Does Anterior Cruciate Ligament Reconstruction with a Hamstring Tendon Autograft Predispose to a Knee Valgus Alignment on Initial Contact during Landing? A Drop Vertical Jump Movement Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Experimental Setup
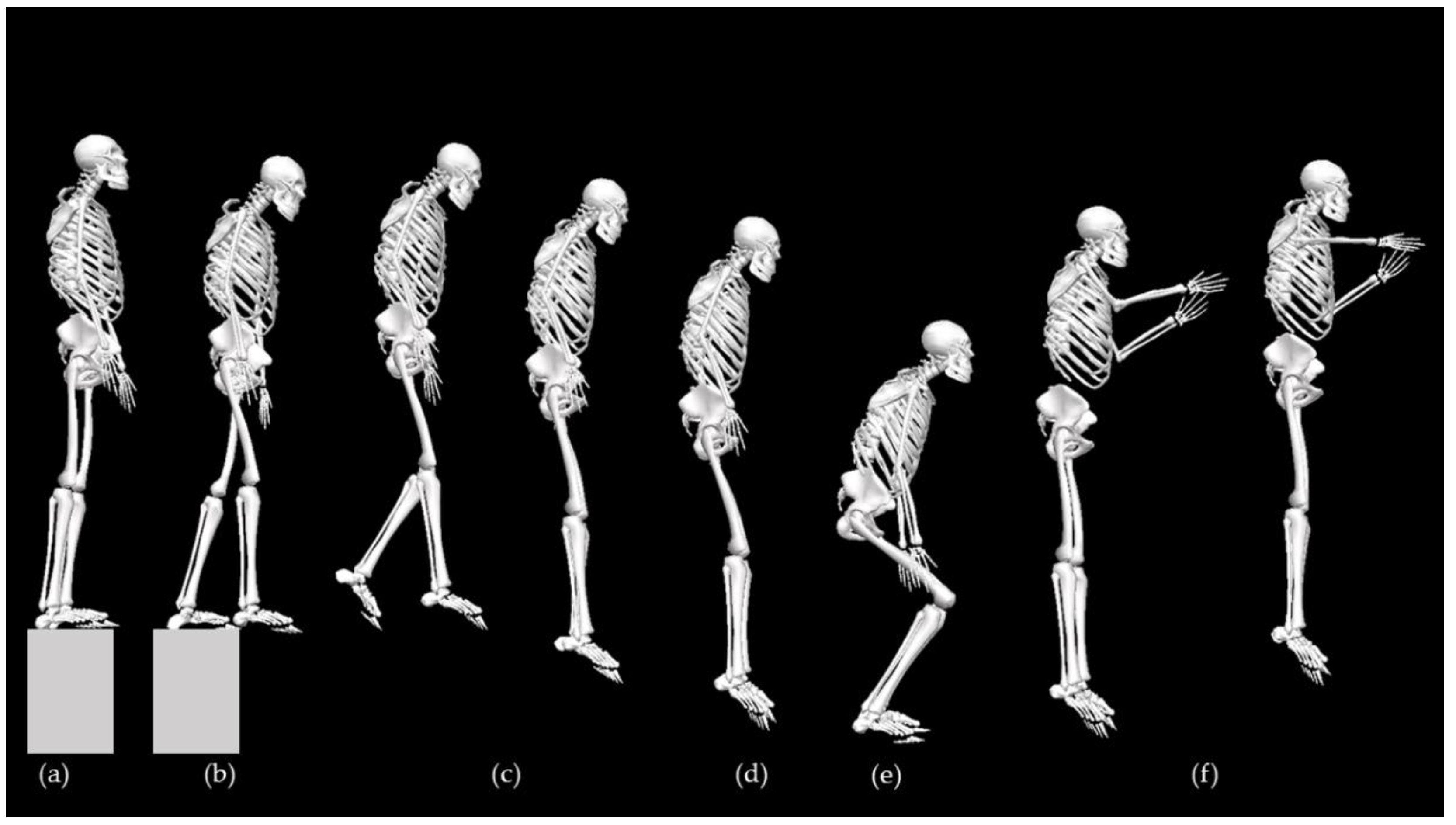
2.3. Experimental Procedure
2.4. Data Processing
2.5. Statistical Analysis
3. Results
4. Discussion
4.1. Peak Knee Valgus
4.2. Peak vGRF
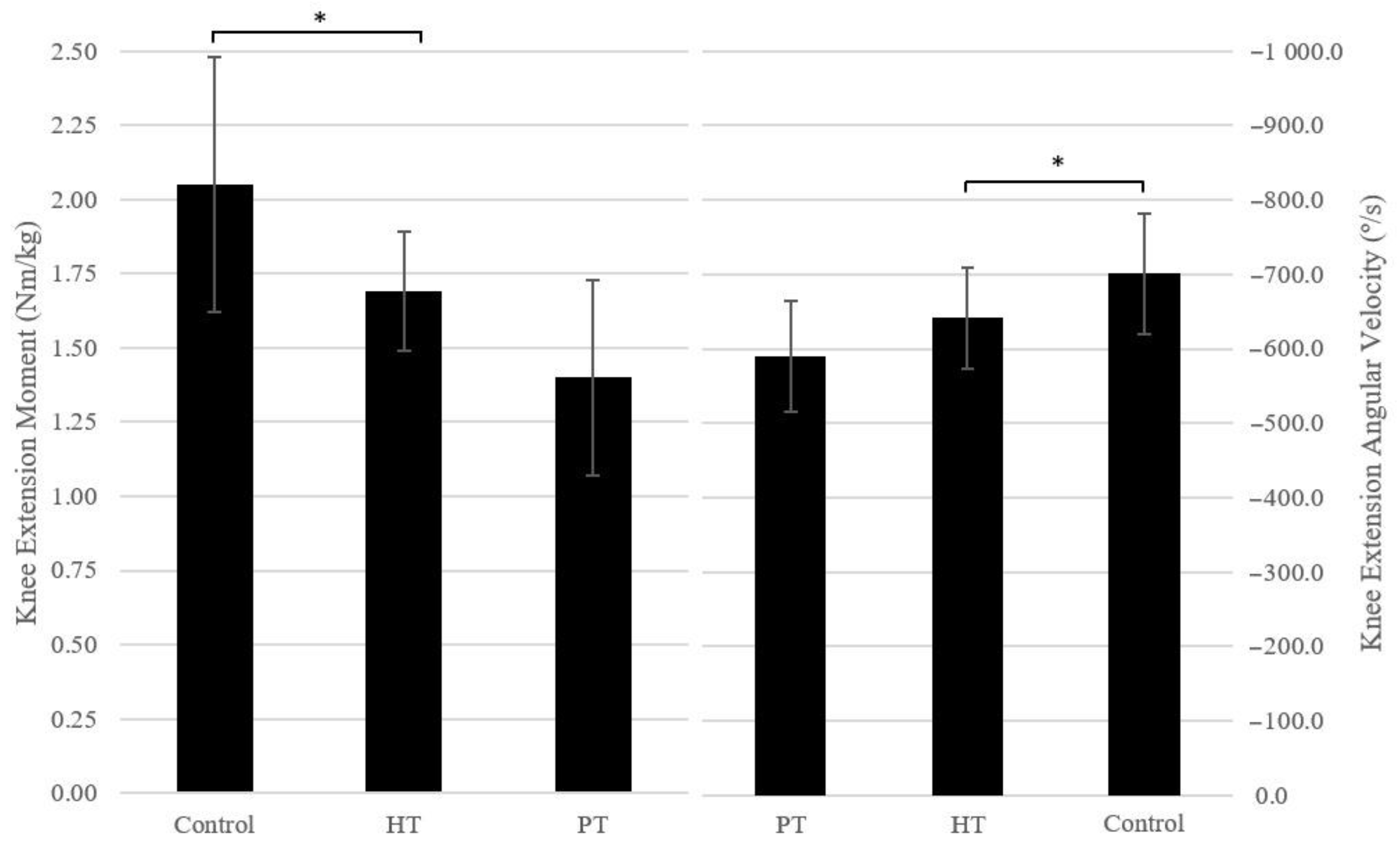
4.3. Knee Extension Angular Moment and Angular Velocity
4.4. Clinical Implications
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kohn, L.; Rembeck, E.; Rauch, A. [Anterior cruciate ligament injury in adults: Diagnostics and treatment]. Orthopade 2020, 49, 1013–1028. [Google Scholar] [CrossRef]
- Sepúlveda, F.; Sánchez, L.; Amy, E.; Micheo, W. Anterior Cruciate Ligament Injury: Return to Play, Function and Long-Term Considerations. Curr. Sports Med. Rep. 2017, 16, 172–178. [Google Scholar] [CrossRef]
- Mall, N.A.; Chalmers, P.N.; Moric, M.; Tanaka, M.J.; Cole, B.J.; Bach, B.R.; Paletta, G.A. Incidence and Trends of Anterior Cruciate Ligament Reconstruction in the United States. Am. J. Sports Med. 2014, 42, 2363–2370. [Google Scholar] [CrossRef]
- Siegel, L.; Vandenakker-Albanese, C.; Siegel, D. Anterior cruciate ligament injuries: Anatomy, physiology, biomechanics, and management. Clin. J. Sport Med. 2012, 22, 349–355. [Google Scholar] [CrossRef]
- Mizuta, H.; Kubota, K.; Shiraishi, M.; Otsuka, Y.; Nagamoto, N.; Takagi, K. The conservative treatment of complete tears of the anterior cruciate ligament in skeletally immature patients. J. Bone Jt. Surg. 1995, 77, 890–894. [Google Scholar] [CrossRef]
- Stone, A.V.; Marx, S.; Conley, C.W. Management of Partial Tears of the Anterior Cruciate Ligament: A Review of the Anatomy, Diagnosis, and Treatment. J. Am. Acad. Orthop. Surg. 2021, 29, 60–70. [Google Scholar] [CrossRef]
- Paschos, N.K.; Howell, S.M. Anterior cruciate ligament reconstruction: Principles of treatment. EFORT Open Rev. 2016, 1, 398–408. [Google Scholar] [CrossRef]
- Tibor, L.; Chan, P.H.; Funahashi, T.T.; Wyatt, R.; Maletis, G.B.; Inacio, M.C. Surgical Technique Trends in Primary ACL Reconstruction from 2007 to 2014. J. Bone Jt. Surg. 2016, 98, 1079–1089. [Google Scholar] [CrossRef] [PubMed]
- Rahr-Wagner, L.; Thillemann, T.M.; Pederson, A.B.; Lind, M. Comparison of hamstring tendon and patellar tendon grafts in anterior cruciate ligament reconstruction in a nationwide population-based cohort study: Results from the Danish registry of knee ligament reconstruction. Am. J. Sport Med. 2014, 42, 278–284. [Google Scholar] [CrossRef] [PubMed]
