Root Resorption during Orthodontic Treatment with Clear Aligners vs. Fixed Appliances—A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Search Processing
2.3. Eligibility Criteria
- Population: adult patients in need of orthodontic treatment, both male and female;
- Intervention: fixed orthodontic appliances or clear aligners for orthodontic therapy;
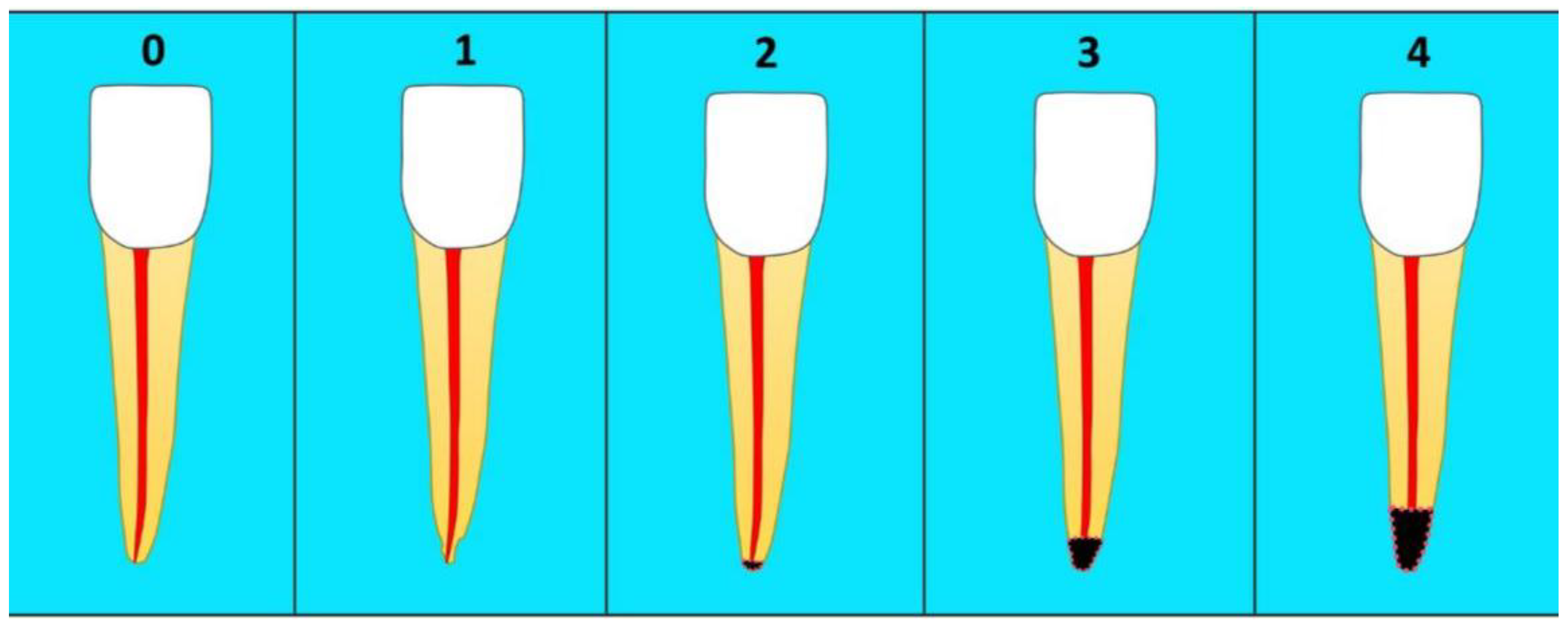
- Comparison: apical root resorption following fixed orthodontic therapy or clear aligners;
- Outcome: root volume variation before and after treatment.
