Abstract
Whether a one-jaw or two-jaw design is used in orthognathic surgery for patients with cleft remains varied and controversial. This study aimed to compare the two approaches using 3-dimensional imaging surgical simulation. This study was conducted on 41 consecutive patients with complete unilateral cleft lip and palate treated in the craniofacial center. All patients had original two-jaw virtual planning and orthognathic surgery. Simulation of one-jaw LeFort I surgery was performed using the same final dental occlusion on 3-dimensional images. Cephalometric data and asymmetry index were collected and compared among the designs. Average advancement of the maxilla was 7.46 mm in one-jaw and 4.80 mm in two-jaw design. SNA, SNB, and A-N perpendicular were significantly greater and close to normative data in the one-jaw design. ANB angles were similar in both designs. The anterior and posterior occlusal plane cants, the deviation of midline landmarks, and the asymmetry index were more improved in the two-jaw approach. It is concluded that the two-jaw cleft orthognathic surgery could significantly improve facial midline and symmetry compared with the one-jaw approach. However, the two-jaw surgery with mandibular setback produced less protrusive facial contour although a harmonious relationship between the maxilla and mandible was achieved.
1. Introduction
Cleft lip and palate are the most common congenital craniofacial malformations, with an incidence ranging from 1.0/1000 to 2.2/1000 [1,2]. The prevalence is higher in the Asian population. Patients with cleft lip and palate could develop maxillary hypoplasia owing to intrinsic growth deficiency and extrinsic factors following surgical interventions. The maxillary deficiency causes dental malocclusion, skeletal discrepancy, maxillomandibular asymmetry, or facial disproportion requiring orthognathic surgery (OGS), with an incidence ranging between 9% and 60% [3,4,5,6,7,8].
Traditional design of OGS for the correction of maxillary retrusion in patients with cleft has been LeFort I osteotomy and advancement, aiming to correct the anteroposterior discrepancy. However, patients with cleft could likely have facial asymmetry and disproportion issues in addition to midface retrusion. Because of the improvement in surgical techniquea, safety in general anesthesia, 3-dimensional (3D) imaging simulation, and patient demand of aesthetic outcomes, there has been an increasing use of two-jaw surgery in the surgical plan. It is still controversial whether to plan one-jaw or two-jaw OGS, as each approach has its reasons and concerns [9,10,11,12]. Surgical design could be based on an individual patient’s maxillofacial condition, surgeon’s preference, or operating room facility. It would be ideal to have a prospective clinical study comparing the two approaches, but this is impractical, and the current data are deficient in this regard.
The trend has evolved over the past 40 years in our center, and two-jaw orthognathic surgery becomes the main approach for the correction of maxillofacial deformity in patients with cleft [13]. This study aimed to evaluate a series of consecutive patients with unilateral cleft lip and palate who had received orthognathic surgery and compare the two different designs (one-jaw versus two-jaw) using 3D imaging surgical simulation.
2. Materials and Methods
2.1. Patient Selection
This retrospective study recruited consecutive patients who received orthodontic treatment and orthognathic surgery in the senior authors’ Craniofacial Center from January 2017 through December 2020. Inclusion criteria were patients with complete unilateral cleft lip and palate, having cone-beam computed tomography (CBCT) with 3D surgical simulation, and surgery performed by the senior surgeon (LJL). Exclusion criteria were the presence of traumatic or syndromic craniofacial deformities, reoperated orthognathic surgery, segmental or subapical osteotomy, and incomplete data. In our practice, we did not perform maxillary expansion before the orthognathic surgery. We preferred to do minimal or minor presurgical orthodontic treatment, i.e., modified surgery (first approach). Maxillary expansion, if required, will be performed after the orthognathic surgery by orthodontic methods. Many times, the expansion was required in the cleft-side canine area, rather than the molar area. Fifty-two patients were recruited in the study. All were two-jaw OGS procedures. It must be mentioned that two-jaw surgery was routinely performed for patients with cleft in our center. Eleven patients were excluded because of incomplete data or poor quality of images (6 patients), combining segmental or subapical osteotomy (4 patients) and redo surgery (1 patient), leaving 41 patients eligible for final evaluation. All patients received preoperative and postoperative care in the same multidisciplinary team. The study was approved by the hospital ethical committee (IRB 202100523B0).
In this study, the original two-jaw surgical design was converted into a one-jaw procedure using the virtual surgical planning. LeFort I osteotomy with advancement was achieved keeping the same final occlusion. Comparisons of the maxillary and mandibular positions between the two-jaw and one-jaw surgical designs were performed.
2.2. Surgical Simulation
CBCT images were acquired using the same protocol and scanner (Imaging Sciences International, Hatfield, PA, USA). The data were processed and imported to Dolphin 3D software program (Dolphin Imaging and Management Solutions, Chatsworth, CA, USA) for virtual surgical planning. Digital dental images were integrated and registered with the CBCT model to replace the dentition [14]. The workflow of computer-assisted surgical planning was described in more detail in previous studies [15,16].
2.3. Two-Jaw Surgical Simulation
Two-jaw surgery was the original surgical plan in this study cohort. LeFort I and bilateral sagittal split osteotomy (BSSO) were performed in the 3D images. The mandibular segment was moved to match the maxillary segment according to the setup final occlusion, forming the maxillomandibular complex (MMC). The MMC was moved and rotated to achieve an ideal facial profile, with adequate facial symmetry, midline, occlusal plane, and no bony collision in the ramus [15,16]. Genioplasty was performed as needed (Figure 1).
