Prediction of Mandibular Third Molar Impaction Using Linear and Angular Measurements in Young Adult Orthopantomograms
Abstract
1. Introduction
2. Materials and Methods
- Condyle length from the highest point of the mandibular condyle’s head to lowest point of the mandibular sigmoid notch plane, along the long axis of the condylar process.
- Coronoid length from the highest point of the mandibular coronoid process to the lowest point of the mandibular sigmoid notch plane, along the long axis of the coronoid process.
- Ramus height from the lowest point of the mandibular sigmoid notch to the point in the antegonial notch of the mandible, the ramus and body of the mandible are joined.
- Total ramus height from the highest point of the mandibular condyle’s head to the intersection point of the ramus plane and the mandibular plane.
- Ramal width from the deepest point of the anterior ramus notch concavity to the deepest point of the posterior ramus notch concavity.
- Mandibular body length from the intersection point of the ramus plane and the mandibular plane to the midpoint of the mandible.
- Sigmoid notch depth: the perpendicular line from the lowest point of the mandibular sigmoid notch to a line from the condylion and coronoid process.
- Posterior ramus notch depth from the perpendicular line from the deepest point of the posterior ramus notch concavity to the line that connects the point where the external contour of the cranial base intersects with the dorsal contour of the condylar head to the point of maximal convexity on the posterior border of the angular process of the mandible.
- Anterior ramus notch depth from the perpendicular line from the deepest point of the anterior ramus notch concavity to the perpendicolar line to the plane of the sigmoid notch and tangent to the descending anterior border of the ramus of the mandible.
- Antegonial notch depth from the perpendicular line from the deepest point of the mandibular inferior border notch concavity to the mandibular plane.
- Third molar width from the mesial aspect to distal aspect of third molar.
