The Effect of Silver Nanoparticles on Bond Strength of Calcium Silicate-Based Sealer: An In Vitro Study
Abstract
1. Introduction
2. Material and Methods
2.1. Characterization of AgNPs
2.2. Specimen Preparation
2.3. Experimental Design
2.4. Push-Out Bond Strength Assessment
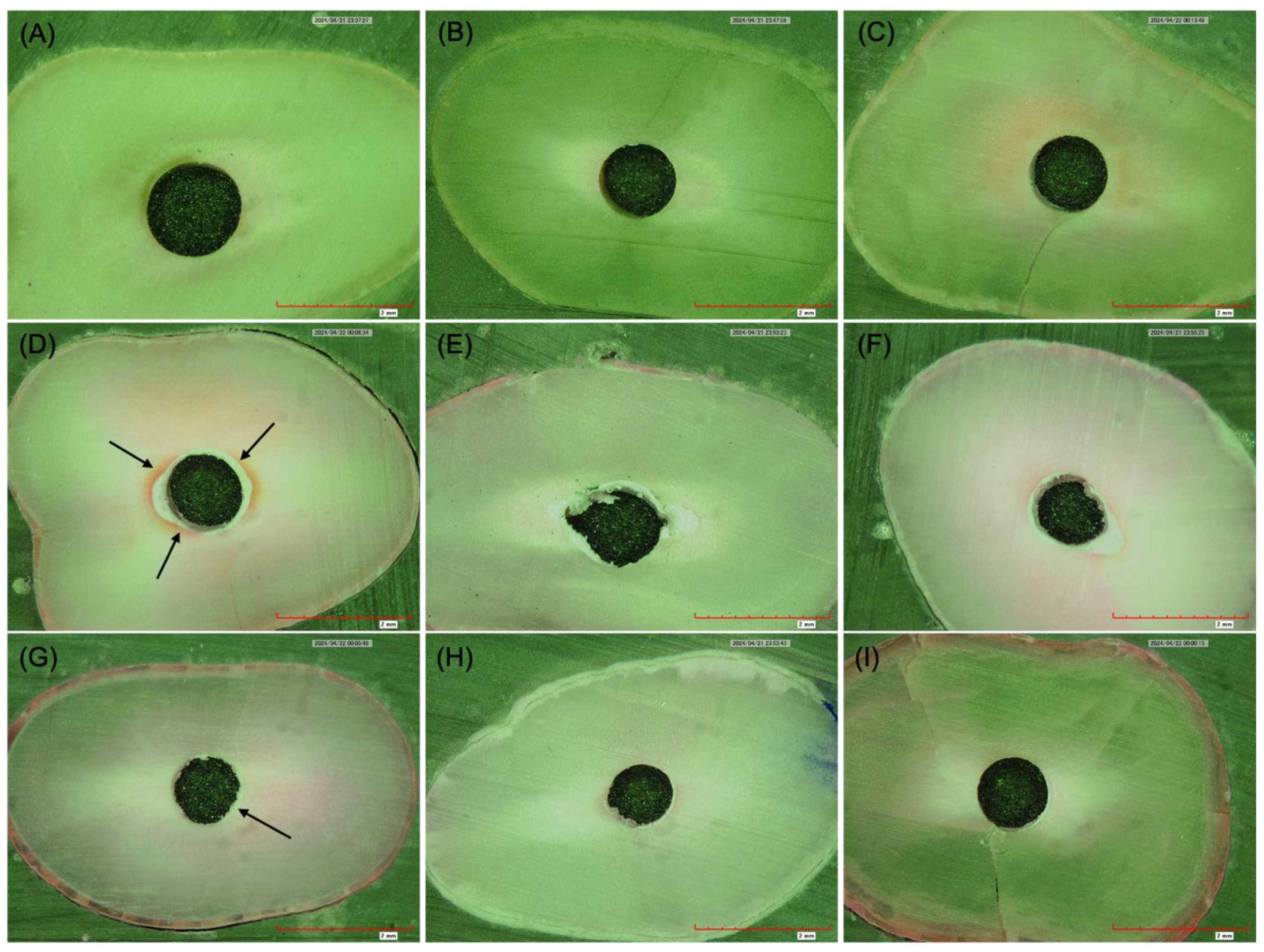
2.5. Failure Modes Assessment
2.6. Statistical Analysis
3. Results
3.1. Characterization of AgNPs
3.2. Push-Out Bond Strength Assessment
3.3. Failure Modes Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Madison, S.; Wilcox, L.R. An Evaluation of Coronal Microleakage in Endodontically Treated Teeth. Part III. In Vivo Study. J. Endod. 1988, 14, 455–458. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.-K.; Fan, B.; Wesselink, P.R. Diminished Leakage along Root Canals Filled with Gutta-percha without Sealer over Time: A Laboratory Study. Int. Endod. J. 2000, 33, 121–125. [Google Scholar] [CrossRef] [PubMed]
- Prüllage, R.-K.; Urban, K.; Schäfer, E.; Dammaschke, T. Material Properties of a Tricalcium Silicate–Containing, a Mineral Trioxide Aggregate–Containing, and an Epoxy Resin–Based Root Canal Sealer. J. Endod. 2016, 42, 1784–1788. [Google Scholar] [CrossRef]
- Atmeh, A.R.; Chong, E.Z.; Richard, G.; Festy, F.; Watson, T.F. Dentin-Cement Interfacial Interaction: Calcium Silicates and Polyalkenoates. J. Dent. Res. 2012, 91, 454–459. [Google Scholar] [CrossRef]
- Camps, J.; Jeanneau, C.; El Ayachi, I.; Laurent, P.; About, I. Bioactivity of a Calcium Silicate–Based Endodontic Cement (BioRoot RCS): Interactions with Human Periodontal Ligament Cells In Vitro. J. Endod. 2015, 41, 1469–1473. [Google Scholar] [CrossRef]
- Pane, E.S.; Palamara, J.E.A.; Messer, H.H. Critical Evaluation of the Push-out Test for Root Canal Filling Materials. J. Endod. 2013, 39, 669–673. [Google Scholar] [CrossRef]
- Gesi, A.; Raffaelli, O.; Goracci, C.; Pashley, D.H.; Tay, F.R.; Ferrari, M. Interfacial Strength of Resilon and Gutta-Percha to Intraradicular Dentin. J. Endod. 2005, 31, 809–813. [Google Scholar] [CrossRef]
- Chisnoiu, R.; Moldovan, M.; Chisnoiu, A.; Hrab, D.; Rotaru, D.; Păstrav, O.; Delean, A. Comparative Apical Sealing Evaluation of Two Bioceramic Endodontic Sealers. Med. Pharm. Rep. 2019, 92, S55–S60. [Google Scholar] [CrossRef] [PubMed]
- Chen, I.; Salhab, I.; Setzer, F.C.; Kim, S.; Nah, H.-D. A New Calcium Silicate–Based Bioceramic Material Promotes Human Osteo- and Odontogenic Stem Cell Proliferation and Survival via the Extracellular Signal-Regulated Kinase Signaling Pathway. J. Endod. 2016, 42, 480–486. [Google Scholar] [CrossRef]
