Autonomous Prostate Segmentation in 2D B-Mode Ultrasound Images
Abstract
:1. Introduction
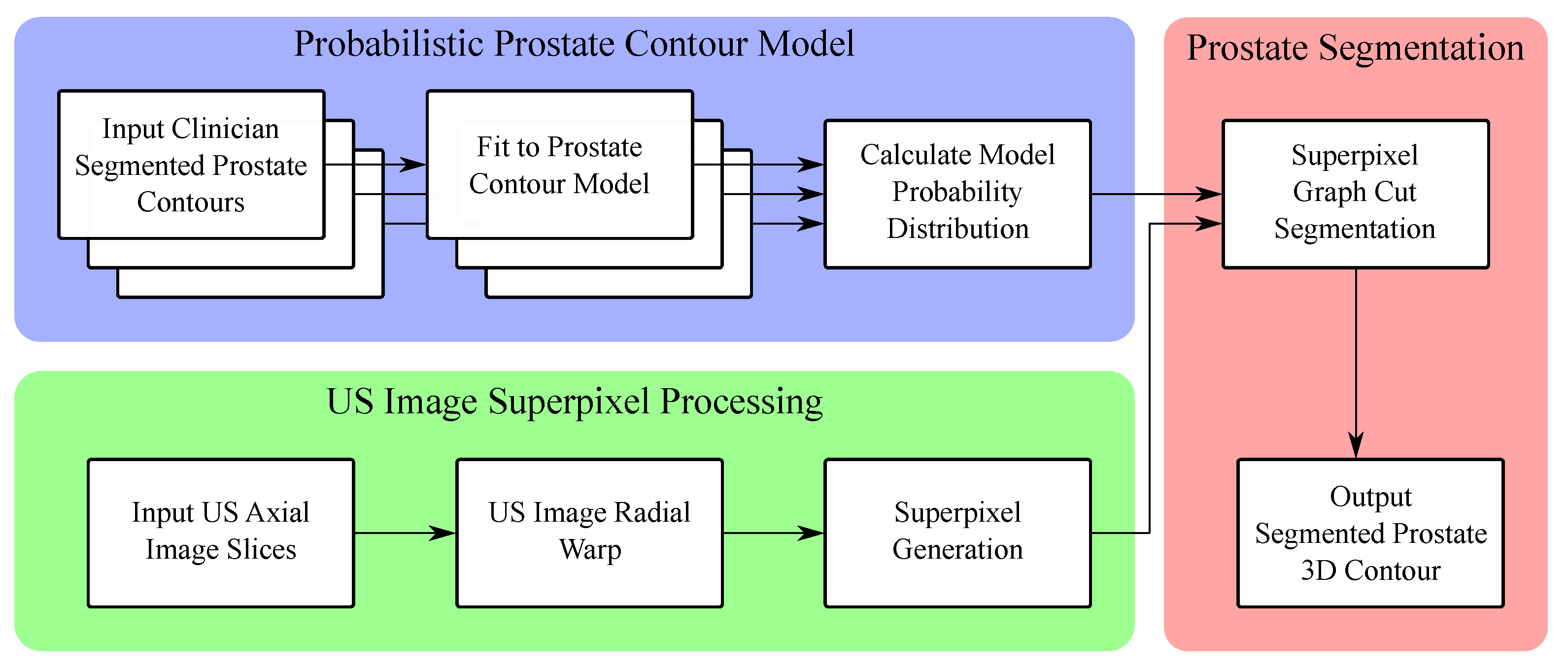
Contributions and Outline
- It incorporates a novel superpixel-based pixel clustering algorithm that includes a secondary graph-based hierarchy to allow for graph-cut image segmentation at the superpixel level.
- A probabilistic prostate model is introduced, and through the use of this probabilistic modeling, the algorithm is highly flexible and can produce contours which statistically resemble the input manual contours from a particular clinician or group of clinicians.