- Xie, X.; Liu, X.; Chen, Z.; Yu, Y.; Peng, S.; Li, Q. A meta-analysis of bone–patellar tendon–bone autograft versus four-strand hamstring tendon autograft for anterior cruciate ligament reconstruction. Knee 2015, 22, 100–110. [Google Scholar] [CrossRef] [PubMed]
- Mohtadi, N.G.; Chan, D.S.; Dainty, K.N.; Whelan, D.B. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst. Rev. 2011, 2011, CD005960. [Google Scholar] [CrossRef]
- Samuelsen, B.T.; Webster, K.E.; Johnson, N.R.; Hewett, T.E.; Krych, A.J. Hamstring Autograft versus Patellar Tendon Autograft for ACL Reconstruction: Is There a Difference in Graft Failure Rate? A Meta-analysis of 47,613 Patients. Clin. Orthop. Relat. Res. 2017, 475, 2459–2468. [Google Scholar] [CrossRef]
- Asaeda, M.; Nakamae, A.; Hirata, K.; Kono, Y.; Uenishi, H.; Adachi, N. Factors associated with dynamic knee valgus angle during single-leg forward landing in patients after anterior cruciate ligament reconstruction. Asia-Pac. J. Sport Med. Arthrosc. Rehabil. Technol. 2020, 22, 56–61. [Google Scholar] [CrossRef]
- Hardy, A.; Casabianca, L.; Andrieu, K.; Baverel, L.; Noailles, T.; Junior French Arthroscopy Society. Complications following harvesting of patellar tendon or hamstring tendon grafts for anterior cruciate ligament reconstruction: Systematic review of literature. Orthop. Traumatol. Surg. Res. 2017, 103, S245–S248. [Google Scholar] [PubMed]
- Muro-De-La-Herran, A.; Garcia-Zapirain, B.; Mendez-Zorrilla, A. Gait Analysis Methods: An Overview of Wearable and Non-Wearable Systems, Highlighting Clinical Applications. Sensors 2014, 14, 3362–3394. [Google Scholar] [CrossRef] [PubMed]
- Kollias, I.; Panoutsakopoulos, V.; Papaiakovou, G. Comparing Jumping Ability among Athletes of Various Sports: Vertical Drop Jumping from 60 Centimeters. J. Strength Cond. Res. 2004, 18, 546–550. [Google Scholar]
- Paz, G.A.; de Freitas Maia, M.; Farias, D.; Santana, H.; Miranda, H.; Lima, V.; Herrington, L. Kinematic Analysis Of Knee Valgus During Drop Vertical Jump And Forward Step-Up In Young Basketball Players. Int. J. Sports Phys. Ther. 2016, 11, 212–219. [Google Scholar] [PubMed]
- Castro, M.; Fonseca, P.; Paiotti, F.; Pocinho, M.; Carvalho, D.; Vinha, E.; Vilas-Boas, J. Gait characteristics in people with diabetes classified in risk categories 0 and 2 of the IWGDF—International Working Group on the Diabetic Foot. Rev. Port. Endocrinol. Diabetes Metab. 2022, 16, 104–109. [Google Scholar] [CrossRef]
