Abstract
This study aimed to identify football players at high risk (HR) for anterior cruciate ligament (ACL) injury via a four-test battery and assess possible factors affecting classification. Ninety-one professional and semi-professional male athletes participated in a field-based pre-season screening. The cut-off points of the test battery were 10% acknowledged inter-limb asymmetry limit for quadriceps and hamstring isometric strength and single-leg triple hop for distance, in addition to the upper limit of 6 errors in the landing error scoring system (LESS). Additional assessment of hip adductors and core stability completed the global functional profile of the players. Sixty-one players were identified as HR and thirty as low-risk (LR) for ACL injury. Discriminant analysis showed that the proposed test battery classified accurately 78.0% of them, with 91.8 sensitivity and 61.9% specificity. Only four misclassified players in the LR group were at risk of inadequate treatment. All participants were considered healthy, and history of a previously rehabilitated injury did not interfere with the results. LESS seems to be the best predictor for injury-risk grouping. Prone bridge time was also a whole-body variable discriminating between groups. The proposed test battery provides a promising option for field-based pre-season ACL risk assessment of football players and needs to be studied prospectively.
1. Introduction
Anterior cruciate ligament (ACL) injury is one of the most dramatic injuries in football, resulting in knee pain and swelling, muscle atrophy, functional instability and at least six months of absence from participation [1]. In the long term, an ACL injury can be devastating for those failing to return to the preinjury level of participation [2], while for those who return to participation, there is an even higher risk for a secondary ACL injury. Re-injury rates in young athletes (<25 years) who return to sports have been reported to reach 23% [3]. Furthermore, it is estimated that one-third of the injured athletes will develop post-traumatic knee osteoarthritis, compromising their quality of life in the future [4,5,6]. Since ACL rupture may be life-changing, apart from career-threatening, the importance of efficient prevention is fundamental.
Although an ACL risk profile is multifactorial, inter-limb asymmetry has been associated with increased risk of both primary [7,8,9,10] and secondary ACL injury [11,12,13]. The passive tissues of the lower limbs are compromised when the impact forces are not equally distributed during landing due to biomechanical or postural control deficits between the two legs [11]. Abnormal asymmetrical landing biomechanics increase the risk of injury [14], as loads which are sustained by the strong leg, may endanger the weak side due to poor dissipation capability [15].
Pre-seasonal assessment (PA) has been recognized as mandatory for injury prevention; however, no clear guidelines are available at the moment [16]. Recently, regarding return to sport (RTS) after ACL reconstruction, the use of a battery of tests has been proposed that evaluate knee function in order to determine safe participation in pivoting sports [17]. An efficient RTS battery should include a combination of muscle strength tests, hop tests, and measures of quality of movement [18]. The main focus of researchers for the optimal PA is to avoid costly and time-consuming laboratory testing, enabling trainers and medical teams to apply low-cost, field-based screening tests, even in low-budget teams, without compromising the training plan. PA for injury risk-profiling with portable equipment such as push dynamometers, in combination with field tests, could be useful for quick assessment of high numbers of athletes, easily repeatable throughout the season [16]. Correct biomechanics during high-impact landing is acknowledged as a key element for load management and injury prevention. Assessment of quality of movement is important to be included in PA, and the landing error scoring system (LESS) is considered a valid and reliable tool for the assessment of the athlete’s landing pattern during a drop-jump task [19,20]. Regarding strength testing, hand-held dynamometry (HHD) is an appropriate method for use in clinical and field-based settings, with moderate to good reliability and validity [21].
The criteria used to discriminate between high and low-risk athletes are subjected to ongoing research, which aims to provide objective information, easily understood and applied to support the decision-making process. For muscle strength and hop tests, a common limb symmetry index > 90% is the most common acceptable criterion [17]. For the quality of movement when using the test landing error scoring system, various cutoff scores have been suggested, with up to six errors indicating acceptable landing mechanics [20,22,23]. Apart from the one-dimensional open-kinetic chain tests for muscle strength, hop performance and landing technique represent a global body function, connected to core stability [24,25,26,27].
For wide use in any location, functional tests to identify footballers prone to ACL injury should to be low-cost and relatively fast to perform, while at the same time, they should ideally balance between simplicity for feasibility and enough complexity for adequate information. Test batteries have been suggested, including strength and hop tests [16,28], while others highlight the need to assess landing biomechanics more thoroughly. LESS was developed to serve this requirement, avoiding the use of sophisticated equipment for in-field assessment. A combination of the above approaches with key muscle strength, low limb functional performance and assessment of landing biomechanics may provide a sensitive tool for identifying ACL injury-prone players.
The main objective in the current study was to identify professional/semi-professional football players at high risk for ACL injury based on a classification battery, including quadriceps and hamstring isometric dynamometry, the single-leg triple hop test for distance and the landing error scoring system (LESS). The low-risk (LR) and high-risk (HR) groups were compared in terms of proportions of players with (a) history of injury (general), (b) history of injury to the lower limbs, and (c) history of injury to the knee. An additional objective of the study was to identify the functional and biomechanical variables that significantly predicted the injury group categorization. In the functional variables, apart from the ones comprising the four criteria, other more global were added, including four that assess core stability and function. We also tested how accurately this criteria-battery classified players correctly into the two groups.