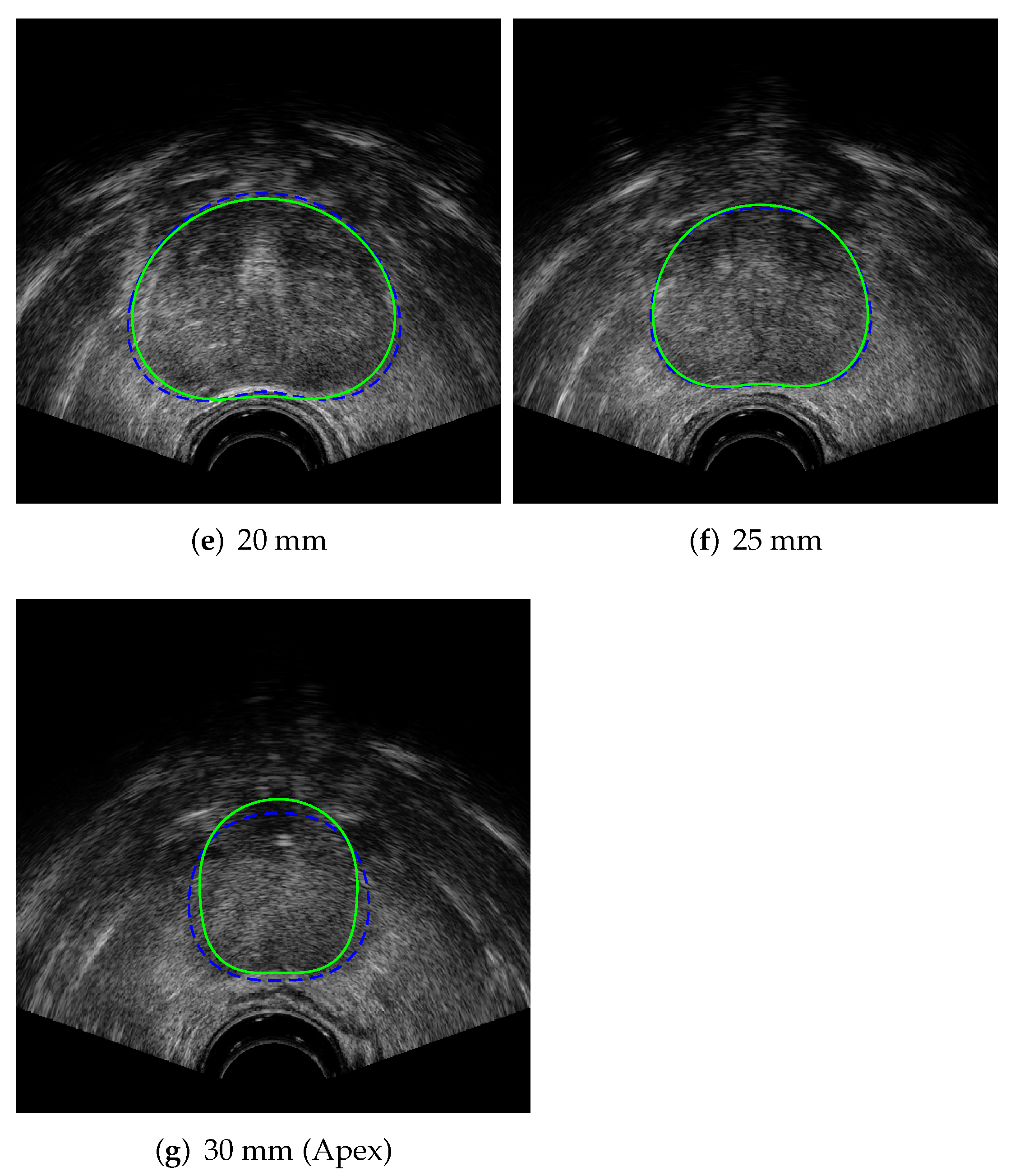
- The prostate contouring algorithm is fully autonomous, and does not require any user input for the segmentation process, nor any manual post-algorithm contour correction.
