Exercise for People with Acquired Brain Injury: An ICF Perspective
Abstract
Featured Application
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
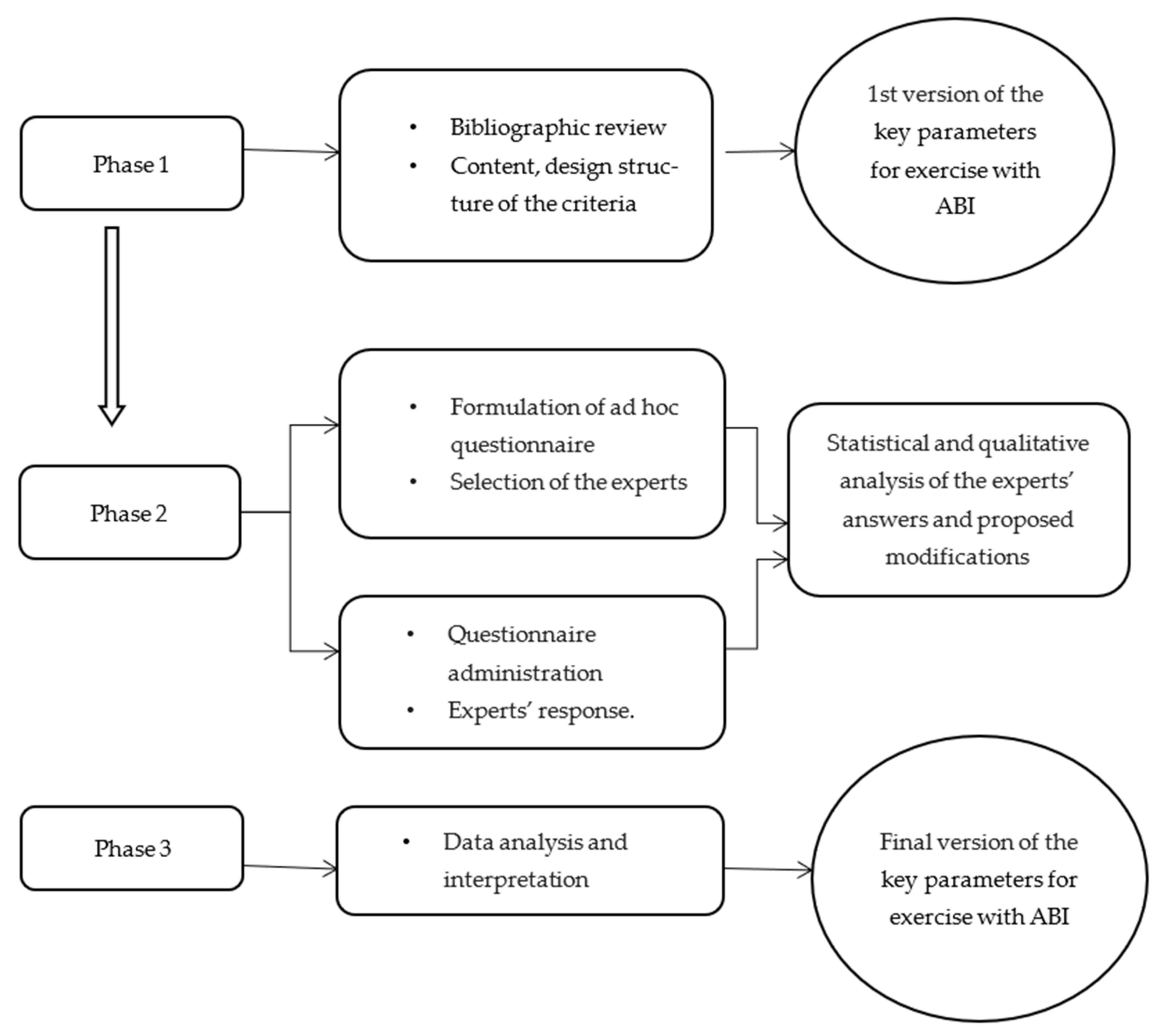
2.2. Design
2.3. Procedure
2.4. Data Analysis
2.4.1. Qualitative Analysis
2.4.2. Statistical Analysis
3. Results
3.1. Mental Health Functions
3.2. Pain and Sensorial Functions
3.3. Voice and Speech Functions
3.4. System Functions
3.5. Neuromusculoskeletal Functions
3.6. Skin Functions
3.7. Activity and Participation
3.8. Contextual Factors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Aidar, F.J.; de Oliveira, R.J.; de Matos, D.G.; Mazini Filho, M.L.; Moreira, O.C.; de Oliveira, C.E.; Hickner, R.C.; Reis, V.M. A Randomized Trial Investigating the Influence of Strength Training on Quality of Life in Ischemic Stroke. Top. Stroke Rehabil. 2016, 23, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Baron, R.; Binder, A.; Wasner, G. Neuropathic pain: Diagnosis, pathophysiological mechanisms, and treatment. Lancet Neurol. 2010, 9, 807–819. [Google Scholar] [CrossRef]
- Belfiore, P.; Miele, A.; Gallè, F.; Liguori, G. Adapted physical activity and stroke: A systematic review. J. Sports Med. Phys. Fit. 2018, 58, 1867–1875. [Google Scholar] [CrossRef] [PubMed]
- Bergmann, J.; Krewer, C.; Bauer, P.; Koenig, A.; Riener, R.; Müller, F. Virtual reality to augment robot-assisted gait training in non-ambulatory patients with a subacute stroke: A pilot randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2018, 54, 397–407. [Google Scholar] [CrossRef]
- Bertills, K.; Granlund, M.; Dahlström, Ö.; Augustine, L. Relationships between physical education (PE) teaching and student self-efficacy, aptitude to participate in PE and functional skills: With a special focus on students with disabilities. Phys. Educ. Sport Pedagog. 2018, 23, 387–401. [Google Scholar] [CrossRef]