| Variable | Control Group (A) | Experimental Group (B) | p Value * | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| 1. Condyle length (cm) | 1.77 | 0.41 | 1.84 | 0.45 | 0.463 |
| 2. Coronoid length (cm) | 1.37 | 0.46 | 1.53 | 0.36 | 0.080 |
| 3. Ramus height (cm) | 6.37 | 0.57 | 6.18 | 0.68 | 0.199 |
| 4. Total ramus height (cm) | 7.40 | 0.73 | 7.30 | 0.80 | 0.540 |
| 5. Ramal width (cm) | 3.62 | 0.52 | 3.66 | 0.39 | 0.676 |
| 6. Mandibular body length (cm) | 10.97 | 1.24 | 10.90 | 1.11 | 0.787 |
| 7. Sigmoid notch depth (cm) | 1.43 | 0.33 | 1.59 | 0.31 | 0.030 |
| 8. Posterior ramus notch depth (cm) | 0.25 | 0.14 | 0.30 | 0.14 | 0.088 |
| 9. Anterior ramus notch depth (cm) | 0.27 | 0.22 | 0.24 | 0.19 | 0.490 |
| 10. Antegonial notch depth (cm) | 0.23 | 0.24 | 0.20 | 0.15 | 0.515 |
| 11. Third molar width (cm) | 1.38 | 0.27 | 1.41 | 0.14 | 0.424 |
| Retromolar space (cm) | 1.52 | 0.63 | 1.14 | 0.60 | 0.007 |
| 1. Angle condyle—coronoid process (deg) | 30.13 | 5.35 | 29.53 | 4.81 | 0.599 |
| 2. Gonial angle (deg) | 124.84 | 6.78 | 122.63 | 68.33 | 0.195 |
| 3.Inclination of lower posterior teeth (deg) | 95.53 | 5.93 | 92.65 | 6.23 | 0.521 |
| 4. Angle of impaction (deg) | 88.61 | 16.72 | 68.53 | 34.06 | 0.002 |
| Retromolar space/3M width (ratio) | 1.09 | 0.40 | 0.81 | 0.44 | 0.004 |
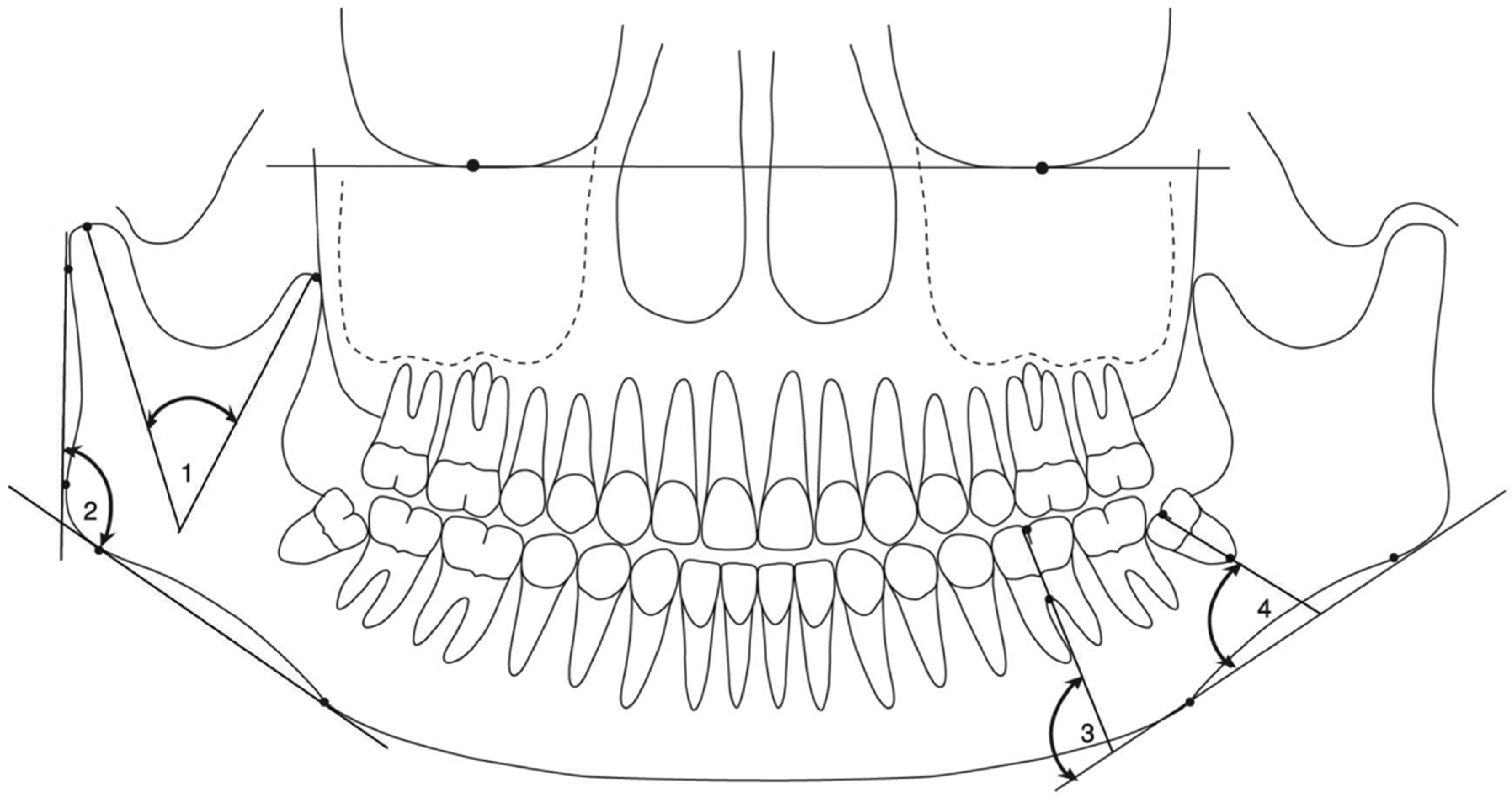
- Angle condyle—coronoid process: the intersection between the highest point of the mandibular condyle’s head to the highest point of the mandibular coronoid process.
- Gonial angle: the intersection between the line that connects the point where the external contour of the cranial base intersects with the dorsal contour of the condylar head to the point of maximal convexity on the posterior border of the angular process of the mandible and the mandibular plane.
- Inclination of lower posterior teeth: the intersection between the mandibular plane and the long axis of the first molar.
- Angle of impaction: the intersection between the mandibular plane and the long axis of the third molar.