2. Background
3. Active Shape Prostate Contour Model
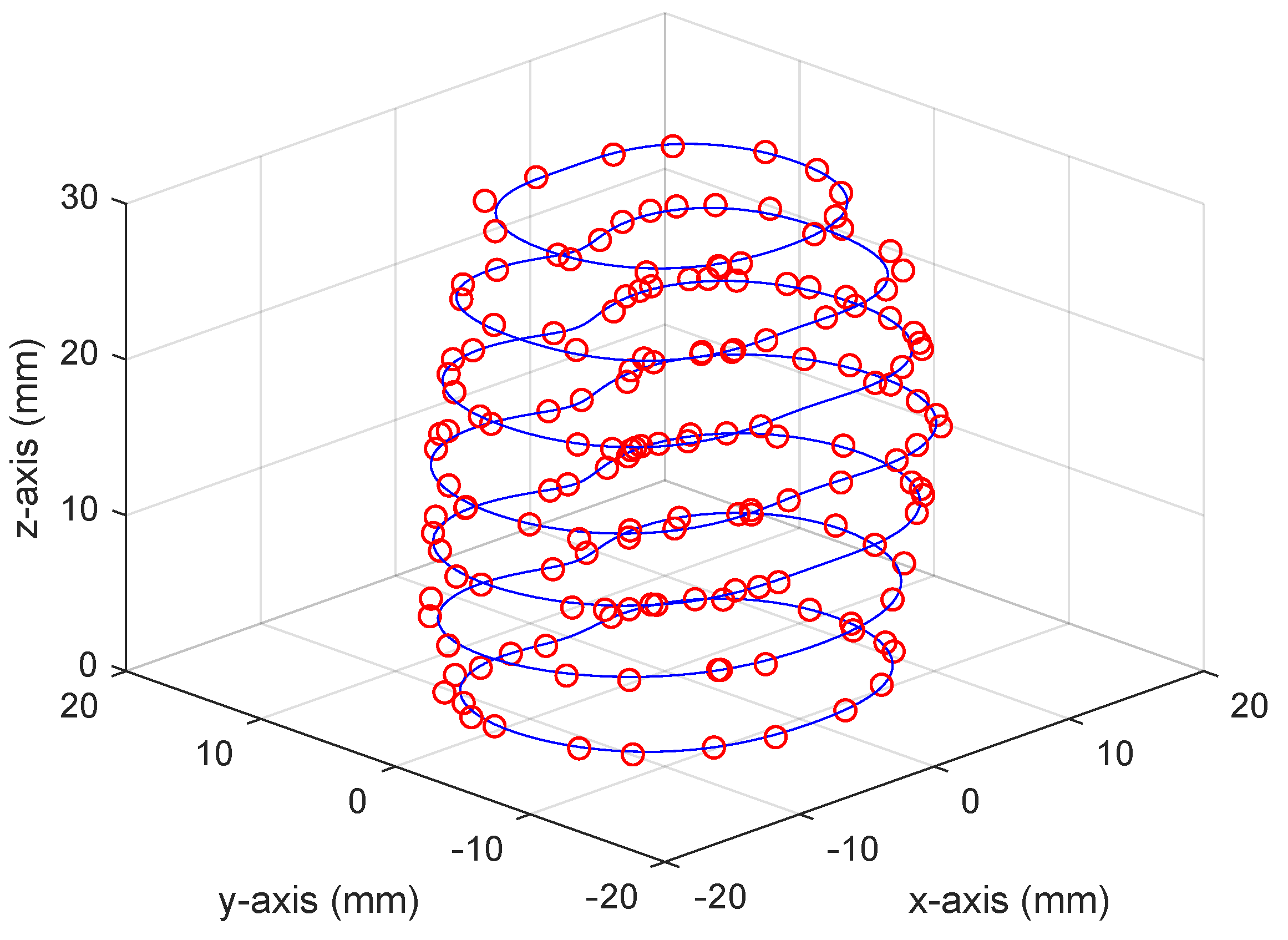
3.1. 3D Prostate Contour Model Fitting
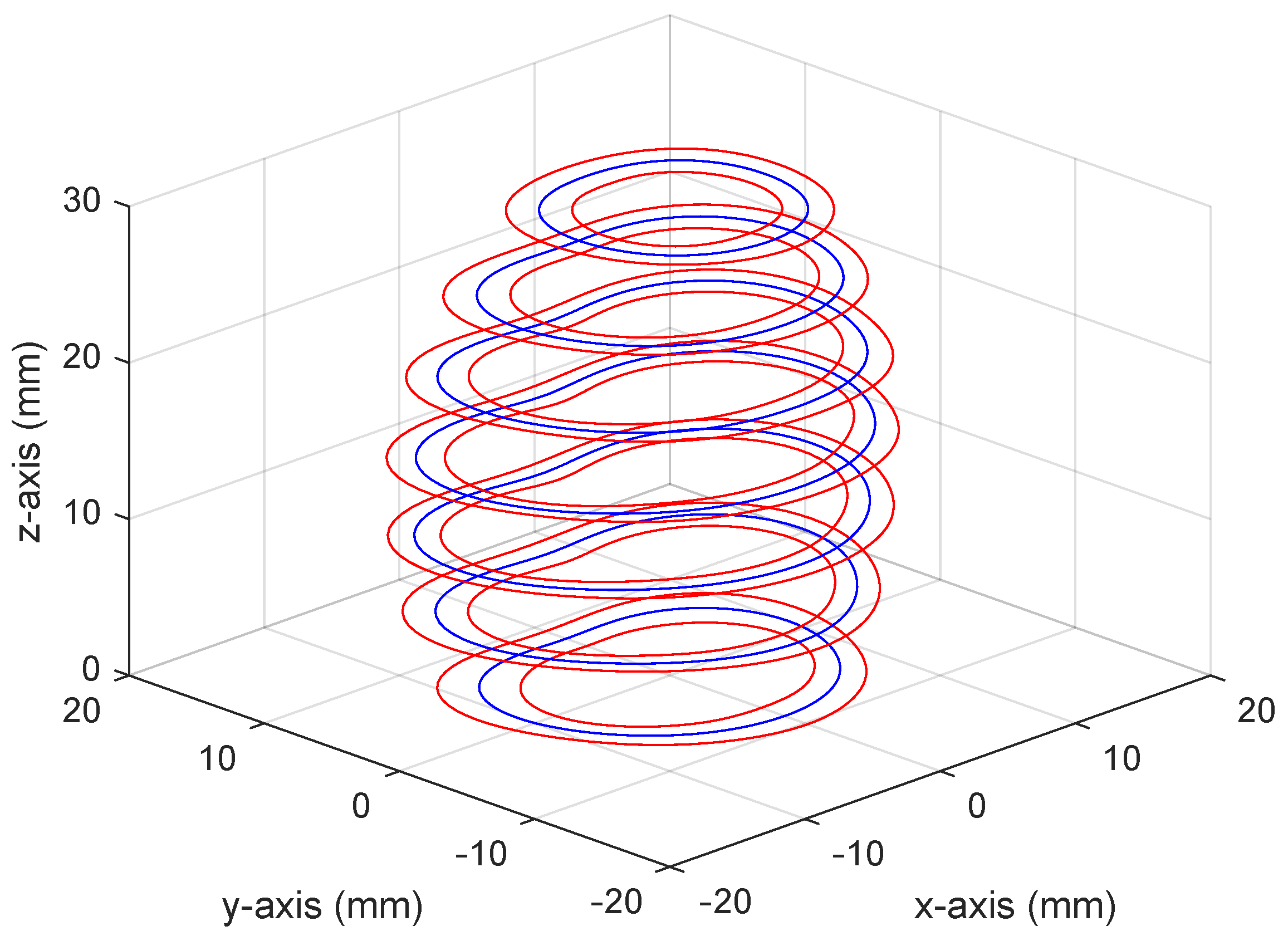
3.2. Statistical Prostate Shape Model
4. Superpixel Algorithm Incorporating Image Statistics
4.1. Pixel Clustering
4.2. Superpixel Regions
4.3. Superpixel Algorithm Outline
4.3.1. Cluster Update
4.3.2. Region Update
4.4. Algorithm Iteration and Output
5. Graph-Cut Segmentation
6. Results
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Appendix A. Appendix Ultrasound Image Preprocessing

References
- Potters, L.; Morgenstern, C.; Calugaru, E.; Fearn, P.; Jassal, A.; Presser, J.; Mullen, E. Adult Urology: Oncology: Prostate/Testis/Penis/Urethra: 12-year outcomes following permanent prostate brachytherapy in patients with clinically localized prostate cancer. J. Urol. 2005, 173, 1562–1566. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bowes, D.; Crook, J. A critical analysis of the long-term impact of brachytherapy for prostate cancer: A review of the recent literature. Curr. Opin. Urol. 2011, 21, 219–224. [Google Scholar] [CrossRef] [PubMed]
- Salembier, C.; Lavagnini, P.; Nickers, P.; Mangili, P.; Rijnders, A.; Polo, A.; Venselaar, J.; Hoskin, P. Tumour and target volumes in permanent prostate brachytherapy: A supplement to the ESTRO/EAU/EORTC recommendations on prostate brachytherapy. Radiother. Oncol. 2007, 83, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Rampun, A.; Tiddeman, B.; Zwiggelaar, R.; Malcolm, P. Computer aided diagnosis of prostate cancer: A texton based approach. Med. Phys. 2016, 43, 5412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, N.; Ahuja, N.; Bansal, R. Object segmentation using graph cuts based active contours. Comput. Vis. Image Underst. 2007, 107, 210–224. [Google Scholar] [CrossRef] [Green Version]
- Zhang, P.; Liang, Y.; Chang, S.; Fan, H. Kidney segmentation in CT sequences using graph cuts based active contours model and contextual continuity. Med. Phys. 2013, 40, 081905. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Udupa, J.K.; Alavi, A.; Torigian, D.A. GC-ASM: Synergistic Integration of Graph-Cut and Active Shape Model Strategies for Medical Image Segmentation. Comput. Vis. Image Underst. 2013, 117, 513–524. [Google Scholar] [CrossRef] [Green Version]