- Sagsen, B.; Ustün, Y.; Demirbuga, S.; Pala, K. Push-out Bond Strength of Two New Calcium Silicate-based Endodontic Sealers to Root Canal Dentine. Int. Endod. J. 2011, 44, 1088–1091. [Google Scholar] [CrossRef]
- Donnermeyer, D.; Dornseifer, P.; Schäfer, E.; Dammaschke, T. The Push-out Bond Strength of Calcium Silicate-Based Endodontic Sealers. Head Face Med. 2018, 14, 13. [Google Scholar] [CrossRef] [PubMed]
- Al-Hiyasat, A.S.; Alfirjani, S.A. The Effect of Obturation Techniques on the Push-out Bond Strength of a Premixed Bioceramic Root Canal Sealer. J. Dent. 2019, 89, 103169. [Google Scholar] [CrossRef] [PubMed]
- Mounes, B.B.; Alhashimi, R. The Push out Bond Strength of Bioceramic Seal-Er (Total Fill) after Warm and Cold Obturation Tech-Niques An in Vitro Comparative Study. J. Baghdad Coll. Dent. 2022, 34, 7–16. [Google Scholar] [CrossRef]
- Bolenwar, A.; Reche, A.; Dhamdhere, N.; Rathi, S. Applications of Silver Nanoparticles in Dentistry. Cureus 2023, 15, e44090. [Google Scholar] [CrossRef]
- Wang, J.; Jiang, W.; Liang, J.; Ran, S. Influence of Silver Nanoparticles on the Resin-Dentin Bond Strength and Antibacterial Activity of a Self-Etch Adhesive System. J. Prosthet. Dent. 2022, 128, 1363.e1–1363.e10. [Google Scholar] [CrossRef]
- Jowkar, Z.; Shafiei, F.; Asadmanesh, E.; Koohpeima, F. Influence of Silver Nanoparticles on Resin-Dentin Bond Strength Durability in a Self-Etch and an Etch-and-Rinse Adhesive System. Restor. Dent. Endod. 2019, 44, e13. [Google Scholar] [CrossRef]
- Yin, I.X.; Zhang, J.; Zhao, I.S.; Mei, M.L.; Li, Q.; Chu, C.H. The Antibacterial Mechanism of Silver Nanoparticles and Its Application in Dentistry. Int. J. Nanomed. 2020, 15, 2555–2562. [Google Scholar] [CrossRef]
- Sheethal Dsouza, T.; Shetty, A.; Dsouza, N. Evaluation of pH, Calcium Ion Release, and Dimensional Stability of an Experimental Silver Nanoparticle-Incorporated Calcium Silicate-Based Cement. Bioinorg. Chem. Appl. 2021, 2021, 3919543. [Google Scholar] [CrossRef] [PubMed]
- Zand, V.; Mokhtari, H.; Hasani, A.; Jabbari, G. Comparison of the Penetration Depth of Conventional and Nano-Particle Calcium Hydroxide into Dentinal Tubules. Iran. Endod. J. 2017, 12, 366–370. [Google Scholar] [CrossRef]
- Hashmi, A.; Zhang, X.; Kishen, A. Impact of Dentin Substrate Modification with Chitosan-Hydroxyapatite Precursor Nanocomplexes on Sealer Penetration and Tensile Strength. J. Endod. 2019, 45, 935–942. [Google Scholar] [CrossRef]
- Balto, H.; Bukhary, S.; Al-Omran, O.; BaHammam, A.; Al-Mutairi, B. Combined Effect of a Mixture of Silver Nanoparticles and Calcium Hydroxide against Enterococcus Faecalis Biofilm. J. Endod. 2020, 46, 1689–1694. [Google Scholar] [CrossRef] [PubMed]
