After Total Knee Arthroplasty, Monitored Active Ankle Pumping Improves Lower Leg Circulation More Than Unmonitored Pumping: A Pilot Study
Abstract
:Featured Application
Abstract
1. Introduction
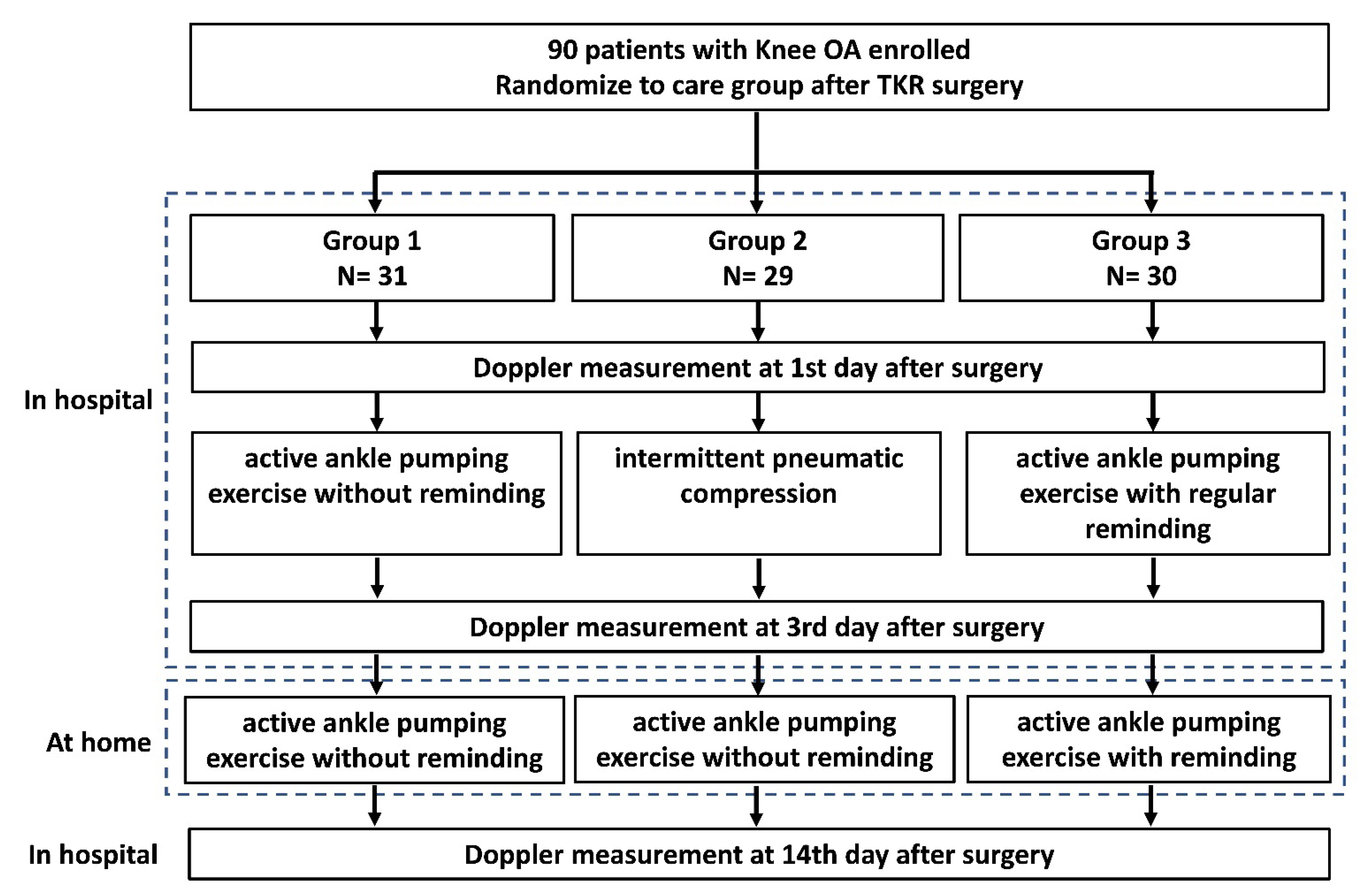
2. Materials and Methods
2.1. Ethics Statement
2.2. Study Subjects
2.3. Surgical Technique and Postoperative Nursing Care
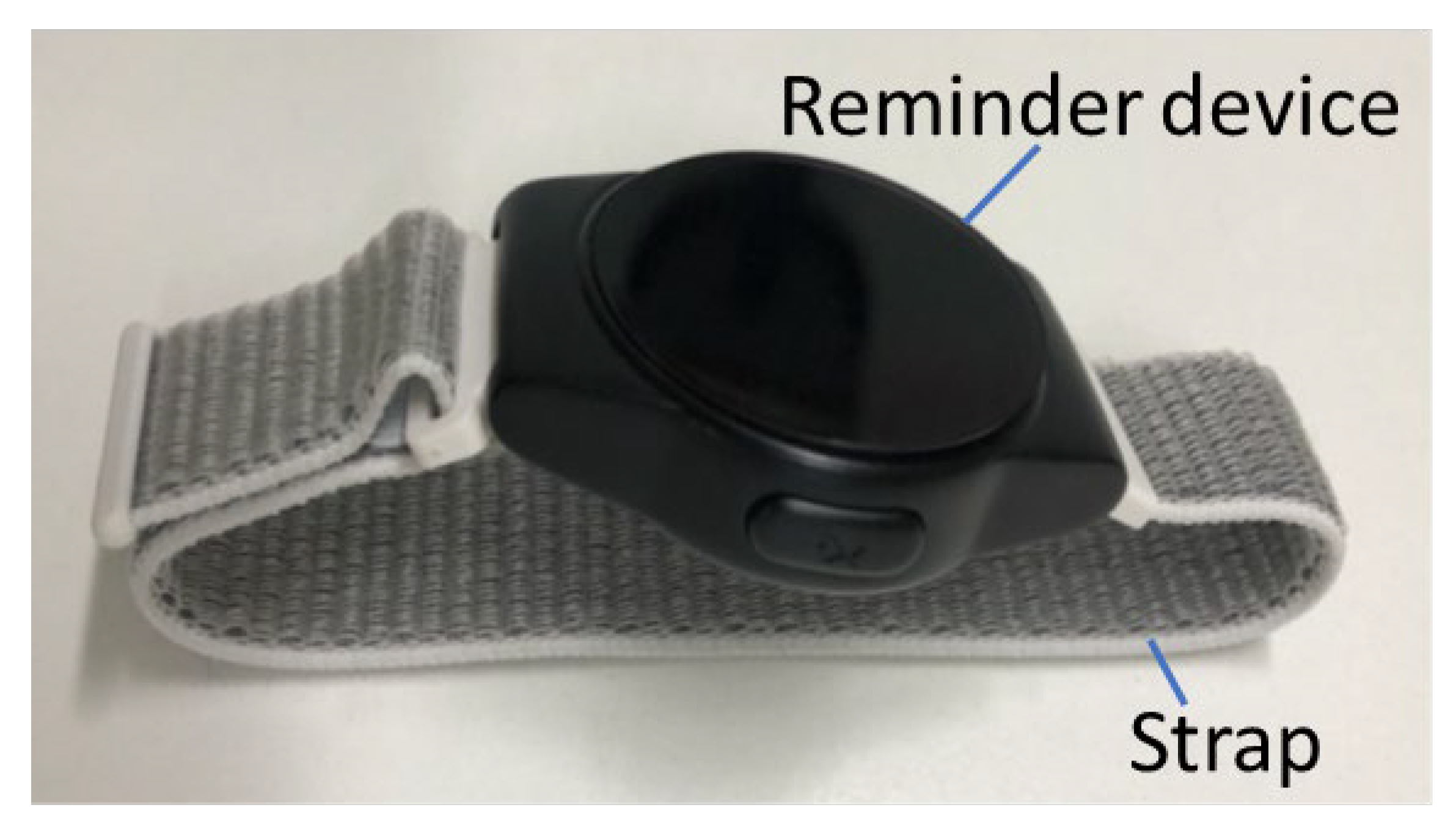
2.4. Intervention Method
2.5. Index for Sonographic Assessment of Lower Limb Veins
2.6. Follow-Up
2.7. Sample Size Calculation
2.8. Data Analysis
2.9. Limitations
3. Results
3.1. Baseline Characteristics
3.2. Peak Flow Velocity and Flow Volume
3.3. Stasis
3.4. Occurrence of DVT during Follow-Up
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Maradit Kremers, H.; Larson, D.R.; Crowson, C.S.; Kremers, W.K.; Washington, R.E.; Steiner, C.A.; Jiranek, W.A.; Berry, D.J. Prevalence of total hip and knee replacement in the united states. J. Bone Jt. Surg. Am. Vol. 2015, 97, 1386–1397. [Google Scholar] [CrossRef] [PubMed]
- Itou, J.; Kuwashima, U.; Itoh, M.; Okazaki, K. No difference in the incidence or location of deep venous thrombosis according to use of pharmacological prophylaxis following total knee arthroplasty. BMC Musculoskelet. Disord. 2021, 22, 819. [Google Scholar] [CrossRef] [PubMed]
- Fujita, S.; Hirota, S.; Oda, T.; Kato, Y.; Tsukamoto, Y.; Fuji, T. Deep venous thrombosis after total hip or total knee arthroplasty in patients in japan. Clin. Orthop. Relat. Res. 2000, 375, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Warren, J.A.; Sundaram, K.; Kamath, A.F.; Molloy, R.M.; Krebs, V.E.; Mont, M.A.; Piuzzi, N.S. Venous thromboembolism rates did not decrease in lower extremity revision total joint arthroplasty from 2008 to 2016. J. Arthroplast. 2019, 34, 2774–2779. [Google Scholar]
- Boylan, M.R.; Perfetti, D.C.; Kapadia, B.H.; Delanois, R.E.; Paulino, C.B.; Mont, M.A. Venous thromboembolic disease in revision vs primary total knee arthroplasty. J. Arthroplast. 2017, 32, 1996–1999. [Google Scholar] [CrossRef] [PubMed]