- Kremkau F, W.; Taylor K, J. Artifacts in ultrasound imaging. J. Ultrasound Med. 1986, 5, 227–237. [Google Scholar] [CrossRef]
- Noble, J.; Boukerroui, D. Ultrasound image segmentation: A survey. Med. Imaging IEEE Trans. 2006, 25, 987–1010. [Google Scholar] [CrossRef] [Green Version]
- Ghose, S.; Oliver, A.; Martí, R.; Lladó, X.; Vilanova, J.C.; Freixenet, J.; Mitra, J.; Sidibé, D.; Meriaudeau, F. A survey of prostate segmentation methodologies in ultrasound, magnetic resonance and computed tomography images. Comput. Methods Programs Biomed. 2012, 108, 262–287. [Google Scholar] [CrossRef] [Green Version]
- Singh, R.P.; Gupta, S.; Acharya, U.R. Segmentation of prostate contours for automated diagnosis using ultrasound images: A survey. J. Comput. Sci. 2017, 21, 223–231. [Google Scholar] [CrossRef]
- Ladak, H.M.; Mao, F.; Wang, Y.; Downey, D.B.; Steinman, D.A.; Fenster, A. Prostate boundary segmentation from 2D ultrasound images. Med. Phys. 2000, 27, 1777–1788. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Cardinal, H.N.; Downey, D.B.; Fenster, A. Semiautomatic three-dimensional segmentation of the prostate using two-dimensional ultrasound images. Med. Phys. 2003, 30, 887–897. [Google Scholar] [CrossRef] [PubMed]
- Hu, N.; Downey, D.B.; Fenster, A.; Ladak, H.M. Prostate boundary segmentation from 3D ultrasound images. Med. Phys. 2003, 30, 1648–1659. [Google Scholar] [CrossRef]
- Abolmaesumi, P.; Sirouspour, M.R. An interacting multiple model probabilistic data association filter for cavity boundary extraction from ultrasound images. IEEE Trans. Med. Imaging 2004, 23, 772–784. [Google Scholar] [CrossRef]
- Knoll, C.; Alcañiz, M.; Grau, V.; Monserrat, C.; Juan, M.C. Outlining of the prostate using snakes with shape restrictions based on the wavelet transform (Doctoral Thesis: Dissertation). Pattern Recognit. 1999, 32, 1767–1781. [Google Scholar] [CrossRef]