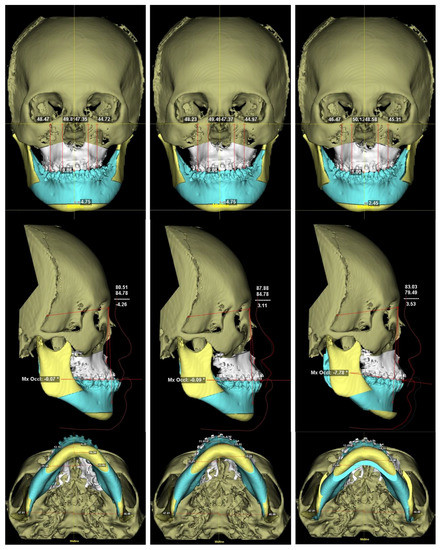
Figure 1.
A case with left cleft lip and palate showing the frontal, lateral, and basal views of 3D surgical simulation using Dolphin 3D software. (Left) Preoperative 3D cephalometric images showing skeletal class III (SNA:80.51°, SNB: 84.78°, ANB: −4.26°), occlusal plane cant (U6R-FH plane: 48.47 mm, U6L-FH plane: 44.72 mm), and chin deviation (Pog deviation of 4.75 mm toward the left side). (Middle) One-jaw surgical plan with maxillary advancement alone. A point of maxilla was advanced 7.24 mm. Skeletal class I was achieved (ANB: 3.11°) without correction of the occlusal plane cant and chin deviation. (Right) Two-jaw surgical plan with a combination of maxillary advancement and mandibular setback osteotomy and rotation. Skeletal class I was achieved by A point advancement of 2.43 mm, B point setback of 8.99 mm, and clockwise (pitch) rotation of 7.69°. Roll rotation (−3°) and yaw rotation (5°) were applied to avoid bony collision and to correct the occlusal plane cant and chin deviation.
2.4. One-Jaw Surgical Simulation
The original two-jaw surgical simulation was converted to one-jaw. Using the same final occlusion, LeFort I osteotomy was performed and advanced to match the mandible. The mandible did not receive ramus osteotomy and remained in its original position without movement (Figure 1). In the other way, the MMC was repositioned so that the mandible returned to its original location by using the software.
2.5. The 3D Cephalometric Measurement
The preoperative (T0), one-jaw, and two-jaw simulation images were exported as STL files and imported to Simplant O&O software (Materialize, Leuven, Belgium) for landmark location and 3D cephalometric measurement (Table 1). All landmarks were identified by the same investigator. Three reference planes were defined. Frankfort horizontal plane (FHP) was the plane passing through bilateral orbitales and the midpoint between the right and left portions. The midsagittal plane (MSP) was the plane passing through nasion and basion and perpendicular to FHP. The coronal plane was the plane passing through nasion and perpendicular to FHP and MSP. After landmark identification, the 3D linear and angular measurements were calculated. Comparisons of cephalometric measurement were conducted among T0, one-jaw, two-jaw designs, as well as normative Taiwanese data [17]. For further investigation in the one-jaw surgical simulation, the samples were divided into large advancement design (more than 6 mm) and regular advancement design (6 mm or less) according to the amount of maxillary movement.

Table 1.
Definition of the three-dimensional skeletal landmarks, angle and reference planes.
2.6. Asymmetry Index (ASI)
The distance from each landmark to the three reference planes was defined as dx, dy, and dz. To assess the degree of facial skeletal asymmetry, the difference between the bilateral landmarks relative to each reference plane was calculated using the asymmetry index [18,19,20] with the following equation:
For the midline landmarks, only dx was calculated with the following equation:
ASI indicated the degree of asymmetry between right and left paired landmarks. A higher ASI value showed more asymmetry. A zero ASI indicated perfect symmetry between the bilateral paired landmarks, or the midline landmarks located in the midsagittal plane.
2.7. Statistical Analysis
To assess intra-observer variability and reproducibility, 10 subjects were randomly selected for repeated tests. Landmark location and measurement were performed at a two-week interval. The intra-observer reproducibility was tested by Bland–Altman analysis. Measurement errors were calculated by the Euclidean distance using the following formula:
Δx, Δy, and Δz were the differences between the first and second landmarks in the X, Y, and Z coordinates.
The T0 was compared with normative Taiwanese data using an independent t-test. The Spearman correlation coefficient was first used to calculate the correlation between one-jaw and two-jaw designs. The p value less than 0.05 indicated that the correlation between two designs was high. Then, the paired or independent t-test was accordingly selected to examine the differences in 3D cephalometric measurements and ASI between the one-jaw and two-jaw designs. A p value of 0.05 was considered statistically significant. Statistical analyses were performed using SPSS software (SPSS Statistics for Windows, Version 17.0., SPSS Inc., Chicago, IL, USA).
3. Results
All subjects had complete unilateral cleft lip and palate (UCLP) (21 were males and 23 were left side) with a mean age of 18.5 years, ranging from 15.3 to 25.7 years. Average period of preoperative orthodontic treatment was 8.8 months. The intra-observer agreement showed excellent reliability and reproducibility in the repeated measurements (Figure 2). The mean and standard deviations of these intrarater differences were 0.0025 and 0.2360, respectively.
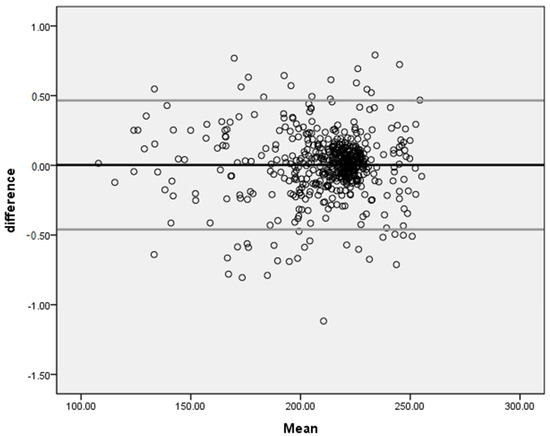
Figure 2.