- Cullen, N. Acquired Brain Injury: An Integrative Neuro-Rehabilitation Approach. N. Engl. J. Med. 2019, 357, 2415–2416. [Google Scholar] [CrossRef]
- Chen, R.; Cohen, L.G.; Hallett, M. Nervous system reorganization following injury. Neuroscience 2002, 111, 761–773. [Google Scholar] [CrossRef]
- Declerck, L.; Kaux, J.F.; Vanderthommen, M.; Lejeune, T.; Stoquart, G. The Effect of Adaptive Sports on Individuals with Acquired Neurological Disabilities and Its Role in Rehabilitation: A Systematic Review. Curr. Sports Med. Rep. 2019, 18, 458–473. [Google Scholar] [CrossRef]
- Dewan, M.C.; Rattani, A.; Gupta, S.; Baticulon, R.E.; Hung, Y.C.; Punchak, M.; Agrawal, A.; Adeleye, A.O.; Shrime, M.G.; Rubiano, A.M.; et al. Estimating the global incidence of traumatic brain injury. J. Neurosurg. 2018, 130, 1–18. [Google Scholar] [CrossRef]
- Doussoulin, A.; Rivas, C.; Bacco, J.; Rivas, R.; & Sepúlveda, P. Efectos de la espasticidad en la recuperación motora posterior a un ACV. Rev. Chil. Neuro.-Psiquiatr. 2019, 57, 377–386. [Google Scholar] [CrossRef]
- Feigin, V.L.; Vos, T.; Nichols, E.; Owolabi, M.O.; Carroll, W.M.; Dichgans, M.; Deuschl, G.; Parmar, P.; Brainin, M.; Murray, C. The global burden of neurological disorders: Translating evidence into policy. Lancet Neurol. 2020, 19, 255–265. [Google Scholar] [CrossRef]
- Fleming, J.; Kuipers, P.; Foster, M.; Smith, S.; & Doig, E. Evaluation of an outpatient, peer group intervention for people with acquired brain injury based on the ICF ‘Environment’ dimension. Disabil. Rehabil. 2009, 31, 1666–1675. [Google Scholar] [CrossRef]
- García-Hernández, J.J.; González-Alted, C.; Bilbao, Á.; Croche, L.F.; Pérez-Rodríguez, M.; Bravo, S.; Hita, L.; Alves, S. Daño Cerebral Adquirido. Guía de Actividades Físico-Deportivas. IMSERSO. 2011. Available online: http://imserso.es/InterPresent2/groups/imserso/documents/binario/32008danocerebral.pdf (accessed on 27 February 2022).