- Sousa, M.V.; Sebastião, R.; Fonseca, P.; Morais, S.; Soares, D.; de Sousa, I.; Machado, L.; Sousa, F.; Vaz, M.; Vilas-Boas, J.P. Can increased load carriage affect lower limbs kinematics during military gait? Ergonomics 2022, 65, 1194–1201. [Google Scholar] [CrossRef]
- Vilas-Boas, M.D.C.; Fonseca, P.F.P.; Sousa, I.M.; Cardoso, M.N.; Cunha, J.P.S.; Coelho, T. Gait Characterization and Analysis of Hereditary Amyloidosis Associated with Transthyretin Patients: A Case Series. J. Clin. Med. 2022, 11, 3967. [Google Scholar] [CrossRef]
- Kessler, S.E.; Rainbow, M.J.; Lichtwark, G.A.; Cresswell, A.G.; D’Andrea, S.E.; Konow, N.; Kelly, L.A. A Direct Comparison of Biplanar Videoradiography and Optical Motion Capture for Foot and Ankle Kinematics. Front. Bioeng. Biotechnol. 2019, 7, 199. [Google Scholar] [CrossRef] [PubMed]
- Kanko, R.M.; Laende, E.; Selbie, W.S.; Deluzio, K.J. Inter-session repeatability of markerless motion capture gait kinematics. J. Biomech. 2021, 121, 110422. [Google Scholar] [CrossRef] [PubMed]
- Kanko, R.M.; Laende, E.K.; Davis, E.M.; Selbie, W.S.; Deluzio, K.J. Concurrent assessment of gait kinematics using marker-based and markerless motion capture. J. Biomech. 2021, 127, 110665. [Google Scholar] [CrossRef] [PubMed]
- Kanko, R.M.; Laende, E.K.; Strutzenberger, G.; Brown, M.; Selbie, W.S.; DePaul, V.; Scott, S.H.; Deluzio, K.J. Assessment of spatiotemporal gait parameters using a deep learning algorithm-based markerless motion capture system. J. Biomech. 2021, 122, 110414. [Google Scholar] [CrossRef]
- Drazan, J.F.; Phillips, W.T.; Seethapathi, N.; Hullfish, T.J.; Baxter, J.R. Moving outside the lab: Markerless motion capture accurately quantifies sagittal plane kinematics during the vertical jump. J. Biomech. 2021, 125, 110547. [Google Scholar] [CrossRef]
- Hewett, T.E.; Myer, G.D.; Ford, K.R.; Heidt, R.S., Jr.; Colosimo, A.J.; McLean, S.G.; van Den Bogert, A.J.; Paterno, M.V.; Succop, P. Biomechanical Measures of Neuromuscular Control and Valgus Loading of the Knee Predict Anterior Cruciate Ligament Injury Risk in Female Athletes: A Prospective Study. Am. J. Sports Med. 2005, 33, 492–501. [Google Scholar] [CrossRef]
- Kobayashi, H.; Kanamura, T.; Koshida, S.; Miyashita, K.; Okado, T.; Shimizu, T.; Yokoe, K. Mechanisms of the anterior cruciate ligament injury in sports activities: A twenty-year clinical research of 1700 athletes. J. Sports Sci. Med. 2010, 9, 669–675. [Google Scholar]
- Shapiro, S.S.; Wilk, M.B. An Analysis of Variance Test for Normality (Complete Samples). Biometrika 1965, 52, 591–611. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Herbort, M.; Michel, P.; Raschke, M.J.; Vogel, N.; Schulze, M.; Zoll, A.; Fink, C.; Peterson, W.; Domnick, C. Should the Ipsilateral Hamstrings Be Used for Anterior Cruciate Ligament Reconstruction in the Case of Medial Collateral Ligament Insufficiency? Biomechanical Investigation Regarding Dynamic Stabilization of the Medial Compartment by the Hamstring Muscles. Am. J. Sports Med. 2017, 45, 819–825. [Google Scholar]
