Abstract
Facial acne vulgaris with post-inflammatory erythema is one of the most common problems encountered in dermatologic clinics. It can leave hypertrophic scars and cause psychological problems. Thus, effective therapeutic interventions are needed. The aim of this study was to evaluate the efficacy and safety of a pulsed-type bipolar radiofrequency (RF) device for treating acne and post-inflammatory erythema. Eighteen patients who had been diagnosed with acne underwent three sessions of bipolar RF treatment at 4 week intervals. Efficacy was assessed based on the number of acne lesions and the total area of lesions. Acne lesion count and area were determined by color correction using the Viola–Jones algorithm after converting the photos into a CIELAB image and extracting the area higher than the erythema threshold from the A* channel. Most patients showed significant clinical improvement after the treatments. Acne lesion counts of the forehead, left malar, right malar, and total areas of the left malar and right malar were decreased significantly after sessions (all p < 0.05). Adverse effects such as pinpoint bleeding and pain were noted. However, they were transient and not severe enough to stop treatment. Thus, such pulsed-type bipolar radiofrequency microneedling is a safe and effective treatment for acne and post-inflammatory erythema.
1. Introduction
Acne vulgaris is one of the most common inflammatory skin disorders, affecting nearly 85% of adolescents and young adults [1]. The current understanding of acne pathogenesis is continuously evolving. Key pathogenic factors that play an essential role in the development of acne are follicular hyperkeratinization, microbial colonization with Cutibacterium acne (C. acnes), sebum production, and complex inflammatory mechanisms [2]. This disease can leave permanent scars and cause psychological problems, such as poor self-image, depression, and anxiety.
Various treatment methods are being used in treating acne, ranging from conventional oral and topical medications to energy-based devices such as a pulsed-dye laser. Increased resistance to traditional treatment options, combined with undesirable side effects, has given way to alternative therapies. Some studies showed that the non-invasive methods (such as hydrogen purification, cosmetic acids, and oxybrasion) reduced skin eruptions and improved skin parameters. However, dermatological treatment cannot be replaced by cosmetological treatment [3,4]. Recently, microneedle electrodes have been applied for many acne vulgaris patients due to their fewer complications and rapid recovery time.
Radiofrequency (RF) devices produce focal thermal damage to the dermis. This focused energy preserves the epidermis and is associated with fewer complications, fewer side effects, and a quicker recovery time [5]. A previous study has found that a radiofrequency microneedle can cause thermal damage to pilosebaceous glands, although it is known to be an effective acne and scar treatment [6]. Various parameters, such as the number of inflammatory and non-inflammatory acne lesions, the erythema index, and transepidermal water loss after serial RF treatment, can be adjusted to improve treatment results [7,8]. However, no study has reported the effectiveness of bipolar RF device treatment using a skin-color imaging system. Kim et al. suggested that the skin-color imaging system, the NRSS grade (national rosacea society standard), and skin physiological factors are all highly significantly correlated in rosacea. Hence, the skin-color analysis system seems helpful in grading the severity of rosacea [9].
Thus, the aim of this study was to investigate the efficacy and safety of non-ablative, pulsed-type, bipolar radiofrequency microneedles in treating acne vulgaris with a novel and objective skin-color imaging system.
2. Materials and Methods
2.1. Subjects
A total of eighteen patients with acne vulgaris and post-inflammatory erythema were enrolled in this study at the Department of Dermatology, Korea University Ansan Hospital, Ansan, Republic of Korea, between January 2021 and August 2022. The study protocol was conducted in accordance with the Declaration of Helsinki. The Institutional Review Board (IRB) of Korea University Ansan Hospital approved this study (IRB no. 2022AS0252). All participants were informed of the benefits and risks of the procedures. Informed consent was obtained from each participant before study enrollment.