- Stelzer, R.; Schaller, H.-G.; Gernhardt, C.R. Push-out Bond Strength of RealSeal SE and AH Plus after Using Different Irrigation Solutions. J. Endod. 2014, 40, 1654–1657. [Google Scholar] [CrossRef]
- Mourdikoudis, S.; Pallares, R.M.; Thanh, N.T.K. Characterization techniques for nanoparticles: Comparison and complementarity upon studying nanoparticle properties. Nanoscale 2018, 10, 12871–12934. [Google Scholar] [CrossRef]
- Nie, B.; Huo, S.; Qu, X.; Guo, J.; Liu, X.; Hong, Q.; Wang, Y.; Yang, J.; Yue, B. Bone Infection Site Targeting Nanoparticle-Antibiotics Delivery Vehicle to Enhance Treatment Efficacy of Orthopedic Implant Related Infection. Bioact. Mater. 2022, 16, 134–148. [Google Scholar] [CrossRef]
- Mallineni, S.K.; Sakhamuri, S.; Kotha, S.L.; AlAsmari, A.R.G.M.; AlJefri, G.H.; Almotawah, F.N.; Mallineni, S.; Sajja, R. Silver Nanoparticles in Dental Applications: A Descriptive Review. Bioengineering 2023, 10, 327. [Google Scholar] [CrossRef]
- AbdelWahed, A.; Roshdy, N.; Elbanna, A. Evaluation of Push-out Bond Strength of CeraSeal Bioceramic Sealer with Different Obturation Techniques. Egypt. Dent. J. 2021, 67, 2655–2662. [Google Scholar] [CrossRef]
- DeLong, C.; He, J.; Woodmansey, K.F. The Effect of Obturation Technique on the Push-out Bond Strength of Calcium Silicate Sealers. J. Endod. 2015, 41, 385–388. [Google Scholar] [CrossRef]
- Alberdi (Koki), J.; Martin, G.; Risso, L.; Kaplan, A. Effect of Heat Generated by Endodontic Obturation Techniques on Bond Strength of Bioceramic Sealers to Dentine. J. Endod. 2023, 49, 1565–1569. [Google Scholar] [CrossRef]
- Besinis, A.; Van Noort, R.; Martin, N. Infiltration of Demineralized Dentin with Silica and Hydroxyapatite Nanoparticles. Dent. Mater. 2012, 28, 1012–1023. [Google Scholar] [CrossRef]
- AlGazlan, A.S.; Auda, S.H.; Balto, H.; Alsalleeh, F. Antibiofilm Efficacy of Silver Nanoparticles Alone or Mixed with Calcium Hydroxide as Intracanal Medicaments: An Ex-Vivo Analysis. J. Endod. 2022, 48, 1294–1300. [Google Scholar] [CrossRef]
- Chen, W.-P.; Chen, Y.-Y.; Huang, S.-H.; Lin, C.-P. Limitations of Push-out Test in Bond Strength Measurement. J. Endod. 2013, 39, 283–287. [Google Scholar] [CrossRef] [PubMed]
- Dewi, A.; Upara, C.; Sastraruji, T.; Louwakul, P. Effect of a Heat-based Root Canal Obturation Technique on Push-out Bond Strength of the Classical Bioceramic and New HiFlow Sealer. Aust. Endod. J. 2022, 48, 116–120. [Google Scholar] [CrossRef] [PubMed]
- Cimpean, S.I.; Burtea, A.L.C.; Chiorean, R.S.; Dudescu, M.C.; Antoniac, A.; Robu, A.; Campian, R.S.; Timis, L.I. Evaluation of Bond Strength of Four Different Root Canal Sealers. Materials 2022, 15, 4966. [Google Scholar] [CrossRef]