- Kimura, Y.; Ishibashi, Y.; Tsuda, E.; Yamamoto, Y.; Hayashi, Y.; Sato, S. Increased knee valgus alignment and moment during single-leg landing after overhead stroke as a potential risk factor of anterior cruciate ligament injury in badminton. Br. J. Sports Med. 2012, 46, 207–213. [Google Scholar] [CrossRef]
- Sasaki, S.; Tsuda, E.; Yamamoto, Y.; Maeda, S.; Kimura, Y.; Fujita, Y.; Ishibashi, Y. Core-Muscle Training and Neuromuscular Control of the Lower Limb and Trunk. J. Athl. Train. 2019, 54, 959–969. [Google Scholar] [CrossRef] [PubMed]
- Baumgart, C.; Hoppe, M.W.; Freiwald, J. Phase-Specific Ground Reaction Force Analyses of Bilateral and Unilateral Jumps in Patients With ACL Reconstruction. Orthop. J. Sports Med. 2017, 5, 2325967117710912. [Google Scholar] [CrossRef] [PubMed]
- Gokeler, A.; Hof, A.; Arnold, M.P.; Dijkstra, P.U.; Postema, K.; Otten, E. Abnormal landing strategies after ACL reconstruction. Scand. J. Med. Sci. Sports 2010, 20, e12–e19. [Google Scholar] [CrossRef]
- Baumgart, C.; Schubert, M.; Hoppe, M.W.; Gokeler, A.; Freiwald, J. Do ground reaction forces during unilateral and bilateral movements exhibit compensation strategies following ACL reconstruction? Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 1385–1394. [Google Scholar] [CrossRef]
- Jordan, M.J.; Aagaard, P.; Herzog, W. Lower limb asymmetry in mechanical muscle function: A comparison between ski racers with and without ACL reconstruction. Scand. J. Med. Sci. Sports 2015, 25, e301–e309. [Google Scholar] [CrossRef]
- Hahn, D.; Herzog, W.; Schwirtz, A. Interdependence of torque, joint angle, angular velocity and muscle action during human multi-joint leg extension. Eur. J. Appl. Physiol. 2014, 114, 1691–1702. [Google Scholar] [CrossRef]
- Stone, W.J.; Arnett, S.W.; Hoover, D.L. Lower Extremity Kinematics of Acl-Repaired and Non-Injured Females When Using Knee Savers®. Int. J. Sports Phys. Ther. 2017, 12, 737–746. [Google Scholar] [CrossRef]
- Orishimo, K.F.; Kremenic, I.J.; Mullaney, M.J.; McHugh, M.P.; Nicholas, S.J. Adaptations in single-leg hop biomechanics following anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 1587–1593. [Google Scholar] [CrossRef]
- Aune, A.K.; Holm, I.; Risberg, M.A.; Jensen, H.K.; Steen, H. Four-Strand Hamstring Tendon Autograft Compared with Patellar Tendon-Bone Autograft for Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med. 2001, 29, 722–728. [Google Scholar] [CrossRef] [PubMed]