The Bland–Altman plot showing adequate intra-observer reproducibility (n = 540).
3.1. The 3D Cephalometric Measurements of T0 Stage
Table 2 presents the linear and angular 3D cephalometric measurements of T0 stage, and the comparisons with the Taiwanese norms in which data gender differences were not found. SNA, ANB, and A-N perpendicular were significantly smaller than norms (p < 0.01). There were no significant differences between the patients with UCLP and normal population on SNB and Pog-N perpendicular (p > 0.05). All five midline landmarks (ANS, A, Me, U1, and L1) presented a significant deviation in relation to MSP in T0 stage (p < 0.01).

Table 2.
The 3D cephalometric measurements of the preoperative image (T0 stage) and the comparisons with normative data.
3.2. Comparisons between One-Jaw and Two-Jaw Designs
Table 3 presents the cephalometric measurements of one-jaw and two-jaw designs. SNA and SNB in the two-jaw design showed significantly smaller angles than those in norms and one-jaw designs. There was no significant difference in terms of ANB angle between one-jaw and two-jaw designs. The distance of A point to the N-perpendicular plane in one-jaw design was 2.66 mm larger than the two-jaw design (p < 0.01). In contrast, the Pog point in the two-jaw design is not significantly lower than the one-jaw design. Anterior and posterior occlusal plane cants in the two-jaw design were significantly improved by 1.54 and 1.58 degrees than the one-jaw design (p < 0.01). The posterior dental cant (between both first molars) was less than 1 degree in the two-jaw approach. The midline discrepancy was measured as the absolute value of the distance from the midsagittal plane. All four midline landmarks (A, Me, U1, and L1) in the one-jaw design were located significantly away from midsagittal plane compared to those in the two-jaw design. The ANS was constantly deviated from the midsagittal line in patients with a unilateral cleft lip and palate. The deviation is shown in Table 2. The ANS was also frequently burred during orthognathic surgery in our practice. Therefore, we did not use ANS as a midline landmark in the simulation as well as the assessment.

Table 3.
The 3D cephalometric measurements of one-jaw and two-jaw designs.
3.3. Larger versus Regular Maxillary Advancement in the One-Jaw Simulation
Advancement of 6 mm was set as the dividing distance in the one-jaw plan. Twenty-six patients (63%) needed larger maxillary advancement and 15 patients (37%) needed regular advancement in the one-jaw virtual surgical plan. In patients with larger maxillary advancement in the one-jaw plan, the two-jaw approach had significantly lower SNA, SNB, and A-N perpendicular data compared to the one-jaw plan (p < 0.01), but the ANB angle was not significantly different. However, in the regular maxillary advancement design, there was no significant difference in terms of SNA and A-N perpendicular between one-jaw and two-jaw surgery plans, but ANB angle in the two-jaw surgery was significantly larger than the one-jaw surgery by 3.28 degrees (p < 0.01) (Table 4).

Table 4.
The 3D cephalometric measurements in the larger (more than 6 mm) and regular (6 mm or less) advancement designs.
3.4. Asymmetry Index
The ASI values of maxillary and mandibular landmarks in each design are shown in Table 5. The ASI of all maxillary landmarks was significantly larger in the one-jaw design compared to T0 and two-jaw designs (except for U1), indicating more asymmetry after surgery. ASI of all maxillary and mandibular landmarks in the two-jaw design were significantly improved compared to those in the one-jaw design.

Table 5.
Asymmetry index of T0 group, one-jaw design, and two-jaw design.
4. Discussion
Cleft lip and palate are the most common congenital craniofacial anomaly. One of the common problems is midfacial retrusion owing to maxillary hypoplasia, which needs to be addressed after skeletal maturity. With the mandible in a relative prognathic position, patients have a class III facial profile. Orthognathic surgery serves as a definitive approach to rehabilitate function and esthetics [3,6]. Traditionally, a single-jaw LeFort I osteotomy with advancement was performed for the skeletal discrepancy, accepting that the mandible was generally in the correct anteroposterior position in order to avoid setting the mandible back [5]. However, orthognathic surgery for patients with cleft is more challenging due to scarring in orofacial tissues, less predictable vascular supply, inadequate tissue quality, and poor dental occlusion [21,22]. Compared to the cephalometric norms, SNA and A-N perpendicular of the subjects were significantly smaller, indicating prominent maxillary retrusion (Table 2). It is expected that the single movement of maxillary advancement could be more difficult.
For comparison of one-jaw and two-jaw designs, SNA, SNB, and A-N perpendicular were significantly smaller in the two-jaw design due to simultaneous mandible setback and clockwise pitch rotation of the maxillomandibular complex. The simulation after two-jaw surgery revealed a relatively bimaxillary retrusive facial profile as compared to the result with one-jaw surgery. However, Pog-N perpendicular was not significantly different because 31 out of 41 subjects received genioplasty in the two-jaw surgery (Table 3).