- Shokouhinejad, N.; Gorjestani, H.; Nasseh, A.A.; Hoseini, A.; Mohammadi, M.; Shamshiri, A.R. Push-out Bond Strength of Gutta-percha with a New Bioceramic Sealer in the Presence or Absence of Smear Layer. Aust. Endod. J. 2013, 39, 102–106. [Google Scholar] [CrossRef] [PubMed]

| Groups | Sealer Type | Filling Technique |
|---|---|---|
| Group 1 | TotalFill® BC Sealer | Single-cone technique |
| Group 2 | TotalFill® BC Sealer + AgNPs | Single-cone technique |
| Group 3 | TotalFill® HiFlow BC Sealer | Continuous wave condensation technique |
| Group 4 | TotalFill® HiFlow BC Sealer + AgNPs | Continuous wave condensation technique |
| N | Mean | Std. Deviation | p-Value | 95% Confidence Interval for Mean | Multiple Comparison Test (Tukey) | MCT * | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | Group 1 | Group 2 | Group 3 | Group 4 | ||||||
| Group 1 | 25 | 9.322 | 1.629 | 0.001 | 8.649 | 9.994 | 1 | a | |||
| Group 2 | 25 | 10.583 | 1.762 | 9.857 | 11.310 | 0.090 | 1 | ab | |||
| Group 3 | 25 | 9.915 | 2.247 | 8.988 | 10.843 | 0.593 | 0.681 | 1 | a | ||
| Group 4 | 25 | 11.406 | 1.831 | 10.650 | 12.162 | 0.001 | 0.414 | 0.031 | 1 | b | |
| Mode of Failure | Total | Ch-sq p-Value | ||||
|---|---|---|---|---|---|---|
| Adhesive | Cohesive | Mixed | ||||
| Group 1 | Count | 8 | 12 | 5 | 25 | 0.003 |
| % within Group | 32.0% | 48.0% | 20.0% | 100.0% | ||
| Group 2 | Count | 9 | 13 | 3 | 25 | |
| % within Group | 36.0% | 52.0% | 12.0% | 100.0% | ||
| Group 3 | Count | 5 | 15 | 5 | 25 | |
| % within Group | 20.0% | 60.0% | 20.0% | 100.0% | ||
| Group 4 | Count | 3 | 16 | 6 | 25 | |
| % within Group | 12.0% | 64.0% | 24.0% | 100.0% | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bukhary, S.; Alkahtany, S.; AlDabeeb, D. The Effect of Silver Nanoparticles on Bond Strength of Calcium Silicate-Based Sealer: An In Vitro Study. Appl. Sci. 2024, 14, 9817. https://doi.org/10.3390/app14219817
Bukhary S, Alkahtany S, AlDabeeb D. The Effect of Silver Nanoparticles on Bond Strength of Calcium Silicate-Based Sealer: An In Vitro Study. Applied Sciences. 2024; 14(21):9817. https://doi.org/10.3390/app14219817
Chicago/Turabian StyleBukhary, Sundus, Sarah Alkahtany, and Dalal AlDabeeb. 2024. "The Effect of Silver Nanoparticles on Bond Strength of Calcium Silicate-Based Sealer: An In Vitro Study" Applied Sciences 14, no. 21: 9817. https://doi.org/10.3390/app14219817
APA StyleBukhary, S., Alkahtany, S., & AlDabeeb, D. (2024). The Effect of Silver Nanoparticles on Bond Strength of Calcium Silicate-Based Sealer: An In Vitro Study. Applied Sciences, 14(21), 9817. https://doi.org/10.3390/app14219817