Exclusion criteria were: (1) patients with a history of keloid and photosensitivity disorder, (2) those with an active cutaneous infection or active dermatologic diseases, (3) patients who had been treated with oral retinoids within the last six months, (4) patients who used supplements or received botulinum toxin or fillers (5) those who received light or laser treatment within the previous three months, and (6) those with a high probability of having keloids or immunosuppression. Pregnant or breastfeeding women were also excluded. However, patients who were taking antibiotics for acne were included in this study.
2.2. Description of the Device and Study Design
The RF device used in our study was a pulsed-type bipolar radiofrequency with non-insulated microneedles. The device consisted of a handheld applicator with a disposable single-use tip (Sylfirm®, Viol, Gyeonggi, Republic of Korea). The 10 × 10 mm disposable tip comprises 25 non-insulated, minimally invasive microneedle electrodes (5 × 5 in a uniformly arranged pattern). Pulsed-type RF was delivered at a frequency of 2 MHz.
Before the RF treatment, patients were routinely applied 2.5% topical lidocaine cream (a eutectic mixture of 2.5% lidocaine HCl and 2.5% prilocaine; Taiguk Pharm Co., Ltd., Gyeonggi, Republic of Korea) to the face under occlusion for 30 min. Face water cleansing was used to remove all cosmetics. The study design is summarized in Figure 1. Patients were treated on both sides of the malar areas as well as the forehead. Patients were treated with three sessions at 4 week intervals (3~5 weeks) with the following settings: a penetration depth of 1.5 mm along the cheeks, nose, chin, and forehead, with <10% overlap for 1–2 passes. The energy level was set to power 3. The use of a non-comedogenic moisturizer several times daily for a few days after each treatment session was recommended in order to promote wound healing and prevent dryness. Patients were instructed to avoid overexposure to sunlight and to apply a broad-spectrum sunscreen after the post-therapy crusting subsided.
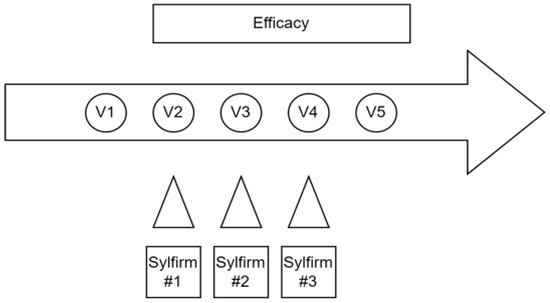
Figure 1.
Study design and visit flowchart.
2.3. Evaluation
Clinical assessment and photographs (EOS 80D; Canon KK, Tokyo, Japan) were documented at each visit, including baseline and final visits. To accurately measure each patient’s condition, the image was measured after resting for about 20 min at a constant temperature and humidity. A coefficient matrix was then obtained using SpyderCUBE® and SpyderChecker® for correction of white balance, exposure color (including redness), and black and white values. Color correction was performed by applying the coefficient matrix to the RGB image. After color correction, the face region was extracted using the Viola–Jones algorithm. In addition, the face region was separated into the forehead, left cheek, and right cheek areas. These divided face region images were converted into CIELAB images.
We set the following two variables to evaluate how much the erythema of acne and acne scars were improved by the radiofrequency microneedle device: the number of lesions exceeding the erythema threshold (NET) and the summation of the area exceeding the erythema threshold (pixel %). Many color channel transformations, including the gray channel, the blue-red difference channel, and the A* channel, were tested to assess the severity of erythema.
Among them, smoothness using the A* channel was used in this study to maximize the description of color difference. We performed pixel counts for the area higher than the threshold-specific value from A* channel images to obtain the NET of the area classified as a lesion from the entire region. After that, a summation of those areas was also obtained. Figure 2 shows the above process sequentially.
