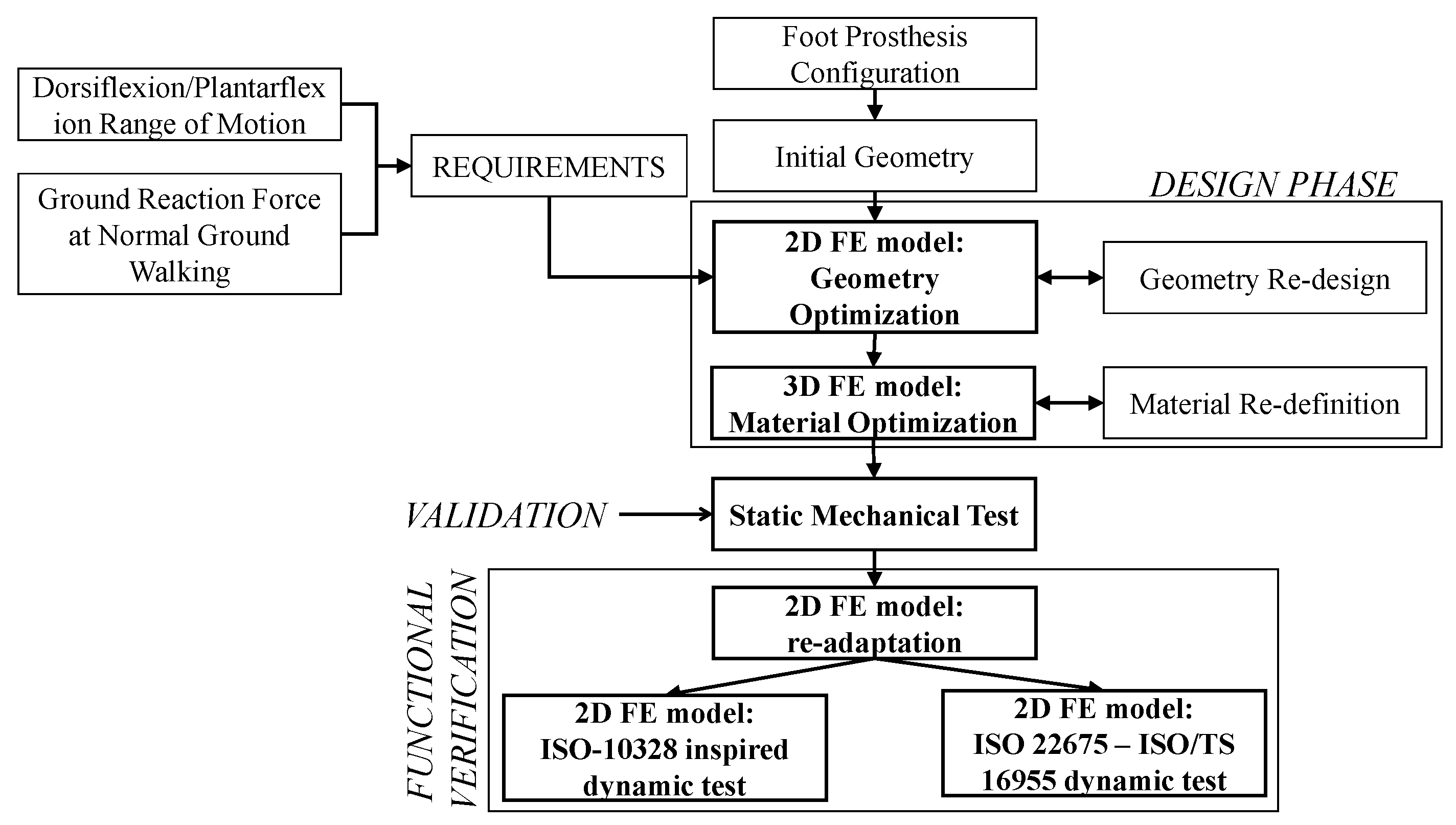
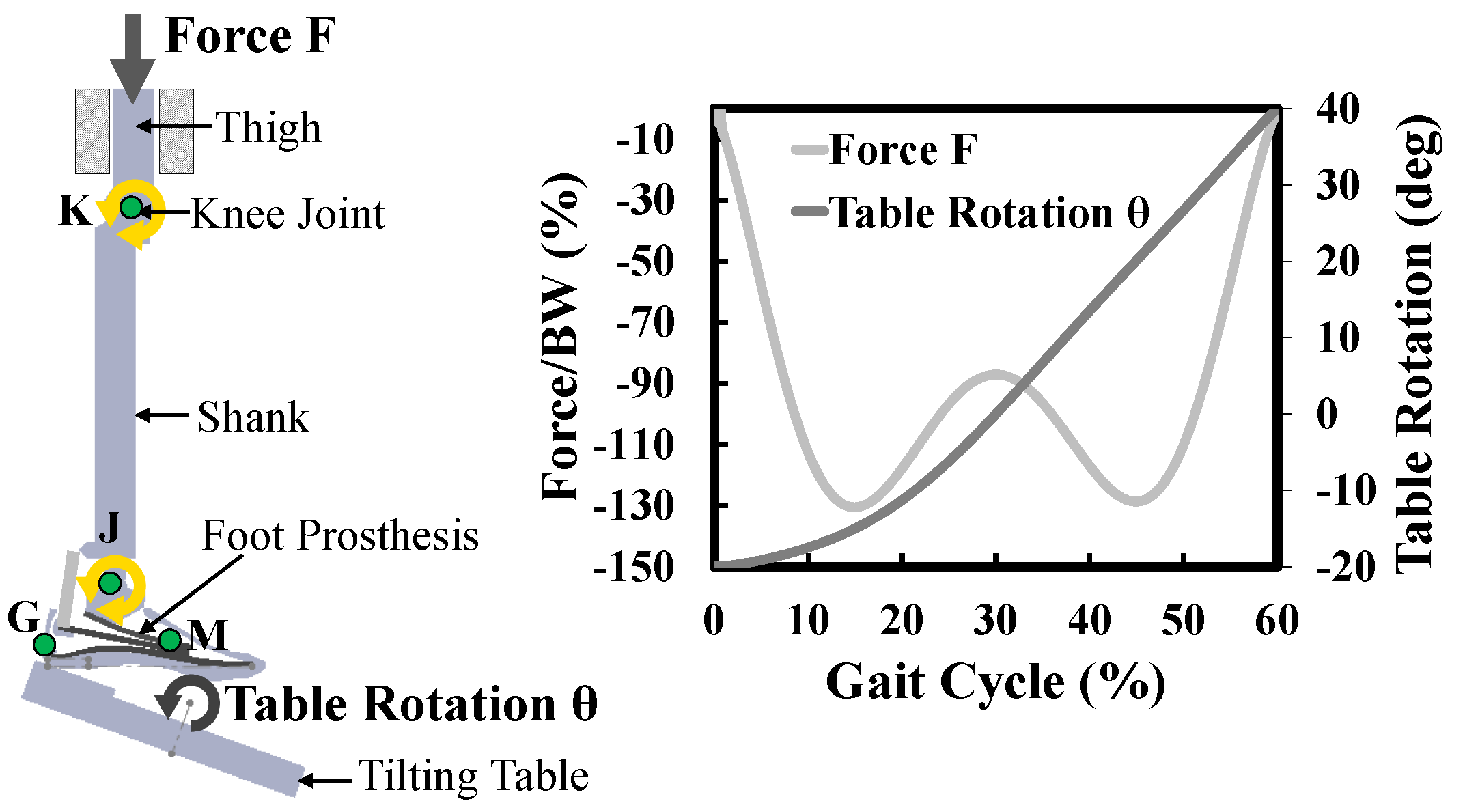
The most important locomotion’s degree of freedom of the foot is the rotation in the sagittal plane. Therefore, to simplify the preliminary stiffness optimization of the prosthesis, based mainly on the modification of the geometry of the prosthetic device, a 2D FE model was built to simulate the motion of the foot in the sagittal plane (
Section 3.1.1). Once the geometry in the sagittal plane was defined, a 3D FE model was built to carry out a more detailed simulation, wherein the composite elastic elements were optimized by modifying the laminate material properties, working mainly on the type, orientation and numbers of layers of CFRP prepregs (
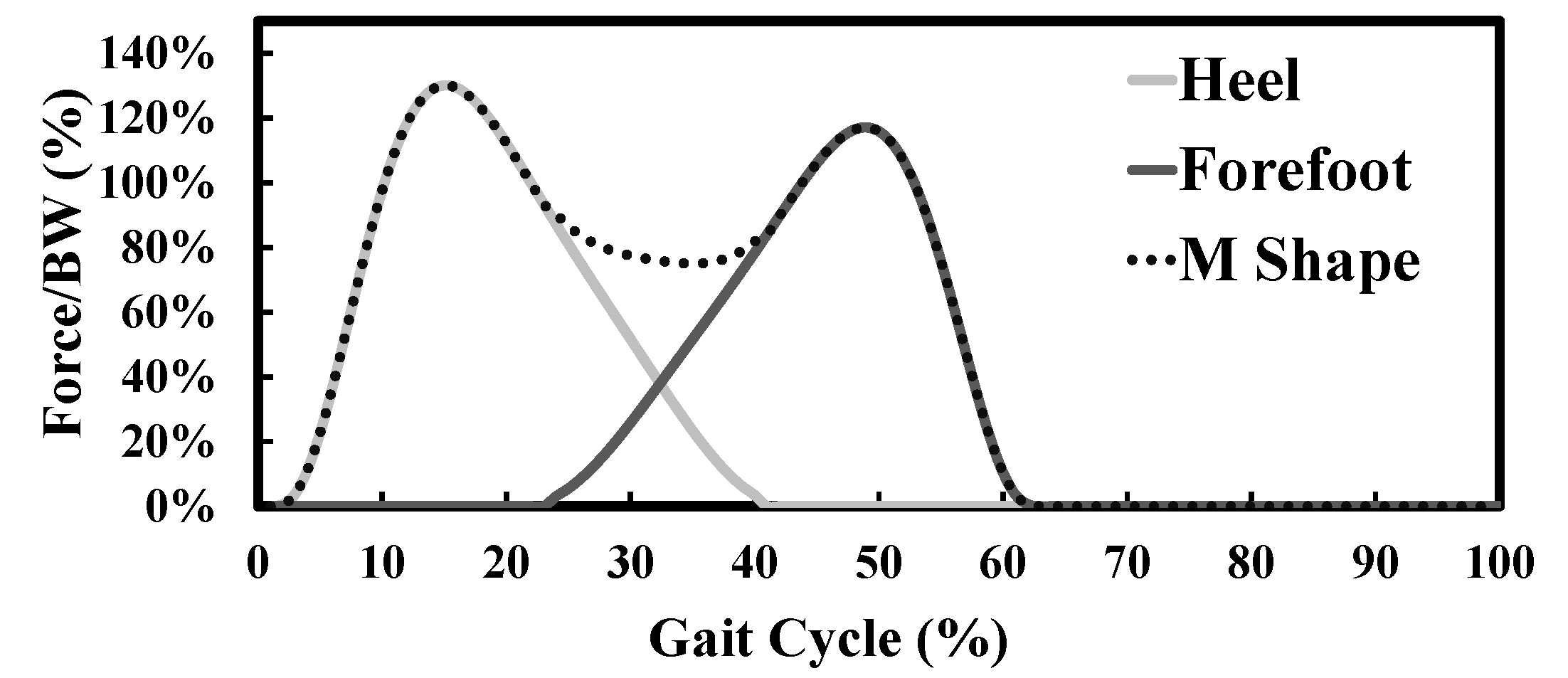