In this computer-assisted surgical simulation study, the occlusal set-up of one-jaw and two-jaw was identical. The final occlusion of all cases was set up by the same orthodontist in this study cohort. Overjet and overbite were set up at 2 mm with upper and lower dental midline coincidence. To achieve stable postoperative occlusion, the movement of maxilla was restricted by mandible and dental occlusion in the one-jaw surgery. Therefore, the occlusal plane cannot be adjusted without a mandibular osteotomy. Both anterior and posterior occlusal plane cants of the two-jaw design were superior to the one-jaw design. However, in clinical practice, we try to level the posterior dental cant but do not intend to make it 0 degrees, but rather coordinate with other parameters for symmetric and harmonious positioning of the maxillomandibular complex. The posterior dental cant was revealed in the range of −0.88–2.68, matching our clinical purpose (Table 3). For the same reason, the midline was easier to align by moving and rotating the maxillomandibular complex. Hence, the anatomic landmarks were more significantly centered and symmetric when undertaking the two-jaw surgery (Table 3).
A large amount of maxillary advancement could cause problems such as postoperative instability, a high relapse rate, velopharyngeal insufficiency, or inadequate blood supply. The limitation of LeFort I maxillary advancement was suggested as 10 mm for non-cleft patients, but the amount was advised to be conservative and no more than 6 mm in patients with cleft [23,24,25,26,27,28]. It was suggested that if the maxillomandibular discrepancy was more than 6 mm, bone graft, a combined mandibular setback osteotomy or distraction osteogenesis should be considered. In the present study, the maxilla was advanced by an average of 7.46 mm in the one-jaw design and 4.80 mm in the two-jaw design, respectively (Table 2 and Table 3, A-N perpendicular). Two-jaw surgery with mandibular setback compensated for the amount of maxillary advancement by an average of 2.66 mm. When completing one-jaw surgery, 26 patients (63%) needed maxillary advancement of more than 6 mm which was an unfavorable condition causing possible relapse (Table 4). Only 15 patients (37%) with moderate maxillary advancement were suitable and qualified for one-jaw surgery design for the correction of anteroposterior discrepancy in this study cohort. Although the regular amount of maxillary advancement was adequate to achieve positive overjet and acceptable occlusion, the skeletal relationship was still a prognathic profile with a mean ANB angle 0.25° (Table 4). Patients would complain of inadequate correction of facial appearance in our practice. By completing the two-jaw surgery, the maxillomandibular complex was allowed to rotate clockwise in the pitch direction in order to increase the ANB angle with A point forward and B point backward in order to achieve skeletal class I appearance with a better facial profile. An average gain of 3.28° (0.25°–3.53°) in ANB angle by the clockwise rotation was achieved in the present study (Table 4). Therefore, the mandibular setback osteotomy was not only able to compensate for the amount of maxillary advancement, but also to improve the jaw relationship by the clockwise rotation in cases of minor sagittal discrepancy (Figure 3).
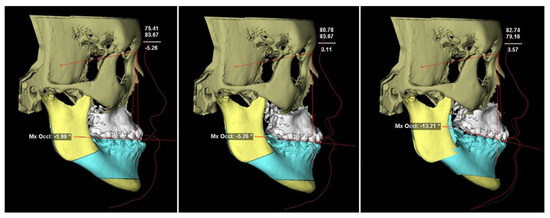
Figure 3.
A case in the regular advancement design showed that the jaw relationship was improved by the clockwise rotation of the maxillomandibular complex. (Left) Preoperative image showing that ANB was −5.26°. (Middle) In one-jaw surgical simulation, the maxilla was advanced 4.63 mm following Le Fort I osteotomy. The skeletal class III jaw relationship was not fully corrected with the ANB angle of 0.11°. (Right) A skeletal class I jaw relationship with an ANB angle of 3.57° was achieved following two-jaw surgery with the clockwise rotation of the maxillomandibular complex.
Patients with a unilateral cleft lip and palate tend to have a more asymmetrical face compared to the normal population, not only showing in the nasomaxillary region, but also in the lower facial skeleton [20,29,30,31]. It is consistent with the results of this study that both maxillary and mandibular midline landmarks were significantly deviated from the midsagittal plane compared to norms (Table 2). The deviation and asymmetry could only be improved by the two-jaw approach but not the one-jaw surgery (Table 3). The asymmetry index (ASI) was first proposed for assessing right and left ramal height symmetry in 2-dimensional orthopantomograms [18]. ASI was then used to evaluate the extent of 3-dimensional asymmetry of facial skeletons [19,32], and applied in cleft orthognathic surgery planning [20]. The present study showed that in comparison with ASI, the two-jaw design obtained more symmetry in both the maxilla and mandible (Figure 1). By undertaking a two-jaw surgery, the U1 in the maxilla and all midline landmarks in the mandible were significantly improved (Table 5). In the one-jaw OGS simulation, the maxillary symmetry could get worse, and the mandibular asymmetry remained the same (Table 5). The results indicated that the two-jaw surgery could more likely achieve facial symmetry and balance, particularly in the lower part of the face [20].
The surgical design of cleft OGS is based on the patient’s deformity, surgeon’s preference and training background. In the literature review, Table 6 shows that the rate of one-jaw or two-jaw surgery varied among different institutions, ranging from 12% to 100% for two-jaw surgery. From 2017 to 2020, all patients with a unilateral cleft lip and palate received two-jaw orthognathic surgery in our center. An important reason for such a high rate of two-jaw cleft OGS was the application of 3D imaging and virtual surgery planning, which accurately detected bony abnormalities to achieve symmetry in the simulation [33]. Mandibular yaw rotation to avoid ramus bony collision and attain cheek symmetry was conveniently achieved in the two-jaw surgery planning (Figure 4). More than 98% of patients with cleft received two-jaw orthognathic surgery when it was indicated. This paradigm shift was mentioned in our previous publications, with the more reasons than facial symmetry, but also including other facial aesthetic purposes, such as smile arc. It is the center’s treatment preference and could be a bias. However, for the discrepancies that remain after the one-jaw surgery, there is the possibility of orthodontic correction with temporary anchorage devices which can correct the occlusal cantus and midline discrepancies for the unoperated maxilla. It is believed that with the right collaboration, some of the cases which were two-jaw surgery at the first glance can be resolved with only one-jaw surgery if temporary anchorage devices are placed. The occlusal plane can also be adjusted by maxillary molar intrusion.