- Garcia-Hernandez, J.J.; Mediavilla-Saldana, L.; Perez-Rodriguez, M.; Perez-Tejero, J.; Gonzalez-Alted, C. Analysis of the effect of physical group activities in patients with acquired brain injury in the subacute phase. Rev. Neurol. 2013, 57, 64–70. [Google Scholar]
- Garcia-Munoz, C.; Casuso-Holgado, M. Effectiveness of Wii Fit Balance board in comparison with other interventions for post-stroke balance rehabilitation. Systematic review and meta-analysis. Rev. Neurol. 2019, 69, 271–279. [Google Scholar]
- George, D.; Mallery, P. SPSS for Windows Step by Step: A Simple Guide and Reference; Allyn and Bacon: Boston, MA, USA, 2003. [Google Scholar]
- Gerber, G.J.; Gargaro, J.; McMackin, S. Community integration and health-related quality-of-life following acquired brain injury for persons living at home. Brain Inj. 2016, 30, 1552–1560. [Google Scholar] [CrossRef]
- Gronek, P.; Adamczyk, J.; Celka, R.; Gronek, J. Cognicise—A New Model of Exercise. Trends Sport Sci. 2021, 28, 5–10. [Google Scholar] [CrossRef]
- Gunn, S.; Burgess, G.H. Factors predicting rehabilitation outcomes after severe acquired brain injury in trauma, stroke and anoxia populations: A cohort study. Neuropsychol. Rehabil. 2020, 18, 1–32. [Google Scholar] [CrossRef]
- Hall, J.; Morton, S.; Fitzsimons, C.F.; Hall, J.F.; Corepal, R.; English, C.; Forster, A.; Lawton, R.; Patel, A.; Mead, G.; et al. Factors influencing sedentary behaviours after stroke: Findings from qualitative observations and interviews with stroke survivors and their caregivers. BMC Public Health 2020, 20, 967. [Google Scholar] [CrossRef]
- Hassett, L.; Tate, R.; Moseley, A.; Gillett, L. Injury severity, age and pre-injury exercise history predict adherence to a home-based exercise programme in adults with traumatic brain injury. Brain Inj. 2011, 25, 698–706. [Google Scholar] [CrossRef]
- Heinemann, K. (Ed.) Introducción a la metodología de la investigación empírica en las ciencias del deporte. In Introduction to the Methodology of Empirical Research in Sports Sciences; Paidotribo: Barcelona, Spain, 2003. [Google Scholar]
- Jennekens, N.; De Casterlé, B.D.; Dobbels, F. A systematic review of care needs of people with traumatic brain injury (TBI) on a cognitive, emotional and behavioural level. J. Clin. Nurs. 2010, 19, 1198–1206. [Google Scholar] [CrossRef]
- Jolliffe, L.; Lannin, N.A.; Cadilhac, D.A.; Hoffmann, T. Systematic review of clinical practice guidelines to identify recommendations for rehabilitation after stroke and other acquired brain injuries. BMJ Open 2018, 8, e018791. [Google Scholar] [CrossRef] [PubMed]
- Kelly, G.; Shanley, J. Rehabilitation of ataxic gait following cerebellar lesions: Applying theory to practice. Physiother. Theory Pr. 2016, 32, 430–437. [Google Scholar] [CrossRef] [PubMed]
- Kuipers, P.; Foster, M.; Smith, S.; Fleming, J. Using ICF-Environment factors to enhance the continuum of outpatient ABI rehabilitation: An exploratory study. Disabil. Rehabil. 2009, 31, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Kwok, N. ICF: A Hands-on Approach for Clinicians and Families. Adapt. Phys. Act. Q. 2020, 38, 170–172. [Google Scholar]
- Lamberti, N.; Straudi, S.; Malagoni, A.M.; Argiro, M.; Felisatti, M.; Nardini, E.; Zambon, C.; Basaglia, N.; Manfredini, F. Effects of low-intensity endurance and resistance training on mobility in chronic stroke survivors: A pilot randomized controlled study. Eur. J. Phys. Rehabil. Med. 2017, 53, 228–239. [Google Scholar] [CrossRef]
- Lorenz, L.S.; Charrette, A.L.; O’Neil-Pirozzi, T.M.; Doucett, J.M.; Fong, J. Healthy body, healthy mind: A mixed methods study of outcomes, barriers and supports for exercise by people who have chronic moderate-to-severe acquired brain injury. Disabil. Health J. 2018, 11, 70–78. [Google Scholar] [CrossRef]