Section 3.1.2). Before explaining in detail the various stages of the proposed methodology, it is reminded that optimizing a passive foot prosthesis means optimizing its stiffness in such a way that it gives rotations in both dorsiflexion and plantarflexion similar to the rotations of a healthy foot, when such prosthesis is subjected to loads (ground reaction forces) similar to those to which a healthy foot is subjected. For the present application, as already mentioned in
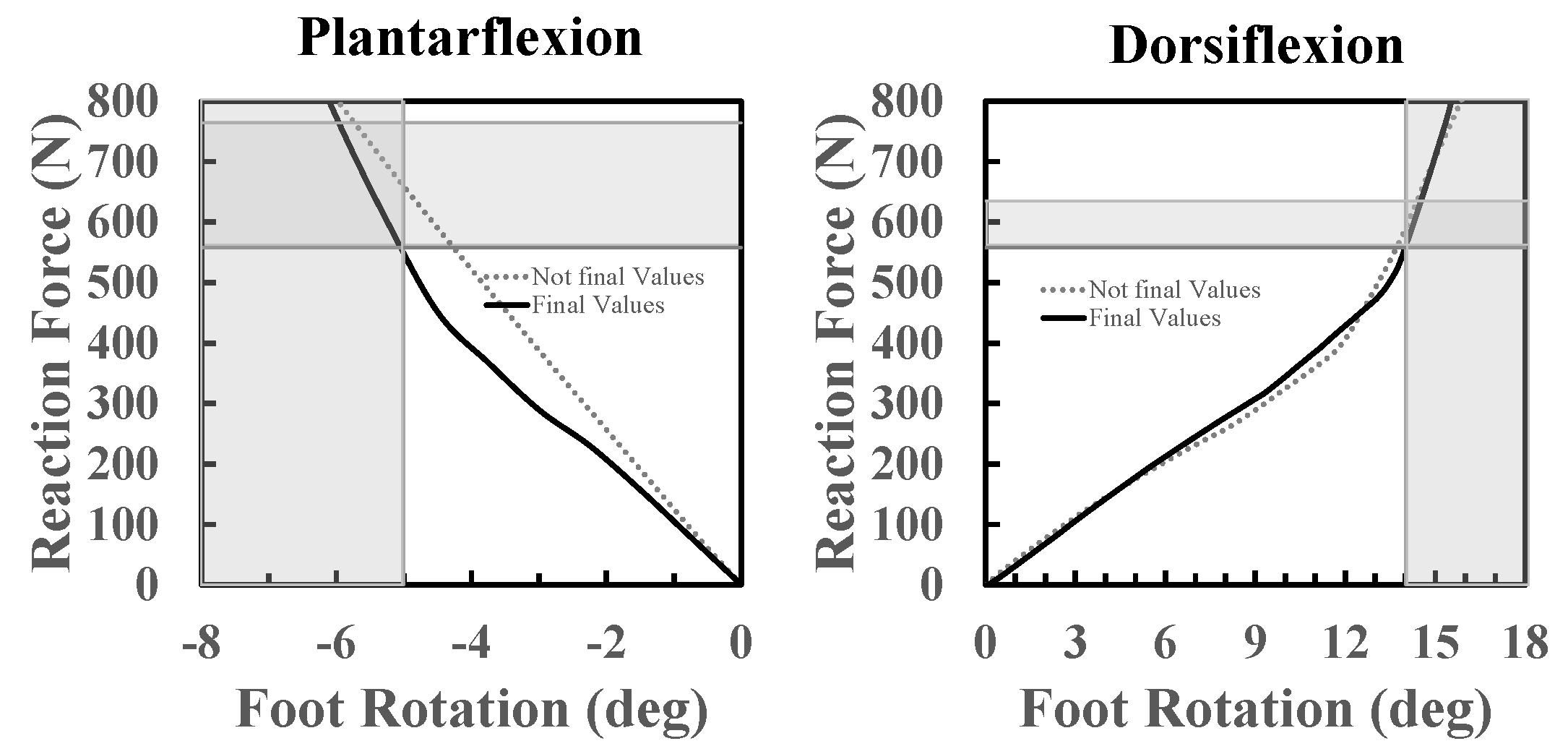
Section 2.4, the aim is to optimize the prosthesis’ stiffness in such a way that, when it is loaded at the heel with a load between 95% and 130% of the weight of the user, it gives a plantarflexion between −5° and −8°; when it is loaded at the toe with a load between 95% and 108% of the body weight, it must give a dorsiflexion between 14° and 18°.