2. Materials and Methods
2.1. Study Design
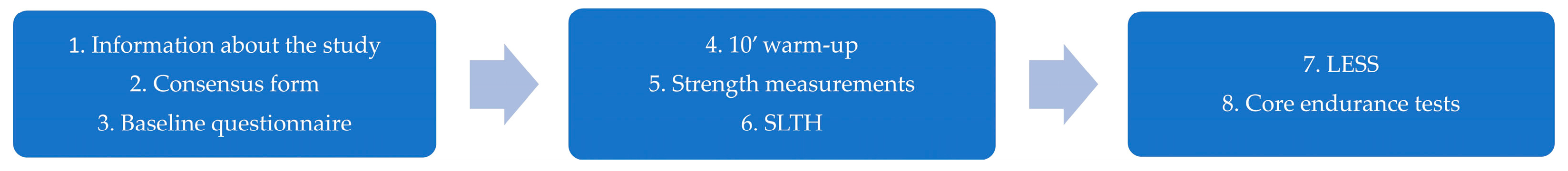
This was a cross-sectional study based on the STROBE (Strengthening the reporting of observational studies in epidemiology) guidelines for cross-sectional studies [29]. In the last week of July to the first week of August 2022, a pre-screening examination was conducted on professional and semi-professional football players to identify possible risk factors for ACL injury. Testing took place at the training facilities of the teams with portable equipment during the first two pre-season weeks. Data collection process is presented in Figure 1. Collected data included athletes’ demographic and previous injury details, hamstring and quadriceps isometric strength, the single-leg triple hop (SLTH) for distance test and scoring of landing mechanics with LESS. The strength and hop asymmetry upper limit of 10% and the maximum of six landing errors were considered the cut-off points to classify players to a low or high ACL injury risk group. Additional core stability tests were included for holistic body assessment. Specific details of each measurement methodology are provided below. The project was approved (ID 12126) by the institutional ethics committee of the University of Patras and is a part of the registered study protocol presented in the public database ClinicalTrials.gov (Identifier: NCT05425303).

Figure 1.
Data collection process.
2.2. Participants
Five football teams were examined: three of them in the professional Greek second division, and the remaining semi-professional, competing at the Greek third division, and the under-19 division. Due to the strict schedules of the teams at the beginning of the preparatory period, we assessed a convenience sample, since not all teams we approached gave their approval to approach their players. From the one-hundred and fifteen male players initially available for the examination, ninety-one eventually participated in the pre-screening examination. The rest were excluded due to recent history of injury, team schedule restrictions, and pain- or instability-induced incomplete measurements. Athletes eligible to participate in the study were free from injury or had been completely rehabilitated, had a professional work contract with their team, and participated in five to six training sessions per week in the previous season, depending on the game schedule. Fifty-seven suffered a previous injury, eleven of them to their knee. Demographics are presented in Table 1.

Table 1.
Participants’ demographic characteristics.
2.3. Baseline Assessment
Each athlete initially completed a questionnaire concerning demographics, sports participation characteristics, and previous injury details [30]. Additionally, athletes filled out a specific injury questionnaire reporting the type of injury, the injured limb, the time of injury, and the time lost from training and competition due to the injury.
2.4. Muscle-Strength Testing
After completing the questionnaire, isometric tests for quadriceps, hamstring, and abductor muscles were performed using an HHD (MicroFET 2; Hoggan Scientific, Salt Lake City, UT, USA). The same examiner performed all strength tests. A previous systematic review [31] indicated that HHD has moderate to good reliability and validity compared with the “gold standard” isokinetic dynamometer. Participants, after a warm-up including two trials of approximately 2 s of submaximal contraction, performed three maximal 5 s contractions, separated by a rest of at least 20 s. All tests were recorded in Newton, and the higher value was used for the calculation of the Limb Symmetry Index.
To assess knee extension strength, participants were seated on a specific metal table with the back straight, and both hip and knee angle at 90° of flexion. The participants kept their hands crossed on their chest. A physical therapist stabilized the thighs with his hands directly above the hip joint to prevent thigh movements during maximal quadriceps isometric contraction. A belt placed just proximally to the medial malleolus across a rigid frame on the back of the tibia, stabilized the HHD on this. Participants were asked to try to extend their tibia as forcefully as possible for five seconds. Hansen et al. [32] report that this testing configuration is a valid and reliable option for knee extensor strength testing.
To assess isometric hamstring strength, participants were placed in a prone position with their feet off the bed. The examiner passively flexed the knee at a height equal to the athlete’s foot length [21,33]. This position is approximately 30° of knee flexion. Then, the examiner placed the dynamometer on the heel and asked the athlete to contract their hamstrings maximally by flexing their knee as forcefully as possible for 5 s. This is an often-mentioned technique in the literature in order to assess hamstring strength using HHD [33,34]. Whiteley et al. [21], using HHD, reported an excellent inter-rater reliability (ICC = 0.96 for quadriceps and ICC = 0.91 for hamstrings) and a moderate-to-good correlation with isokinetic assessment.
Hip abductor strength was also measured to add information regarding the pelvis-stabilizing function, according to the protocol by Thorborg et al. [35], who reported high-to-excellent reliability (ICC = 0.76–0.98). The athletes were in a side-lying position, with the testing hip on the upside in a neutral position. The opposite leg was flexed in the hip and knee at approximately 90 degrees. The participants stabilized themselves by holding the examination table with their hands. The examiner stood behind them, one hand stabilizing the pelvis while the other hand held the HHD 5 cm proximal to the lateral malleolus. Then, the participants pushed maximally against the dynamometer for 5 s.