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Al-Gunaid, T.H.; Bukhari, A.K.; El Khateeb, S.M.; Yamaki, M. Relationship of Mandibular Ramus Dimensions to Lower Third Molar Impaction. Eur. J. Dent. 2019, 13, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Al-Zoubi, H.; Alharbi, A.A.; Ferguson, D.J.; Zafar, M.S. Frequency of impacted teeth and categorization of impacted canines: A retrospective radiographic study using orthopantomograms. Eur. J. Dent. 2017, 11, 117–121. [Google Scholar] [CrossRef] [PubMed]
- Andreasen, J.O. Epidemiology of third molar impaction. In Textbook and Color Atlas of Tooth Impactions; Andreasen, J.O., Peterson, J.K., Laskin, D.M., Eds.; Munksgaard: Copenhagen, Denmark, 1997; pp. 222–223. [Google Scholar]
- Behbehani, F.; Årtun, J.; Thalib, L. Prediction of mandibular third-molar impaction in adolescent orthodontic patients. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Capelli, J., Jr. Mandibular growth and third molar impaction in extraction cases. Angle Orthod. 1991, 61, 223–229. [Google Scholar] [PubMed]
- Dierkes, D.D. An investigation of the mandibular third molars in orthodontic cases. Angle Orthod. 1975, 45, 207–212. [Google Scholar]
- Forsberg, C.M.; Vingren, B.; Wesslén, U. Mandibular third molar eruption in relation to available space as assessed on lateral cephalograms. Swed. Dent. J. 1989, 13, 23–31. [Google Scholar]
- Ganss, C.; Hochban, W.; Kielbassa, A.M.; Umstadt, H.E. Prognosis of third molar eruption. Oral Surg. Oral Med. Oral Pathol. 1993, 76, 688–693. [Google Scholar] [CrossRef]
- Gonca, M.; Gunacar, D.N.; Kose, T.E.; Karamehmetoglu, I. Evaluation of mandibular morphologic measurements and trabecular structure among subgroups of impacted mandibular third molars. Oral Radiol. 2021, 38, 63–71. [Google Scholar] [CrossRef]
- Vaibhav, N.; Vivek, G.; Shetty, A.; Mohammad, I.; Ahmed, N.; Umeshappa, H. Efficacy of various routes of dexamethasone administration in reducing postoperative sequelae following impacted third molar surgery. Ann. Maxillofac. Surg. 2020, 10, 61–65. [Google Scholar] [CrossRef]
- Garcia, R.I.; Chauncey, H.H. The eruption of third molarsin adults: A 10-year longitudinal study. Oral Surg. Oral Med. Oral Pathol. 1989, 68, 9–13. [Google Scholar] [CrossRef]
- Ghaeminia, H.; Nienhuijs, M.E.; Toedtling, V.; Perry, J.; Tummers, M.; Hoppenreijs, T.J.; Van der Sanden, W.J.; Mettes, T.G. Interventions for treating trouble-free impacted wisdom teeth in adults. Cochrane Database Syst Rev. 2020, 5, CD003879. [Google Scholar] [CrossRef]
- Mettes, T.D.; Ghaeminia, H.; Nienhuijs, M.E.; Perry, J.; van der Sanden, W.J.; Plasschaert, A. Surgical removal versus retention for the management of asymptomatic impacted wisdom teeth. Cochrane Database Syst Rev. 2012, 13, CD003879. [Google Scholar] [CrossRef]
- Jeevitha, J.Y.; Thiagarajan, A.; Sivalingam, B. Influence and Impact of Mandibular Ramal Dimensions on the Incidence of Lower Third Molar Impaction: A Prospective Study. J. Pharm. Bioallied Sci. 2022, 14 (Suppl. 1), S364–S368. [Google Scholar] [CrossRef]
- Bodner, L.; Brennan, P.A.; McLeod, N.M. Characteristics of iatrogenic mandibular fractures associated with tooth removal: Review and analysis of 189 cases. Br. J. Oral Maxillofac. Surg. 2011, 49, 567–572. [Google Scholar] [CrossRef]