- Shahi, A.; Chen, A.F.; Tan, T.L.; Maltenfort, M.G.; Kucukdurmaz, F.; Parvizi, J. The incidence and economic burden of in-hospital venous thromboembolism in the united states. J. Arthroplast. 2017, 32, 1063–1066. [Google Scholar] [CrossRef]
- Shahi, A.; Bradbury, T.L.; Guild, G.N., 3rd; Saleh, U.H.; Ghanem, E.; Oliashirazi, A. What are the incidence and risk factors of in-hospital mortality after venous thromboembolism events in total hip and knee arthroplasty patients? Arthroplast. Today 2018, 4, 343–347. [Google Scholar] [CrossRef]
- Matharu, G.S.; Kunutsor, S.K.; Judge, A.; Blom, A.W.; Whitehouse, M.R. Clinical effectiveness and safety of aspirin for venous thromboembolism prophylaxis after total hip and knee replacement: A systematic review and meta-analysis of randomized clinical trials. JAMA Intern. Med. 2020, 180, 376–384. [Google Scholar] [CrossRef]
- Millar, J.S.; Lawes, C.M.; Farrington, B.; Andrew, P.; Misur, P.; Merriman, E.; Walker, M. Incidence of venous thromboembolism after total hip, total knee and hip fracture surgery at waitemata district health board following a peer-reviewed audit. N. Z. Med. J. 2020, 133, 52–60. [Google Scholar]
- Anderson, D.R.; Dunbar, M.; Murnaghan, J.; Kahn, S.R.; Gross, P.; Forsythe, M.; Pelet, S.; Fisher, W.; Belzile, E.; Dolan, S.; et al. Aspirin or rivaroxaban for vte prophylaxis after hip or knee arthroplasty. N. Engl. J. Med. 2018, 378, 699–707. [Google Scholar] [CrossRef]
- Sung, J.J.; Lau, J.Y.; Ching, J.Y.; Wu, J.C.; Lee, Y.T.; Chiu, P.W.; Leung, V.K.; Wong, V.W.; Chan, F.K. Continuation of low-dose aspirin therapy in peptic ulcer bleeding: A randomized trial. Ann. Intern. Med. 2010, 152, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Lanas, A. Gastrointestinal bleeding associated with low-dose aspirin use: Relevance and management in clinical practice. Expert Opin. Drug Saf. 2011, 10, 45–54. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Guan, X.H.; Wang, R.; Li, B.; Ning, B.; Su, W.; Sun, T.; Li, H.Y. Active ankle movements prevent formation of lower-extremity deep venous thrombosis after orthopedic surgery. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2016, 22, 3169–3176. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Chen, Q.; Ye, M.; Shi, G.H.; Zhang, B. Active ankle movement may prevent deep vein thrombosis in patients undergoing lower limb surgery. Ann. Vasc. Surg. 2016, 32, 65–72. [Google Scholar] [CrossRef]