3.1.1. Geometry Optimization: 2D FE Model
In this first step of the design phase, geometry optimization was carried out through a 2D FEA. For example, this step can be used to optimize the profile shapes of an already defined configuration of elastic elements, to configure the energy-storing parts of a new ESR foot, or to investigate the behavior of an existing prosthetic device after modifications or additions of other functional components, such as dampers and actuators.
Optimizing the geometry of a foot prosthesis is very important, especially with regard to ESR feet and their elastic components. Although the result of the 2D FE model in terms of stiffness is not definitive, this model is essential to optimize the shapes of the various elastic components to ensure the full range of motion needed to walk. A non-optimization of the shapes of the elastic components can bring a range of motion too reduced or too wide. Regardless of the stiffness of the elastic components, if the range of motion is too small, the foot rotates around the ankle joint up to a certain angle and then, a sudden sensation of increase in the equivalent rotational stiffness around the ankle joint follows. Due to this sudden increase in stiffness of the ankle joint, the foot no longer rotates around the ankle and the heel comes off the ground before the desired moment. This situation can be perceived by the user as a sudden disappearance of the support, which can cause discomfort or even a fall of the user. If the range of motion is too wide, the foot may continue to rotate in dorsiflexion beyond the desired limit by delaying the hell-off. Even this situation can generate discomfort or even a fall of the user.
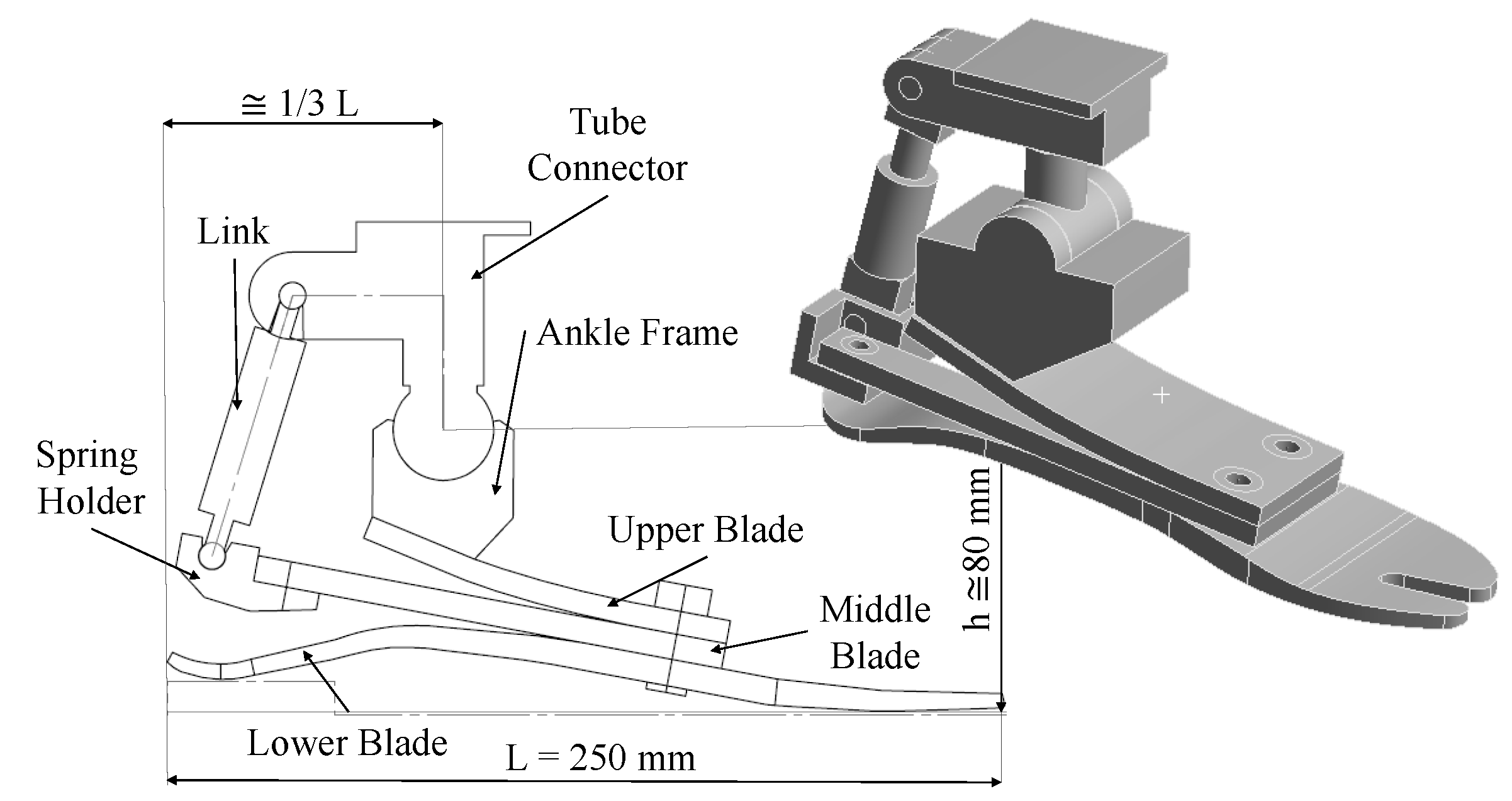
For MyFlex-
, geometry optimization was focused on the profile shape of the middle blade and the upper blade, aiming to meet the biomechanical requirements previously defined (
Section 2.4). The lower blade used for the present application was provided by Össur and it was already optimized for the chosen weight category. Then, an initial 2D geometry of the foot was drawn bearing in mind the dimensional parameters defined by the human anatomy such as length
L of the foot, the height
h of the ankle joint from the ground and the distance
d of the ankle joint from the heel, which is around 1/3 of the foot length. For the present application, the length of the foot was 250 mm and the height of the ankle joint was between 80 mm and 100 mm, as shown in
Figure 1.
