Anterior Incisal Onlay—A Minimally Invasive Non-Surgical Approach to Correct an Esthetic Complication of an Implant Supported Crown in the Anterior Zone
Abstract
1. Introduction
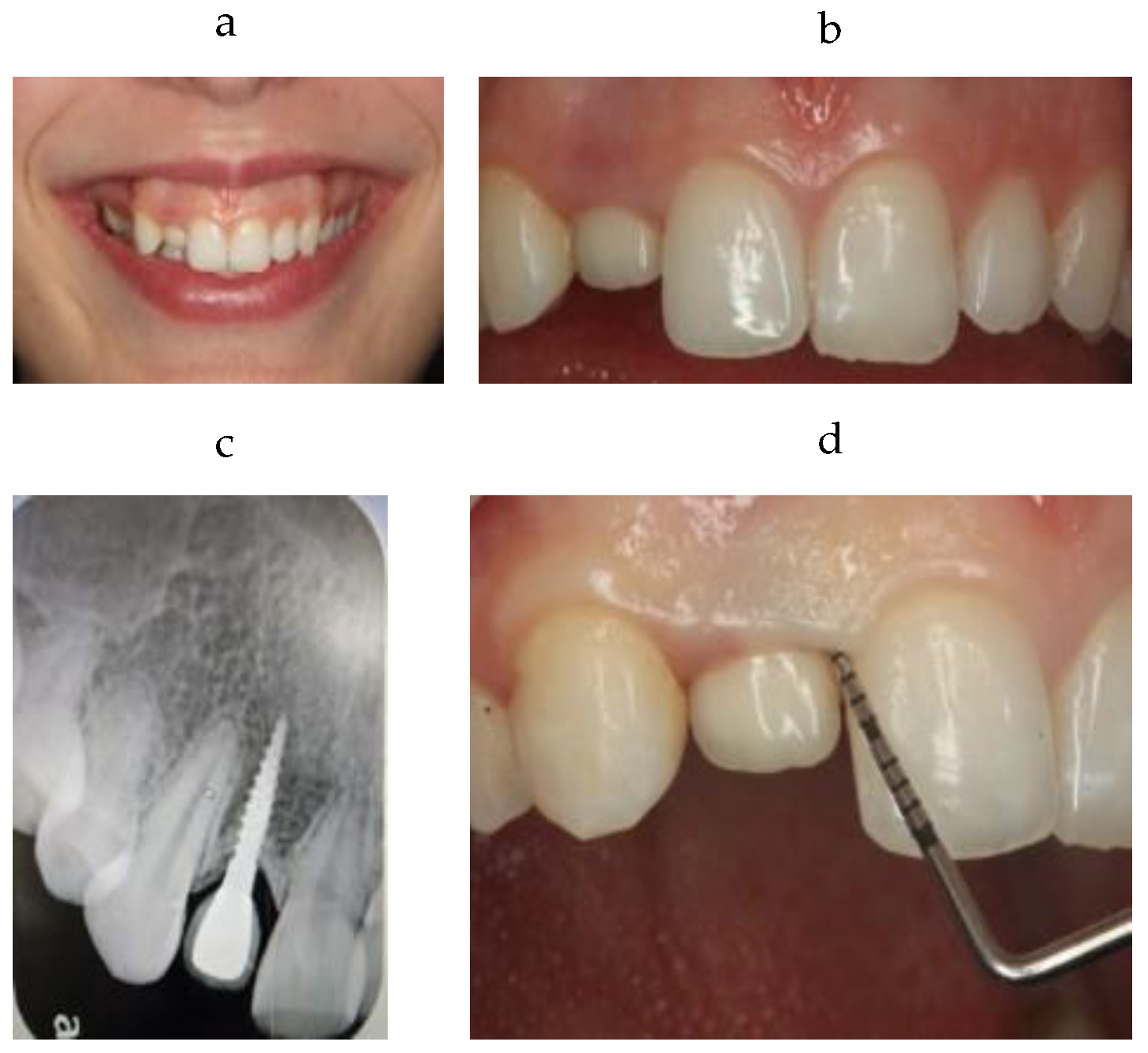
2. Clinical Case
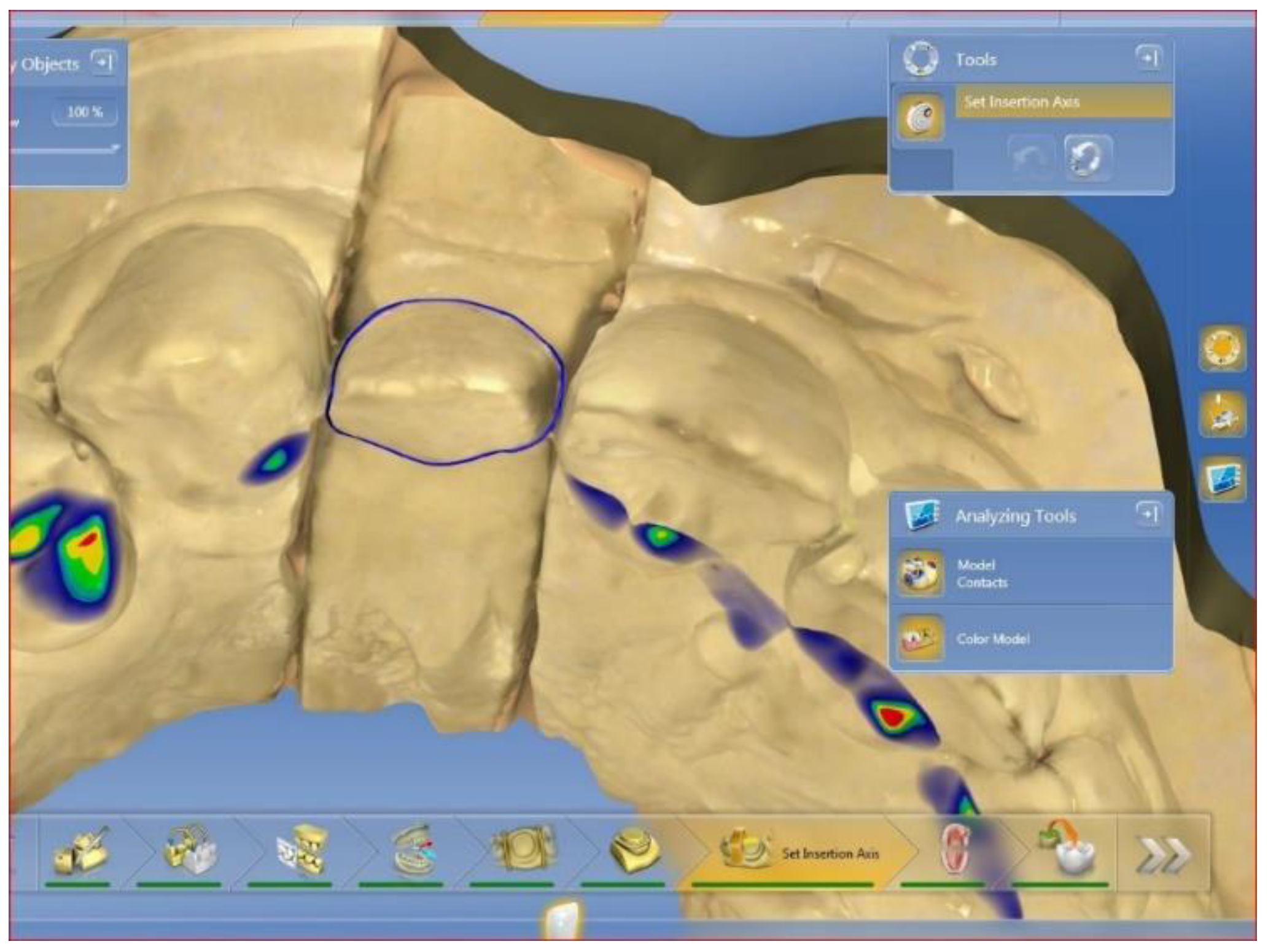
3. Treatment Plan
4. Treatment Sequence
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Op Heij, D.G.; Opdebeeck, H.; van Steenberghe, D.; Quirynen, M. Age as compromising factor for implant insertion. Periodontology 2000 2003, 33, 172–844. [Google Scholar] [CrossRef] [PubMed]
- Daftary, F.; Mahallati, R.; Bahat, O.; Sullivan, R.M. Lifelong craniofacial growth and the implications for Osseo integrated implants. Int. J. Oral Maxillofac. Implant. 2013, 28, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Cocchetto, R.; Pradies, G.; Celletti, R.; Canullo, L. Continuous craniofacial growth in adult patients treated with dental implants in the anterior maxilla. Clin. Implant Dent. Relat. Res. 2019, 21, 627–634. [Google Scholar] [CrossRef] [PubMed]
- Schwartz-Arad, D.; Bichacho, N. Effect of Age on Single Implant Submersion Rate in the Central Maxillary Incisor Region: A Long-Term Retrospective Study. Clin. Implant Dent. Relat. Res. 2013, 17, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Barrachina-Diez, J.M.; Tashkandi, E.; Stampf, S.; Att, W. Long-term outcome of one-piece implants. Part I: Implant characteristics and loading protocols. A systematic literature review with meta-analysis. Int. J. Oral Maxillofac. Implant. 2013, 28, 503–518. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tallarico, M.; Caneva, M.; Meloni, S.M.; Xhanari, E.; Omori, Y.; Canullo, L. Survival and Success Rates of Different Shoulder Designs: A Systematic Review of the Literature. Int. J. Dent. 2018, 2018, 6812875. [Google Scholar] [CrossRef] [PubMed]