- Snyder, M.A.; Sympson, A.N.; Scheuerman, C.M.; Gregg, J.L.; Hussain, L.R. Efficacy in deep vein thrombosis prevention with extended mechanical compression device therapy and prophylactic aspirin following total knee arthroplasty: A randomized control trial. J. Arthroplast. 2017, 32, 1478–1482. [Google Scholar] [CrossRef]
- Tyagi, V.; Tomaszewski, P.; Lukasiewicz, A.; Theriault, S.; Pelker, R. The role of intraoperative intermittent pneumatic compression devices in venous thromboembolism prophylaxis in total hip and total knee arthroplasty. Orthopedics 2018, 41, e98–e103. [Google Scholar] [CrossRef]
- Kim, K.I.; Kim, D.K.; Song, S.J.; Hong, S.J.; Bae, D.K. Pneumatic compression device does not show effective thromboprophylaxis following total knee arthroplasty in a low incidence population. Orthop. Traumatol. Surg. Res. OTSR 2019, 105, 71–75. [Google Scholar] [CrossRef]
- Chen, Q.; Huang, S.; Chen, X.; Feng, L.; Zhu, X. Clinical efficacy of multi-pattern detumescence after total knee arthroplasty treated with acupoint massage and mild moxibustion. Zhongguo Zhen Jiu = Chin. Acupunct. Moxibust. 2016, 36, 471–475. [Google Scholar]
- Moloney, M.C.; Lyons, G.M.; Egan, M.; Wallis, F.; Burke, P.E.; Kavanagh, E.; Grace, P.A. Does size matter? The impact of calf muscle volume on venous return in patients with venous leg ulcers. Phlebology 2007, 22, 65–69. [Google Scholar] [CrossRef]
- Zhen, K.Y.; Zhai, Z.G. Progress of intermittent pneumatic compression device application in prevention of venous thromboembolism in inpatients. Zhonghua Jie He He Hu Xi Za Zhi = Zhonghua Jiehe He Huxi Zazhi = Chin. J. Tuberc. Respir. Dis. 2020, 43, 599–603. [Google Scholar]
- Esserman, D.; Allore, H.G.; Travison, T.G. The method of randomization for cluster-randomized trials: Challenges of including patients with multiple chronic conditions. Int. J. Stat. Med. Res. 2016, 5, 2–7. [Google Scholar] [PubMed]