- Heijne, A.; Werner, S. A 2-year follow-up of rehabilitation after ACL reconstruction using patellar tendon or hamstring tendon grafts: A prospective randomised outcome study. Knee Surgery, Sports Traumatol. Arthrosc. 2009, 18, 805–813. [Google Scholar] [CrossRef]
- Ardern, C.L.; Bizzini, M.; Bahr, R. It is time for consensus on return to play after injury: Five key questions. Br. J. Sports Med. 2015, 50, 506–508. [Google Scholar] [CrossRef] [PubMed]
- Barber-Westin, S.D.; Noyes, F.R. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy 2011, 27, 1697–1705. [Google Scholar] [CrossRef] [PubMed]
- Hildebrandt, C.; Müller, L.; Zisch, B.; Huber, R.; Fink, C.; Raschner, C. Functional assessments for decision-making regarding return to sports following ACL reconstruction. Part I: Development of a new test battery. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 1273–1281. [Google Scholar] [PubMed]
- Ryan, J.; Magnussen, R.A.; Cox, C.; Hurbanek, J.G.; Flanigan, D.C.; Kaeding, C.C. ACL reconstruction: Do outcomes differ by sex?: A systematic review. JBJS 2014, 96, 507–512. [Google Scholar] [CrossRef] [PubMed]
- Eshuis, R.; Lentjes, G.W.; Tegner, Y.; Wolterbeek, N.; Veen, M.R. Dutch Translation and Cross-cultural Adaptation of the Lysholm Score and Tegner Activity Scale for Patients With Anterior Cruciate Ligament Injuries. J. Orthop. Sports Phys. Ther. 2016, 46, 976–983. [Google Scholar] [CrossRef]
| Group | Control vs. Case Group | Autograft | Control vs. HT Autograft | Control vs. PT Autograft | HT vs. PT Autograft | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Parameter | Control (n = 11) | Case (n = 14) | p | MD ± SD | HT (n = 8) | PT (n = 6) | p | M ± SD | p | MD ± SD) | p | MD ± SD |
| Age (years) | 29.40 ± 7.37 | 36.93 ± 8.19 | 0.031 * | −7.53 ± 3.26 | 39.75 ± 6.34 | 33.17 ± 9.41 | 0.027 * | −10.35 ± 3.60 | 1.000 | −3.77 ± 3.92 | 0.371 | 6.58 ± 4.10 |
| Height (cm) | 169.50 ± 6.12 | 175.07 ± 7.38 | 0.056 | −5.57 ± 2.77 | 176.25 ± 3.65 | 173.50 ± 10. 86 | 0.144 | −6.75 ± 3.22 | 0.804 | −4.00 ± 3.52 | 1.000 | 2.75 ± 3.74 |
| Mass (kg) | 69.78 ± 9.66 | 83.16 ± 16.54 | 0.026 * | −13.38 ± 5.63 | 84.73 ± 10.07 | 81.08 ± 23.67 | 0.102 | −14.94 ± 6.60 | 0.394 | −11.30 ± 7.21 | 1.000 | 3.64 ± 7.68 |
| BMI (kg/m2) | 24.25 ± 2.79 | 26.92 ± 3.42 | 0.047 * | −2.67 ± 1.27 | 27.28 ± 3.17 | 26.44 ± 3.99 | 0.165 | −3.03 ± 1.49 | 0.577 | −2.20 ± 1.63 | 1.000 | 0.84 ± 1.74 |
| Time since surgery (years) | - | 4.14 ± 1.66 | - | - | 4.13 ± 1.89 | 4.17 ± 1.47 | - | - | - | - | 0.965 | −0.04 ± 0.93 |