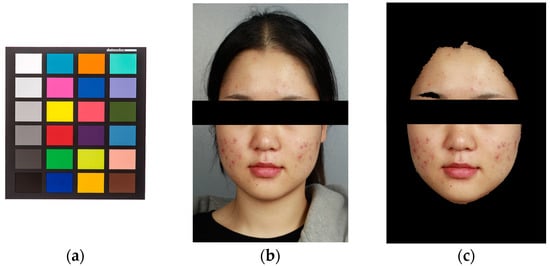
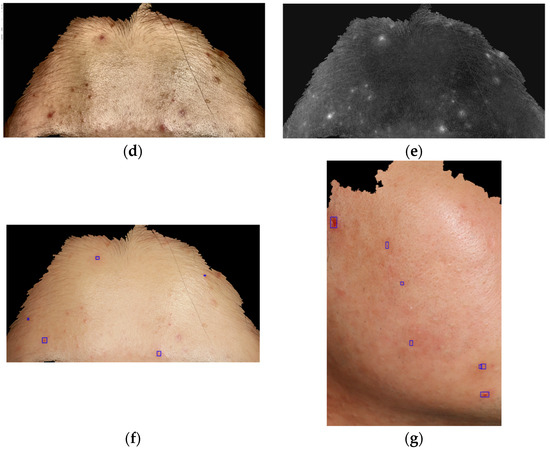
Figure 2.
Evaluation of the number of lesions exceeding the erythema threshold (NET) and summation of the area exceeding the erythema threshold (Pixel %) using a skin color analysis system. (a) SpyderCUBE® and SpyderChkecker® for correction of white balance, exposure color, and black and white values. (b) Facial region extraction with the Viola–Jones algorithm before (c) and after (d) converting into a CIELAB image. (e) A* channel images. (f,g) Area higher than the threshold-specific erythema value from A* channel images to evaluate the number of lesions exceeding the erythema threshold (NET) and the summation of the area exceeding the erythema threshold (pixel %).
2.4. Safety Assessment
The treatment site was visually inspected at each visit. Patients were questioned about treatment-related adverse events such as pain, tingling, bruising, edema, and/or irritation. All recorded side effects were reassessed at each session.
2.5. Statistical Analysis
All statistical analyses were performed using SPSS version 25 statistical software. A repeated ANOVA (analysis of variance) was used to compare whether variables changed over time. This analysis was limited to time variables with no control. Additionally, the Mann–Whitney U test was used to evaluate differences in NET and Pixel % between adjacent visits. A probability of less than 0.05 was considered statistically significant.
3. Results
The demographic and clinical data of all patients are summarized in Table 1. A total of 18 acne patients were enrolled in this study. Among them, ten patients were male and eight patients were female. Their mean age was 22.7 years. All patients were between 16 and 35 years old. All 18 patients completed this study. Five patients were taking oral antibiotics for acne: doxycycline and minocycline. There were no patients who had been treated with systemic retinoids and had a high probability of becoming pregnant or a propensity for keloids or immunosuppression.

Table 1.
Demographic data of acne vulgaris patients.
Table 2 and Table 3 summarize the clinical results. Almost all patients experienced decreases in the number and area of lesions. The mean number of NET (the number of lesions exceeding the erythema threshold) was significantly decreased from the first visit to the final visit (forehead, p = 0.039; left malar, p = 0.031; and right malar, p = 0.012). The mean number of Pixels % (summation of the area exceeding the erythema threshold) was significantly decreased from the first visit to the final visit for the left malar (p = 0.007) and the right malar (p = 0.002), but not for the forehead (p = 0.181). The forehead Pixel % showed no statistically significant difference after treatment.

Table 2.
Mean NET (number of lesions exceeding the erythema threshold) and Pixel % (summation of the area exceeding the erythema threshold) of acne vulgaris patients at each visit.

Table 3.
Median and IQR (interquartile range) of NET (number of lesions exceeding the erythema threshold) and Pixel % (summation of the area exceeding the erythema threshold) of acne vulgaris patients at each visit, suggested [median, IQR].