- Luo, L.; Meng, H.; Wang, Z.; Zhu, S.; Yuan, S.; Wang, Y.; Wang, Q. Effect of high-intensity exercise on cardiorespiratory fitness in stroke survivors: A systematic review and meta-analysis. Ann. Phys. Rehabil. Med. 2020, 63, 59–68. [Google Scholar] [CrossRef]
- Malá, H.; Rasmussen, C.P. The effect of combined therapies on recovery after acquired brain injury: Systematic review of preclinical studies combining enriched environment, exercise, or task-specific training with other therapies. Restor. Neurol. Neurosci. 2017, 35, 25–64. [Google Scholar] [CrossRef]
- McAllister, T.W. Neurobiological consequences of traumatic brain injury. Dialogues Clin. Neurosci. 2011, 13, 287–300. [Google Scholar] [CrossRef]
- McCarron, R.H.; Watson, S.; Gracey, F. What do Kids with Acquired Brain Injury Want? Mapping Neuropsychological Rehabilitation Goals to the International Classification of Functioning, Disability and Health. J. Int. Neuropsychol. Soc. 2019, 25, 403–412. [Google Scholar] [CrossRef]
- McDonald, S.; Togher, L.; Code, C. Social and Communication Disorders Following Traumatic Brain Injury, 2nd ed. Psychology Press: Hove, UK, 2016.
- Middag-van Spanje, M.; Smeets, S.; van Haastregt, J.; van Heugten, C. Outcomes of a community-based treatment programme for people with acquired brain injury in the chronic phase: A pilot study. Neuropsychol. Rehabil. 2019, 29, 305–321. [Google Scholar] [CrossRef]
- Moore, G.; Durstine, J.L.; Painter, P. ACSM’s Exercise Management for Persons with Chronic Diseases and Disabilities, 4th ed.; Human Kinetics: Champaign, IL, USA, 2016. [Google Scholar]
- Morgan, A.T.; Vogel, A.P. Intervention for dysarthria associated with acquired brain injury in children and adolescents. Cochrane Database Syst. Rev. 2008, 3, 006279. [Google Scholar] [CrossRef]
- Noe-Sebastian, E.; Balasch-Bernat, M.; Colomer-Font, C.; Moliner-Munoz, B.; Rodriguez Sanchez-Leiva, C.; Ugart, P.; Llorens, R.; Ferri-Campos, J. Disability after stroke: A longitudinal study in moderate and severe stroke patients included in a multidisciplinary rehabilitation program. Rev. Neurol. 2017, 64, 385–392. [Google Scholar]
- O’Neil-Pirozzi, T.M.; Marcinczyk, K.A.; Peltier, A.N.; Rodano, K.M. Survivor-perceived motivational facilitators and barriers to participation in cognitive exercise following chronic acquired brain injury. Brain Inj. 2019, 33, 1308–1319. [Google Scholar] [CrossRef]
- Odumuyiwa, T.; Kennedy, M.; Norman, A.; Holloway, M.; Suffield, F.; Forrest, H.; Dicks, H. Improving access to social care services following acquired brain injury: A needs analysis. J. Long-Term Care 2019, 11, 164–175. [Google Scholar] [CrossRef]
- Omar, N.H.; Mohd Nordin, N.A.; Chai, S.C.; Abdul Aziz, A.F. Functionality among stroke survivors with upper limb impairment attending community-based rehabilitation. Med. J. Malays. 2020, 75, 146–151. [Google Scholar]
- Ozgozen, S.; Guzel, R.; Basaran, S.; Coskun Benlidayi, I. Residual Deficits of Knee Flexors and Plantar Flexors Predict Normalized Walking Performance in Patients with Poststroke Hemiplegia. J. Stroke Cereb. Dis. 2020, 29, 104658. [Google Scholar] [CrossRef]
- Paolucci, S.; Martinuzzi, A.; Scivoletto, G.; Smania, N.; Solaro, C.; Aprile, I.; Armando, M.; Bergamaschi, R.; Berra, E.; Berto, G.; et al. Assessing and treating pain associated with stroke, multiple sclerosis, cerebral palsy, spinal cord injury and spasticity. Evidence and recommendations from the Italian Consensus Conference on Pain in Neurorehabilitation. Eur. J. Phys. Rehabil. Med. 2016, 52, 827–840. [Google Scholar]
- Parker, H.A.; Rapport, L.J.; Williams, M.W.; Hanks, R.A.; Lumley, M.A.; Bogg, T. Functional independence after acquired brain injury: Prospective effects of health self-efficacy and cognitive impairment. Rehabil. Psychol. 2018, 63, 595–603. [Google Scholar] [CrossRef]