- Boffano, P.; Roccia, F.; Gallesio, C.; Berrone, S. Pathological mandibular fractures: A review of the literature of the last two decades. Dent. Traumatol. 2013, 29, 185–196. [Google Scholar] [CrossRef]
- Memè, L.; Strappa, E.M.; Monterubbianesi, R.; Bambini, F.; Mummolo, S. SEM and FT-MIR Analysis of Human Demineralized Dentin Matrix: An In Vitro Study. Appl. Sci. 2022, 12, 1480. [Google Scholar] [CrossRef]
- Rossi, R.; Modoni, M.; Monterubbianesi, R.; Dallari, G.; Memè, L. The ‘Guided Tissue Regeneration (GTR) Effect’ of Guided Bone Regeneration (GBR) with the Use of Bone Lamina: A Report of Three Cases with More than 36 Months of Follow-Up. Appl. Sci. 2022, 12, 11247. [Google Scholar] [CrossRef]
- Rossi, R.; Memè, L.; Strappa, E.M.; Bambini, F. Restoration of Severe Bone and Soft Tissue Atrophy by Means of a Xenogenic Bone Sheet (Flex Cortical Sheet): A Case Report. Appl. Sci. 2023, 13, 692. [Google Scholar] [CrossRef]
- Grassi, A.; Memè, L.; Strappa, E.M.; Martini, E.; Bambini, F. Modified Periosteal Inhibition (MPI) Technique for Extraction Sockets: A Case Series Report. Appl. Sci. 2022, 12, 12292. [Google Scholar] [CrossRef]
- Khalil, H. Skeletal tracing of impacted and erupted mandibular third molar areas using panoramic radiographs. Biosci. Biotechnol. Res. Asia 2016, 7, 1–6. [Google Scholar]
- Richardson, M.E. The etiology and prediction of mandibular third molar impaction. Angle Orthod. 1977, 47, 165–172. [Google Scholar] [PubMed]
- Chen, Y.W.; Lee, C.T.; Hum, L.; Chuang, S.K. Effect of flap design on periodontal healing after impacted third molar extraction: A systematic review and meta-analysis. Int. J. Oral. Maxillofac. Surg. 2017, 46, 363–372. [Google Scholar] [CrossRef] [PubMed]
- Trakiniene, G.; Šidlauskas, A.; Švalkauskienė, V.; Smailienė, D.; Urbonė, J. The magnification in the lower third and second molar region in the digital panoramic radiographs. J. Forensic. Dent. Sci. 2017, 9, 91–95. [Google Scholar] [CrossRef]
- Caymaz, M.G.; Buhara, O. Association of Oral Hygiene and Periodontal Health with Third Molar Pericoronitis: A Cross-Sectional Study. Biomed. Res. Int. 2021, 2021, 6664434. [Google Scholar] [CrossRef]
- Ongkosuwito, E.M.; Dieleman, M.M.; Kuijpers-Jagtman, A.M.; Mulder, P.G.; van Neck, J.W. Linear mandibular measurements: Comparison between orthopantomograms and lateral cephalograms. Cleft Palate Craniofac. J. 2009, 46, 147–153. [Google Scholar] [CrossRef]
- Uthman, A.T. Retromolar space analysis in relation to selected linear and angular measurements for an Iraqi sample. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2007, 104, e76–e82. [Google Scholar] [CrossRef]
- Gupta, S.; Jain, S. Orthopantomographic Analysis for Assessment of Mandibular Asymmetry. J. Indian Orthod. Soc. 2012, 46, 33–37. [Google Scholar] [CrossRef]
- Haralabakis, H. Observations on the time of eruption, congenital absence and impaction of the third molar teeth. Trans. Eur. Orthod. Soc. 1957, 33, 308–309. [Google Scholar]
- Hassan, A.H. Mandibular cephalometric characteristic of a Saudi sample of patients having impacted third molars. Saudi Dent. J. 2011, 23, 73–80. [Google Scholar] [CrossRef]
- Hattab, F.N.; Alhaija, E.S. Radiographic evaluation of mandibular third molar eruption space. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1999, 88, 285–291. [Google Scholar] [CrossRef]
- Kaplan, R.G. Some factors related to mandibular third molar impaction. Angle Orthod. 1975, 45, 153–158. [Google Scholar] [PubMed]