2.5. Single-Leg Triple Hop (SLTH) for Distance Test
After an approximately five-minute rest, the SLTH test was performed, which can highly discriminate strength and power deficits between the lower limbs [12,36,37], with high test–retest reliability (ICC = 0.91) [37]. Participants had up to 2 practice trials to familiarize themselves and a trial was classified as successful when the athlete maintained a single-leg stance for about 2 s after landing without losing balance., Participants alternated their legs for each trial to prevent fatigue, with an interval of approximately 20 s. Three successful hop trials for each leg were recorded to the closer centimeter, and the average value entered the analysis. The examiner kneeled close to the expected landing site to minimize the error of the measurement.
2.6. Landing Error Scoring System (LESS)
Subsequently, we used LESS to identify possible landing errors that may increase the risk of ACL injury. The LESS was performed after a five-minute rest from the SLTH test. The LESS is a valid and reliable tool [19,20] that assesses the participant’s landing pattern during a drop-jump task. The athletes jumped from a 30 cm box with both feet, landed at a distance equal to half of their height, and performed a maximum vertical jump. Beyond the information on the proper execution of the test, no other information was given regarding the proper landing technique. Athletes performed 1–2 trials for familiarization with the test, and then we recorded three successful jump-landing trials. No unsuccessful trials were observed. Two conventional cameras (Panasonic HC-V770 (Panasonic, Kadoma, Osaka, Japan) and Sony HDR-CX625 (Sony Corporation, Minato, Tokyo, Japan)) captured the trials from the frontal and sagittal view. The recorded video of three successful trials was stored on a personal computer and analyzed using the Kinovea software (0.8.26 experimental version). We used the scoring form and the guidelines of Padua et al. [20] to evaluate the landing technique. According to standardized guidelines, the scoring form contains 19 rating items that evaluate knee, hip, and trunk flexion angles from the side view, and knee valgus, base of support width, and toes position from the frontal view. The first fifteen items were assessed at initial contact and maximum knee flexion and given the value of “zero” for no error, thus a biomechanically correct landing, or “one” if landing error was observed. The prevailing value of the three attempts was representative of the specific item. The last two items contained the rater’s sense of the landing technique in terms of overall joint displacement and whole-body control, and there were three options: “zero” for no error, “one” for average and “two” for poor technique. More strict rules apply for those two items, and “two” is the final value even in case it presents only once during the three attempts. For the rest of the scenarios, the previous principle for the predominant value applies. The LESS total score can range from 0 to 19, with a higher value indicating a worse landing technique [20]. The average LESS score from the three trials was used for statistical analysis. Athletes with a total LESS score > 6 were considered to have a high-risk landing pattern for ACL injury [20,38]. The same examiner (NIL) who rated all videos had clinical experience in sports injury assessment and rehabilitation and the proper use of the LESS scoring instrument [39,40]. Test–retest reliability was examined in a random subgroup of 37 players and proved to be excellent (ICC = 0.927, 95% CI = 0.859–0.982).
2.7. Core Stability Tests
Two symmetric and one bilateral core stability tests were applied, intercepted by 5 min rest. The valid and reliable prone to bridge test was used to assess the capability of the abdominal muscles for core stability [41]. Both lateral abdominal muscles were tested via the side bridging test, according to the protocol proposed by McGill et al. [42]. Finally, the Biering-Sørensen test was used as a valid test for back muscle endurance [43]. For each test, players were informed about the proper execution and performed one trial for a few seconds for familiarization. The core endurance tests were performed in random order and as the last tests of the whole screening protocol to prevent the effect of fatigue on the other tests. Athletes were instructed to maintain the proper position of each test as long as possible until fatigue or discomfort. The examiner gave feedback about maintaining the appropriate position during the execution of each test. The assessor stopped the test if the proper position could not be held for two seconds. The maximum time in seconds that athletes maintained the proper position was recorded and used for analysis. Asymmetry index was calculated for the bilateral test.
2.8. Statistical Analysis
We calculated asymmetry for quadriceps, hamstring and abductor isometric strength, as well as for the core performance tests, regardless of dominance (absolute asymmetry). Asymmetry (%) was calculated using the equation (Dominant leg—Non-dominant leg)/Maximum (Dominant: Non-dominant) × 100. For all between-group comparisons, asymmetries were expressed in positive values regardless of limb dominance. As previously proposed [17], we considered asymmetries > 10% as critical for the risk of ACL injury and this applied for the strength and hop tests. In addition, the criterion of maximum 6 landing errors was used for the LESS test [38]. Statistical analysis was conducted using IBM SPSS (v.26). We used Chi-square test to compare the proportions of players with (a) a history of injury (general), (b) a history of injury to the lower limbs, and (c) a history of knee injury, between LRG and HRG. Discriminant analysis was used to investigate whether the original grouped cases were classified correctly. The significance level α = 0.05 was used. Binary logistic regression was used to identify possible predicting variables for the players who were misplaced by the proposed test battery. Apart from the four criteria for group splitting, independent variables connected to a more whole-body functionality entered the analysis, namely, LSI of isometric hip abductor strength, LSI of the time maintaining the lateral bridge position, time holding the prone bridge position and the Biering-Sørensen test for back extensors endurance.