- Pérez-de la Cruz, S. Influence of an Aquatic Therapy Program on Perceived Pain, Stress, and Quality of Life in Chronic Stroke Patients: A Randomized Trial. Int. J. Env. Res. Public Health 2020, 17, 4796. [Google Scholar] [CrossRef]
- Pérez-Rodríguez, M.; Pérez-Tejero, J.; García-Hernández, J.J.; Franco, E.; Coterón, J. La actividad física en personas con daño cerebral adquirido en la fase crónica: Influencia sobre la salud en relación a la calidad de vida. Psicol. Del. Deporte 2020, 29, 16–23. [Google Scholar]
- Perry, S.A.; Coetzer, R.; Saville, C.W.N. The effectiveness of physical exercise as an intervention to reduce depressive symptoms following traumatic brain injury: A meta-analysis and systematic review. Neuropsychol. Rehabil. 2018, 10, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Pescatello, L.S.; Riebe, D.; Thompson, P.D. ACSM’s Guidelines for Exercise Testing and Prescription; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2014. [Google Scholar]
- Proctor, C.J.; Best, L.A. Social and psychological influences on satisfaction with life after brain injury. Disabil. Health J. 2019, 12, 387–393. [Google Scholar] [CrossRef] [PubMed]
- Quemada, J.I.; Ruíz, M.J.; Bori, I.; Gangoiti, L.; Marin, J. Modelo de Atención a las Personas con Daño Cerebral; Ministerio de Trabajo y Asuntos Sociales Secretaría de Estado de Servicios Sociales, Familias y Discapacidad; Instituto de Mayores y Servicios Sociales (IMSERSO): Madrid, Spain, 2007. [Google Scholar]
- Rabinowitz, A.R.; Levin, H.S. Cognitive sequelae of traumatic brain injury. Psychiatr. Clin. N. Am. 2014, 37, 1. [Google Scholar] [CrossRef] [PubMed]
- Raggi, A.; Leonardi, M.; Covelli, V.; Sattin, D.; Scaratti, C.; Schiavolin, S.; Willems, M.; Meucci, P. The ICF as a framework to collect and interpret data on the extent and variety of disability in neurological conditions. NeuroRehabilitation 2014, 14, 1186. [Google Scholar] [CrossRef] [PubMed]
- Reavenall, S.; Blake, H. Determinants of physical activity participation following traumatic brain injury. Int. J. Ther. Rehabil. 2010, 17, 360–369. [Google Scholar] [CrossRef]
- Reina, R.; Sanz, D. Actividades Físicas y Deportes Adaptados Para Personas con Discapacidad; Paidotribo: Barcelona, Spain, 2012. [Google Scholar]
- Rimmer, J.H. Use of the ICF in identifying factors that impact participation in physical activity/rehabilitation among people with disabilities. Disabil. Rehabil. 2006, 28, 1087–1095. [Google Scholar] [CrossRef] [PubMed]
- Ríos-Lago, M.; Muñoz-Céspedes, J.M.; Paúl-Lapedriza, N. Alteraciones de la atención tras daño cerebral traumático: Evaluación y rehabilitación. Rev. Neurol. 2007, 44, 291–0297. [Google Scholar] [CrossRef]
- Rosenfeldt, A.B.; Linder, S.M.; Davidson, S.; Clark, C.; Zimmerman, N.M.; Lee, J.J.; Alberts, J.L. Combined Aerobic Exercise and Task Practice Improve Health-Related Quality of Life Poststroke: A Preliminary Analysis. Arch. Phys. Med. Rehabil. 2019, 100, 923–930. [Google Scholar] [CrossRef]
- Saunders, D.H.; Sanderson, M.; Hayes, S.; Kilrane, M.; Greig, C.A.; Brazzelli, M.; Mead, G.E. Physical fitness training for stroke patients. Cochrane Database Syst. Rev. 2016, 3, CD003316. [Google Scholar] [CrossRef]
- Sexton, E.; McLoughlin, A.; Williams, D.J.; Merriman, N.A.; Donnelly, N.; Rohde, D.; Hickey, A.; Wren, M.-A.; Bennett, K. Systematic review and meta-analysis of the prevalence of cognitive impairment no dementia in the first year post-stroke. Eur. Stroke J. 2019, 4, 160–171. [Google Scholar] [CrossRef]
- Sheehy, L.; Taillon-Hobson, A.; Sveistrup, H.; Bilodeau, M.; Yang, C.; Finestone, H. Sitting balance exercise performed using Virtual Reality training on a stroke rehabilitation inpatient service: A randomized controlled study. PMR 2020, 12, 754–765. [Google Scholar] [CrossRef]