- Arthur, J.R.; Spangehl, M.J. Tourniquet use in total knee arthroplasty. J. Knee Surg. 2019, 32, 719–729. [Google Scholar] [CrossRef] [PubMed]
- Ku, M.C.; Chen, W.J.; Lo, C.S.; Chuang, C.H.; Ho, Z.P.; Kumar, A. Femoral component alignment with a new extramedullary femoral cutting guide technique. Indian J. Orthop. 2019, 53, 276–281. [Google Scholar] [CrossRef] [PubMed]
- Soffin, E.M.; Memtsoudis, S.G. Anesthesia and analgesia for total knee arthroplasty. Minerva Anestesiol. 2018, 84, 1406–1412. [Google Scholar] [CrossRef]
- Lucas, B. Total hip and total knee replacement: Postoperative nursing management. Br. J. Nurs. Mark Allen Publ. 2008, 17, 1410–1414. [Google Scholar] [CrossRef]
- Werkmeister, R.M.; Dragostinoff, N.; Palkovits, S.; Told, R.; Boltz, A.; Leitgeb, R.A.; Gröschl, M.; Garhöfer, G.; Schmetterer, L. Measurement of absolute blood flow velocity and blood flow in the human retina by dual-beam bidirectional doppler fourier-domain optical coherence tomography. Investig. Ophthalmol. Vis. Sci. 2012, 53, 6062–6071. [Google Scholar] [CrossRef]
- Line, B.R. Pathophysiology and diagnosis of deep venous thrombosis. Semin. Nucl. Med. 2001, 31, 90–101. [Google Scholar] [CrossRef]
- O’Brien, J.G.; Chennubhotla, S.A.; Chennubhotla, R.V. Treatment of edema. Am. Fam. Physician 2005, 71, 2111–2117. [Google Scholar]
- Fortier, L.M.; Rockov, Z.A.; Chen, A.F.; Rajaee, S.S. Activity recommendations after total hip and total knee arthroplasty. J. Bone Jt. Surg. Am. Vol. 2021, 103, 446–455. [Google Scholar] [CrossRef]
- Prvu Bettger, J.; Green, C.L.; Holmes, D.N.; Chokshi, A.; Mather, R.C., 3rd; Hoch, B.T.; de Leon, A.J.; Aluisio, F.; Seyler, T.M.; Del Gaizo, D.J.; et al. Effects of virtual exercise rehabilitation in-home therapy compared with traditional care after total knee arthroplasty: Veritas, a randomized controlled trial. J. Bone Jt. Surg. Am. Vol. 2020, 102, 101–109. [Google Scholar] [CrossRef]