2.4. Data Processing
3. Results
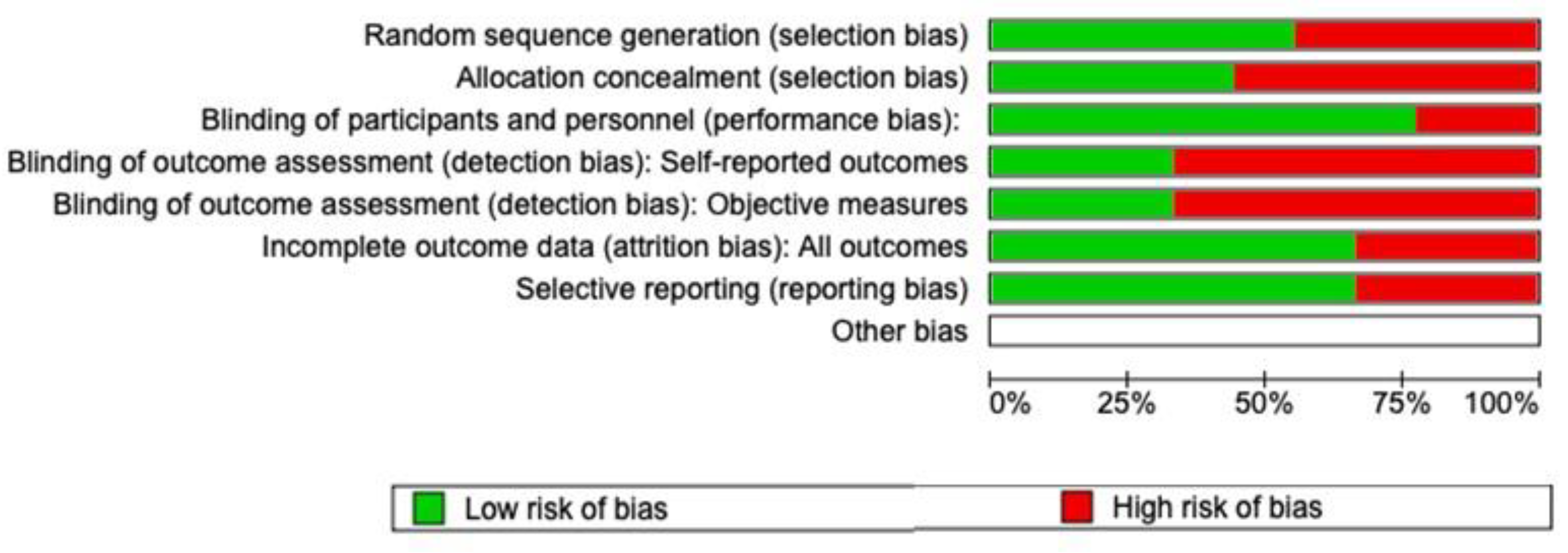
Quality Assessment and Risk of Bias
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Robertson, L.; Kaur, H.; Fagundes, N.C.F.; Romanyk, D.; Major, P.; Flores Mir, C. Effectiveness of Clear Aligner Therapy for Orthodontic Treatment: A Systematic Review. Orthod. Craniofac. Res. 2020, 23, 133–142. [Google Scholar] [CrossRef] [PubMed]
- Upadhyay, M.; Arqub, S.A. Biomechanics of Clear Aligners: Hidden Truths & First Principles. J. World Fed. Orthod. 2022, 11, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Bichu, Y.M.; Alwafi, A.; Liu, X.; Andrews, J.; Ludwig, B.; Bichu, A.Y.; Zou, B. Advances in Orthodontic Clear Aligner Materials. Bioact. Mater. 2022, 22, 384–403. [Google Scholar] [CrossRef] [PubMed]
- Lynch, N.M.; Shroff, B.; Carrico, C.K.; Sawicki, V.; Sabol, M.; Lindauer, S.J. Clear Aligner Therapy in the Mixed Dentition: Indications and Practitioner Perspectives. Am. J. Orthod. Dentofac. Orthop. 2023, 164, 172–182. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.M.; Weir, T.; Kaang, A.; Farella, M. Predictability of Lower Incisor Tip Using Clear Aligner Therapy. Prog. Orthod. 2022, 23, 37. [Google Scholar] [CrossRef]
- Simon, M.; Keilig, L.; Schwarze, J.; Jung, B.A.; Bourauel, C. Treatment Outcome and Efficacy of an Aligner Technique—Regarding Incisor Torque, Premolar Derotation and Molar Distalization. BMC Oral Health 2014, 14, 68. [Google Scholar] [CrossRef]
- Rapone, B.; Ferrara, E.; Santacroce, L.; Topi, S.; Gnoni, A.; Dipalma, G.; Mancini, A.; Di Domenico, M.; Tartaglia, G.M.; Scarano, A.; et al. The Gaseous Ozone Therapy as a Promising Antiseptic Adjuvant of Periodontal Treatment: A Randomized Controlled Clinical Trial. Int. J. Environ. Res. Public Health 2022, 19, 985. [Google Scholar] [CrossRef]
- Marrelli, M.; Tatullo, M.; Dipalma, G.; Inchingolo, F. Oral Infection by Staphylococcus Aureus in Patients Affected by White Sponge Nevus: A Description of Two Cases Occurred in the Same Family. Int. J. Med. Sci. 2012, 9, 47–50. [Google Scholar] [CrossRef]
- Inchingolo, F.; Tatullo, M.; Abenavoli, F.M.; Marrelli, M.; Inchingolo, A.D.; Villabruna, B.; Inchingolo, A.M.; Dipalma, G. Severe Anisocoria after Oral Surgery under General Anesthesia. Int. J. Med. Sci. 2010, 314–318. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Inchingolo, A.M.; Marinelli, G.; Malcangi, G.; Montenegro, V.; Laudadio, C.; Pede, C.D.; et al. The Efficacy of a New AMCOP® Elastodontic Protocol for Orthodontic Interceptive Treatment: A Case Series and Literature Overview. Int. J. Environ. Res. Public Health 2022, 19, 988. [Google Scholar] [CrossRef]
- Jung, W.-S.; Kim, K.; Cho, S.; Ahn, S.-J. Adhesion of Periodontal Pathogens to Self-Ligating Orthodontic Brackets: An in-Vivo Prospective Study. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Di Paola, A.; Tortora, C.; Argenziano, M.; Marrapodi, M.M.; Rossi, F. Emerging Roles of the Iron Chelators in Inflammation. Int. J. Mol. Sci. 2022, 23, 7977. [Google Scholar] [CrossRef] [PubMed]
- Coloccia, G.; Inchingolo, A.D.; Inchingolo, A.M.; Malcangi, G.; Montenegro, V.; Patano, A.; Marinelli, G.; Laudadio, C.; Limongelli, L.; Di Venere, D.; et al. Effectiveness of Dental and Maxillary Transverse Changes in Tooth-Borne, Bone-Borne, and Hybrid Palatal Expansion through Cone-Beam Tomography: A Systematic Review of the Literature. Medicina (B Aires) 2021, 57, 288. [Google Scholar] [CrossRef]