- Badiei, S.; Salcudean, S.E.; Varah, J.; Morris, W. Prostate Segmentation in 2D Ultrasound Images Using Image Warping and Ellipse Fitting. In Medical Image Computing and Computer-Assisted Intervention–MICCAI 2006; Larsen, R., Nielsen, M., Sporring, J., Eds.; Springer: Berlin/Heidelberg, Germany, 2006; Volume 4191, pp. 17–24. [Google Scholar] [CrossRef] [Green Version]
- Gong, L.; Pathak, S.D.; Haynor, D.R.; Cho, P.S.; Kim, Y. Parametric shape modeling using deformable superellipses for prostate segmentation. IEEE Trans. Med. Imaging 2004, 23, 340–349. [Google Scholar] [CrossRef]
- Mahdavi, S.S.; Chng, N.; Spadinger, I.; Morris, W.J.; Salcudean, S.E. Semi-automatic segmentation for prostate interventions. Med. Image Anal. 2011, 15, 226–237. [Google Scholar] [CrossRef] [Green Version]
- Cootes, T.; Taylor, C.; Cooper, D.; Graham, J. Active Shape Models-Their Training and Application. Comput. Vis. Image Underst. 1995, 61, 38–59. [Google Scholar] [CrossRef] [Green Version]
- Nouranian, S.; Mahdavi, S.; Spadinger, I.; Morris, W.; Salcudean, S.; Abolmaesumi, P. A Multi-Atlas-Based Segmentation Framework for Prostate Brachytherapy. Med. Imaging IEEE Trans. 2015, 34, 950–961. [Google Scholar] [CrossRef]
- Nouranian, S.; Ramezani, M.; Spadinger, I.; Morris, W.J.; Salcudean, S.E.; Abolmaesumi, P. Learning-Based Multi-Label Segmentation of Transrectal Ultrasound Images for Prostate Brachytherapy. IEEE Trans. Med. Imaging 2016, 35, 921–932. [Google Scholar] [CrossRef] [PubMed]
- Pathak, S.D.; Haynor, D.R.; Kim, Y. Edge-guided boundary delineation in prostate ultrasound images. IEEE Trans. Med. Imaging 2000, 19, 1211–1219. [Google Scholar] [CrossRef] [PubMed]
- Ding, M.; Chen, C.; Wang, Y.; Gyacskov, I.; Fenster, A. Prostate segmentation in 3D US images using the cardinal-spline-based discrete dynamic contour. In Medical Imaging 2003: Visualization, Image-Guided Procedures, and Display; Galloway, R.L., Jr., Ed.; International Society for Optics and Photonics, SPIE: San Diego, CA, USA, 2003; Volume 5029, pp. 69–76. [Google Scholar] [CrossRef]