- Chughtai, M.; Kelly, J.J.; Newman, J.M.; Sultan, A.A.; Khlopas, A.; Sodhi, N.; Bhave, A.; Kolczun, M.C., 2nd; Mont, M.A. The role of virtual rehabilitation in total and unicompartmental knee arthroplasty. J. Knee Surg. 2019, 32, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Owens, J.M.; Bedard, N.A.; Dowdle, S.B.; Gao, Y.; Callaghan, J.J. Venous thromboembolism following total knee arthroplasty: Does race matter? J. Arthroplast. 2018, 33, S239–S243. [Google Scholar] [CrossRef] [PubMed]
| Date 14 November 2019–22 October 2020 | Group 1 (N = 29) | Group 2 (N = 31) | Group 3 (N = 30) | p-Value |
|---|---|---|---|---|
| Case | 31 | 29 | 30 | |
| Gender (Male/female) | 7/22 | 8/23 | 6/24 | 0.859 |
| Age | 69.7 ± 8.4 | 67.9 ± 8.1 | 70.3 ± 7.8 | 0.502 |
| Rt/Lt | 17/12 | 19/12 | 12/18 | 0.196 |
| Bleeding | 1 | 0 | 0 | |
| Hemovac drainage (mL) | 602.0 ± 228.6 | 753.0 ± 288.6 | 552.7 ± 281.9 | 0.013 |
| Group 1 (N = 31) | Group 2 (N = 29) | Group 3 (N = 30) | ||||||
|---|---|---|---|---|---|---|---|---|
| Average | Standard Deviation | Average | Standard Deviation | Average | Standard Deviation | F | p | |
| Peak flow velocity (cm/s) in the operative limb | ||||||||
| CFV | ||||||||
| 1st day | 18.2 | 3.6 | 26.1 † | 9.6 | 30.0 †,§ | 5.9 | 20.153 | <0.001 |
| 3rd day | 18.3 | 4.0 | 26.2 † | 8.0 | 31.3 †,§ | 7.0 | 29.290 | <0.001 |
| 14th day | 20.5 | 4.7 | 22.6 | 4.4 | 34.6 †,§ | 10.9 | 31.920 | <0.001 |
| PV | ||||||||
| 1st day | 13.4 | 2.9 | 24.7 † | 10.3 | 26.8 † | 9.0 | 22.984 | <0.001 |
| 3rd day | 13.4 | 3.0 | 26.1 † | 12.1 | 30.0 † | 11.7 | 22.600 | <0.001 |
| 14th day | 13.7 | 3.4 | 19.4 † | 8.1 | 29.0 †,§ | 10.3 | 28.640 | <0.001 |
| Peak flow velocity (cm/s) in nonoperative limb | ||||||||
| CFV | ||||||||
| 1st day | 19.5 | 4.4 | 19.0 | 4.3 | 20.2 | 3.2 | 0.780 | 0.461 |
| 3rd day | 18.3 | 3.9 | 19.7 | 4.7 | 20.2 | 3.4 | 1.783 | 0.174 |
| 14th day | 20.1 | 4.0 | 20.6 | 5.1 | 22.7 | 5.7 | 2.392 | 0.097 |
| PV | ||||||||
| 1st day | 14.7 | 4.3 | 15.5 | 2.9 | 15.5 | 2.5 | 0.578 | 0.563 |
| 3rd day | 14.6 | 4.4 | 16.1 | 3.4 | 15.2 | 2.6 | 1.365 | 0.261 |
| 14th day | 13.6 | 3.4 | 15.4 | 3.9 | 16.5 | 3.2 | 4.936 | 0.009 |