- Rapone, B.; Inchingolo, A.D.; Trasarti, S.; Ferrara, E.; Qorri, E.; Mancini, A.; Montemurro, N.; Scarano, A.; Inchingolo, A.M.; Dipalma, G.; et al. Long-Term Outcomes of Implants Placed in Maxillary Sinus Floor Augmentation with Porous Fluorohydroxyapatite (Algipore® FRIOS®) in Comparison with Anorganic Bovine Bone (Bio-Oss®) and Platelet Rich Plasma (PRP): A Retrospective Study. J. Clin. Med. 2022, 11, 2491. [Google Scholar] [CrossRef] [PubMed]
- Feller, L.; Khammissa, R.A.G.; Thomadakis, G.; Fourie, J.; Lemmer, J. Apical External Root Resorption and Repair in Orthodontic Tooth Movement: Biological Events. BioMed Res. Int. 2016, 2016, 4864195. [Google Scholar] [CrossRef] [PubMed]
- Malcangi, G.; Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Garibaldi, M.; Inchingolo, A.M.; Piras, F.; Cardarelli, F.; Settanni, V.; et al. Impacted Central Incisors in the Upper Jaw in an Adolescent Patient: Orthodontic-Surgical Treatment—A Case Report. Appl. Sci. 2022, 12, 2657. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Inchingolo, A.M.; Marinelli, G.; Malcangi, G.; Montenegro, V.; Laudadio, C.; Palmieri, G.; et al. Genetic Pattern, Orthodontic and Surgical Management of Multiple Supplementary Impacted Teeth in a Rare, Cleidocranial Dysplasia Patient: A Case Report. Medicina 2021, 57, 1350. [Google Scholar] [CrossRef] [PubMed]
- Vimercati, L.; De Maria, L.; Quarato, M.; Caputi, A.; Gesualdo, L.; Migliore, G.; Cavone, D.; Sponselli, S.; Pipoli, A.; Inchingolo, F.; et al. Association between Long COVID and Overweight/Obesity. J. Clin. Med. 2021, 10, 4143. [Google Scholar] [CrossRef]
- Malcangi, G.; Inchingolo, A.D.; Inchingolo, A.M.; Piras, F.; Settanni, V.; Garofoli, G.; Palmieri, G.; Ceci, S.; Patano, A.; Mancini, A.; et al. COVID-19 Infection in Children and Infants: Current Status on Therapies and Vaccines. Children 2022, 9, 249. [Google Scholar] [CrossRef]
- Yassir, Y.A.; Nabbat, S.A.; McIntyre, G.T.; Bearn, D.R. Clinical Effectiveness of Clear Aligner Treatment Compared to Fixed Appliance Treatment: An Overview of Systematic Reviews. Clin. Oral Investig. 2022, 26, 2353–2370. [Google Scholar] [CrossRef]
- Inchingolo, F.; Tatullo, M.; Abenavoli, F.M.; Marrelli, M.; Inchingolo, A.D.; Inchingolo, A.M.; Dipalma, G. Non-Hodgkin Lymphoma Affecting the Tongue: Unusual Intra-Oral Location. Head Neck Oncol. 2011, 3, 1. [Google Scholar] [CrossRef]
- Tortora, C.; Di Paola, A.; Argenziano, M.; Creoli, M.; Marrapodi, M.M.; Cenni, S.; Tolone, C.; Rossi, F.; Strisciuglio, C. Effects of CB2 Receptor Modulation on Macrophage Polarization in Pediatric Celiac Disease. Biomedicines 2022, 10, 874. [Google Scholar] [CrossRef]
- Di Cosola, M.; Cazzolla, A.P.; Charitos, I.A.; Ballini, A.; Inchingolo, F.; Santacroce, L. Candida albicans and Oral Carcinogenesis. A Brief Review. J. Fungi 2021, 7, 476. [Google Scholar] [CrossRef]
- Lin, E.; Julien, K.; Kesterke, M.; Buschang, P.H. Differences in Finished Case Quality between Invisalign and Traditional Fixed Appliances. Angle Orthod. 2022, 92, 173–179. [Google Scholar] [CrossRef]
- Reddy, L.K.V.; Madithati, P.; Narapureddy, B.R.; Ravula, S.R.; Vaddamanu, S.K.; Alhamoudi, F.H.; Minervini, G.; Chaturvedi, S. Perception about Health Applications (Apps) in Smartphones towards Telemedicine during COVID-19: A Cross-Sectional Study. J. Pers. Med. 2022, 12, 1920. [Google Scholar] [CrossRef]