3. Results
Results showed no significant differences in the proportion of previously injured players in the LRG and HRG (Table 2), thus ensuring that those factors did not interfere with the analysis. Binary logistic regression model included two predictors for risk grouping, the LESS score and the prone bridge time (Table 3). Scoring higher in the LESS and holding for a shorter period the prone bridge gave a significant predicting efficiency for the players that may be prone to ACL injury in the future.

Table 2.
The proportion of previous injury among LRG and HRG.

Table 3.
Predictors for the categorical “ACL risk” variable (0 = Low risk, 1 = High risk).
The criteria battery classified accurately in 78.0% of the originally grouped cases, which gave a statistically significant Chi-square = 27.485, p = 0.000. Its sensitivity, the ability to determine the HR players correctly, was 91.8% and its specificity, the ability to determine the LR players correctly was 61.9%.
We isolated four false negative cases from the LRG and sixteen false positive cases in the HRG, and treated them as separate subgroups to identify a possible different pattern in their four criteria scores. For this profiling, absolute asymmetry values were used to produce meaningful means (Table 4).

Table 4.
The absolute values of percent asymmetry and LESS score for the 4 and 16 misclassified players, in the respective Low-risk and High-risk groups (mean ± SD).
Observing the results, we notice that the four players were initially placed in the LRG, but were corrected as HRG according to the discriminant analysis; their mean LESS score was close to the acceptable upper limit of 6 errors, while strength and functional symmetry percentages were low.
For the sixteen players initially placed in the HRG and then corrected as LRG according to the discriminant analysis, their means of asymmetry, as well as the mean LESS score, were far below the criteria. They were initially considered as high risk because they presented either only one asymmetry > 10% and the rest of the criteria were clearly passed (values much lower than the cutoffs), or they exceeded critical values in two criteria, but only marginally. It is noticeable that the mean LESS of the initially LR players was higher than the mean LESS of the initially HR players.
4. Discussion
The main objective in the current study was to identify professional/semi-professional football players at high risk for ACL injury based on a classification battery of tests (four criteria). The critical values were based on the current consensus for inter-limb asymmetry (10%) and the upper limit of 6 landing errors as proposed for the LESS. Pre-season screening of the professional/semiprofessional football players classified the majority of players in the high-risk group for ACL injury. Only 30 of the 91 athletes met the four criteria and were considered low-risk. Previous injuries which were considered healed, regardless of location, did not interfere with the results, since proportions were very similar between the two risk-prediction groups. This can be explained on the basis that, players with incomplete rehabilitation, recent injuries, or those who failed to perform maximally due to pain or instability, were excluded from the study. Our results are in line with Markström et al. [44], who, based on a battery of tests including hop tests and isometric strength tests, found that 83% of the athletes with ACL reconstruction and 76% of the non-injured athletes failed to pass the criteria for symmetry of ≤10%. Thus, when formulating either prevention or rehabilitation programs, acceptable functional asymmetry should be considered without being tested, even among competitive athletes.
Enough evidence supports the use of a battery of tests for ACL injury risk assessment [16,17]. Holistic body functionality is also connected to ACL protective mechanisms and all recent prevention programs try to restore correct landing biomechanics [28]. LESS is a tool that assesses the latter, considering trunk mechanics as well [7]. In addition, injury prognostic tools should be easy to perform in any non-laboratory location, without expensive and too-sophisticated equipment, while at the same time maintaining high standards of reliability and external validity. Therefore, we considered that a battery comprising of isometric testing of the major antagonistic thigh muscle groups, a functional test of multiple jumps and a more global-technically oriented test would create a meaningful tool to enhance the ACL injury predictive potential in soccer.
The most important predictor variable for risk categorization was the LESS score, followed by the prone bridge test. This finding highlights the importance of a holistic approach during pre-season screening for ACL injury risk. The total LESS score is derived from 17 different scores assessing separate variables of landing technique after a drop jump. This obviously depends on the global body’s potential to provide correct limb alignment and efficient force dissipation. We considered this test as a necessary supplement to the triple-hop test. The prone bridge test was among the supplementary tests we selected to structure a more holistic functional profile of the players. It assessed the endurance of the frontal trunk and lower limb muscles while stabilizing the trunk in a high-leverage position. Core stability has drawn attention to its connection to functional performance and injury prevention [25,26,41]. A stable core provides the basis for the effective load transmission between body segments and especially during hopping or high-velocity cutting, it keeps torques produced by the torso to safe limits. Failing to control the trunk during dynamic high-energy maneuvers, often occurring in football, would let the upper body sway excessively and put the knee under ACL injury predisposing stress [27]. From a variety of core stability tests [45], we selected two symmetrical endurance tests [46] for the flexors and extensors and one performed unilaterally from both sides to ensure a complete multi-dimensional muscle assessment of the thoracic spine, the lumbopelvic hip complex, and the abdomen. We included a hip abductors strength test, which seems to be correlated with non-contact lower limb injury [46]. Most of the functional variables we introduced did not play a role in group separation. This might imply that other tests could be tested in future studies. Despite that, the finding that LESS was a significant predictor of group separation suggests that a more technique-focusing assessment of unilateral landing is fundamental for a proper pre-season ACL injury risk screening.
Muscle fatigue has been suggested to alter landing biomechanics, predisposing the lower limb to ACL injuries [47,48,49,50]. Performance in muscle endurance tests reflects the athlete’s ability to resist fatigue and this was the reason for inclusion of these tests in the PA [27]. It might be useful to include such tests within the criteria for risk-level classification of athletes; however, muscle endurance has not been studied as an ACL injury predictor enough to provide cutoff values, as it applies to thigh muscle strength and hop tests. In the present study, the frontal core muscle endurance performance was a separating variable between high- and low-risk players indicating a direction for future investigation.