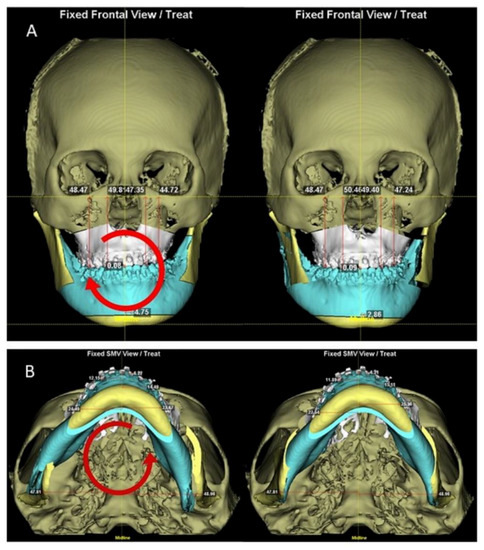
Figure 4.
The same case as in Figure 1 demonstrated roll and yaw rotations of the maxillomandibular complex for asymmetry correction in two-jaw surgical planning. (A) Occlusal plane and chin deviation were improved after clockwise rotation in the roll direction. (B) Elimination of residual asymmetry of contour and interference between the osteotomized bony segments by counterclockwise rotation of the maxillomandibular complex in the yaw direction. As a result, the advancement in the LeFort I level was 1.50 mm in the right piriform and 5.07 mm in the left piriform.
Ethnic differences should be considered in designing the cleft OGS. It is noted that Asians have a higher incidence of Angle class III malocclusion and a relatively large mandible compared to maxilla and cranial base [34,35]. It is, therefore, favorable and popular to include mandibular setback and rotation in the cleft OGS [36,37,38]. Possible drawbacks from the addition of mandibular osteotomy should also be concerned. These included longer operative time, infection, blood loss, and chin numbness. With preoperative imaging of the inferior alveolar nerves and careful performance of the ramus split osteotomy, the neurosensory disturbance should be kept to a minimum [39,40]. Airway decrease by mandibular setback was reported and should be cautioned in patients with breathing problems [41,42]. However, the improvement in sleep apnea and snoring without airway-related problems was also described [43,44]. This is consistent with our clinical experience.

Table 6.
The incidence of one-jaw and two-jaw cleft orthognathic surgery in different institutions.
Table 6.
The incidence of one-jaw and two-jaw cleft orthognathic surgery in different institutions.
| Author Year | Country | Patient Number | One-Jaw Surgery (LeFort I) | Two-Jaw Surgery |
|---|---|---|---|---|
| Posnick et al., 1996 [45] | USA | 116 | 72.4% | 27.6% |
| Iannetti et al., 2004 [46] | Italy | 93 | 40.0% | 60.0% |
| Chong et al., 2009 [47] | USA | 103 | 50.5% | 49.5% |
| Broome et al., 2010 [48] | Switzerland | 58 | 84.5% | 15.5% |
| Watts et al., 2014 [49] | Canada | 30 | 46.7% | 53.3% |
| Fahradyan et al., 2018 [50] | USA | 136 | 46.3% | 53.7% |
| Impieri et al., 2018 [51] | Norway | 47 | 63.8% | 36.2% |
| Marion et al., 2019 [52] | France | 54 | 68.5% | 31.5% |
| Yatabe-Ioshida et al., 2019 [44] | Brazil | 9 | 22.2% | 77.8% |
| Chung et al., 2019 [53] | Korea | 44 | 0% | 100% |
| Hwang et al., 2019 [22] | Korea | 17 | 0% | 100% |
| Harjunpää et al., 2019 [54] | Finland | 93 | 74.2% | 25.8% |
| Wang et al., 2020 [55] | China | 90 | 52.2% | 47.8% |
| Wangsrimongkol et al., 2021 [56] | USA | 73 | 88.0% | 12.0% |
The limitations in this study were the retrospective nature and the virtual surgical planning without looking at the actual postoperative outcome between the two designs. As satisfactory translation of the 3D plan to the operating theater has been confirmed in the previous reports, the extended outcome assessment between one-jaw and two-jaw cleft OGS appeared to be unimportant in this report. The final dental occlusion was set and applied in both study designs of one-jaw and two-jaw surgery. In actual clinical practice, the final occlusion could be modified in order to obtain a better maxillomandibular relationship for the movement in virtual planning, as the patients with cleft might have dental deficiency and irregularity. One should carefully interpret the data in this study. A routine two-jaw OGS planning for patients with cleft is not advocated. The patient’s deformity, expectation, and surgeon’s preference should be considered. The planning is best undertaken by the multidisciplinary team.
Author Contributions
Y.-H.T. was responsible for data collection, analysis, and writing manuscript. B.C.J.P. was responsible for setting up final occlusion in the study patients. H.-H.L. was in charge of the image measurement and data analysis. C.-T.H. supervised the measurement and data analysis. L.-J.L. was responsible for analysis and editing of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
None of the authors have any source of financial or other support, or any financial or professional relationship that may pose a competing interest.