- Rathi, S.; Chaturvedi, S.; Abdullah, S.; Rajput, G.; Alqahtani, N.M.; Chaturvedi, M.; Gurumurthy, V.; Saini, R.; Bavabeedu, S.S.; Minervini, G. Clinical Trial to Assess Physiology and Activity of Masticatory Muscles of Complete Denture Wearer Following Vitamin D Intervention. Medicina (B Aires) 2023, 59, 410. [Google Scholar] [CrossRef] [PubMed]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Ronsivalle, V.; Shapira, I.; Cicciù, M. Prevalence of Temporomandibular Disorders in Subjects Affected by Parkinson Disease: A Systematic Review and Metanalysis. J. Oral Rehabil. 2023, 50, 877–885. [Google Scholar] [CrossRef] [PubMed]
- Crescente, G.; Minervini, G.; Spagnuolo, C.; Moccia, S. Cannabis Bioactive Compound-Based Formulations: New Perspectives for the Management of Orofacial Pain. Molecules 2022, 28, 106. [Google Scholar] [CrossRef]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Di Blasio, M.; Ronsivalle, V.; Cicciù, M. Children Oral Health and Parents Education Status: A Cross Sectional Study. BMC Oral Health 2023, 23, 787. [Google Scholar] [CrossRef]
- Deregibus, A.; Ferrillo, M.; Grazia Piancino, M.; Chiara Domini, M.; de Sire, A.; Castroflorio, T. Are Occlusal Splints Effective in Reducing Myofascial Pain in Patients with Muscle-Related Temporomandibular Disorders? A Randomized-Controlled Trial. Turk. J. Phys. Med. Rehabil. 2021, 67, 32–40. [Google Scholar] [CrossRef]
- Gay, G.; Ravera, S.; Castroflorio, T.; Garino, F.; Rossini, G.; Parrini, S.; Cugliari, G.; Deregibus, A. Root Resorption during Orthodontic Treatment with Invisalign®: A Radiometric Study. Prog. Orthod. 2017, 18, 12. [Google Scholar] [CrossRef] [PubMed]
- Pasini, M.; Giuca, M.R.; Ligori, S.; Mummolo, S.; Fiasca, F.; Marzo, G.; Quinzi, V. Association between Anatomical Variations and Maxillary Canine Impaction: A Retrospective Study in Orthodontics. Appl. Sci. 2020, 10, 5638. [Google Scholar] [CrossRef]
- Adina, S.; Dipalma, G.; Bordea, I.R.; Lucaciu, O.; Feurdean, C.; Inchingolo, A.D.; Septimiu, R.; Malcangi, G.; Cantore, S.; Martin, D.; et al. Orthopedic Joint Stability Influences Growth and Maxillary Development: Clinical Aspects. J. Biol. Regul. Homeost. Agents 2020, 34, 747–756. [Google Scholar] [CrossRef] [PubMed]
- Cirulli, N.; Inchingolo, A.D.; Patano, A.; Ceci, S.; Marinelli, G.; Malcangi, G.; Coloccia, G.; Montenegro, V.; Pede, C.D.; Ciocia, A.M.; et al. Innovative Application of Diathermy in Orthodontics: A Case Report. Int. J. Environ. Res. Public Health 2022, 19, 7448. [Google Scholar] [CrossRef]
- Li, Y.; Deng, S.; Mei, L.; Li, Z.; Zhang, X.; Yang, C.; Li, Y. Prevalence and Severity of Apical Root Resorption during Orthodontic Treatment with Clear Aligners and Fixed Appliances: A Cone Beam Computed Tomography Study. Prog. Orthod. 2020, 21, 1. [Google Scholar] [CrossRef]
- Fanali, S.; Tumedei, M.; Pignatelli, P.; Inchingolo, F.; Pennacchietti, P.; Pace, G.; Piattelli, A. Implant Primary Stability with an Osteocondensation Drilling Protocol in Different Density Polyurethane Blocks. Comput. Methods Biomech. Biomed. Engin 2021, 24, 14–20. [Google Scholar] [CrossRef]
- Zhang, X.; Zhou, H.; Liao, X.; Liu, Y. The Influence of Bracket Torque on External Apical Root Resorption in Bimaxillary Protrusion Patients: A Retrospective Study. BMC Oral Health 2022, 22, 7. [Google Scholar] [CrossRef] [PubMed]