- Sommerfeld, D.K.; Eek, E.U.-B.; Svensson, A.-K.; Holmqvist, L.W.; von Arbin, M.H. Spasticity after stroke: Its occurrence and association with motor impairments and activity limitations. Stroke 2004, 35, 134–139. [Google Scholar] [CrossRef]
- Stiekema, A.P.M.; Winkens, I.; Ponds, R.; De Vugt, M.E.; Van Heugten, C.M. Finding a new balance in life: A qualitative study on perceived long-term needs of people with acquired brain injury and partners. Brain Inj. 2020, 34, 421–429. [Google Scholar] [CrossRef]
- Stroke Unit Trtialist’ Colaboration. Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst. Rev. 2013, 2013, CD000197. [Google Scholar] [CrossRef]
- Townsend, R.C.; Huntley, T.D.; Cushion, C.J.; Culver, D. Infusing disability into coach education and development: A critical review and agenda for change. Phys. Educ. Sport Pedagog. 2021, 10, 1–14. [Google Scholar] [CrossRef]
- Turner-Stokes, L.; Pick, A.; Nair, A.; Disler, P.B.; Wade, D.T. Multi-disciplinary rehabilitation for acquired brain injury in adults of working age. Cochrane Database Syst. Rev. 2015, 12, 124. [Google Scholar] [CrossRef]
- Tweedy, S.M. Taxonomic Theory and the ICF: Foundations for a Unified Disability Athletics Classification. Adapt. Phys. Act. Q. 2002, 19, 220–237. [Google Scholar] [CrossRef]
- Vander Werff, K.R. The Application of the International Classification of Functioning, Disability and Health to Functional Auditory Consequences of Mild Traumatic Brain Injury. Semin. Hear. 2016, 37, 216–232. [Google Scholar] [CrossRef][Green Version]
- Vanderbeken, I.; Kerckhofs, E. A systematic review of the effect of physical exercise on cognition in stroke and traumatic brain injury patients. NeuroRehabilitation 2017, 40, 33–48. [Google Scholar] [CrossRef]
- Verdugo, M.A.; Fernández, M.; Gómez, L.E.; Amor, A.M.; Aza, A. Predictive factors of quality of life in acquired brain injury. Int. J. Clin. Health Psychol. 2019, 19, 189–197. [Google Scholar] [CrossRef] [PubMed]
- West, C.; Bowen, A.; Hesketh, A.; Vail, A. Interventions for motor apraxia following stroke. Cochrane Database Syst. Rev. 2008, 1, Cd004132. [Google Scholar] [CrossRef] [PubMed]
- CDC. International Classification of Functionality Disability and Health: ICF; CDC: Atlanta, GA, USA, 2010. [Google Scholar]
- Williams, M.W.; Rapport, L.J.; Hanks, R.A.; Parker, H.A. Engagement in rehabilitation therapy and functional outcomes among individuals with acquired brain injuries. Disabil. Rehabil. 2021, 43, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Winstein, C.J.; Stein, J.; Arena, R.; Bates, B.; Cherney, L.R.; Cramer, S.C.; Deruyter, F.; Eng, J.J.; Fisher, B.; Harvey, R.L. Guidelines for adult stroke rehabilitation and recovery: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2016, 47, e98–e169. [Google Scholar] [CrossRef]
- World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [CrossRef]
- Yoo, J.S.; Hwang, A.R.; Lee, H.C.; Kim, C.J. Development and validation of a computerized exercise intervention program for patients with type 2 diabetes mellitus in Korea. Yonsei. Med. J. 2003, 44, 892–904. [Google Scholar] [CrossRef]
- Zhang, Q.; Schwade, M.; Smith, Y.; Wood, R.; Young, L. Exercise-based interventions for post-stroke social participation: A systematic review and network meta-analysis. Int. J. Nurs. Stud. 2020, 111, 103738. [Google Scholar] [CrossRef]
| Mental Function (b1) |
| Increase time required for execution of movements |
| Establish progression in the performance of dual tasks |
| Simplify task or progressively increase the number of rules to be assimilated |
| Design exercises or tasks involving both motor and cognitive actions |
| Select global-specific or specific-global method according to the cognitive deficits |
| Vary the use of methodological resources (game, exercise, circuit) |
| Sensory Functions and Pain (b2) |