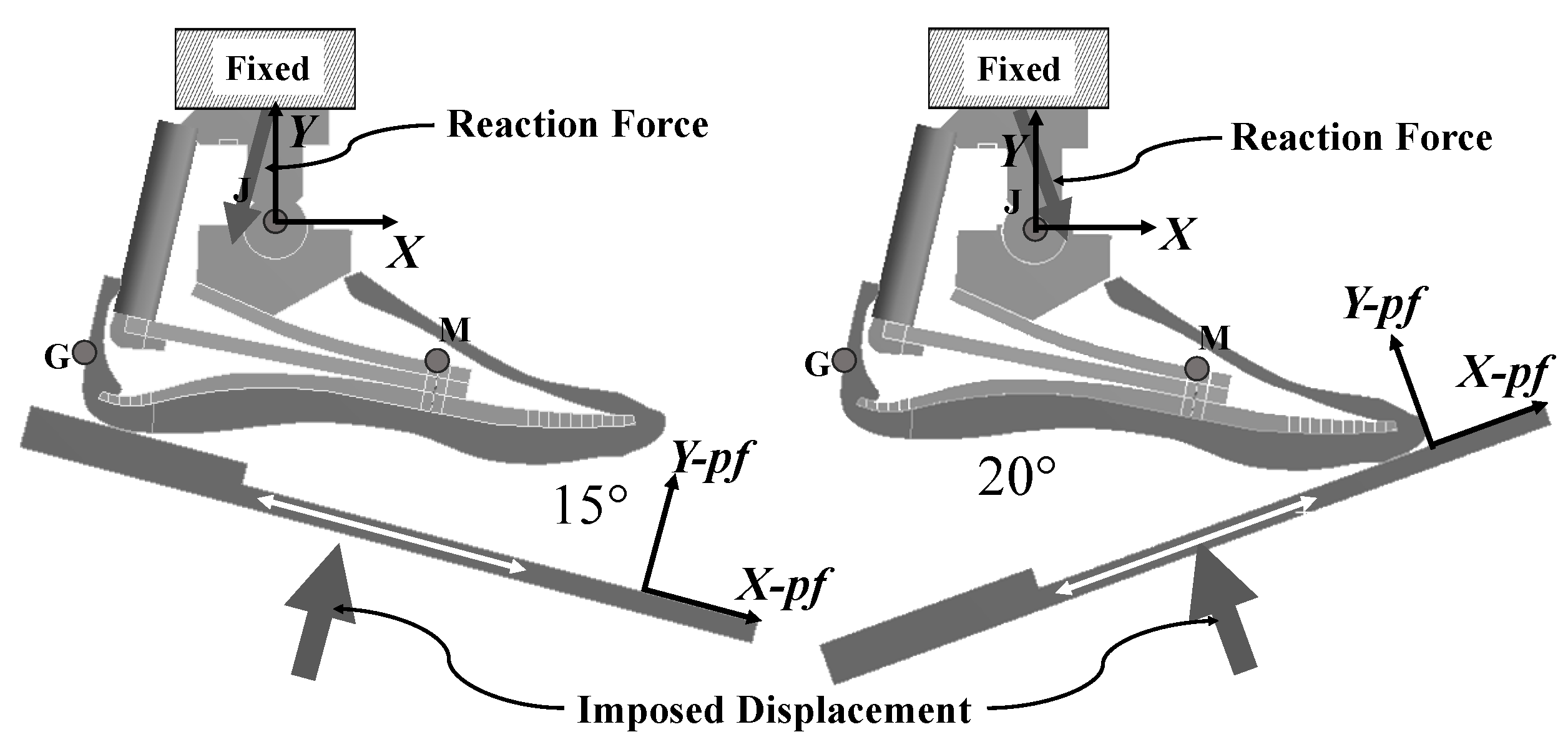
Load conditions. The CAD model was drawn in the
x–y plane and imported into ANSYS Workbench. The FE model was simulated in a 2D static structural analysis. Following the ISO 10328 standard, the dorsiflexion test was simulated by loading the FE model with a platform at the forefoot. For the plantarflexion test, the FE model was loaded at the heel. The platforms were moved by imposing 10 mm of displacement for the plantarflexion test and 50 mm for the dorsiflexion test. The shank was constrained with a fixed support at the top of the tube connector. For the present application, the loads and the constraints are depicted in
Figure 4.
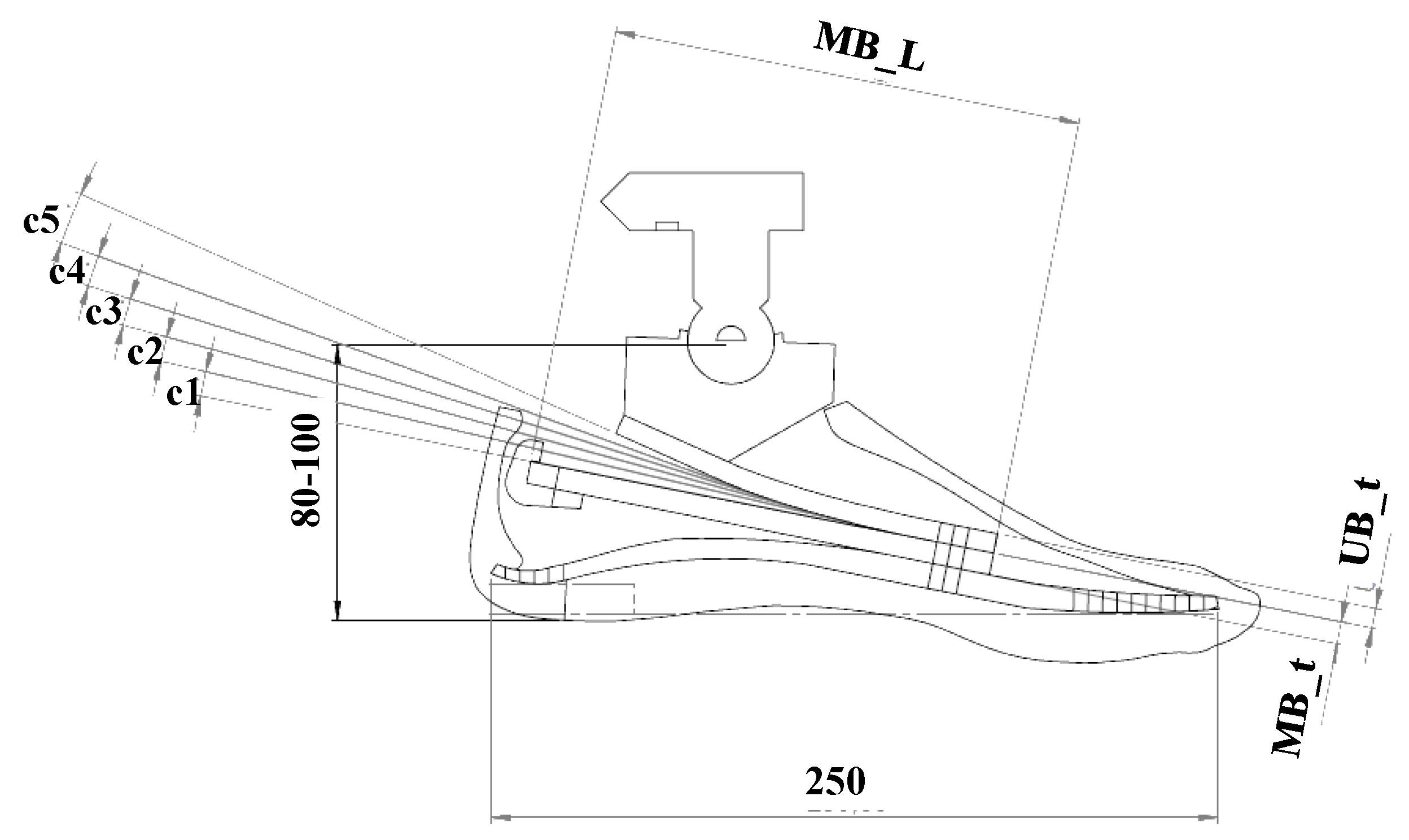
The geometry optimization was carried out by varying the geometric parameters. These parameters depend on the foot prosthesis architecture and the designers can choose them. For MyFlex-
, the parameters are depicted in
Figure 5 and listed in
Table 3. The upper blade was defined in the sagittal plane by 6 parameters. The parameter UB
is the thickness, while the parameters c
, c
, c
, c
and c
define the curvatures of the curved profile of the upper blade, which was composed by 6 straight sections—starting from the metatarsus (front), c
is the relative inclination between the first and the second section, c
is the relative inclination between the second and third section, etc. The middle blade, which had a straight profile in the sagittal plane, was defined only by its length (MB
) and thickness (MB
). The lower blade, provided by Össur, had been already optimized, in terms of shape and material properties, for specific users’ weight categories.