- Niedzielska, I.A.; Drugacz, J.; Kus’, N.; Kręska, J. Panoramic radiographic predictors of mandibular third molar eruption. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2006, 102, 154–158. [Google Scholar] [CrossRef]
- Qamruddin, I.; Qayyum, W.; Haider, S.M.; Siddiqui, S.W.; Rehan, F. Differences in various measurements on panoramic radiograph among erupted and impacted lower third molar groups. J. Pak. Med. Assoc. 2012, 62, 883–887. [Google Scholar]
- Shiller, W.R. Positional changes in mesio-angular impacted mandibular third molars during a year. J. Am. Dent. Assoc. 1979, 99, 460–464. [Google Scholar] [CrossRef]
- Ventä, I.; Murtomaa, H.; Turtola, L.; Meurman, J.; Ylipaavalniemi, P. Clinical follow-up study of third molar eruption from ages 20 to 26 years. Oral Surg. Oral Med. Oral Pathol. 1991, 72, 150–153. [Google Scholar] [CrossRef]
- Ricketts, R.M. A principle of arcial growth of the mandible. Angle Orthod. 1972, 42, 368–386. [Google Scholar]
- Hugoson, A.; Kugelberg, C.F. The prevalence of third molars in a Swedish population. An epidemiological study. Community Dent. Health 1988, 5, 121–138. [Google Scholar]

| Variable | Control Group (A) | Experimental Group (B) | ||||||
|---|---|---|---|---|---|---|---|---|
| Retromolar Space | Retromolar Space | |||||||
| r | R2 | R2 (ADJ) | p Value | r | R2 | R2 (ADJ) | p Value | |
| Condyle length | −0.172 | 0.029 | 0.003 | 0.303 | −0.157 | 0.025 | 0.001 | 0.314 |
| Coronoid length | 0.354 | 0.125 | 0.101 | 0.029 | 0.035 | 0.001 | −0.023 | 0.826 |
| Ramus height | 0.222 | 0.049 | 0.023 | 0.181 | 0.151 | 0.023 | −0.001 | 0.335 |
| Total ramus height | 0.197 | 0.039 | 0.012 | 0.236 | 0.194 | 0.038 | 0.014 | 0.213 |
| Ramal width | 0.307 | 0.095 | 0.069 | 0.061 | 0.025 | 0.001 | −0.024 | 0.875 |
| Mandibular body length | 0.081 | 0.007 | −0.021 | 0.629 | −0.288 | 0.083 | 0.061 | 0.061 |
| Sigmoid notch depth | 0.064 | 0.004 | −0.024 | 0.701 | −0.149 | 0.022 | −0.002 | 0.339 |
| Posterior ramus notch depth | −0.192 | 0.037 | 0.010 | 0.249 | 0.188 | 0.035 | 0.012 | 0.227 |
| Anterior ramus notch depth | −0.521 | 0.271 | 0.251 | 0.001 | −0.454 | 0.206 | 0.187 | 0.002 |
| Antegonial notch depth | −0.379 | 0.144 | 0.120 | 0.019 | 0.295 | 0.087 | 0.065 | 0.055 |
| Third molar width | 0.456 | 0.208 | 0.186 | 0.004 | 0.095 | 0.009 | −0.015 | 0.545 |
| Gonial angle | 0.312 | 0.097 | 0.072 | 0.056 | 0.182 | 0.033 | 0.010 | 0.243 |
| Angle condyle—coronoid process | 0.071 | 0.005 | −0.023 | 0.673 | 0.402 | 0.162 | 0.141 | 0.008 |
| Inclination of lower posterior teeth | 0.142 | 0.020 | −0.007 | 0.396 | 0.397 | 0.157 | 0.137 | 0.008 |
| Angle of impaction | 0.176 | 0.031 | 0.004 | 0.290 | 0.245 | 0.060 | 0.037 | 0.113 |
| Retromolar space/3M width (ratio) | 0.966 | 0.933 | 0.931 | <0.001 | 0.971 | 0.942 | 0.941 | <0.001 |
| Variable | Control Group (Male Group A, n = 26) | Experimental Group (Male Group B, n = 24) | p Value * | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Condyle length (cm) | 1.76 | 0.43 | 1.86 | 0.37 | 0.365 |
| Coronoid length (cm) | 1.49 | 0.48 | 1.55 | 0.36 | 0.608 |
| Ramus height (cm) | 6.43 | 0.52 | 6.13 | 0.67 | 0.087 |
| Total ramus height (cm) | 7.48 | 0.70 | 7.25 | 0.79 | 0.294 |
| Ramal width (cm) | 3.69 | 0.55 | 3.58 | 0.33 | 0.421 |
| Mandibular body length (cm) | 10.81 | 1.11 | 10.88 | 1.18 | 0.836 |