| Group 1 (N = 31) | Group 2 (N = 29) | Group 3 (N = 30) | ||||||
|---|---|---|---|---|---|---|---|---|
| Average | Standard Deviation | Average | Standard Deviation | Average | Standard Deviation | F | p | |
| The flow volume (mL/min) in Operative limb | ||||||||
| CFV | ||||||||
| 1st day | 191.9 | 59.2 | 270.5 † | 102.5 | 296.0 † | 134.4 | 8.031 | 0.001 |
| 3rd day | 195.9 | 65.3 | 277.4 † | 94.5 | 294.7 † | 134.2 | 7.836 | 0.001 |
| 14th day | 234.2 | 74.9 | 256.8 | 62.8 | 352.1 †,§ | 193.6 | 7.458 | 0.001 |
| PV | ||||||||
| 1st day | 92.1 | 70.5 | 163.5 † | 55.0 | 155.6 † | 104.1 | 7.240 | 0.001 |
| 3rd day | 87.6 | 39.1 | 173.5 † | 67.5 | 167.6 † | 99.9 | 12.617 | <0.001 |
| 14th day | 98.0 | 49.5 | 147.2 † | 56.5 | 189.9 †,§ | 103.2 | 11.456 | <0.001 |
| Flow volume (mL/min) in the nonoperative limb | ||||||||
| CFV | ||||||||
| 1st day | 196.3 | 79.0 | 192.6 | 61.5 | 176.4 | 45.7 | 0.828 | 0.440 |
| 3rd day | 183.1 | 70.5 | 213.9 | 70.3 | 182.6 | 74.9 | 1.891 | 0.157 |
| 14th day | 222.4 | 67.1 | 228.0 | 61.1 | 204.2 | 88.7 | 0.873 | 0.421 |
| PV | ||||||||
| 1st day | 97.2 | 65.3 | 105.7 | 40.8 | 83.5 | 50.0 | 1.378 | 0.258 |
| 3rd day | 90.7 | 59.7 | 108.7 | 47.2 | 82.9 | 50.1 | 1.951 | 0.148 |
| 14th day | 86.6 | 42.9 | 106.5 | 43.5 | 105.9 | 43.1 | 2.042 | 0.136 |
| Group 1 (N = 31) | Group 2 (N = 29) | Group 3 (N = 30) | ||||||
|---|---|---|---|---|---|---|---|---|
| Average | Standard Deviation | Average | Standard Deviation | Average | Standard Deviation | F | p | |
| Women | ||||||||
| Peak flow velocity (cm/s) in the operative limb | ||||||||
| CFV | ||||||||
| 1st day | 18.9 | 3.1 | 26.2 † | 7.8 | 30.5 †,§ | 6.0 | 21.371 | <0.001 |
| 3rd day | 18.8 | 4.1 | 26.5 † | 7.3 | 32.6 †,§ | 6.0 | 30.861 | <0.001 |
| 14th day | 20.9 | 5.0 | 22.7 | 4.3 | 36.4 †,§ | 11.4 | 28.104 | <0.001 |
| PV | ||||||||
| 1st day | 13.7 | 2.9 | 24.2 † | 10.1 | 25.8 † | 8.8 | 15.082 | <0.001 |
| 3rd day | 13.9 | 3.0 | 26.7 † | 13.1 | 30.5 † | 11.8 | 15.922 | <0.001 |
| 14th day | 13.7 | 3.4 | 19.9 † | 9.3 | 28.9 †,§ | 11.0 | 18.053 | <0.001 |
