. Eng. Chem. 2015, 27, 102–107. [Google Scholar] [CrossRef]
- Vermoortele, F.; Ameloot, R.; Vimont, A.; Serre, C.; De Vos, D. An amino-modified Zr-terephthalate metal–organic framework as an acid–base catalyst for cross-aldol condensation. Chem. Commun. 2011, 47, 1521–1523. [Google Scholar] [CrossRef] [PubMed]
- Carson, C.G.; Hardcastle, K.; Schwartz, J.; Liu, X.; Hoffmann, C.; Gerhardt, R.A.; Tannenbaum, R. Synthesis and Structure Characterization of Copper Terephthalate Metal–Organic Frameworks. Eur. J. Inorg. Chem. 2009, 2009, 2338–2343. [Google Scholar] [CrossRef]
- Chowdhuri, A.R.; Laha, D.; Chandra, S.; Karmakar, P.; Sahu, S.K. Synthesis of multifunctional upconversion NMOFs for targeted antitumor drug delivery and imaging in triple negative breast cancer cells. Chem. Eng. J. 2017, 319, 200–211. [Google Scholar] [CrossRef]
- Jarai, B.M.; Stillman, Z.; Attia, L.; Decker, G.E.; Bloch, E.D.; Fromen, C.A. Evaluating UiO-66 Metal–Organic Framework Nanoparticles as Acid-Sensitive Carriers for Pulmonary Drug Delivery Applications. ACS Appl. Mater. Interfaces 2020, 12, 38989–39004. [Google Scholar] [CrossRef]
- Lázaro, I.A.; Haddad, S.; Sacca, S.; Orellana-Tavra, C.; Fairen-Jimenez, D.; Forgan, R.S. Selective Surface PEGylation of UiO-66 Nanoparticles for Enhanced Stability, Cell Uptake, and pH-Responsive Drug Delivery. Chem 2017, 2, 561–578. [Google Scholar] [CrossRef] [PubMed]
- Bůžek, D.; Adamec, S.; Lang, K.; Demel, J. Metal–organic frameworks vs. buffers: Case study of UiO-66 stability. Inorg. Chem. Front. 2021, 8, 720–734. [Google Scholar] [CrossRef]
- Al Neyadi, S.S.; Al Blooshi, A.G.; Nguyen, H.L.; Alnaqbi, M.A. UiO-66-NH2 as an effective solid support for quinazoline derivatives for antibacterial agents against Gram-negative bacteria. New J. Chem. 2021, 45, 20386–20395. [Google Scholar] [CrossRef]
- Docter, D.; Westmeier, D.; Markiewicz, M.; Stolte, S.; Knauer, S.K.; Stauber, R.H. The nanoparticle biomolecule corona: Lessons learned–challenge accepted? Chem. Soc. Rev. 2015, 44, 6094–6121. [Google Scholar] [CrossRef] [PubMed]
- Rampado, R.; Crotti, S.; Caliceti, P.; Pucciarelli, S.; Agostini, M. Recent Advances in Understanding the Protein Corona of Nanoparticles and in the Formulation of “Stealthy” Nanomaterials. Front. Bioeng. Biotechnol. 2020, 8, 166. [Google Scholar] [CrossRef] [PubMed]
- Westmeier, D.; Stauber, R.H.; Docter, D. The concept of bio-corona in modulating the toxicity of engineered nanomaterials (ENM). Toxicol. Appl. Pharmacol. 2016, 299, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Liang, Z.; Yang, Z.; Yuan, H.; Wang, C.; Qi, J.; Liu, K.; Cao, R.; Zheng, H. A Protein@Metal−Organic Framework Nanocomposite for pH-Triggered Anticancer Drug Delivery. Dalton Trans. 2018, 47, 10223–10228. [Google Scholar] [CrossRef] [PubMed]
- Al-Jouhani, S.; Al-Azwari, R.; Al-Shemari, S.; Al-Anezi, R.; Khasim, S.; Mohamed, S.; Al-Ghamdi, S.A.; Darwish, A.A.; Hamdalla, T.A. The effect of human serum albumin on ZIF-8 used in drug delivery: Structural, linear and nonlinear optical properties. J. Umm Al-Qura Univ. Appl. Sci. 2023, 9, 521–528. [Google Scholar] [CrossRef]