Mesh modeling. The FE model was built in ANSYS Workbench. PLANE183 (ANSYS) elements were used for mesh building; these were two-dimensional 8- and 6-node elements with quadratic displacement behavior and two translations at each node as degrees of freedom. The final 2D FE model of MyFlex-
was meshed (
Figure 6), presenting a total of 10,000 nodes corresponding to 20,000 degrees of freedom.
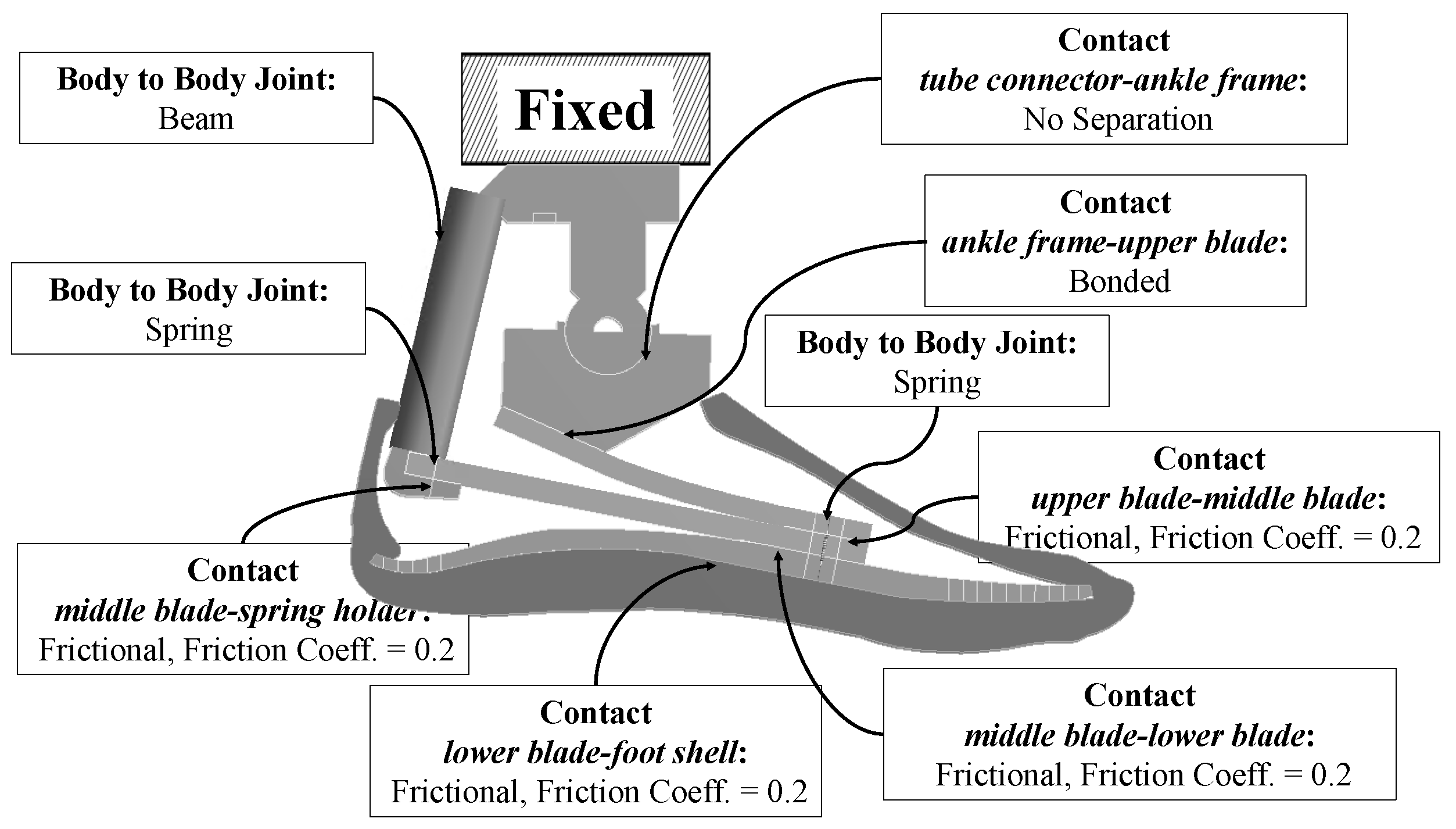
Contacts modeling. The contacts between parts had to be modeled differently according to the real conditions. For parts that worked bending toward each other with slight sliding, the contacts were modeled as frictional using pure penalty formulation and 0.1 was set as the normal stiffness factor. For contacts that could be modeled as glued/bonded, the bonded contact type was used with augmented Lagrange formulation and 1 was set as the normal stiffness factor.
In the present work, the upper blade, middle blade and lower blade bent toward each other with slight sliding when the foot was loaded. Therefore, the contacts between the upper blade and middle blade and between the middle blade and the lower blade were modeled as
frictional contact using
pure penalty formulation. The ankle frame and the upper blade were joined together with two M8 bolts along the longitudinal direction; for this condition, the contact between the ankle frame bottom surface and the upper blade top surface could be modeled as
bonded to simplify the simulation, using
augmented Lagrange formulation. A summary of the contacts is presented in
Table 4.
For the 2D FE model of MyFlex-
, a
no-separation contact type between the tube connector and the ankle frame (see
Figure 7) was used to model the ankle joint; a
no-separation contact type allows frictionless motions to be performed without separation of the parts.
Joints: Pretensioned bolts were modeled as preloaded springs, where the preload given as force was equal to the bolt pretension of the corresponding bolt. More specifically, the bolts were modeled as longitudinal springs body-to-body joints (longitudinal COMBIN14, ANSYS). Both the nodes of the COMBIN14 element were applied as direct attachment to the nodes of the connected parts. The elastic elements were joined together with two pretensioned M8 bolts in the physical MyFlex- that could be seen as a single bolt in the sagittal plane. In addition, the middle blade and the spring holder were joined with preloaded M6 screws. Bolt pretension was simulated as a normal force given to the longitudinal springs body-to-body joints, which corresponded to the standard bolt pretensions for M6 (7.4 kN, 8.8 class, frictional coefficient = 0.20) and M8 (13.7 kN, 8.8 class, frictional coefficient = 0.20). Connection links with hinge joints at both extremities were modeled with body-to-body beam joints (BEAM3, ANSYS). BEAM3 is a 2D uniaxial element with tension, compression and bending capabilities and it has the translations in both directions of the x–y plane and the rotation around the z-direction at each node. In MyFlex-, the link part, characterized by two hinge joints that connected the tube connector to the spring holder, was modeled by BEAM3.
Simulation conditions: ESR feet elastic elements are subjected to high deflections. Therefore, the 2D FE model was simulated in a nonlinear static structural analysis environment.