Additionally, a comparison was conducted between adjacent visits. Table 4 and Table 5 summarize the clinical results. NET (number of lesions exceeding the erythema threshold) on the forehead was significantly different between visits 1 and 2 (p = 0.015). Pixel % (summation of the area exceeding the erythema threshold) on the forehead was significantly different between visits 1 and 2 (p = 0.042). Pixel % on the right malar area was significantly different between visits 1 and 2 and between visits 2 and 3. No statistical significance was found between other visits. Figure 3 shows the changing severity of erythema according to treatment. These results are summarized in Table 4 and Table 5.

Table 4.
Mean difference of NET (number of lesions exceeding the erythema threshold) between adjacent visits.

Table 5.
Mean difference of pixel % (summation of the area exceeding the erythema threshold) between adjacent visits.
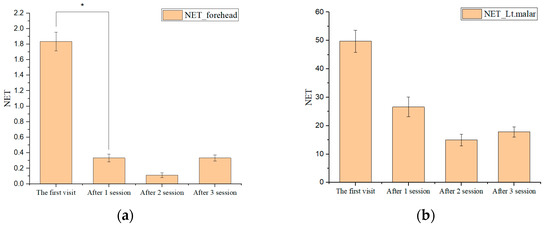
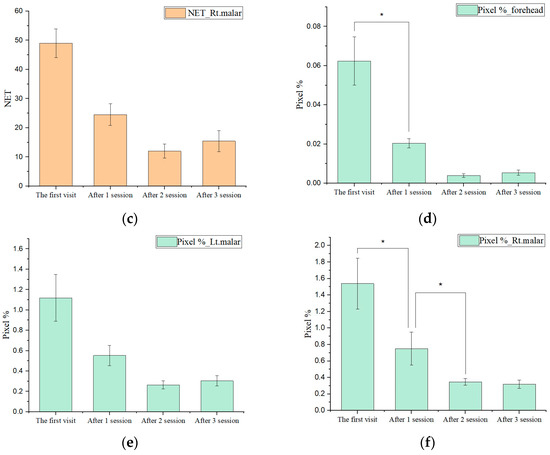
Figure 3.
Graphs of NET (number of lesions exceeding the erythema threshold) and pixel % (summation of the area exceeding the erythema threshold) at each session (a) NET of the forehead. (b) NET of left malar. (c) NET of right malar. (d) Pixel % of the forehead. (e) Pixel % of the left malar. (f) Pixel % of the right malar (* p < 0.05).
The side effects, such as transient pain, tingling sensations, and erythema, were reported after the treatment. However, these symptoms were mild and temporary and improved within one or two days. Other treatment-related adverse effects, such as hyperpigmentation, bruises, purpura, or infection, were not observed. During RF treatment and after the final treatment, temporary aggravation of acne vulgaris or folliculitis was not found. The results mentioned above are summarized in Figure 3. The patient’s clinical symptom improvement is shown in Figure 4.
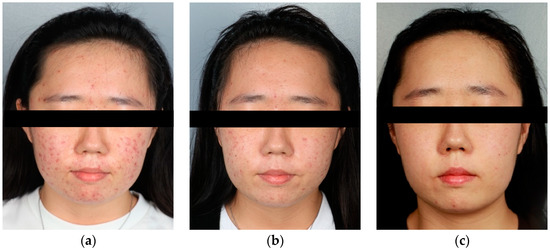
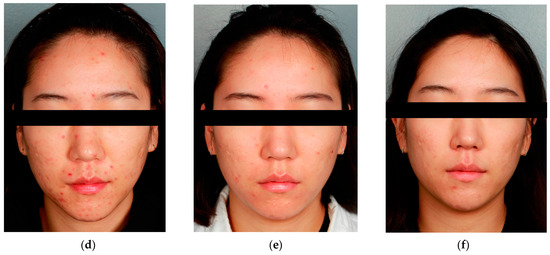
Figure 4.
Examples of improved clinical photos. (a,d) V1 (before the first session), (b,e) V3 (after the second session), and (c,f) V4 (after the third session).