- Chiu, B.; Freeman, G.H.; Salama, M.M.A.; Fenster, A. Prostate segmentation algorithm using dyadic wavelet transform and discrete dynamic contour. Phys. Med. Biol. 2004, 49, 4943–4960. [Google Scholar] [CrossRef] [PubMed]
- Hodge, A.C.; Fenster, A.; Downey, D.B.; Ladak, H.M. Prostate boundary segmentation from ultrasound images using 2D active shape models: Optimisation and extension to 3D. Comput. Methods Programs Biomed. 2006, 84, 99–113. [Google Scholar] [CrossRef]
- Tutar, I.B.; Pathak, S.D.; Gong, L.; Cho, P.S.; Wallner, K.; Kim, Y. Semiautomatic 3-D Prostate Segmentation from TRUS Images Using Spherical Harmonics. IEEE Trans. Med. Imaging 2006, 25, 1645–1654. [Google Scholar] [CrossRef]
- Shen, D.; Zhan, Y.; Davatzikos, C. Segmentation of prostate boundaries from ultrasound images using statistical shape model. IEEE Trans. Med. Imaging 2003, 22, 539–551. [Google Scholar] [CrossRef]
- Yan, P.; Xu, S.; Turkbey, B.; Kruecker, J. Discrete Deformable Model Guided by Partial Active Shape Model for TRUS Image Segmentation. IEEE Trans. Biomed. Eng. 2010, 57, 1158–1166. [Google Scholar] [CrossRef]
- Qin, X.; Li, X.; Liu, Y.; Lu, H.; Yan, P. Adaptive Shape Prior Constrained Level Sets for Bladder MR Image Segmentation. IEEE J. Biomed. Health Inform. 2014, 18, 1707–1716. [Google Scholar] [CrossRef]
- Achanta, R.; Shaji, A.; Smith, K.; Lucchi, A.; Fua, P.; Süsstrunk, S. SLIC Superpixels Compared to State-of-the-Art Superpixel Methods. IEEE Trans. Pattern Anal. Mach. Intell. 2012, 34, 2274–2282. [Google Scholar] [CrossRef] [Green Version]
- Ando, S. Image field categorization and edge/corner detection from gradient covariance. IEEE Trans. Pattern Anal. Mach. Intell. 2000, 22, 179–190. [Google Scholar] [CrossRef]
- Kaltenbach, H.M. A Concise Guide to Statistics; Springer: Berlin/Heidelberg, Germany; Basel, Switzerland, 2012. [Google Scholar]
- van der Heijden, F. Edge and line feature extraction based on covariance models. IEEE Trans. Pattern Anal. Mach. Intell. 1995, 17, 16–33. [Google Scholar] [CrossRef]
- Reyes-Aldasoro, C.; Bhalerao, A. The Bhattacharyya space for feature selection and its application to texture segmentation. Pattern Recognit. 2006, 39, 812–826. [Google Scholar] [CrossRef] [Green Version]