| Flow volume (mL/min) in operative limb | ||||||||
| CFV | ||||||||
| 1st day | 191.3 | 60.4 | 267.0 † | 70.3 | 289.9 † | 106.6 | 8.927 | <0.001 |
| 3rd day | 195.9 | 69.1 | 272.9 † | 91.0 | 307.8 † | 127.2 | 7.510 | 0.001 |
| 14th day | 228.1 | 79.1 | 252.4 | 67.3 | 353.0 †,§ | 170.9 | 7.478 | 0.001 |
| PV | ||||||||
| 1st day | 86.0 | 78.4 | 155.4 † | 54.2 | 143.3 † | 100.9 | 4.756 | 0.012 |
| 3rd day | 84.8 | 39.7 | 174.2 † | 74.8 | 172.5 † | 100.1 | 10.029 | <0.001 |
| 14th day | 83.7 | 33.7 | 146.7 † | 61.9 | 195.3 †,§ | 108.8 | 12.432 | <0.001 |
| Men | ||||||||
| Peak flow velocity (cm/s) in the operative limb | ||||||||
| CFV | ||||||||
| 1st day | 15.9 | 4.4 | 25.8 | 14.3 | 28.2 | 5.6 | 3.045 | 0.073 |
| 3rd day | 16.6 | 3.8 | 25.3 | 10.3 | 26.2 | 8.9 | 2.887 | 0.082 |
| 14th day | 19.5 | 3.7 | 22.5 | 5.1 | 27.5 †,§ | 3.7 | 5.585 | 0.013 |
| PV | ||||||||
| 1st day | 12.3 | 3.0 | 25.9 † | 11.5 | 30.8 † | 9.0 | 8.016 | 0.003 |
| 3rd day | 11.8 | 24.3 † | 2.6 | 9.0 | 27.9 † | 12.0 | 6.567 | 0.007 |
| 14th day | 13.8 | 3.6 | 17.8 | 2.9 | 29.4 †,§ | 7.2 | 19.072 | <0.001 |
| Flow volume (mL/min) in operative limb | ||||||||
| CFV | ||||||||
| 1st day | 194.1 | 59.8 | 280.6 | 171.4 | 320.3 | 227.3 | 1.028 | 0.378 |
| 3rd day | 195.8 | 56.6 | 290.4 | 109.7 | 242.5 | 161.1 | 1.293 | 0.299 |
| 14th day | 253.5 | 60.5 | 269.5 | 49.2 | 348.8 | 288.0 | 0.659 | 0.529 |
| PV | ||||||||
| 1st day | 111.3 | 33.6 | 186.6 | 53.9 | 204.9 | 111.0 | 3.390 | 0.056 |
| 3rd day | 96.3 | 38.7 | 171.2 | 43.7 | 148.1 | 106.0 | 2.475 | 0.112 |
| 14th day | 142.7 | 66.0 | 148.8 | 40.4 | 168.2 | 81.9 | 0.285 | 0.756 |
| Group 1 (N = 31) | Group 2 (N = 29) | Group 1 (N = 30) | Total | p | |||||
|---|---|---|---|---|---|---|---|---|---|
| Patient | % | Patient | % | Patient | % | Patient | % | ||
| Operative limb | |||||||||
| 1st day | 0.009 | ||||||||
| Stasis (−) | 25 | 86.2% | 31 | 100.0% | 30 | 100.0% | 86 | 95.6% | |
| Stasis (+) | 4 | 13.8% | 0 | 0.0% | 0 | 0.0% | 4 | 4.4% | |
| 3rd day | 0.101 | ||||||||
| Stasis (−) | 27 | 93.1% | 31 | 100.0% | 30 | 100.0% | 88 | 97.8% | |