4. Discussion
Acne is a multifactorial inflammatory disease affecting pilosebaceous follicles of the skin. Acne may leave post-inflammatory hyperpigmentation, post-inflammatory erythema, and scars with a textural change. Post-inflammatory erythema is common after acne inflammation. It is cosmetically unacceptable without adequate treatment [10]. Post-inflammatory erythema is considered a low-grade scar, not a superficial erythematous or vascular lesion [11].
RF devices have been used to treat acne vulgaris and post-inflammatory erythema. They have a minimal post-treatment recovery time and a high safety profile, especially for darker skin types [12]. Non-ablative RF needles can cause thermal damage to sebaceous glands. They can help treat acne by lowering sebum excretion, and several studies have found a quantitative relationship between sebum production and acne. [13]. Ruiz-Esparza et al. have treated 22 acne patients with a non-ablative RF device that could deliver RF energy at 6 MHz [14]. They showed a 75% or better diminution of active acne lesion counts in 82% of their patients.
Unlike monopolar RF, bipolar RF affects only the microneedle radiofrequency zone, allowing surrounding tissues to accelerate the wound healing process, which can result in a shorter recovery time [8]. A bipolar configuration provides a more controlled energy distribution and less pain than a monopolar RF. Moreover, newly developed pulsed-type RF differs from conventional continuous-type RF in that it transmits energy at very close intervals, thereby providing sufficient energy with less damage [15]. One study has demonstrated dramatic improvements in post-inflammatory erythema according to investigators’ and patients’ subjective assessments when using a bipolar pulsed RF device [8]. Additionally, after pulsed-type RF, in vivo mouse model histological specimens exhibited coagulation columns of thermal injury around each microneedle electrode in the dermis without noticeable tissue injury in the epidermis [16].
The first mechanism of bipolar pulsed RF for treating erythema is to create coagulation columns, a water-drop-shaped oval zone of thermal injury, at the tip of each electrode [16]. The electric current generates heat as it travels through the skin and meets tissue resistance. This heat causes collagen shrinkage and coagulation columns. Partial collagen denaturation occurs due to this heating, leading to collagen contraction and thickening, which can trigger neo-collagenosis and remodeling. Bipolar RF can not only cause dermal collagen remodeling but can also cause CD31-positive blood vessels to collapse and shrink in size due to coagulation [15]. Small, collapsed, slit-like CD31-positive blood vessels were noted throughout the dermis [15]. It could be one of the reasons why bipolar pulsed RF could reduce post-inflammatory erythema after acne.
The second mechanism of bipolar pulsed RF improving erythema is associated with the downregulation of VEGF-A (vascular endothelial growth factor-A). Several studies have suggested that post-inflammatory erythema due to acne is related to VEGF-mediated angiogenesis and lymphangiogenesis [17]. NF-kB, which activates IL-8 and VEGF expression, is chronically active in inflammatory diseases, including acne [10]. Histologically, IL-8, NF-κB, and VEGF staining intensity reductions are also observed eight weeks after the second session of RF treatment [10]. In other studies, downregulation of VEGF-A mRNA expression has been found in specimens from RF treatment groups compared with untreated control skin samples [15]. Additionally, Western blot analyses revealed gradual downexpression of the VEGF protein after treatment that was suppressed over the following 14 days in the RF treatment group, compared with untreated control skin [15].
In this study, pulsed-type bipolar RF microneedling devices decreased NET (number of lesions exceeding the erythema threshold) and pixel % (summation of the area exceeding the erythema threshold) when comparing each visit to the last visit. Previous studies have only performed subjective evaluations of erythema or only evaluated local erythema indexes [8]. However, in this study, the exact severity of erythema was evaluated after correcting the brightness, depth, and color of the entire photo of a patient’s face using a skin analysis system. After that, we accurately obtained erythema lesions using CIELAB. Observed clinical improvement in the present study was consistent with previous studies [8,9,10].
We set two variables: the number of lesions exceeding the erythema threshold (NET) and the summation of the area exceeding the erythema threshold (pixel %). In rosacea, the erythema of the entire face is important, but post-inflammatory erythema related to acne usually appears sparsely. Therefore, analyzing lesions above a certain threshold of redness was necessary. Using CIELAB, the number of red lesions exceeding a certain threshold and the sum of the total area were set as disease severity.