| Units | Control Group | Case Group | p | MD ± SD | |
|---|---|---|---|---|---|
| Touch Down | |||||
| Thorax Flexion | deg | 19.91 ± 9.53 | 24.04 ± 8.07 | 0.253 | −4.13 ± 3.52 |
| Hip Flexion | deg | 16.94 ± 16.65 | 12.04 ± 13.02 | 0.354 | 4.90 ± 5.18 |
| Knee Flexion | deg | 25.73 ± 12.99 | 23.56 ± 19.93 | 0.758 | 2.17 ± 6.95 |
| Deepest Position | |||||
| Max Hip Extension Torque | Nm/kg | 1.12 ± 0.53 | 1.13 ± 0.36 | 0.954 | −0.01 ± 0.18 |
| Max Knee Extension Torque | Nm/kg | 1.49 ± 0.83 | 1.39 ± 0.38 | 0.697 | 0.10 ± 0.25 |
| Max Ankle Extension Torque | Nm/kg | 1.20 ± 0.71 | 0.86 ± 0.33 | 0.124 | 0.34 ± 0.21 |
| Max Knee Valgus Torque | Nm/kg | −0.06 ± 0.27 | −0.79 ± 2.83 | 0.402 | 0.74 ± 0.86 |
| General | |||||
| Jump Height | cm | 22.28 ± 6.47 | 22.29 ± 3.81 | 0.995 | −0.01 ± 2.07 |
| Depth of countermovement | cm | 24.82 ± 6.74 | 24.93 ± 5.84 | 0.964 | −0.11 ± 2.42 |
| Max Hip Flexion | deg | 54.10 ± 25.02 | 66.92 ± 13.98 | 0.117 | −12.82 ± 7.88 |
| Max Knee Flexion | deg | 80.01 ± 25.03 | 92.04 ± 13.38 | 0.136 | −12.03 ± 7.79 |
| Max Ankle Flexion | deg | 27.85 ± 7.30 | 29.28 ± 4.35 | 0.550 | −1.42 ± 2.34 |
| Peak vGRF | N/kg | 20.11 ± 6.29 | 15.44 ± 4.97 | 0.049 * | 4.67 ± 2.25 |
| Hip Rotation at IC | deg | −4.54 ± 3.79 | −5.94 ± 3.11 | 0.321 | 1.40 ± 1.38 |
| Knee Flexion at IC | deg | 25.73 ± 13.99 | 23.56 ± 19.93 | 0.758 | 2.17 ± 6.95 |
| Knee Valgus at IC | deg | −0.69 ± 3.98 | 1.36 ± 3.87 | 0.198 | −2.05 ± 1.54 |
| Peak Foot/Pelvis Angle | deg | −7.97 ± 12.63 | −9.17 ± 4.72 | 0.745 | 1.20 ± 3.65 |
| At Peak Knee Valgus | |||||
| Max Knee Valgus | deg | 1.86 ± 3.97 | 4.00 ± 3.84 | 0.187 | −2.14 ± 1.57 |
| Max Knee Flexion | deg | 42.31 ± 32.80 | 52.60 ± 26.38 | 0.393 | −10.29 ± 11.82 |
| Max Knee Rotation | deg | −11.11 ± 4.79 | −12.15 ± 4.95 | 0.601 | 1.04 ± 1.97 |
| Angular Moments | |||||
| Knee Extension | Nm/kg | 2.05 ± 0.43 | 1.57 ± 0.30 | 0.003 * | 0.48 ± 0.14 |
| Knee Flexion | Nm/kg | −0.26 ± 0.19 | −0.14 ± 0.12 | 0.067 | −0.12 ± 0.06 |
| Knee Valgus | Nm/kg | 0.29 ± 0.22 | 0.24 ± 0.12 | 0.413 | 0.06 ± 0.07 |
| Knee Varus | Nm/kg | −0.23 ± 0.20 | −0.19 ± 0.08 | 0.459 | −0.04 ± 0.06 |
| Angular Velocities | |||||
| Knee Extension | deg/s | −701.06 ± 80.94 | −619.22 ± 72.91 | 0.014 * | −81.84 ± 30.82 |
| Knee Flexion | deg/s | 517.84 ± 78.64 | 498.83 ± 96.79 | 0.601 | 19.01 ± 36.00 |
| Control vs. HT Autograft | Control vs. PT Autograft | HT vs. PT Autograft | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Units | Control Group | HT Autograft | PT Autograft | p | MD ± SD | p | MD ± SD | p | MD ± SD | |