It appears that the tested battery of criteria significantly classified players and could be useful for pre-season ACL risk assessment of football players. It was not directly tested for its injury-predictive potential, but the criterion in every single factor was the most widely accepted. Discriminant analysis showed that the overall successful classification was very high. It is important that our test-battery placed players into the low-risk group with higher accuracy than in the high-risk group. Only four players were misplaced in this category. Should the opposite occur, a higher number of them would be falsely considered safe for exposure to unrestricted participation in football, with an increased chance of being injured. A higher proportion of players were misplaced in the high-risk category, which is a possible error towards the safe side, accompanied by extra attention for those who might not need it. A question is raised regarding the approach to prevent these misclassifications. Observation of these particular cases, since the low number would not provide safe statistics, shows that the key variable for further consideration is the LESS score. For the four players that were initially considered safe, but in fact, may need a closer attention, we noticed that their mean functional asymmetries were low, while the LESS score marginally missed the upper limit of six mistakes (5.83). On the contrary, those who entered the high-risk group, but possibly belonged to the other group, had a mean of low LESS scores (4.69). This suggests that a cutoff point of LESS = 5 might lead to an even better risk prediction.
Limitations apply to the current study, starting with its cross-sectional design. Players were assessed and categorized via a composite tool, comprising of separately acknowledged tests, which has not been evaluated as a whole. Its validation needs to be done via a prospective study, which is the next step scheduled. The number of participants, although adequate for the current study, should be increased for a prospective design. In addition, to increase the predictability of this proposed tool, players’ assessments should be updated throughout the season, as values might change with accumulated training, fatigue and injuries. Indeed, continuous screening throughout the season has been proposed for ACL injury prevention [51]. In reality, no model is expected to be entirely sensitive for high injury risk classification of players, since the neuromechanics of the unpredicted dynamic maneuvers in contact, cutting and twisting sports cannot be assessed in detail during field testing, but need more elaborate measures such as surface electromyography [52,53]. To make things worse, an endless list of intrinsic and extrinsic factors influence players’ profiles. Scientists ought to constantly seek additional factors in order to improve understanding of the causal relationships predisposing ACL injury [54], thus producing sensitive and specific prognostic tools.
5. Conclusions
The screening battery of four criteria, comprising asymmetries to the thigh muscle strength, the single-leg triple hop for distance and the landing error scoring system, appeared to classify football players efficiently into the high-risk group for ACL injury. Additional holistic assessment was conducted and LESS and the prone bridge test were significant predictors for risk-group classification, indicating the importance of global body functionality for player screening. It is imperative to test this tool prospectively to identify its actual predictive strength.
Author Contributions
Conceptualization, C.T., N.I.L., S.A.X. and E.T.; methodology, S.A.X., K.F., M.T. and E.T.; validation, C.T. and N.I.L.; formal analysis, E.T.; investigation, C.T. and N.I.L.; data curation, C.T. and N.I.L.; writing—original draft preparation, C.T., N.I.L., S.A.X. and E.T.; writing—review and editing, M.T. and K.F.; visualization, C.T. and N.I.L.; supervision, S.A.X. and E.T.; project administration, S.A.X. and E.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Ethics Committee of the University of Patras-Greece (ID 12126) and is a part of the registered study protocol presented in the public database ClinicalTrials.gov (Identifier: NCT05430581).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy of professional football players’ performance and history of injury information.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Tayfur, B.; Charuphongsa, C.; Morrissey, D.; Miller, S.C. Neuromuscular Function of the Knee Joint Following Knee Injuries: Does It Ever Get Back to Normal? A Systematic Review with Meta-Analyses. Sports Med. 2021, 51, 321–338. [Google Scholar] [CrossRef] [PubMed]