This study showed that a bipolar pulsed RF treatment could significantly reduce the number and area of acne and erythematous lesions. The mean number of NET (the number of lesions exceeding the erythema threshold) at three sites (the forehead, left malar, and right malar) was significantly decreased after the treatments. It indicates that the number of acne and acne scars has decreased. Additionally, Pixel % (the summation of the area exceeding the erythema threshold) was significantly decreased in two sites (left malar and right malar). It means the area affected by acne has improved. Although the area index on the forehead did not significantly improve, it might be due to obstacles such as hair while taking photos.
In this paper, to evaluate each aspect in more detail, our analysis compared adjacent visits. Significant differences were confirmed between visits one and two at three parts (NET of the forehead, pixel % of the forehead, and pixel % of the right malar), and between visits two and three at one part (right malar). According to this result, treatment response is significant in the early phase. This clinical improvement is consistent with the previous study [8].
Adverse effects such as pinpoint bleeding and pain were noted. However, they were transient and not severe enough to stop treatment. Other treatment-related adverse effects, such as hyperpigmentation, bruises, purpura, or infections, were not observed.
Our study has several limitations. First, it was a single-centered retrospective design. There may be selection bias because of the single-centered design and the small number of patients included. Second, since this study does not include a control group, the analysis was conducted only in time-variables without control in a repeated ANOVA (analysis of variance). Additionally, patients taking oral medications such as doxycycline and minocycline were included in this study. A multi-centered study with more patients and more control, including oral medications, might be needed.
5. Conclusions
Our study conclusion indicates that treatment with a bipolar pulsed RF device could be effective and safe for treating facial erythema in acne vulgaris. This was objectively demonstrated using the skin color analysis system and CIELAB. Herein, via a skin color analysis system, we found pulsed-type bipolar non-insulated microneedle RF treatment to be safe and effective in treating acne lesions and scars in Korean patients. This treatment modality can be another choice for patients who take only oral medication or pulsed dye laser for acne and scars. Additionally, the skin color analysis system and CIELAB are helpful for grading the severity of acne and post-inflammatory erythema, so those can be objective assessment tools in follow-up studies.
Author Contributions
Conceptualization, H.J.R.; methodology, J.Y.K.; investigation, H.J.R. and T.W.S.; writing—original draft preparation, T.W.S. and J.H.P.; writing—review and editing, H.J.R.; visualization, H.J.R.; supervision, H.J.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki. It was approved by the Institutional Review Board of Korea University Ansan Hospital (protocol code: 2022AS0252, date of approval: 27 September 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study. Written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
Not applicable.
Acknowledgments
This work was supported by a Korea University grant (K2208381).
Conflicts of Interest
The authors have no conflict of interest relevant to this study to disclose.