| Touch Down | ||||||||||
| Thorax Flexion | deg | 19.91 ± 9.53 | 27.24 ± 4.87 | 19.77 ± 9.90 | 0.224 | −7.33 ± 3.92 | 1.000 | 0.14 ± 4.23 | 0.345 | 7.47 ± 4.55 |
| Hip Flexion | deg | 16.94 ± 12.65 | 11.25 ± 14.45 | 13.08 ± 12.08 | 1.000 | 5.69 ± 6.10 | 1.000 | 3.85 ± 6.66 | 1.000 | −1.83 ± 7.09 |
| Knee Flexion | deg | 25.73 ± 12.99 | 25.71 ± 24.49 | 20.68 ± 13.28 | 1.000 | 0.01 ± 8.15 | 1.000 | 5.04 ± 8.90 | 1.000 | 5.03 ± 9.47 |
| Deepest Position | ||||||||||
| Max Hip Extension Torque | Nm/kg | 1.12 ± 0.53 | 1.09 ± 0.32 | 1.18 ± 0.44 | 1.000 | 0.03 ± 0.21 | 1.000 | −0.07 ± 0.23 | 1.000 | −0.10 ± 0.24 |
| Max Knee Extension Torque | Nm/kg | 1.49 ± 0.83 | 1.51 ± 0.44 | 1.23 ± 0.23 | 1.000 | −0.02 ± 0.29 | 1.000 | 0.26 ± 0.32 | 1.000 | 0.28 ± 0.34 |
| Max Ankle Extension Torque | Nm/kg | 1.20 ± 0.71 | 0.90 ± 0.37 | 0.82 ± 0.31 | 0.710 | 0.31 ± 0.25 | 0.511 | 0.39 ± 0.27 | 1.000 | 0.08 ± 0.29 |
| Max Knee Valgus Torque | Nm/kg | −0.06 ± 0.27 | −1.33 ± 3.76 | −0.08 ± 0.11 | 0.638 | 1.27 ± 1.08 | 1.000 | 0.02 ± 1.08 | 0.868 | −1.25 ± 1.15 |
| General | ||||||||||
| Jump Height | cm | 22.28 ± 6.47 | 22.50 ± 4.11 | 22.00 ± 3.74 | 1.000 | −0.23 ± 2.44 | 1.000 | 0.27 ± 2.66 | 1.000 | 0.50 ± 2.83 |
| Depth of countermovement | cm | 24.82 ± 6.74 | 23.88 ± 6.38 | 26.33 ± 3.78 | 1.000 | 0.94 ± 2.82 | 1.000 | −1.52 ± 3.08 | 1.000 | −2.46 ± 3.28 |
| Max Hip Flexion | deg | 54.10 ± 25.02 | 62.96 ± 14.57 | 72.20 ± 12.36 | 1.000 | −8.86 ± 9.14 | 0.250 | −18.10 ± 9.98 | 1.000 | −9.24 ± 10.62 |
| Max Knee Flexion | deg | 80.01 ± 25.03 | 89.76 ± 15.08 | 95.08 ± 11.30 | 0.891 | −9.75 ± 9.13 | 0.434 | −15.07 ± 9.97 | 1.000 | −5.32 ± 10.61 |
| Max Ankle Flexion | deg | 27.85 ± 7.30 | 28.85 ± 5.70 | 29.85 ± 1.75 | 1.000 | −0.99 ± 2.76 | 1.000 | −2.00 ± 3.01 | 1.000 | −1.00 ± 3.21 |
| Peak vGRF | N/kg | 20.11 ± 6.29 | 16.33 ± 5.72 | 14.26 ± 3.94 | 0.492 | −3.78 ± 2.62 | 0.161 | 5.85 ± 2.87 | 1.000 | 2.07 ± 3.05 |
| Hip Rotation at IC | deg | −4.54 ± 3.79 | −7.23 ± 2.98 | −4.22 ± 2.54 | 0.278 | 2.69 ± 1.53 | 1.000 | −0.32 ± 1.67 | 0.315 | −3.01 ± 1.78 |
| Knee Flexion at IC | deg | 25.73 ± 13.99 | 25.71 ± 24.49 | 20.68 ± 13.28 | 1.000 | 0.01 ± 8.15 | 1.000 | 5.04 ± 8.90 | 1.000 | 5.03 ± 9.47 |
| Knee Valgus at IC | deg | −0.69 ± 3.98 | 2.28 ± 4.84 | 1.33 ± 1.74 | 0.329 | −2.97 ± 1.78 | 1.000 | −0.82 ± 1.94 | 0.935 | 2.14 ± 2.07 |
| Peak Foot/Pelvis Angle | deg | −7.97 ± 12.63 | −10.49 ± 5.03 | −7.40 ± 4.00 | 1.000 | 2.53 ± 4.26 | 1.000 | −0.57 ± 4.66 | 1.000 | −3.09 ± 4.96 |
| At Peak Knee Valgus | ||||||||||
| Max Knee Valgus | deg | 1.86 ± 3.97 | 4.71 ± 4.90 | 3.05 ± 1.65 | 0.399 | −2.85 ± 1.83 | 1.000 | −1.19 ± 2.00 | 1.000 | 1.66 ± 2.12 |