- Donoser, M.; Bischof, H. Using covariance matrices for unsupervised texture segmentation. In Proceedings of the 2008 19th International Conference on Pattern Recognition, Tampa, FL, USA, 8–11 December 2008; pp. 1–4. [Google Scholar] [CrossRef] [Green Version]
- Tsui, P.H.; Wan, Y.L.; Tai, D.I.; Shu, Y.C. Effects of Estimators on Ultrasound Nakagami Imaging in Visualizing the Change in the Backscattered Statistics from a Rayleigh Distribution to a Pre-Rayleigh Distribution. Ultrasound Med. Biol. 2015, 41, 2240–2251. [Google Scholar] [CrossRef] [PubMed]
- Tsui, P.H. Current status and future prospects of scattering statistics in ultrasound imaging. J. Med. Ultrasound 2016, 24, 83–85. [Google Scholar] [CrossRef] [Green Version]
- Destrempes, F.; Cloutier, G. A Critical Review and Uniformized Representation of Statistical Distributions Modeling the Ultrasound Echo Envelope. Ultrasound Med. Biol. 2010, 36, 1037–1051. [Google Scholar] [CrossRef]
- Boykov, Y.; Veksler, O. Graph Cuts in Vision and Graphics:Theories and Applications. In Handbook of Mathematical Models in Computer Vision; Springer: Boston, MA, USA, 2006. [Google Scholar]
- Smith, W.L.; Lewis, C.; Bauman, G.; Rodrigues, G.; D’Souza, D.; Ash, R.; Ho, D.; Venkatesan, V.; Downey, D.; Fenster, A. Prostate volume contouring: A 3D analysis of segmentation using 3DTRUS, CT, and MR. Int. J. Radiat. Oncol. 2007, 67, 1238–1247. [Google Scholar] [CrossRef]
- Liu, D.; Usmani, N.; Ghosh, S.; Kamal, W.; Pedersen, J.; Pervez, N.; Yee, D.; Danielson, B.; Murtha, A.; Amanie, J.; et al. Comparison of prostate volume, shape, and contouring variability determined from preimplant magnetic resonance and transrectal ultrasound images. Brachytherapy 2012, 11, 284–291. [Google Scholar] [CrossRef]











| Data Set | Average MSE (mm) | Average Max Abs Error (mm) | Range of Max Abs Error (mm) |
|---|---|---|---|
| US Contours | 0.611 (±0.165) | 1.519 (±0.310) | 0.679–2.031 |
| MR Contours | 0.616 (±0.167) | 1.565 (±0.305) | 0.794–2.124 |