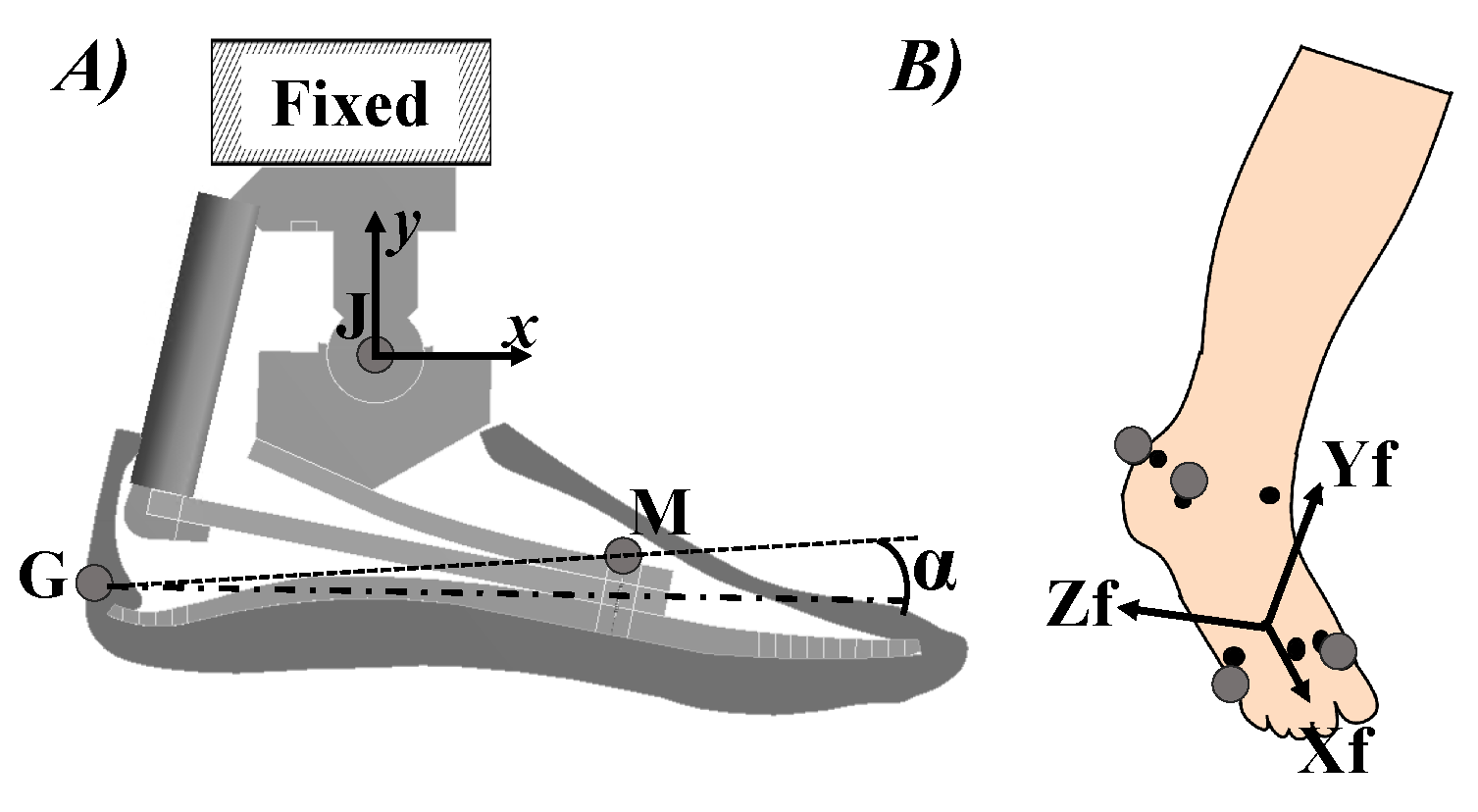
Simulation outputs: The behavior of the foot can be evaluated in two different modalities by plotting the
reaction force at the fixed constraint against the platform
displacement in the
direction (see
Figure 4) or against the foot
rotation. The
foot rotation is calculated by using two virtual markers (
G and
M in
Figure 8). The positions of the virtual markers were chosen considering the marker-set protocol [
21,
25]. Since the shank was fixed, the
J marker was considered as (0,0).
The displacements of the virtual markers (given in the global
x–y reference) are given as direct output of the simulation and they can be considered as functions of the platform displacement
in the vertical direction
of the same platform (see
Figure 4). Therefore, the displacements of the G marker in the global
x- and
y-directions are
The displacement of the M marker in the global
x- and
y-directions are
If (
;
) and (
;
) are the initial positions of G and M markers, referred to J (0;0), the coordinates of G and M are:
The foot rotation
is calculated as the variation of the angle between the GM line and the horizontal direction (
Figure 9). The initial angle
between the GM line and the horizontal direction and the rotation
of the foot are calculated as:
In Equation (
10),
is determined as
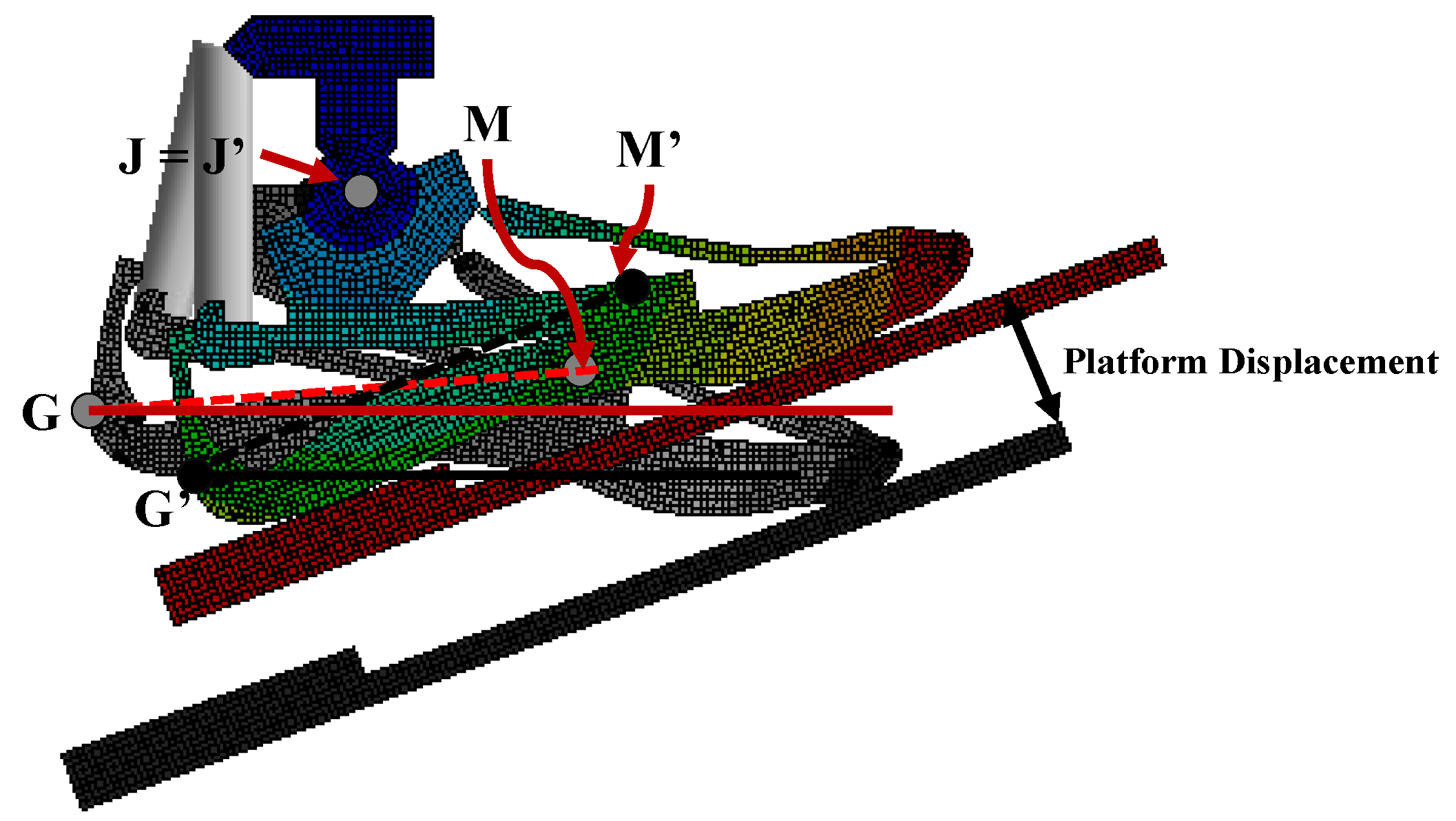
3.1.2. Material Properties Optimization: 3D FE Model
With the 2D FE model, the profile of the elastic elements and the general geometry of the foot prosthesis in the sagittal plane were defined. The 3D CAD model for the 3D FE model was built upon the geometry obtained in the previous step of the