| Perform pain-free movement |
| Use bright colors and varied shapes |
| Select material locations according to deficits and using auditory or visual references |
| Regulate sounds and noises before hyperacusis |
| Voice and Speech Function (b3) |
| Use visual elements through body expression, pictograms, or images |
| Use brief explanations, concise feedback, and positive reinforcement during task |
| Establish keywords that facilitate technical-user communication |
| Simplify task or progressively increase the number of rules to be assimilated |
| Functions of the cardiovascular, hematological, immunological, and respiratory system (b4); functions of the digestive, metabolic, and endocrine systems (b5), and genitourinary and reproductive functions (b6) |
| Control the maximum heart rate |
| Assess possibility if necessary of analysis of the Vo2max through stress test |
| Assess the need to use a heart rate monitor |
| Neuromusculoskeletal and movement-related functions (b7) |
| Know the alteration of static and dynamic balance: walking autonomy. Use technical support, do activity in safe and supervised space |
| Assess muscle action and control and control the articular range in which tremor occurs |
| Understand and restrict movement of the joints and works without pain. |
| Upper limb: check possibility of gripping with paretic hand with different materials and positions |
| Lower limb: assess clubfoot, splints or orthotics. Special care in aquatic activities with the possibility of using weights to hold the foot |
| Know the potential for hand-eye and foot-eye coordination |
| Ask the dominant side if has changed due to hemiparesis or hemiplegia |
| Know the alteration of static and dynamic equilibrium: autonomy |
| Functions of the skin and related structures (b8) |
| Regulation of water temperature to avoid spasticity |
| Take into account sensory lack on the affected side when making transfers, grips, and supports |
| Check that the auxiliary material does not cause injury to the skin and related structures (Ex: fins with socks) |
| Know if there is hypersensitivity in the affected area and if there is, avoid catching him |
| Activity and Participation |
|---|
| Choose aquatic activity if there is a risk of falling |
| Select different teaching methods to ensure the assimilation of basic concepts |
| Design task that can be performed sitting, standing or moving |
| Evaluate needs and determine ratio for each person |
| Assess the level of involvement in practice and set objectives |
| Generate relaxed and motivating environment |
| Design tasks that have transfer to activities of daily life |
| Environmental Factors |
|---|
| Analyze the place of practice ensuring universal accessibility |
| Incorporate education in values into activities |
| Know and empathize with the personal situation of each user |
| Maintain a good relationship with the multidisciplinary team and the family |
| Relevance | Adequation | |||
|---|---|---|---|---|
| Criteria | X | XS | X | XS |
| Body Function | 4.54 | 0.97 | 4.46 | 1.50 |
| Establish progression in the performance of dual task | 4.92 | 0.64 | 4.92 | 0.64 |
| Simplify task or progressively increase the number of rules to be assimilated | 4.85 | 0.69 | 4.69 | 0.75 |
| Design exercises or task involving both motor and cognitive actions | 4.77 | 0.93 | 4.77 | 0.93 |
| Select global-specific or specific-global method according to the cognitive deficits | 4.38 | 1.12 | 4.38 | 1.12 |
| Vary in the use of methodological resources | 4.69 | 0.95 | 4.69 | 0.95 |
| 5.08 | 0.862 | 5.15 | 0.80 | |
| Use bright colors and varied shapes | 4.46 | 1.33 | 4.38 | 1.19 |
| Select material locations according to deficits and using auditory or visual references | 4.85 | 0.80 | 4.85 | 0.69 |