References
- Collier, C.N.; Harper, J.C.; Cafardi, J.A.; Cantrell, W.C.; Wang, W.; Foster, K.W.; Elewski, B.E. The prevalence of acne in adults 20 years and older. J. Am. Acad. Dermatol. 2008, 58, 56–59. [Google Scholar] [CrossRef] [PubMed]
- Katsambas, A.; Dessinioti, C. New and emerging treatments in dermatology: Acne. Dermatol. Ther. 2008, 21, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Chilicka, K.; Rusztowicz, M.; Rogowska, A.M.; Szygula, R.; Asanova, B.; Nowicka, D. Efficacy of Hydrogen Purification and Cosmetic Acids in the Treatment of Acne Vulgaris: A Preliminary Report. J. Clin. Med. 2022, 11, 6269. [Google Scholar] [CrossRef] [PubMed]
- Chilicka, K.; Rogowska, A.M.; Szygula, R.; Rusztowicz, M.; Nowicka, D. Efficacy of Oxybrasion in the Treatment of Acne Vulgaris: A Preliminary Report. J. Clin. Med. 2022, 11, 3824. [Google Scholar] [CrossRef]
- Biesman, B.S.; Pope, K. Monopolar radiofrequency treatment of the eyelids: A safety evaluation. Dermatol. Surg. 2007, 33, 794–801. [Google Scholar] [CrossRef] [PubMed]
- Lolis, M.S.; Goldberg, D.J. Radiofrequency in cosmetic dermatology: A review. Dermatol. Surg. 2012, 38, 1765–1776. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Goo, J.W.; Shin, J.; Chung, W.S.; Kang, J.M.; Kim, Y.K.; Bin Cho, S. Use of fractionated microneedle radiofrequency for the treatment of inflammatory acne vulgaris in 18 Korean patients. Dermatol. Surg. 2012, 38, 400–405. [Google Scholar] [CrossRef] [PubMed]
- Jung, Y.J.; Ro, Y.S.; Ryu, H.J.; Kim, J.E. Therapeutic effects of a new invasive pulsed-type bipolar radiofrequency for facial erythema associated with acne vulgaris and rosacea. J. Cosmet. Laser Ther. 2020, 22, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Ahn, J.W.; Ha, S.; Kwon, S.H.; Lee, O.; Oh, C. Clinical assessment of rosacea severity: Oriental score vs. quantitative assess-ment method with imaging and biomedical tools. Skin Res. Technol. 2017, 23, 186–193. [Google Scholar] [CrossRef]
- Min, S.; Park, S.Y.; Yoon, J.Y.; Kwon, H.H.; Suh, D.H. Fractional Microneedling Radiofrequency Treatment for Acne-related Post-inflammatory Erythema. Acta Derm. Venereol. 2016, 96, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.; Bourdes, V.; Bissonnette, R.; Petit, B.E.L.; Reynier, P.; Khammari, A.; Dreno, B. Prospective Study of Pathogenesis of Atrophic Acne Scars and Role of Macular Erythema. J. Drugs Dermatol. 2017, 16, 566–572. [Google Scholar] [PubMed]
- Gulfan, M.C.B.; Wanitphakdeedecha, R.; Wongdama, S.; Jantanapornchai, N.; Yan, C.; Rakchart, S. Efficacy and Safety of Using Noninsulated Microneedle Radiofrequency Alone Versus in Combination with Polynucleotides for the Treatment of Melasma: A Pilot Study. Dermatol. Ther. 2022, 12, 1325–1336. [Google Scholar] [CrossRef] [PubMed]
- Janiczek-Dolphin, N.; Cook, J.; Thiboutot, D.; Harness, J.; Clucas, A. Can sebum reduction predict acne outcome? Br. J. Dermatol. 2010, 163, 683–688. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Esparza, J.; Gomez, J.B. Nonablative radiofrequency for active acne vulgaris: The use of deep dermal heat in the treatment of moderate to severe active acne vulgaris (thermotherapy): A report of 22 patients. Dermatol. Surg. 2003, 29, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.B.; Na, J.; Zheng, Z.; Lim, J.M.; Kang, J.S.; Lee, J.H.; Lee, S.E. In vivo skin reactions from pulsed-type, bipolar, alternating current radiofrequency treatment using invasive noninsulated electrodes. Skin Res. Technol. 2018, 24, 318–325. [Google Scholar] [CrossRef] [PubMed]
- Na, J.; Zheng, Z.; Dannaker, C.; Lee, S.E.; Kang, J.S.; Cho, S.B. Electromagnetic Initiation and Propagation of Bipolar Radiofrequency Tissue Reactions via Invasive Non-Insulated Microneedle Electrodes. Sci. Rep. 2015, 5, 16735. [Google Scholar] [CrossRef] [PubMed]
- Gerber, P.A.; Buhren, B.A.; Steinhoff, M.; Homey, B. Rosacea: The cytokine and chemokine network. J. Investig. Dermatol. Symp. Proc. 2011, 15, 40–47. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).