- Vibet, S.; Mahéo, K.; Goré, J.; Dubois, P.; Bougnoux, P.; Chourpa, I. Differential Subcellular Distribution of Mitoxantrone in Relation to Chemosensitization in Two Human Breast Cancer Cell Lines. Drug Metab. Dispos. 2007, 35, 822–828. [Google Scholar] [CrossRef]
- Carlisi, D.; De Blasio, A.; Drago-Ferrante, R.; Di Fiore, R.; Buttitta, G.; Morreale, M.; Scerri, C.; Vento, R.; Tesoriere, G. Parthenolide prevents resistance of MDA-MB231 cells to doxorubicin and mitoxantrone: The role of Nrf2. Cell Death Discov. 2017, 3, 17078. [Google Scholar] [CrossRef]
- Greijer, A.E.; de Jong, M.C.; Scheffer, G.L.; Shvarts, A.; van Diest, P.J.; van der Wall, E. Hypoxia-Induced Acidification Causes Mitoxantrone Resistance Not Mediated by Drug Transporters in Human Breast Cancer Cells. Anal. Cell. Pathol. 2005, 27, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Tao, X.; Tao, T.; Wen, Y.; Yi, J.; He, L.; Huang, Z.; Nie, Y.; Yao, X.; Wang, Y.; He, C.; et al. Novel Delivery of Mitoxantrone with Hydrophobically Modified Pullulan Nanoparticles to Inhibit Bladder Cancer Cell and the Effect of Nano-drug Size on Inhibition Efficiency. Nanoscale Res. Lett. 2018, 13, 345. [Google Scholar] [CrossRef] [PubMed]
| Weight Ratio MOF:MTX [mg:mg] | UiO-66-LC% | UiO-66-NH2-LC% |
|---|---|---|
| 1:1 | 40.7 ± 1.4 | 8 ± 1.3 |
| 2:1 | 29.6 ± 1.0 | 8 ± 1.7 |
| 4:1 | 15.8 ± 0.3 | 21.41 ± 0.1 |
| MOFs | Size (nm) | PdI | Zeta Potential (mV) |
|---|---|---|---|
| UiO-66 | 156 ± 0.4 | 0.279 | 26.7 ± 2.23 |
| UiO-66-MTX | 211 ± 8 | 0.42 | 19.8 ± 0.94 |
| UiO-66-NH2 | 170 ± 2.3 | 0.212 | 30.8 ± 0.81 |
| UiO-66-NH2-MTX | 487 ± 3 | 0.179 | 14.1 ± 0.66 |
| Cell Lines | IC50 (nM) | ||
|---|---|---|---|
| MTX | UiO-66-MTX | UiO-66-NH2-MTX | |
| MDA-MB-231 | 29 ± 0.13 | 103 ± 0.25 | 1069 ± 0.35 |
| MDA-MB-468 | 28 ± 0.15 | 113 ± 0.09 | 425 ± 0.21 |
| MCF7 | 75 ± 0.21 | 203 ± 0.14 | 1632 ± 0.24 |
| MCF10A | 67 ± 0.10 | 73 ± 0.36 | 1129 ± 0.12 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Singhal, M.; Riches-Suman, K.; Pors, K.; Addicoat, M.A.; Ruiz, A.; Nayak, S.; Elies, J. Encapsulation and Delivery of Mitoxantrone Using Zirconium-Based Metal–Organic Frameworks (MOFs) and Their Cytotoxic Potential in Breast Cancer Cells. Appl. Sci. 2024, 14, 1902. https://doi.org/10.3390/app14051902
Singhal M, Riches-Suman K, Pors K, Addicoat MA, Ruiz A, Nayak S, Elies J. Encapsulation and Delivery of Mitoxantrone Using Zirconium-Based Metal–Organic Frameworks (MOFs) and Their Cytotoxic Potential in Breast Cancer Cells. Applied Sciences. 2024; 14(5):1902. https://doi.org/10.3390/app14051902
Chicago/Turabian StyleSinghal, Mitali, Kirsten Riches-Suman, Klaus Pors, Matthew A. Addicoat, Amalia Ruiz, Sanjit Nayak, and Jacobo Elies. 2024. "Encapsulation and Delivery of Mitoxantrone Using Zirconium-Based Metal–Organic Frameworks (MOFs) and Their Cytotoxic Potential in Breast Cancer Cells" Applied Sciences 14, no. 5: 1902. https://doi.org/10.3390/app14051902
APA StyleSinghal, M., Riches-Suman, K., Pors, K., Addicoat, M. A., Ruiz, A., Nayak, S., & Elies, J. (2024). Encapsulation and Delivery of Mitoxantrone Using Zirconium-Based Metal–Organic Frameworks (MOFs) and Their Cytotoxic Potential in Breast Cancer Cells. Applied Sciences, 14(5), 1902. https://doi.org/10.3390/app14051902