design phase methodology (
Section 3.1.1). The elastic elements of ESR feet, in general, are laminate composite and they are built by stacking, in sequence, layers of CFRP (carbon fiber-reinforced plastic) or GFRP (glass fiber-reinforced plastic) prepregs, which are sheets of pre-impregnated fibers (generally pre-impregnated with resin) and they can be unidirectional or woven. The stiffness of each of the elastic elements of the ESR feet is defined by lamination sequence, type, number, orientation and order of each layer. For MyFlex-
, unidirectional and woven CFRP prepregs were used. The lamination sequence of CFRP prepregs layers was optimized to reach the targeted stiffness, thus meeting the biomechanical requirements defined in
Section 2.4. The elastic properties of the CFRP prepregs used are gathered in
Table 5.
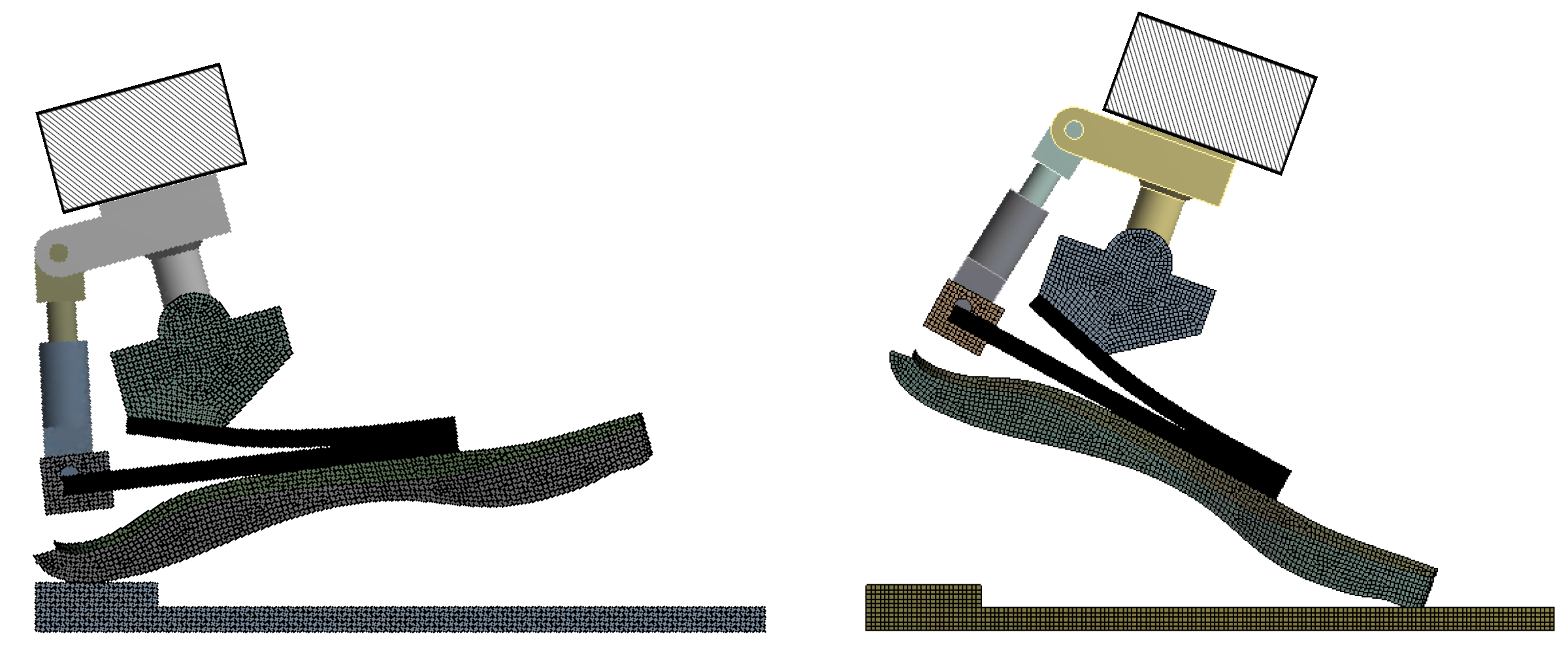
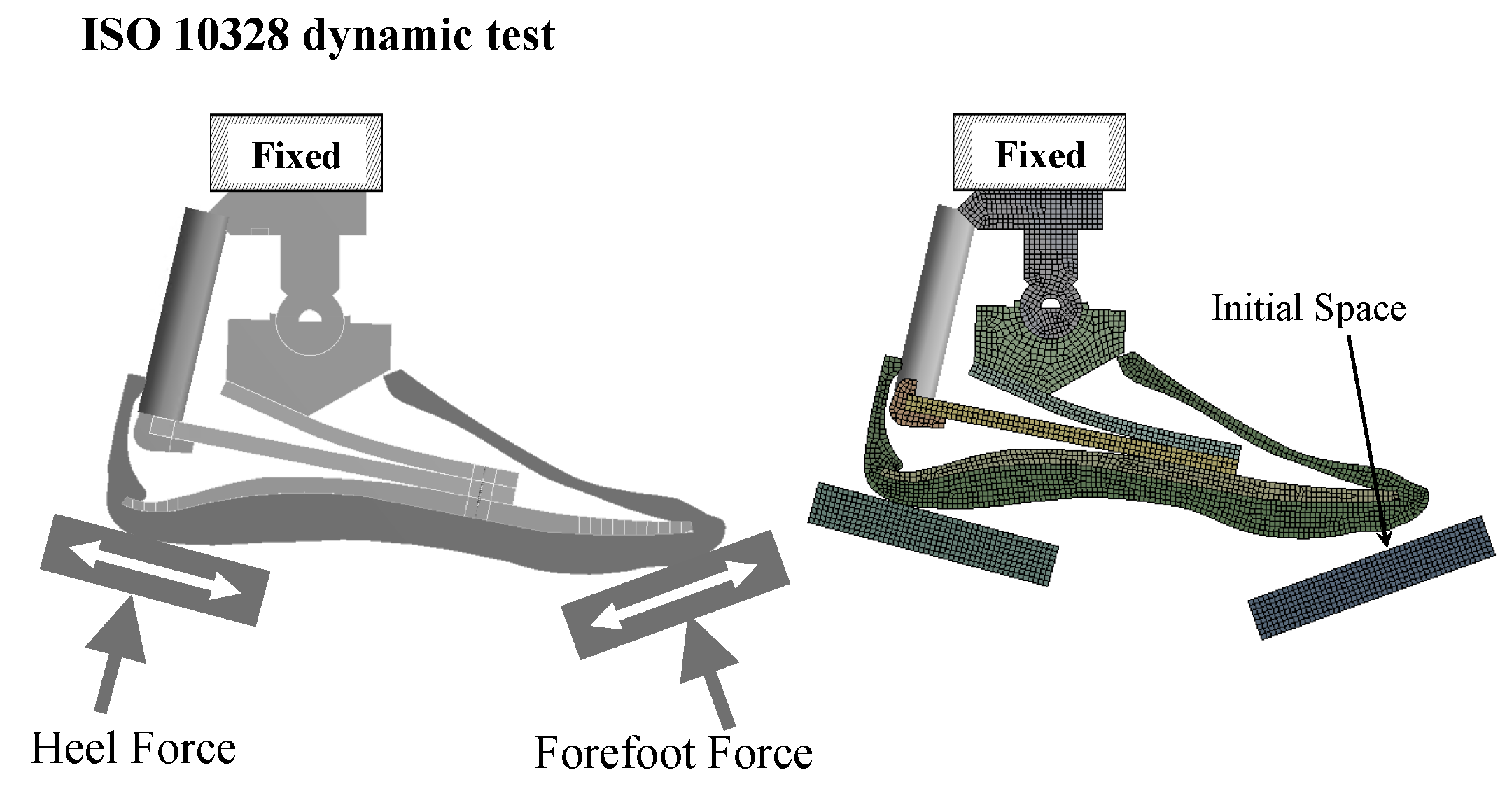
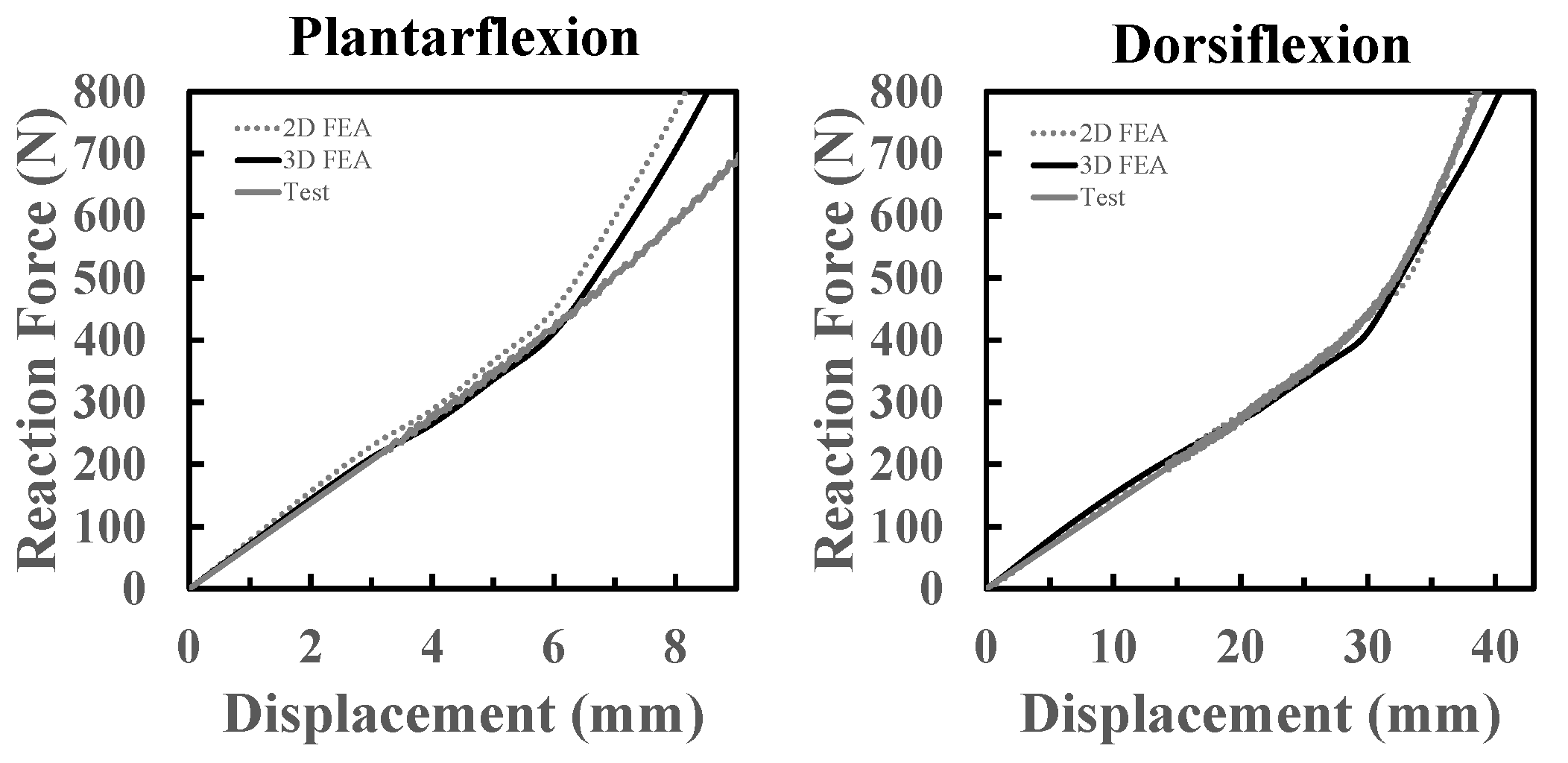
Loads and constraints: The 3D FE model is intended to be validated with a mechanical test on a physical prototype of a foot prosthesis. In the ISO 10328 standard, the foot is loaded with an inclined platform, which means two inclined actuators are required, one for the heel and one for the toe, to compress the foot prosthesis. A dedicated test setup was designed and built (