- Ardern, C.L.; Taylor, N.F.; Feller, J.A.; Webster, K.E. Fifty-Five per Cent Return to Competitive Sport Following Anterior Cruciate Ligament Reconstruction Surgery: An Updated Systematic Review and Meta-Analysis Including Aspects of Physical Functioning and Contextual Factors. Br. J. Sports Med. 2014, 48, 1543–1552. [Google Scholar] [CrossRef] [PubMed]
- Wiggins, A.J.; Grandhi, R.K.; Schneider, D.K.; Stanfield, D.; Webster, K.E.; Myer, G.D. Risk of Secondary Injury in Younger Athletes after Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-Analysis. Am. J. Sports Med. 2016, 44, 1861–1876. [Google Scholar] [CrossRef] [PubMed]
- Kessler, M.A.; Behrend, H.; Henz, S.; Stutz, G.; Rukavina, A.; Kuster, M.S. Function, Osteoarthritis and Activity after ACL-Rupture: 11 Years Follow-up Results of Conservative versus Reconstructive Treatment. Knee Surg. Sport. Traumatol. Arthrosc. 2008, 16, 442–448. [Google Scholar] [CrossRef]
- Lie, M.M.; Risberg, M.A.; Storheim, K.; Engebretsen, L.; Øiestad, B.E. What’s the Rate of Knee Osteoarthritis 10 Years after Anterior Cruciate Ligament Injury? An Updated Systematic Review. Br. J. Sports Med. 2019, 53, 1162–1167. [Google Scholar] [CrossRef]
- Kuenze, C.; Pietrosimone, B.; Currie, K.D.; Walton, S.R.; Kerr, Z.Y.; Brett, B.L.; Chandran, A.; DeFreese, J.D.; Mannix, R.; Echemendia, R.J.; et al. Joint Injury and OA Are Associated with Cardiovascular Disease Risk Factors in Former NFL Athletes: An NFL-LONG Study. J. Athl. Train. 2023. [Google Scholar] [CrossRef]
- Padua, D.A.; DiStefano, L.J.; Beutler, A.I.; De La Motte, S.J.; DiStefano, M.J.; Marshall, S.W. The Landing Error Scoring System as a Screening Tool for an Anterior Cruciate Ligament Injury-Prevention Program in Elite-Youth Soccer Athletes. J. Athl. Train. 2015, 50, 589–595. [Google Scholar] [CrossRef]
- Hewett, T.E.; Ford, K.R.; Hoogenboom, B.J.; Myer, G.D. Understanding and Preventing Acl Injuries: Current Biomechanical and Epidemiologic Considerations—Update 2010. N. Am. J. Sports Phys. Ther. 2010, 5, 234–251. [Google Scholar]
- Hewett, T.E.; Myer, G.D.; Ford, K.R.; Heidt, R.S.; Colosimo, A.J.; McLean, S.G.; Van Den Bogert, A.J.; Paterno, M.V.; Succop, P. Biomechanical Measures of Neuromuscular Control and Valgus Loading of the Knee Predict Anterior Cruciate Ligament Injury Risk in Female Athletes: A Prospective Study. Am. J. Sports Med. 2005, 33, 492–501. [Google Scholar] [CrossRef]
- Pappas, E.; Carpes, F.P. Lower Extremity Kinematic Asymmetry in Male and Female Athletes Performing Jump-Landing Tasks. J. Sci. Med. Sport 2012, 15, 87–92. [Google Scholar] [CrossRef]
- Paterno, M.V.; Schmitt, L.C.; Ford, K.R.; Rauh, M.J.; Myer, G.D.; Huang, B.; Hewett, T.E. Biomechanical Measures during Landing and Postural Stability Predict Second Anterior Cruciate Ligament Injury after Anterior Cruciate Ligament Reconstruction and Return to Sport. Am. J. Sports Med. 2010, 38, 1968–1978. [Google Scholar] [CrossRef]
- Paterno, M.V.; Huang, B.; Thomas, S.; Hewett, T.E.; Schmitt, L.C. Clinical Factors That Predict a Second ACL Injury After ACL Reconstruction and Return to Sport: Preliminary Development of a Clinical Decision Algorithm. Orthop. J. Sport. Med. 2017, 5, 2325967117745279. [Google Scholar] [CrossRef] [PubMed]
- Nagelli, C.V.; Hewett, T.E. Should Return to Sport Be Delayed Until 2 Years after Anterior Cruciate Ligament Reconstruction? Biological and Functional Considerations. Sport. Med. 2017, 47, 221–232. [Google Scholar] [CrossRef] [PubMed]
- Morishige, Y.; Harato, K.; Kobayashi, S.; Niki, Y.; Matsumoto, M.; Nakamura, M.; Nagura, T. Difference in Leg Asymmetry between Female Collegiate Athletes and Recreational Athletes during Drop Vertical Jump. J. Orthop. Surg. Res. 2019, 14, 424. [Google Scholar] [CrossRef] [PubMed]
- Guan, Y.; Bredin, S.S.D.; Taunton, J.; Jiang, Q.; Wu, N.; Warburton, D.E.R. Association between Inter-Limb Asymmetries in Lower-Limb Functional Performance and Sport Injury: A Systematic Review of Prospective Cohort Studies. J. Clin. Med. 2022, 11, 360. [Google Scholar] [CrossRef]
- Mendonça, L.D.M. To Do or Not to Do?—The Value of the Preseason Assessment in Sport Injury Prevention. Int. J. Sports Phys. Ther. 2022, 17, 111–113. [Google Scholar] [CrossRef]
- Gokeler, A.; Welling, W.; Zaffagnini, S.; Seil, R.; Padua, D. Development of a Test Battery to Enhance Safe Return to Sports after Anterior Cruciate Ligament Reconstruction. Knee Surg. Sport. Traumatol. Arthrosc. 2017, 25, 192–199. [Google Scholar] [CrossRef]