- Quinzi, V.; Saccomanno, S.; Manenti, R.; Giancaspro, S.; Paskay, L.; Marzo, G. Efficacy of Rapid Maxillary Expansion with or without Previous Adenotonsillectomy for Pediatric Obstructive Sleep Apnea Syndrome Based on Polysomnographic Data: A Systematic Review and Meta-Analysis. Appl. Sci. 2020, 10, 6485. [Google Scholar] [CrossRef]
- De Felice, M.E.; Nucci, L.; Fiori, A.; Flores-Mir, C.; Perillo, L.; Grassia, V. Accuracy of Interproximal Enamel Reduction during Clear Aligner Treatment. Prog. Orthod. 2020, 21, 28. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Dipalma, G.; Palmieri, G.; Di Pede, C.; Semjonova, A.; Patano, A.; Ceci, S.; Cardarelli, F.; Montenegro, V.; Garibaldi, M.; et al. Functional Breastfeeding: From Nutritive Sucking to Oral Health. J. Biol. Regul. Homeost. Agents 2022, 36, 121–137. [Google Scholar]
- Maspero, C.; Cappella, A.; Dolci, C.; Cagetti, M.G.; Inchingolo, F.; Sforza, C. Is Orthodontic Treatment with Microperforations Worth It? A Scoping Review. Children 2022, 9, 208. [Google Scholar] [CrossRef]
- Folco, A.A.; Benítez-Rogé, S.C.; Iglesias, M.; Calabrese, D.; Pelizardi, C.; Rosa, A.; Brusca, M.I.; Hecht, P.; Mateu, M.E. Gingival Response in Orthodontic Patients: Comparative Study between Self-Ligating and Conventional Brackets. Acta Odontol. Latinoam. 2014, 27, 120–124. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Lin, S.; Chen, J.; Huang, L.; Huang, Z.; Li, H. Risk Factors for Midcourse Correction during Treatment of First Series of Aligners with Invisalign. Am. J. Orthod. Dentofac. Orthop. 2022, 162, e96–e102. [Google Scholar] [CrossRef] [PubMed]
- Iglesias-Linares, A.; Sonnenberg, B.; Solano, B.; Yañez-Vico, R.-M.; Solano, E.; Lindauer, S.J.; Flores-Mir, C. Orthodontically Induced External Apical Root Resorption in Patients Treated with Fixed Appliances vs. Removable Aligners. Angle Orthod. 2017, 87, 3–10. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Ceci, S.; Patano, A.; Inchingolo, A.M.; Montenegro, V.; Di Pede, C.; Malcangi, G.; Marinelli, G.; Coloccia, G.; Garibaldi, M.; et al. Elastodontic Therapy of Hyperdivergent Class II Patients Using AMCOP® Devices: A Retrospective Study. Appl. Sci. 2022, 12, 3259. [Google Scholar] [CrossRef]
- Jiang, T.; Wu, R.Y.; Wang, J.K.; Wang, H.H.; Tang, G.H. Clear Aligners for Maxillary Anterior En Masse Retraction: A 3D Finite Element Study. Sci. Rep. 2020, 10, 10156. [Google Scholar] [CrossRef]
- Krishnan, V. Critical Issues Concerning Root Resorption: A Contemporary Review. World J. Orthod. 2005, 6, 30–40. [Google Scholar]
- Brezniak, N.; Wasserstein, A. Root Resorption after Orthodontic Treatment: Part 2. Literature Review. Am. J. Orthod. Dentofac. Orthop. 1993, 103, 138–146. [Google Scholar] [CrossRef]
- Baumrind, S.; Korn, E.L.; Boyd, R.L. Apical Root Resorption in Orthodontically Treated Adults. Am. J. Orthod. Dentofac. Orthop. 1996, 110, 311–320. [Google Scholar] [CrossRef]
- Mirabella, A.D.; Artun, J. Risk Factors for Apical Root Resorption of Maxillary Anterior Teeth in Adult Orthodontic Patients. Am. J. Orthod. Dentofac. Orthop. 1995, 108, 48–55. [Google Scholar] [CrossRef]
- Levander, E.; Bajka, R.; Malmgren, O. Early Radiographic Diagnosis of Apical Root Resorption during Orthodontic Treatment: A Study of Maxillary Incisors. Eur. J. Orthod. 1998, 20, 57–63. [Google Scholar] [CrossRef]
- Killiany, D.M. Root Resorption Caused by Orthodontic Treatment: An Evidence-Based Review of Literature. Semin. Orthod. 1999, 5, 128–133. [Google Scholar] [CrossRef] [PubMed]