Institutional Review Board Statement
The Institutional Review Board of Chang Gung Foundation (IRB 202100523B0) approved this study.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Acknowledgments
We would like to thank Ping-Hsuan Huang, Center for Big Data Analytics and Statistics, Chang Gung Memorial Hospital, for statistical consultation. This study was supported by grants from Chang Gung Memorial Hospital (CMRPG3K0981 and CMRPG3L0351).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Derijcke, A.; Eerens, A.; Carels, C. The incidence of oral clefts: A review. Br. J. Oral Maxillofac. Surg. 1996, 34, 488–494. [Google Scholar] [CrossRef]
- Chang, W.-J.; See, L.-C.; Lo, L.-J. Time trend of incidence rates of cleft lip/palate in Taiwan from 1994 to 2013. Biomed. J. 2016, 39, 150–154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ross, R.B. Treatment variables affecting facial growth in complete unilateral cleft lip and palate. Cleft Palate J. 1987, 24, 5–77. [Google Scholar] [PubMed]
- DeLuke, D.M.; Marchand, A.; Robles, E.C.; Fox, P. Facial growth and the need for orthognathic surgery after cleft palate repair: Literature review and report of 28 cases. J. Oral Maxillofac. Surg. 1997, 55, 694–697. [Google Scholar] [CrossRef]
- Daskalogiannakis, J.; Mehta, M. The Need for Orthognathic Surgery in Patients with Repaired Complete Unilateral and Complete Bilateral Cleft Lip and Palate. Cleft Palate-Craniofacial J. 2009, 46, 498–502. [Google Scholar] [CrossRef]
- Oberoi, S.; Hoffman, W.Y.; Chigurupati, R.; Vargervik, K. Frequency of Surgical Correction for Maxillary Hypoplasia in Cleft Lip and Palate. J. Craniofacial Surg. 2012, 23, 1665–1667. [Google Scholar] [CrossRef]
- Dalle Ore, C.; Schoenbrunner, A.; Brandel, M.; Kronstadt, N.; McIntyre, J.; Jones, M.; Gosman, A. Incidence of Le Fort Surgery in a Mature Cohort of Patients With Cleft Lip and Palate. Ann. Plast. Surg. 2017, 78 (Suppl. S4), S199–S203. [Google Scholar] [CrossRef]
- Pai, B.C.J.; Hung, Y.T.; Wang, R.S.H.; Lo, L.J. Outcome of patients with complete unilateral cleft lip and palate: 20-year follow-up of a treatment protocol. Plast. Reconstr. Surg. 2019, 143, 359e–367e. [Google Scholar] [CrossRef]
- Phillips, J.H.; Nish, I.; Daskalogiannakis, J. Orthognathic Surgery in Cleft Patients. Plast. Reconstr. Surg. 2012, 129, 535e–548e. [Google Scholar] [CrossRef]
- James, J.N.; Costello, B.J.; Ruiz, R.L. Management of Cleft Lip and Palate and Cleft Orthognathic Considerations. Oral Maxillofac. Surg. Clin. N. Am. 2014, 26, 565–572. [Google Scholar] [CrossRef]
- Wong, F.; Heggie, A.; Shand, J.; Schneider, P. Skeletal stability of maxillary advancement with and without a mandibular reduction in the cleft lip and palate patient. Int. J. Oral Maxillofac. Surg. 2016, 45, 1501–1507. [Google Scholar] [CrossRef] [PubMed]
- Roy, A.-A.; Rtshiladze, M.A.; Stevens, K.; Phillips, J. Orthognathic Surgery for Patients with Cleft Lip and Palate. Clin. Plast. Surg. 2019, 46, 157–171. [Google Scholar] [CrossRef]
- Denadai, R.; Chou, P.Y.; Pai, B.C.; Chen, C.; Lin, C.C.H.; Huang, C.S.; Chen, Y.R.; Lo, L.J. Skeletofacial reconstruction for cleft-related deformities: Four decades of evolving cleft care. Ann. Plast. Surg. 2020, 85, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Ho, C.T.; Lin, H.H.; Lo, L.J. Intraoral scanning and setting up the digital final occlusion in three-dimensional planning of orthognathic surgery: Its comparison with the dental model approach. Plast. Reconstr. Surg. 2019, 143, 1027e–1036e. [Google Scholar] [CrossRef]
- Seo, H.J.; Denadai, R.; Pai, B.C.-J.; Lo, L.-J. Modern Surgery-First Approach Concept in Cleft-Orthognathic Surgery: A Comparative Cohort Study with 3D Quantitative Analysis of Surgical-Occlusion Setup. J. Clin. Med. 2019, 8, 2116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Denadai, R.; Chen, Y.-R.; Lo, L.-J. Three-Dimensional Computer-Assisted Single-Splint 2-Jaw Cleft Orthognathic Surgery: Toward Patient-Centered Surgical Rationale. Cleft Palate-Craniofacial J. 2020, 57, 1428–1433. [Google Scholar] [CrossRef]
- Wang, R.H.; Ho, C.-T.; Lin, H.-H.; Lo, L.-J. Three-dimensional cephalometry for orthognathic planning: Normative data and analyses. J. Formos. Med. Assoc. 2020, 119 Pt 2, 191–203. [Google Scholar] [CrossRef]
- Habets, L.L.M.H.; Bezuur, J.N.; Naeiji, M.; Hansson, T.L. The Orthopantomogram, an aid in diagnosis of temporomandibular joint problems. II. The vertical symmetry. J. Oral Rehabil. 1988, 15, 465–471. [Google Scholar] [CrossRef]
- Katsumata, A.; Fujishita, M.; Maeda, M.; Ariji, Y.; Ariji, E.; Langlais, R.P. 3D-CT evaluation of facial asymmetry. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2005, 99, 212–220. [Google Scholar] [CrossRef]