| Stasis (+) | 2 | 6.9% | 0 | 0.0% | 0 | 0.0% | 2 | 2.2% | |
| 14th day | 0.015 | ||||||||
| Stasis (−) | 24 | 82.8% | 30 | 96.8% | 30 | 100.0% | 84 | 93.3% | |
| Stasis (+) | 5 | 17.2% | 1 | 3.2% | 0 | 0.0% | 6 | 6.7% | |
| Nonoperative limb | |||||||||
| 1st day | 0.294 | ||||||||
| Stasis (−) | 25 | 86.2% | 29 | 93.5% | 29 | 96.7% | 83 | 92.2% | |
| Stasis (+) | 4 | 13.8% | 2 | 6.5% | 1 | 3.3% | 7 | 7.8% | |
| 3rd day | 0.162 | ||||||||
| Stasis (−) | 24 | 82.8% | 29 | 93.5% | 29 | 96.7% | 82 | 91.1% | |
| Stasis (+) | 5 | 17.2% | 2 | 6.5% | 1 | 3.3% | 8 | 8.9% | |
| 14th day | 0.004 | ||||||||
| Stasis (−) | 20 | 69.0% | 29 | 93.5% | 29 | 96.7% | 78 | 86.7% | |
| Stasis (+) | 9 | 31.0% | 2 | 6.5% | 1 | 3.3% | 12 | 13.3% | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ku, M.-C.; Tsai, Y.-H.; Cheng, P.-C.; Yang, T.-I.; Ho, H.-W.; Liao, M.-F.; Tseng, Y.-T.; Lee, M.-T.; Chen, Y.-N. After Total Knee Arthroplasty, Monitored Active Ankle Pumping Improves Lower Leg Circulation More Than Unmonitored Pumping: A Pilot Study. Appl. Sci. 2022, 12, 9028. https://doi.org/10.3390/app12189028
Ku M-C, Tsai Y-H, Cheng P-C, Yang T-I, Ho H-W, Liao M-F, Tseng Y-T, Lee M-T, Chen Y-N. After Total Knee Arthroplasty, Monitored Active Ankle Pumping Improves Lower Leg Circulation More Than Unmonitored Pumping: A Pilot Study. Applied Sciences. 2022; 12(18):9028. https://doi.org/10.3390/app12189028
Chicago/Turabian StyleKu, Ming-Chou, Yuan-Hsin Tsai, Po-Cheng Cheng, Ting-I Yang, Hui-Wen Ho, Min-Fei Liao, Yu-Tzu Tseng, Ming-Tsung Lee, and Yen-Nien Chen. 2022. "After Total Knee Arthroplasty, Monitored Active Ankle Pumping Improves Lower Leg Circulation More Than Unmonitored Pumping: A Pilot Study" Applied Sciences 12, no. 18: 9028. https://doi.org/10.3390/app12189028
APA StyleKu, M.-C., Tsai, Y.-H., Cheng, P.-C., Yang, T.-I., Ho, H.-W., Liao, M.-F., Tseng, Y.-T., Lee, M.-T., & Chen, Y.-N. (2022). After Total Knee Arthroplasty, Monitored Active Ankle Pumping Improves Lower Leg Circulation More Than Unmonitored Pumping: A Pilot Study. Applied Sciences, 12(18), 9028. https://doi.org/10.3390/app12189028