- Sameshima, G.T.; Sinclair, P.M. Predicting and Preventing Root Resorption: Part II. Treatment Factors. Am. J. Orthod. Dentofac. Orthop. 2001, 119, 511–515. [Google Scholar] [CrossRef]
- Malmgren, O.; Goldson, L.; Hill, C.; Orwin, A.; Petrini, L.; Lundberg, M. Root Resorption after Orthodontic Treatment of Traumatized Teeth. Am. J. Orthod. 1982, 82, 487–491. [Google Scholar] [CrossRef]
- Brezniak, N.; Wasserstein, A. Orthodontically Induced Inflammatory Root Resorption. Part. II: The Clinical Aspects. Angle Orthod. 2002, 72, 180–184. [Google Scholar] [CrossRef]
- Linge, L.; Linge, B.O. Patient Characteristics and Treatment Variables Associated with Apical Root Resorption during Orthodontic Treatment. Am. J. Orthod. Dentofac. Orthop. 1991, 99, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Harris, E.F. Root Resorption during Orthodontic Therapy. Semin. Orthod. 2000, 6, 183–194. [Google Scholar] [CrossRef]
- Levander, E.; Malmgren, O.; Eliasson, S. Evaluation of Root Resorption in Relation to Two Orthodontic Treatment Regimes. A Clinical Experimental Study. Eur. J. Orthod. 1994, 16, 223–228. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Healthcare Interventions: Explanation and Elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef]
- Aman, C.; Azevedo, B.; Bednar, E.; Chandiramami, S.; German, D.; Nicholson, E.; Nicholson, K.; Scarfe, W.C. Apical Root Resorption during Orthodontic Treatment with Clear Aligners: A Retrospective Study Using Cone-Beam Computed Tomography. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 842–851. [Google Scholar] [CrossRef]
- Yi, J.; Xiao, J.; Li, Y.; Li, X.; Zhao, Z. External Apical Root Resorption in Non-Extraction Cases after Clear Aligner Therapy or Fixed Orthodontic Treatment. J. Dent. Sci. 2018, 13, 48–53. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Shao, J.; Li, S.; Al-Balaa, M.; Xia, L.; Li, H.; Hua, X. Volumetric Cone-Beam Computed Tomography Evaluation and Risk Factor Analysis of External Apical Root Resorption with Clear Aligner Therapy. Angle Orthod. 2021, 91, 597–603. [Google Scholar] [CrossRef]
- Toyokawa-Sperandio, K.C.; Conti, A.C.d.C.F.; Fernandes, T.M.F.; Almeida-Pedrin, R.R.; Almeida, M.R.; Oltramari, P.V.P. External Apical Root Resorption 6 Months after Initiation of Orthodontic Treatment: A Randomized Clinical Trial Comparing Fixed Appliances and Orthodontic Aligners. Korean J. Orthod. 2021, 51, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Almagrami, I.; Almashraqi, A.A.; Almaqrami, B.S.; Mohamed, A.S.; Wafaie, K.; Al-Balaa, M.; Qiao, Y. A Quantitative Three-Dimensional Comparative Study of Alveolar Bone Changes and Apical Root Resorption between Clear Aligners and Fixed Orthodontic Appliances. Prog. Orthod. 2023, 24, 6. [Google Scholar] [CrossRef] [PubMed]
- Alqadasi, B.; Xia, H.Y.; Alhammadi, M.S.; Hasan, H.; Aldhorae, K.; Halboub, E. Three-Dimensional Assessment of Accelerating Orthodontic Tooth Movement-Micro-Osteoperforations vs. Piezocision: A Randomized, Parallel-Group and Split-Mouth Controlled Clinical Trial. Orthod. Craniofac. Res. 2021, 24, 335–343. [Google Scholar] [CrossRef]
- Patianna, A.G.; Ballini, A.; Meneghello, M.; Cantore, S.; Inchingolo, A.M.; Dipalma, G.; Inchingolo, A.D.; Inchingolo, F.; Malcangi, G.; Lucchese, A.; et al. Comparison of Conventional Orthognathic Surgery and “Surgery-First” Protocol: A New Weapon against Time. J. Biol. Regul. Homeost. Agents 2019, 33, 59–67. [Google Scholar]
- Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Inchingolo, A.M.; Marinelli, G.; Malcangi, G.; Di Pede, C.; Garibaldi, M.; Ciocia, A.M.; et al. Treatment of Class III Malocclusion and Anterior Crossbite with Aligners: A Case Report. Medicina 2022, 58, 603. [Google Scholar] [CrossRef]
- Pasciuti, E.; Coloccia, G.; Inchingolo, A.D.; Patano, A.; Ceci, S.; Bordea, I.R.; Cardarelli, F.; Venere, D.D.; Inchingolo, F.; Dipalma, G. Deep Bite Treatment with Aligners: A New Protocol. Appl. Sci. 2022, 12, 6709. [Google Scholar] [CrossRef]
- Patano, A.; Malcangi, G.; Inchingolo, A.D.; Garofoli, G.; De Leonardis, N.; Azzollini, D.; Latini, G.; Mancini, A.; Carpentiere, V.; Laudadio, C.; et al. Mandibular Crowding: Diagnosis and Management—A Scoping Review. J. Pers. Med. 2023, 13, 774. [Google Scholar] [CrossRef]


| Article Screening Strategy | Databases: Scopus, Web of Science, and PubMed |
| Keywords: A “APICAL ROOT RESORPTION”; B “CLEAR ALIGNES” | |
| Boolean variable: “AND” | |
| Timespan: 2013–2023 | |
| Language: English |
| Authors (Year) | Type of the Study | Aim of the Study | Materials | Results |
|---|---|---|---|---|
| Gay et al. [31] 2017 | Radiometric study | The study’s goal was to look at the prevalence and severity of root resorption in adult patients wearing aligners. | Panoramic radiographs taken at the start (T0) and end (T1) of the clear aligner therapy were used to measure the lengths of 1083 teeth’s roots and crowns. | Root resorption (RR) could result from Invisalign® orthodontic treatment. However, it turned out that its incidence was extremely comparable to that which was described for orthodontic mild forces. |
| Iglesias-linares et al. [44] 2017 | Case-control genetic association study | To evaluate risk factors of EARR after CAT or FOT. | Genetic and clinical factors were evaluated in 172 patients treated with CA or fixed appliances. | Similar results were obtained after both treatments. |
| Aman et al. [60] 2018 | Retrospective study | The aim of the study was to investigate the incidence and severity of orthodontically induced root resorption with clear aligner therapy. | Maxillary incisor root lengths were measured using CBCT before and after treatment in 160 patients treated with clear aligners. | Minimal root resorption was the consequence of thorough treatment with clear aligners. |
| Eissa et al. [19] 2018 | Pilot study | The aim of this study was to evaluate the root resorption of maxillary incisors after treatment with aligners, compared with fixed appliances. | Thirty-three patients were divided into three groups. group 1: patients treated with clear aligners; group 2: patients treated with Damon brackets; group 3: patients treated with twin brackets. Maxillary incisor tooth lengths were evaluated using CBCT. | Root resorption after orthodontic treatment was a complication with various orthodontic techniques. Less root resorption was reported with the use of invisible aligners. |
| Yi et al. [61] 2018 | Clinical study | The amount of EARR in non-extraction patients undergoing CAT or fixed orthodontic treatment. | Panoramic radiographs of 80 patients treated with FOT and CAT. | EARR was lower in non-extraction patients treated with CA than in those treated with fixed appliances. |
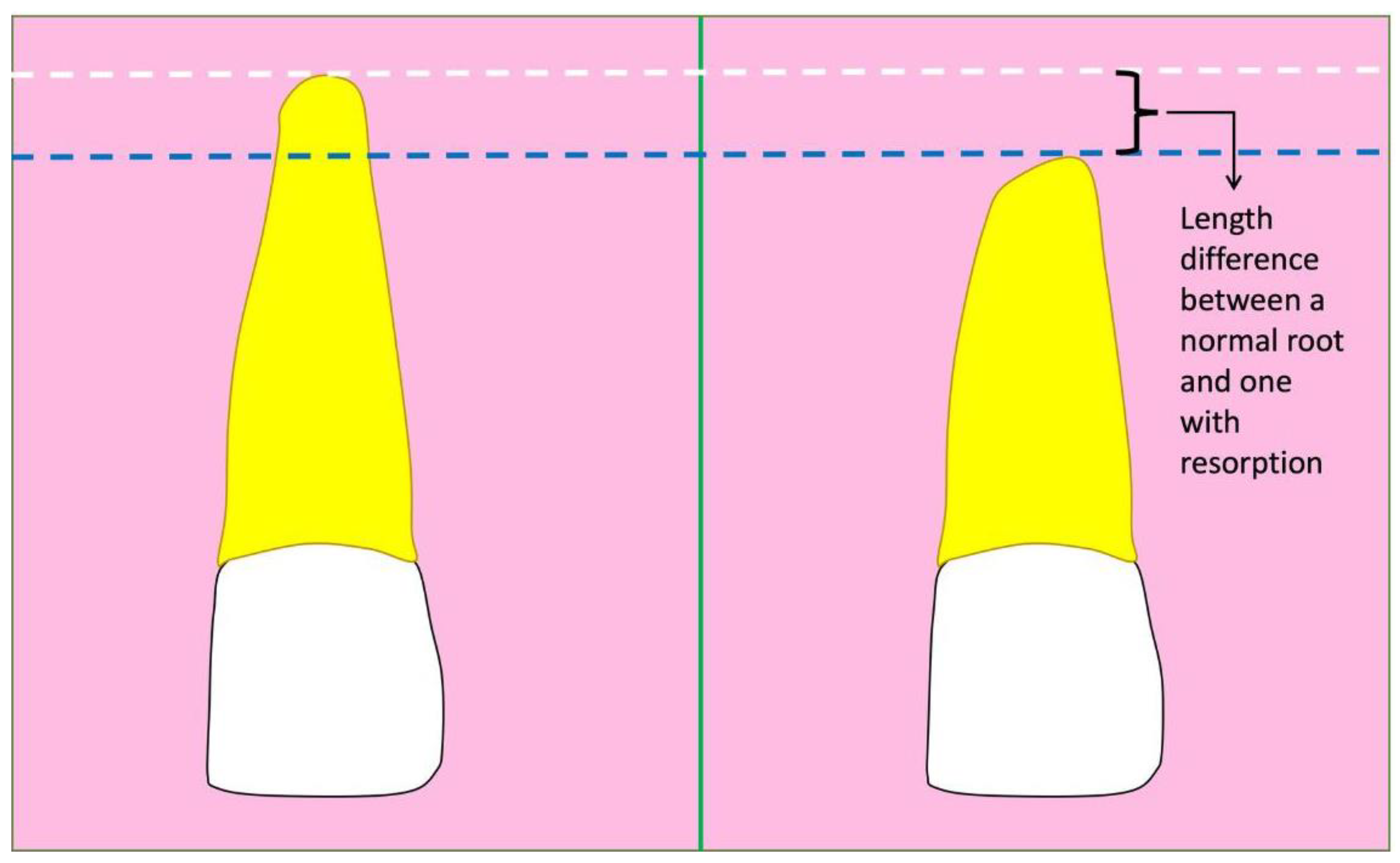