- Patel, D.S.; Jacobson, R.; Duan, Y.; Zhao, L.; Morris, D.; Cohen, M.N. Cleft skeletal asymmetry: Asymmetry index, classification and application. Cleft Palate-Craniofacial J. 2018, 55, 348–355. [Google Scholar] [CrossRef]
- Hochban, W.; Ganß, C.; Austermann, K.H. Long-term results after maxillary advancement in patients with clefts. Cleft Palate-Craniofacial J. 1993, 30, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Hwang, D.; Choi, H.S.; Kim, U.K.; Song, J.-M. Complications Following Orthognathic Surgery for Patients with Cleft Lip/Palate. J. Craniofacial Surg. 2019, 30, 1815–1819. [Google Scholar] [CrossRef] [PubMed]
- Polley, J.W.; Figueroa, A.A. Management of Severe Maxillary Deficiency in Childhood and Adolescence through Distraction Osteogenesis With an External, Adjustable, Rigid Distraction Device. J. Craniofacial Surg. 1997, 8, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Yamaji, K.E.; Gateno, J.; Xia, J.J.; Teichgraeber, J.F. New Internal Le Fort I Distractor for the Treatment of Midface Hypoplasia. J. Craniofacial Surg. 2004, 15, 124–127. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.X.; Wang, X.; Yi, B.; Li, Z.L.; Liang, C.; Lin, Y. Internal midface distraction in correction of severe maxillary hypoplasia secondary to cleft lip and palate. Plast. Reconstr. Surg. 2005, 116, 51–60. [Google Scholar] [CrossRef]
- Cheung, L.K.; Chua, H.D.P.; Hägg, M.B. Cleft maxillary distraction versus orthognathic surgery: Clinical morbidities and surgical relapse. Plast. Reconstr. Surg. 2006, 118, 996–1008. [Google Scholar] [CrossRef]
- Scolozzi, P. Distraction osteogenesis in the management of severe maxillary hypoplasia in cleft lip and palate patients. J. Craniofacial Surg. 2008, 19, 1199–1214. [Google Scholar] [CrossRef] [Green Version]
- Combs, P.D.; Harshbarger, R.J., 3rd. Le fort I maxillary advancement using distraction osteogenesis. Semin. Plast. Surg. 2014, 28, 193–198. [Google Scholar] [CrossRef] [Green Version]
- Laspos, C.P.; Kyrkanides, S.; Tallents, R.H.; E Moss, M.; Subtelny, J.D. Mandibular and maxillary asymmetry in individuals with unilateral cleft lip and palate. Cleft Palate-Craniofacial J. 1997, 34, 232–239. [Google Scholar] [CrossRef]
- Kyrkanides, S.; Klambani, M.; Subtelny, J.D. Cranial base and facial skeleton asymmetries in individuals with unilateral cleft lip and palate. Cleft Palate-Craniofacial J. 2000, 37, 556–561. [Google Scholar] [CrossRef]
- Lin, Y.; Chen, G.; Fu, Z.; Ma, L.; Li, W. Cone-beam computed tomography assessment of lower facial asymmetry in unilateral cleft lip and palate and non-cleft patients with class iii skeletal relationship. PLoS ONE 2015, 10, e0130235. [Google Scholar]
- Choi, Y.-K.; Park, S.-B.; Kim, Y.-I.; Son, W.-S. Three-dimensional evaluation of midfacial asymmetry in patients with nonsyndromic unilateral cleft lip and palate by cone-beam computed tomography. Korean J. Orthod. 2013, 43, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Lonic, D.; Pai, B.C.-J.; Yamaguchi, K.; Chortrakarnkij, P.; Lin, H.-H.; Lo, L.-J. Computer-assisted orthognathic surgery for patients with cleft lip/palate: From traditional planning to three-dimensional surgical simulation. PLoS ONE 2016, 11, e0152014. [Google Scholar] [CrossRef]
- Lew, K.K.; Foong, W.C.; Loh, E. Malocclusion prevalence in an ethnic Chinese population. Aust. Dent. J. 1993, 38, 442–449. [Google Scholar] [CrossRef] [PubMed]
- Zere, E.; Chaudhari, P.K.; Sharan, J.; Dhingra, K.; Tiwari, N. Developing Class III malocclusions: Challenges and solutions. Clin. Cosmet. Investig. Dent. 2018, 10, 99–116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, E.K.; Soh, J.; Petocz, P.; Darendeliler, M.A. Esthetic evaluation of Asian-Chinese profiles from a white perspective. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 532–538. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, S.; Sugahara, T.; Takabatake, S.; Taketa, H.; Ando, R.; Takano-Yamamoto, T. Influence of anteroposterior mandibular positions on facial attractiveness in Japanese adults. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 73–78. [Google Scholar] [CrossRef]
- Lee, L.H.; Jun, J.H.; Danganan, M.; Pogrel, M.A.; Kushner, H.; Lee, J.S. Orthognathic surgery for the Asian patient and the influence of the surgeon’s background on treatment. Int. J. Oral Maxillofac. Surg. 2011, 40, 458–463. [Google Scholar] [CrossRef]
- Chortrakarnkij, P.; Lonic, D.; Lin, H.H.; Yamaguchi, K.; Kim, S.G.; Lo, L.J. A Modified Technique of Mandibular Ramus Sagittal Split Osteotomy for Prevention of Inferior Alveolar Nerve Injury: A Prospective Cohort Study and Outcome Assessment. Ann. Plast. Surg. 2017, 78 (Suppl. S2), S108–S116. [Google Scholar] [CrossRef]