| Sigmoid notch depth (cm) | 1.47 | 0.36 | 1.60 | 0.29 | 0.137 |
| Posterior ramus notch depth (cm) | 0.24 | 0.13 | 0.30 | 0.16 | 0.110 |
| Anterior ramus notch depth (cm) | 0.26 | 0.19 | 0.24 | 0.18 | 0.656 |
| Antegonial notch depth (cm) | 0.22 | 0.24 | 0.20 | 0.14 | 0.737 |
| Third molar width (cm) | 1.39 | 0.12 | 1.41 | 0.15 | 0.608 |
| Retromolar space (cm) | 1.54 | 0.59 | 1.10 | 0.58 | 0.010 |
| Angle condyle—coronoid process (deg) | 31.04 | 5.38 | 28.75 | 5.06 | 0.129 |
| Gonial angle (deg) | 124.81 | 7.48 | 122.33 | 8.76 | 0.287 |
| Inclination of lower posterior teeth (deg) | 91.15 | 5.70 | 92.70 | 6.65 | 0.753 |
| Angle of impaction (deg) | 90.93 | 8.69 | 69.46 | 32.66 | 0.002 |
| Retromolar space/3M width (ratio) | 1.09 | 0.39 | 0.77 | 0.39 | 0.006 |
| Variable | Control Group (Female Group A, n = 12) | Experimental Group (Female Group B, n = 19) | p Value * | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Condyle length (cm) | 1.81 | 0.36 | 1.82 | 0.53 | 0.943 |
| Coronoid length (cm) | 1.10 | 0.28 | 1.50 | 0.37 | 0.004 |
| Ramus height (cm) | 6.23 | 0.67 | 6.25 | 0.70 | 0.930 |
| Total ramus height (cm) | 7.23 | 0.77 | 7.35 | 0.82 | 0.688 |
| Ramal width (cm) | 3.46 | 0.41 | 3.75 | 0.45 | 0.077 |
| Mandibular body length (cm) | 11.32 | 1.48 | 10.93 | 1.04 | 0.396 |
| Sigmoid notch depth (cm) | 1.35 | 0.23 | 1.56 | 0.33 | 0.069 |
| Posterior ramus notch depth (cm) | 0.27 | 0.17 | 0.30 | 0.13 | 0.537 |
| Anterior ramus notch depth (cm) | 0.28 | 0.26 | 0.24 | 0.20 | 0.584 |
| Antegonial notch depth (cm) | 0.25 | 0.25 | 0.20 | 0.16 | 0.505 |
| Third molar width (cm) | 1.35 | 0.46 | 1.42 | 0.13 | 0.525 |
| Retromolar space (cm) | 1.49 | 0.76 | 1.19 | 0.65 | 0.255 |
| Angle condyle—coronoid process (deg) | 28.17 | 4.95 | 30.53 | 4.41 | 0.177 |
| Gonial angle (deg) | 124.92 | 5.23 | 123.00 | 7.83 | 0.461 |
| Inclination of lower posterior teeth (deg) | 96.50 | 5.50 | 92.58 | 5.81 | 0.072 |
| Angle of impaction (deg) | 83.58 | 26.98 | 67.37 | 36.62 | 0.197 |
| Retromolar space/3M width (ratio) | 1.07 | 0.45 | 0.85 | 0.50 | 0.240 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mummolo, S.; Gallusi, G.; Strappa, E.M.; Grilli, F.; Mattei, A.; Fiasca, F.; Bambini, F.; Memè, L. Prediction of Mandibular Third Molar Impaction Using Linear and Angular Measurements in Young Adult Orthopantomograms. Appl. Sci. 2023, 13, 4637. https://doi.org/10.3390/app13074637
Mummolo S, Gallusi G, Strappa EM, Grilli F, Mattei A, Fiasca F, Bambini F, Memè L. Prediction of Mandibular Third Molar Impaction Using Linear and Angular Measurements in Young Adult Orthopantomograms. Applied Sciences. 2023; 13(7):4637. https://doi.org/10.3390/app13074637
Chicago/Turabian StyleMummolo, Stefano, Gianni Gallusi, Enrico M. Strappa, Filippo Grilli, Antronella Mattei, Fabiana Fiasca, Fabrizio Bambini, and Lucia Memè. 2023. "Prediction of Mandibular Third Molar Impaction Using Linear and Angular Measurements in Young Adult Orthopantomograms" Applied Sciences 13, no. 7: 4637. https://doi.org/10.3390/app13074637
APA StyleMummolo, S., Gallusi, G., Strappa, E. M., Grilli, F., Mattei, A., Fiasca, F., Bambini, F., & Memè, L. (2023). Prediction of Mandibular Third Molar Impaction Using Linear and Angular Measurements in Young Adult Orthopantomograms. Applied Sciences, 13(7), 4637. https://doi.org/10.3390/app13074637