| Li et al. [35] 2020 | Cone beam computed tomography study | This study used CBCT to examine and evaluate the prevalence and severity of ARR in individuals receiving treatment with clear aligners and fixed appliances. | Total of 373 roots from 70 subjects divided into two groups (clear aligners group and fixed appliances group). The root length of each anterior tooth was measured on the basis of CBCT images. The ARR on each tooth was calculated as the difference in root length before and after orthodontic treatment. | Clear aligner patients had lower prevalence and severity of ARR than fixed appliance patients, as determined by CBCT. |
| Liu et al. [62] 2021 | Retrospective study | The purpose of the study was to investigate the prevalence and severity of root resorption with clear aligner therapy using CBCT. | This research included 320 incisors from 40 Class II patients with Invisalign aligners. Pre-treatment (T0) and post-treatment (T1) CBCT pictures were collected. | During aligner therapy, the majority of incisors had mild to moderate resorption; a very small proportion displayed severe resorption. |
| Toyokawa-Sperandio et al. [63] 2021 | Randomized clinical trial | To compare the amount of ARR after orthodontic therapy (fixed appliances vs. CA). | Intraoral radiographs of anterior teeth from 40 patients before (T0) and after 6 months (T1) of CAT or FOT. | Intraoral radiographs showed how both techniques resulted in a comparable ARR that does not affect the longevity of the teeth. |
| Almagrami et al. [64] 2023 | Retrospective study | The study’s goal was to examine the severity of orthodontically caused root resorption of maxillary incisors in those who used transparent aligners vs. fixed appliances. | One hundred and sixty maxillary incisors from 40 patients. Quantitative dentoalveolar changes were analyzed using pre- (T0) and post-treatment (T1) CBCT. | Treatments with clear aligners and fixed appliances appeared to cause increased root resorption in the maxillary incisor, with a higher incidence in fixed appliance treatments. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Inchingolo, F.; Inchingolo, A.M.; Palmieri, G.; Di Pede, C.; Garofoli, G.; de Ruvo, E.; Inchingolo, A.D.; Palermo, A.; Mancini, A.; Di Venere, D.; et al. Root Resorption during Orthodontic Treatment with Clear Aligners vs. Fixed Appliances—A Systematic Review. Appl. Sci. 2024, 14, 690. https://doi.org/10.3390/app14020690
Inchingolo F, Inchingolo AM, Palmieri G, Di Pede C, Garofoli G, de Ruvo E, Inchingolo AD, Palermo A, Mancini A, Di Venere D, et al. Root Resorption during Orthodontic Treatment with Clear Aligners vs. Fixed Appliances—A Systematic Review. Applied Sciences. 2024; 14(2):690. https://doi.org/10.3390/app14020690
Chicago/Turabian StyleInchingolo, Francesco, Angelo Michele Inchingolo, Giulia Palmieri, Chiara Di Pede, Grazia Garofoli, Elisabetta de Ruvo, Alessio Danilo Inchingolo, Andrea Palermo, Antonio Mancini, Daniela Di Venere, and et al. 2024. "Root Resorption during Orthodontic Treatment with Clear Aligners vs. Fixed Appliances—A Systematic Review" Applied Sciences 14, no. 2: 690. https://doi.org/10.3390/app14020690
APA StyleInchingolo, F., Inchingolo, A. M., Palmieri, G., Di Pede, C., Garofoli, G., de Ruvo, E., Inchingolo, A. D., Palermo, A., Mancini, A., Di Venere, D., Malcangi, G., & Dipalma, G. (2024). Root Resorption during Orthodontic Treatment with Clear Aligners vs. Fixed Appliances—A Systematic Review. Applied Sciences, 14(2), 690. https://doi.org/10.3390/app14020690