- Gokeler, A.; Dingenen, B.; Hewett, T.E. Rehabilitation and Return to Sport Testing After Anterior Cruciate Ligament Reconstruction: Where Are We in 2022? Arthrosc. Sport. Med. Rehabil. 2022, 4, e77–e82. [Google Scholar] [CrossRef]
- Everard, E.; Lyons, M.; Harrison, A.J. Examining the Reliability of the Landing Error Scoring System with Raters Using the Standardized Instructions and Scoring Sheet. J. Sport Rehabil. 2020, 29, 519–525. [Google Scholar] [CrossRef]
- Padua, D.A.; Marshall, S.W.; Boling, M.C.; Thigpen, C.A.; Garrett, W.E.; Beutler, A.I. The Landing Error Scoring System (LESS) Is a Valid and Reliable Clinical Assessment Tool of Jump-Landing Biomechanics: The Jump-ACL Study. Am. J. Sports Med. 2009, 37, 1996–2002. [Google Scholar] [CrossRef]
- Whiteley, R.; Jacobsen, P.; Prior, S.; Skazalski, C.; Otten, R.; Johnson, A. Correlation of Isokinetic and Novel Hand-Held Dynamometry Measures of Knee Flexion and Extension Strength Testing. J. Sci. Med. Sport 2012, 15, 444–450. [Google Scholar] [CrossRef]
- Welling, W.; Benjaminse, A.; Lemmink, K.; Gokeler, A. Passing Return to Sports Tests after ACL Reconstruction Is Associated with Greater Likelihood for Return to Sport but Fail to Identify Second Injury Risk. Knee 2020, 27, 949–957. [Google Scholar] [CrossRef]
- van Melick, N.; Pronk, Y.; Nijhuis-van der Sanden, M.; Rutten, S.; van Tienen, T.; Hoogeboom, T. Meeting Movement Quantity or Quality Return to Sport Criteria Is Associated with Reduced Second ACL Injury Rate. J. Orthop. Res. 2022, 40, 117–128. [Google Scholar] [CrossRef] [PubMed]
- Zazulak, B.T.; Hewett, T.E.; Reeves, N.P.; Goldberg, B.; Cholewicki, J. The Effects of Core Proprioception on Knee Injury: A Prospective Biomechanical-Epidemiological Study. Am. J. Sports Med. 2007, 35, 368–373. [Google Scholar] [CrossRef]
- Kibler, W.B.; Press, J.; Sciascia, A. The Role of Core Stability in Athletic Function. Sports Med. 2006, 36, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Wilkerson, G.B.; Giles, J.L.; Seibel, D.K. Prediction of Core and Lower Extremity Strains and Sprains in Collegiate Football Players: A Preliminary Study. J. Athl. Train. 2012, 47, 264–272. [Google Scholar] [CrossRef] [PubMed]
- De Blaiser, C.; Roosen, P.; Willems, T.; De Bleecker, C.; Vermeulen, S.; Danneels, L.; De Ridder, R. The Role of Core Stability in the Development of Non-Contact Acute Lower Extremity Injuries in an Athletic Population: A Prospective Study. Phys. Ther. Sport 2021, 47, 165–172. [Google Scholar] [CrossRef]
- Mehl, J.; Diermeier, T.; Herbst, E.; Imhoff, A.B.; Stoffels, T.; Zantop, T.; Petersen, W.; Achtnich, A. Evidence-Based Concepts for Prevention of Knee and ACL Injuries. 2017 Guidelines of the Ligament Committee of the German Knee Society (DKG). Arch. Orthop. Trauma Surg. 2018, 138, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE). Epidemiology 2007, 18, 805–835. [Google Scholar] [CrossRef]
- Pasanen, K.; Rossi, M.T.; Parkkari, J.; Heinonen, A.; Steffen, K.; Myklebust, G.; Krosshaug, T.; Vasankari, T.; Kannus, P.; Avela, J.; et al. Predictors of Lower Extremity Injuries in Team Sports (PROFITS-Study): A Study Protocol. BMJ Open Sport Exerc. Med. 2017, 1, e000076. [Google Scholar] [CrossRef]
- Stark, T.; Walker, B.; Phillips, J.K.; Fejer, R.; Beck, R. Hand-Held Dynamometry Correlation with the Gold Standard Isokinetic Dynamometry: A Systematic Review. PM&R 2011, 3, 472–479. [Google Scholar] [CrossRef]
- Hansen, E.M.; McCartney, C.N.; Sweeney, R.S.; Palimenio, M.R.; Grindstaff, T.L. Hand-Held Dynamometer Positioning Impacts Discomfort During Quadriceps Strength Testing: A Validity and Reliability Study. Int. J. Sports Phys. Ther. 2015, 10, 62–68. [Google Scholar]
- Whiteley, R.; van Dyk, N.; Wangensteen, A.; Hansen, C. Clinical Implications from Daily Physiotherapy Examination of 131 Acute Hamstring Injuries and Their Association with Running Speed and Rehabilitation Progression. Br. J. Sports Med. 2018, 52, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Goossens, L.; Witvrouw, E.; Vanden Bossche, L.; De Clercq, D. Lower Eccentric Hamstring Strength and Single Leg Hop for Distance Predict Hamstring Injury in PETE Students. Eur. J. Sport Sci. 2015, 15, 436–442. [Google Scholar] [CrossRef] [PubMed]
- Thorborg, K.; Petersen, J.; Magnusson, S.P.; Hölmich, P. Clinical Assessment of Hip Strength Using a Hand-Held Dynamometer Is Reliable. Scand. J. Med. Sci. Sports 2010, 20, 493–501. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.; Squillante, A.; Dawes, J. The Single Leg Triple Hop for Distance Test. Strength Cond. J. 2017, 39, 94–98. [Google Scholar] [CrossRef]