| Regulate sounds and noises before hyperacusis | 4.46 | 1.33 | 4.54 | 1.13 |
| Use visual elements through body expression, pictograms or images | 4.31 | 1.60 | 4.38 | 1.56 |
| Use brief explanations, concise feedback, and positive reinforcement during task | 4.54 | 1.56 | 4.62 | 1.50 |
| Establish keywords that facilitate technical-user communication | 4.62 | 1.50 | 4.54 | 1.51 |
| Control of the maximum heart rate | 5.00 | 0.82 | 4.77 | 1.01 |
| Assess possibility if necessary of analysis of the Vo2max through stress test | 4.92 | 1.19 | 4.69 | 1.44 |
| Simplify task or progressively increase the number of rules to be assimilated | 5.31 | 0.63 | 5.08 | 0.96 |
| Assess the need to use an heart rate monitor | 4.46 | 1.94 | 4.62 | 1.90 |
| Select material locations according to deficits and using auditory or visual references | 4.69 | 1.25 | 4.77 | 1.09 |
| Know the alteration of static and dynamic balance: walking autonomy. | 5.00 | 0.91 | 5.00 | 0.91 |
| Muscular control | 4.85 | 1.29 | 4.92 | 1.26 |
| Understand and restrict movement of the joints and works without pain. | 5.08 | 1.12 | 5.08 | 1.12 |
| Upper limb functionality | 5.23 | 0.73 | 5.15 | 0.90 |
| Lower limb functionality | 5.15 | 0.80 | 5.23 | 0.73 |
| Know the potential for hand-eye and foot-eye coordination | 4.77 | 1.90 | 4.92 | 0.95 |
| Ask if the dominant side has changed due to hemiparesis or hemiplegia | 4.77 | 0.83 | 4.69 | 0.86 |
| Regulation of water temperature to avoid spasticity | 4.92 | 1.26 | 4.92 | 1.12 |
| Regulate sounds and noises before hyperacusia | 4.85 | 0.99 | 4.77 | 1.09 |
| Check that the auxiliary material does not cause injury to the skin and related structures | 5.08 | 0.49 | 4.92 | 0.64 |
| Know if there is hypersensitivity in the affected area | 5.08 | 0.49 | 4.92 | 0.64 |
| Activity and Participation | ||||
| Choose aquatic activity if there is a risk of falling | 4.38 | 1.38 | 4.08 | 1.50 |
| Select different teaching methods to ensure the assimilation of basic concepts | 4.54 | 1.05 | 4.62 | 1.04 |
| Design task that can be performed sitting, standing or moving | 5.08 | 0.64 | 5.00 | 0.71 |
| Evaluate needs and determine ratio for each person | 5.00 | 0.58 | 5.00 | 0.58 |
| Assess the level of involvement in practice and set objectives | 4.69 | 0.75 | 4.69 | 0.63 |
| Generate relaxed and motivating environment | 4.54 | 0.88 | 4.69 | 0.75 |
| Design tasks that have transfer to activities of daily life | 4.46 | 4.13 | 4.62 | 0.77 |
| Environmental Factors | ||||
| Analyze the place of practice ensuring universal accessibility | 4.54 | 0.88 | 4.54 | 0.78 |
| Incorporate education in values into activities | 4.08 | 1.04 | 4.38 | 0.65 |
| Know and empathize with the personal situation of each user | 4.23 | 0.93 | 4.38 | 0.88 |
| Maintain a good relationship with the multidisciplinary team and the family | 4.85 | 0.38 | 4.92 | 0.28 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pérez-Rodríguez, M.; García-Hernández, J.J.; García-Gómez, S.; Pérez-Tejero, J. Exercise for People with Acquired Brain Injury: An ICF Perspective. Appl. Sci. 2022, 12, 3862. https://doi.org/10.3390/app12083862
Pérez-Rodríguez M, García-Hernández JJ, García-Gómez S, Pérez-Tejero J. Exercise for People with Acquired Brain Injury: An ICF Perspective. Applied Sciences. 2022; 12(8):3862. https://doi.org/10.3390/app12083862
Chicago/Turabian StylePérez-Rodríguez, Marta, Juan José García-Hernández, Saleky García-Gómez, and Javier Pérez-Tejero. 2022. "Exercise for People with Acquired Brain Injury: An ICF Perspective" Applied Sciences 12, no. 8: 3862. https://doi.org/10.3390/app12083862
APA StylePérez-Rodríguez, M., García-Hernández, J. J., García-Gómez, S., & Pérez-Tejero, J. (2022). Exercise for People with Acquired Brain Injury: An ICF Perspective. Applied Sciences, 12(8), 3862. https://doi.org/10.3390/app12083862