| Max Knee Flexion | deg | 42.31 ± 32.80 | 55.55 ± 29.44 | 48.66 ± 23.73 | 1.000 | −13.24 ± 13.88 | 1.000 | −6.35 ± 15.16 | 1.000 | 6.90 ± 16.14 |
| Max Knee Rotation | deg | −11.11 ± 4.79 | −11.90 ± 4.72 | −12.49 ± 5.67 | 1.000 | 0.79 ± 2.32 | 1.000 | 1.38 ± 2.53 | 1.000 | 0.59 ± 2.69 |
| Angular Knee Moments | ||||||||||
| Knee Extension | Nm/kg | 2.05 ± 0.43 | 1.69 ± 0.20 | 1.40 ± 0.33 | 0.113 | 0.36 ± 0.16 | 0.004 * | 0.65 ± 0.18 | 0.412 | 0.29 ± 0.19 |
| Knee Flexion | Nm/kg | −0.26 ± 0.19 | −0.14 ± 0.15 | −0.15 ± 0.08 | 0.305 | −0.13 ± 0.07 | 0.526 | −0.11 ± 0.08 | 1.000 | 0.01 ± 0.09 |
| Knee Valgus | Nm/kg | 0.29 ± 0.22 | 0.27 ± 0.11 | 0.19 ± 0.12 | 1.000 | 0.02 ± 0.08 | 0.748 | 0.10 ± 0.09 | 1.000 | 0.08 ± 0.09 |
| Knee Varus | Nm/kg | −0.23 ± 0.20 | −0.17 ± 0.09 | −0.21 ± 0.07 | 1.000 | −0.06 ± 0.07 | 1.000 | −0.02 ± 0.07 | 1.000 | 0.04 ± 0.08 |
| Angular Velocities | ||||||||||
| Knee Extension | deg/s | −701.06 ± 80.94 | −641.47 ± 68.03 | −589.55 ± 74.11 | 0.310 | −59.60 ± 35.08 | 0.024 * | −111.51 ± 38.31 | 0.649 | −51.91 ± 40.77 |
| Knee Flexion | deg/s | 517.84 ± 78.64 | 476.06 ± 88.38 | 529.18 ± 107.17 | 0.969 | 41.78 ± 41.32 | 1.000 | −11.34 ± 45.13 | 0.842 | −53.12 ± 48.02 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Andrade, D.; Fonseca, P.; Sousa, F.; Gutierres, M. Does Anterior Cruciate Ligament Reconstruction with a Hamstring Tendon Autograft Predispose to a Knee Valgus Alignment on Initial Contact during Landing? A Drop Vertical Jump Movement Analysis. Appl. Sci. 2023, 13, 7363. https://doi.org/10.3390/app13137363
Andrade D, Fonseca P, Sousa F, Gutierres M. Does Anterior Cruciate Ligament Reconstruction with a Hamstring Tendon Autograft Predispose to a Knee Valgus Alignment on Initial Contact during Landing? A Drop Vertical Jump Movement Analysis. Applied Sciences. 2023; 13(13):7363. https://doi.org/10.3390/app13137363
Chicago/Turabian StyleAndrade, Daniel, Pedro Fonseca, Filipa Sousa, and Manuel Gutierres. 2023. "Does Anterior Cruciate Ligament Reconstruction with a Hamstring Tendon Autograft Predispose to a Knee Valgus Alignment on Initial Contact during Landing? A Drop Vertical Jump Movement Analysis" Applied Sciences 13, no. 13: 7363. https://doi.org/10.3390/app13137363
APA StyleAndrade, D., Fonseca, P., Sousa, F., & Gutierres, M. (2023). Does Anterior Cruciate Ligament Reconstruction with a Hamstring Tendon Autograft Predispose to a Knee Valgus Alignment on Initial Contact during Landing? A Drop Vertical Jump Movement Analysis. Applied Sciences, 13(13), 7363. https://doi.org/10.3390/app13137363