- Hamilton, R.T.; Shultz, S.J.; Schmitz, R.J.; Perrin, D.H. Triple-Hop Distance as a Valid Predictor of Lower Limb Strength and Power. J. Athl. Train. 2008, 43, 144–151. [Google Scholar] [CrossRef]
- Smith, H.C.; Johnson, R.J.; Shultz, S.J.; Tourville, T.; Holterman, L.A.; Slauterbeck, J.; Vacek, P.M.; Beynnon, B.D. A Prospective Evaluation of the Landing Error Scoring System (LESS) as a Screening Tool for Anterior Cruciate Ligament Injury Risk. Am. J. Sports Med. 2012, 40, 521–526. [Google Scholar] [CrossRef] [PubMed]
- Liveris, N.I.; Tsarbou, C.; Tsimeas, P.D.; Papageorgiou, G.; Xergia, S.A.; Tsiokanos, A. Evaluating the Effects of Match-Induced Fatigue on Landing Ability; the Case of the Basketball Game. Int. J. Exerc. Sci. 2021, 14, 768–778. [Google Scholar]
- Tsarbou, C.; Liveris, N.I.; Tsimeas, P.D.; Papageorgiou, G.; Xergia, S.A.; Tsiokanos, A. The Effect of Fatigue on Jump Height and the Risk of Knee Injury after a Volleyball Training Game: A Pilot Study. Biomed. Hum. Kinet. 2021, 13, 197–204. [Google Scholar] [CrossRef]
- De Blaiser, C.; De Ridder, R.; Willems, T.; Danneels, L.; Vanden Bossche, L.; Palmans, T.; Roosen, P. Evaluating Abdominal Core Muscle Fatigue: Assessment of the Validity and Reliability of the Prone Bridging Test. Scand. J. Med. Sci. Sports 2018, 28, 391–399. [Google Scholar] [CrossRef]
- McGill, S.M.; Childs, A.; Liebenson, C. Endurance Times for Low Back Stabilization Exercises: Clinical Targets for Testing and Training from a Normal Database. Arch. Phys. Med. Rehabil. 1999, 80, 941–944. [Google Scholar] [CrossRef] [PubMed]
- Coorevits, P.; Danneels, L.; Cambier, D.; Ramon, H.; Vanderstraeten, G. Assessment of the Validity of the Biering-Sørensen Test for Measuring Back Muscle Fatigue Based on EMG Median Frequency Characteristics of Back and Hip Muscles. J. Electromyogr. Kinesiol. 2008, 18, 997–1005. [Google Scholar] [CrossRef] [PubMed]
- Markström, J.L.; Naili, J.E.; Häger, C.K. A Minority of Athletes Pass Symmetry Criteria in a Series of Hop and Strength Tests Irrespective of Having an ACL Reconstructed Knee or Being Noninjured. Sports Health 2022, 15, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Waldhelm, A.; Li, L. Endurance Tests Are the Most Reliable Core Stability Related Measurements. J. Sport Health Sci. 2012, 1, 121–128. [Google Scholar] [CrossRef]
- De Blaiser, C.; Roosen, P.; Willems, T.; Danneels, L.; Bossche, L.V.; De Ridder, R. Is Core Stability a Risk Factor for Lower Extremity Injuries in an Athletic Population? A Systematic Review. Phys. Ther. Sport 2018, 30, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Wesley, C.A.; Aronson, P.A.; Docherty, C.L. Lower Extremity Landing Biomechanics in Both Sexes after a Functional Exercise Protocol. J. Athl. Train. 2015, 50, 914–920. [Google Scholar] [CrossRef]
- Zhang, X.; Xia, R.; Dai, B.; Sun, X.; Fu, W. Effects of Exercise-Induced Fatigue on Lower Extremity Joint Mechanics, Stiffness, and Energy Absorption during Landings. J. Sport. Sci. Med. 2018, 17, 640–649. [Google Scholar]
- Liederbach, M.; Kremenic, I.J.; Orishimo, K.F.; Pappas, E.; Hagins, M. Comparison of Landing Biomechanics between Male and Female Dancers and Athletes, Part 2: Influence of Fatigue and Implications for Anterior Cruciate Ligament Injury. Am. J. Sports Med. 2014, 42, 1089–1095. [Google Scholar] [CrossRef]
- O’Connor, K.M.; Johnson, C.; Benson, L.C. The Effect of Isolated Hamstrings Fatigue on Landing and Cutting Mechanics. J. Appl. Biomech. 2015, 31, 211–220. [Google Scholar] [CrossRef]
- Fonseca, S.T.; Souza, T.R.; Verhagen, E.; van Emmerik, R.; Bittencourt, N.F.N.; Mendonça, L.D.M.; Andrade, A.G.P.; Resende, R.A.; Ocarino, J.M. Sports Injury Forecasting and Complexity: A Synergetic Approach. Sport. Med. 2020, 50, 1757–1770. [Google Scholar] [CrossRef] [PubMed]
- Marotta, N.; Demeco, A.; de Scorpio, G.; Indino, A.; Iona, T.; Ammendolia, A. Late Activation of the Vastus Medialis in Determining the Risk of Anterior Cruciate Ligament Injury in Soccer Players. J. Sport Rehabil. 2020, 29, 952–955. [Google Scholar] [CrossRef] [PubMed]
- Zebis, M.K.; Andersen, L.L.; Bencke, J.; Kjær, M.; Aagaard, P. Identification of Athletes at Future Risk of Anterior Cruciate Ligament Ruptures by Neuromuscular Screening. Am. J. Sports Med. 2009, 37, 1967–1973. [Google Scholar] [CrossRef] [PubMed]
- Bittencourt, N.F.N.; Meeuwisse, W.H.; Mendonça, L.D.; Nettel-Aguirre, A.; Ocarino, J.M.; Fonseca, S.T. Complex Systems Approach for Sports Injuries: Moving from Risk Factor Identification to Injury Pattern Recognition—Narrative Review and New Concept. Br. J. Sports Med. 2016, 50, 1309–1314. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).