- Silberberg, N.; Goldstein, M.; Smidt, A. Excessive gingival display–etiology, diagnosis, and treatment modalities. Quintessence Int. 2009, 40, 809–818. [Google Scholar] [PubMed]
- Strasding, M.; Fehmer, V.; Pjetursson, B.E.; Sailer, I. Extending the service life of existing dental restorations with esthetic and functional limitations. J. Prosthet. Dent. 2018, 119, 893–896. [Google Scholar] [CrossRef] [PubMed]
- Blum, I.R.; Jagger, D.C.; Wilson, N.H. Defective dental restorations: To repair or not to repair? Part 2: All–ceramics and porcelain fused to metal systems. Dent. Update 2011, 38, 150–158. [Google Scholar] [CrossRef] [PubMed]
- Zandinejad, A.; Lin, W.S.; Atarodi, M.; Abdel-Azim, T.; Metz, M.J.; Morton, D. Digital workflow for virtually designing and milling ceramic lithium disilicate veneers: A clinical report. Oper. Dent. 2015, 40, 241–246. [Google Scholar] [CrossRef] [PubMed]
- Vidal, P.C.; Utrilla, T.M.; Souza, A.J. Surface Treatment of Lithium Disilicate with Different Concentrations of Hydrofluoric Acid and Orthophosphoric Acid. J. Dent. Sci. 2019, 18, 1128–1137. [Google Scholar]
- Straface, A.; Rupp, L.; Gintaute, A.; Fischer, J.; Zitzmann, N.U.; Rohr, N. HF etching of CAD/CAM materials: Influence of HF concentration and etching time on shear bond strength. Head Face Med. 2019, 15, 21. [Google Scholar] [CrossRef] [PubMed]
- Moura, D.M.D.; Araújo, A.M.M.D.; Souza, K.B.D.; Veríssimo, A.H.; Tribst, J.P.M.; Souza, R.O.D.A. Hydrofluoric acid concentration, time and use of phosphoric acid on the bond strength of feldspathic ceramics. Braz. Oral Res. 2020, 34, e018. [Google Scholar] [CrossRef] [PubMed]