- Choi, B.-K.; Lee, W.; Lo, L.-J.; Yang, E.-J. Is injury to the inferior alveolar nerve still common during orthognathic surgery? Manual twist technique for sagittal split ramus osteotomy. Br. J. Oral Maxillofac. Surg. 2018, 56, 946–951. [Google Scholar] [CrossRef]
- Hsieh, Y.J.; Chen, Y.C.; Chen, Y.A.; Liao, Y.F.; Chen, Y.R. Effect of bimaxillary rotational setback surgery on upper airway structure in skeletal class III deformities. Plast. Reconstr. Surg. 2015, 135, 361e–369e. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Wang, Y.; Hu, H.; Liao, Q.; Zhang, W.; Xiang, X.; Fan, X. Impact on the upper airway space of different types of orthognathic surgery for the correction of skeletal class III malocclusion: A systematic review and meta-analysis. Int. J. Surg. 2017, 38, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.-S.; Wallace, C.G.; Hsiao, Y.-C.; Hsieh, Y.-J.; Wang, Y.-C.; Chen, N.-H.; Liao, Y.-F.; Liou, E.J.-W.; Chen, P.K.-T.; Chen, J.-P.; et al. Airway Changes after Cleft Orthognathic Surgery Evaluated by Three-Dimensional Computed Tomography and Overnight Polysomnographic Study. Sci. Rep. 2017, 7, 12260. [Google Scholar] [CrossRef]
- Yatabe-Ioshida, M.S.; Campos, L.D.; Yaedu, R.Y.; Trindade-Suedam, I. Upper Airway 3D Changes of Patients with Cleft Lip and Palate After Orthognathic Surgery. Cleft Palate-Craniofacial J. 2019, 56, 314–320. [Google Scholar] [CrossRef]
- Posnick, J.C. Orthognathic surgery for the cleft lip and palate patient. Semin. Orthod. 1996, 2, 205–214. [Google Scholar] [CrossRef]
- Iannetti, G.; Cascone, P.; Saltarel, A.; Ettaro, G. Le Fort I in cleft patients: 20 years’ experience. J. Craniofacial Surg. 2004, 15, 662–669. [Google Scholar] [CrossRef]
- Chong, D.K.; Portnof, J.E.; Xu, H.; Salyer, K.E. Reviewing the orthognathic surgical care of the patient with cleft lip and palate: The single surgeon experience. J. Craniofacial Surg. 2009, 20 (Suppl. S2), 1895–1904. [Google Scholar] [CrossRef] [Green Version]
- Broome, M.; Herzog, G.; Hohlfeld, J.; Roessingh, A.D.B.; Jaques, B. Influence of the Primary Cleft Palate Closure on the Future Need for Orthognathic Surgery in Unilateral Cleft Lip and Palate Patients. J. Craniofacial Surg. 2010, 21, 1615–1618. [Google Scholar] [CrossRef] [Green Version]
- Watts, G.D.; Antonarakis, G.S.; Forrest, C.R.; Tompson, B.D.; Phillips, J.H. Single Versus Segmental Maxillary Osteotomies and Long-Term Stability in Unilateral Cleft Lip and Palate Related Malocclusion. J. Oral Maxillofac. Surg. 2014, 72, 2514–2521. [Google Scholar] [CrossRef]
- Fahradyan, A.; Wolfswinkel, E.M.; Clarke, N.; Park, S.; Tsuha, M.; Urata, M.M.; Hammoudeh, J.A.; Yamashita, D.-D.R. Impact of the Distance of Maxillary Advancement on Horizontal Relapse After Orthognathic Surgery. Cleft Palate-Craniofacial J. 2018, 55, 546–553. [Google Scholar] [CrossRef]
- Impieri, D.; Tønseth, K.; Hide, Ø.; Brinck, E.; Høgevold, H.; Filip, C. Impact of orthognathic surgery on velopharyngeal function by evaluating speech and cephalometric radiographs. J. Plast. Reconstr. Aesthetic Surg. 2018, 71, 1786–1795. [Google Scholar] [CrossRef] [PubMed]
- Marion, F.; Mercier, J.; Odri, G.-A.; Perrin, J.; Longis, J.; Kün-Darbois, J.-D.; Corre, P.; Bertin, H. Associated relaps factors in Le Fort I osteotomy. A retrospective study of 54 cases. J. Stomatol. Oral Maxillofac. Surg. 2019, 120, 419–427. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.; Lim, J.; Park, H.; Yoo, A.; Kim, S.; Koo, Y. Correlation Between Speech Outcomes and the Amount of Maxillary Advancement After Orthognathic Surgery (Le Fort I Conventional Osteotomy and Distraction Osteogenesis) in Patients With Cleft Lip and Palate. J. Craniofacial Surg. 2019, 30, 1855–1858. [Google Scholar] [CrossRef] [PubMed]
- Harjunpää, R.; Alaluusua, S.; Leikola, J.; Heliövaara, A. Le Fort I osteotomy in cleft patients: Maxillary advancement and velopharyngeal function. J. Cranio-Maxillofacial Surg. 2019, 47, 1868–1874. [Google Scholar] [CrossRef]
- Wang, Y.; Li, J.; Xu, Y.; Huang, N.; Shi, B.; Li, J. Accuracy of virtual surgical planning-assisted management for maxillary hypoplasia in adult patients with cleft lip and palate. J. Plast. Reconstr. Aesthetic Surg. 2020, 73, 134–140. [Google Scholar] [CrossRef] [Green Version]
- Wangsrimongkol, B.; Flores, R.L.; Staffenberg, D.A.; Rodriguez, E.D.; Shetye, P.R. Skeletal and dental correction and stability following LeFort I advancement in patients with cleft lip and palate with mild, moderate, and severe maxillary hypoplasia. Cleft Palate-Craniofacial J. 2021, 59, 98–109, Online ahead of print. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).