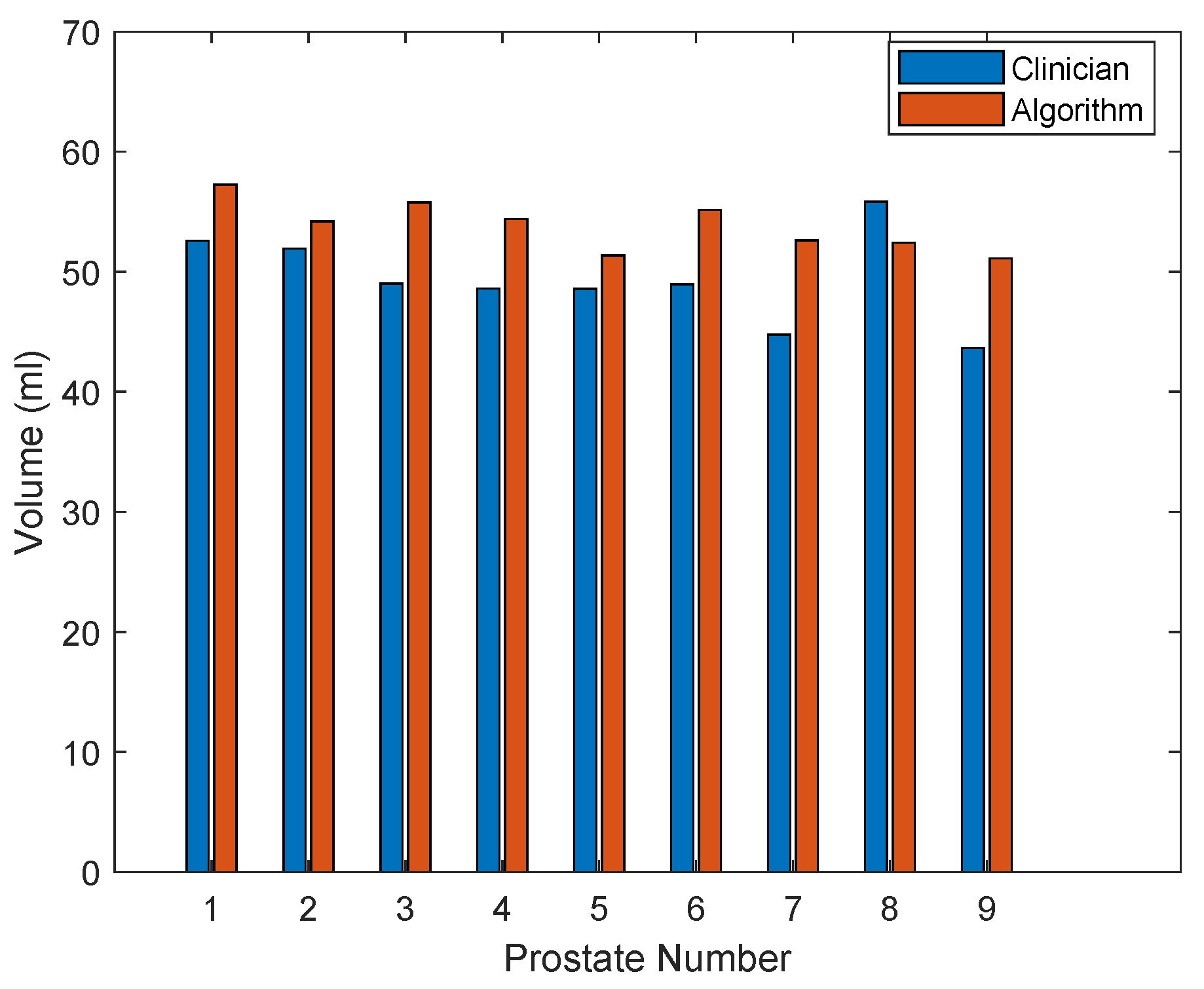
| Dataset | Mean Absolute Difference (mm) | Max Absolute Difference (mm) | Volume Difference (mL) | Volume Difference |
|---|---|---|---|---|
| Prostate 1 | 2.01 (±1.30) | 5.89 | 4.65 | 8.85 |
| Prostate 2 | 1.87 (±1.29) | 6.91 | 2.27 | 4.37 |
| Prostate 3 | 3.03 (±2.21) | 8.50 | 6.75 | 13.77 |
| Prostate 4 | 2.54 (±1.48) | 6.00 | 5.77 | 11.88 |
| Prostate 5 | 2.46 (±1.60) | 6.82 | 2.80 | 5.76 |
| Prostate 6 | 2.24 (±1.43) | 6.70 | 6.20 | 12.68 |
| Prostate 7 | 3.08 (±2.06) | 8.82 | 7.86 | 17.56 |
| Prostate 8 | 2.73 (±1.71) | 8.90 | -3.39 | 6.07 |
| Prostate 9 | 2.76 (±1.65) | 6.20 | 7.47 | 17.11 |
| Average | 2.52 (±1.66) | 7.19 (±1.22) | 4.49 (±3.53) | 10.89 (±4.90) |
| Dataset | Average Jaccard Index | Min Jaccard Index | Max Jaccard Index |
|---|---|---|---|
| Prostate 1 | 0.84 (±0.04) | 0.79 | 0.92 |
| Prostate 2 | 0.85 (±0.06) | 0.75 | 0.91 |
| Prostate 3 | 0.77 (±0.02) | 0.73 | 0.79 |
| Prostate 4 | 0.79 (±0.06) | 0.73 | 0.87 |
| Prostate 5 | 0.79 (±0.04) | 0.72 | 0.83 |
| Prostate 6 | 0.82 (±0.06) | 0.71 | 0.90 |
| Prostate 7 | 0.74 (±0.07) | 0.66 | 0.85 |
| Prostate 8 | 0.77 (±0.07) | 0.66 | 0.84 |
| Prostate 9 | 0.77 (±0.09) | 0.61 | 0.89 |
| Average | 0.79 (±0.07) | 0.71 (±0.05) | 0.87 (±0.04) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carriere, J.; Sloboda, R.; Usmani, N.; Tavakoli, M. Autonomous Prostate Segmentation in 2D B-Mode Ultrasound Images. Appl. Sci. 2022, 12, 2994. https://doi.org/10.3390/app12062994
Carriere J, Sloboda R, Usmani N, Tavakoli M. Autonomous Prostate Segmentation in 2D B-Mode Ultrasound Images. Applied Sciences. 2022; 12(6):2994. https://doi.org/10.3390/app12062994
Chicago/Turabian StyleCarriere, Jay, Ron Sloboda, Nawaid Usmani, and Mahdi Tavakoli. 2022. "Autonomous Prostate Segmentation in 2D B-Mode Ultrasound Images" Applied Sciences 12, no. 6: 2994. https://doi.org/10.3390/app12062994
APA StyleCarriere, J., Sloboda, R., Usmani, N., & Tavakoli, M. (2022). Autonomous Prostate Segmentation in 2D B-Mode Ultrasound Images. Applied Sciences, 12(6), 2994. https://doi.org/10.3390/app12062994