- Butera, A.; Gallo, S.; Pascadopoli, M.; Maiorani, C.; Milone, A.; Alovisi, M.; Scribante, A. Paraprobiotics in non-surgical periodontal therapy: Clinical and microbiological aspects in a 6-month follow-up domiciliary protocol for oral hygiene. Microorganisms 2022, 10, 337. [Google Scholar] [CrossRef] [PubMed]
- Butera, A.; Gallo, S.; Pascadopoli, M.; Luraghi, G.; Scribante, A. Ozonized water administration in peri-implant mucositis sites: A randomized clinical trial. Appl. Sci. 2021, 11, 7812. [Google Scholar] [CrossRef]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zabrovsky, A.; Bar-on, H.; Beyth, N.; Smidt, A.; Ben-Gal, G. Anterior Incisal Onlay—A Minimally Invasive Non-Surgical Approach to Correct an Esthetic Complication of an Implant Supported Crown in the Anterior Zone. Appl. Sci. 2022, 12, 3808. https://doi.org/10.3390/app12083808
Zabrovsky A, Bar-on H, Beyth N, Smidt A, Ben-Gal G. Anterior Incisal Onlay—A Minimally Invasive Non-Surgical Approach to Correct an Esthetic Complication of an Implant Supported Crown in the Anterior Zone. Applied Sciences. 2022; 12(8):3808. https://doi.org/10.3390/app12083808
Chicago/Turabian StyleZabrovsky, Asher, Hilit Bar-on, Nurit Beyth, Ami Smidt, and Gilad Ben-Gal. 2022. "Anterior Incisal Onlay—A Minimally Invasive Non-Surgical Approach to Correct an Esthetic Complication of an Implant Supported Crown in the Anterior Zone" Applied Sciences 12, no. 8: 3808. https://doi.org/10.3390/app12083808
APA StyleZabrovsky, A., Bar-on, H., Beyth, N., Smidt, A., & Ben-Gal, G. (2022). Anterior Incisal Onlay—A Minimally Invasive Non-Surgical Approach to Correct an Esthetic Complication of an Implant Supported Crown in the Anterior Zone. Applied Sciences, 12(8), 3808. https://doi.org/10.3390/app12083808