Figure 10) to avoid the necessity of two inclined actuators. The ISO 10328-equivalent test setup was characterized by a vertical piston that pushed a platform upward. The relative inclination between the foot and the platform was created by two different adapters that inclined the foot backwards by 15° and forwards by 20°. The platform, free to move along the longitudinal direction of the foot, compressed the foot prosthesis, fixed at the top. A vertical displacement was imposed to the platform to compress the foot at the heel and at the toe in two different tests to simulate the
ground reaction forces at both the early and the late stance, respectively. The total displacement was 10 mm and 50 mm at the heel and the toe load conditions, respectively, because of the different range of motion of the foot during plantarflexion and dorsiflexion. For the toe load, the platform was moved upward linearly at a rate from 3 mm/s to 4 mm/s. The platform moved linearly along the vertical direction for the heel load to compress the foot at a rate from 0.6 mm/s to 0.8 mm/s. These rate values, both for the plantarflexion and dorsiflexion tests, were chosen for a reason of convergence of the simulations. It was verified that the results did not change if the dorsiflexion simulation was performed at a rate of 3 mm/s or at a rate of 4 mm/s. The exact same applies to the plantarflexion simulation. This is justified by the fact that the simulation was still in rate values under static conditions.
The results from the design phase FEAs can be plotted as reaction force against the rotation, or reaction force against the platform displacement.
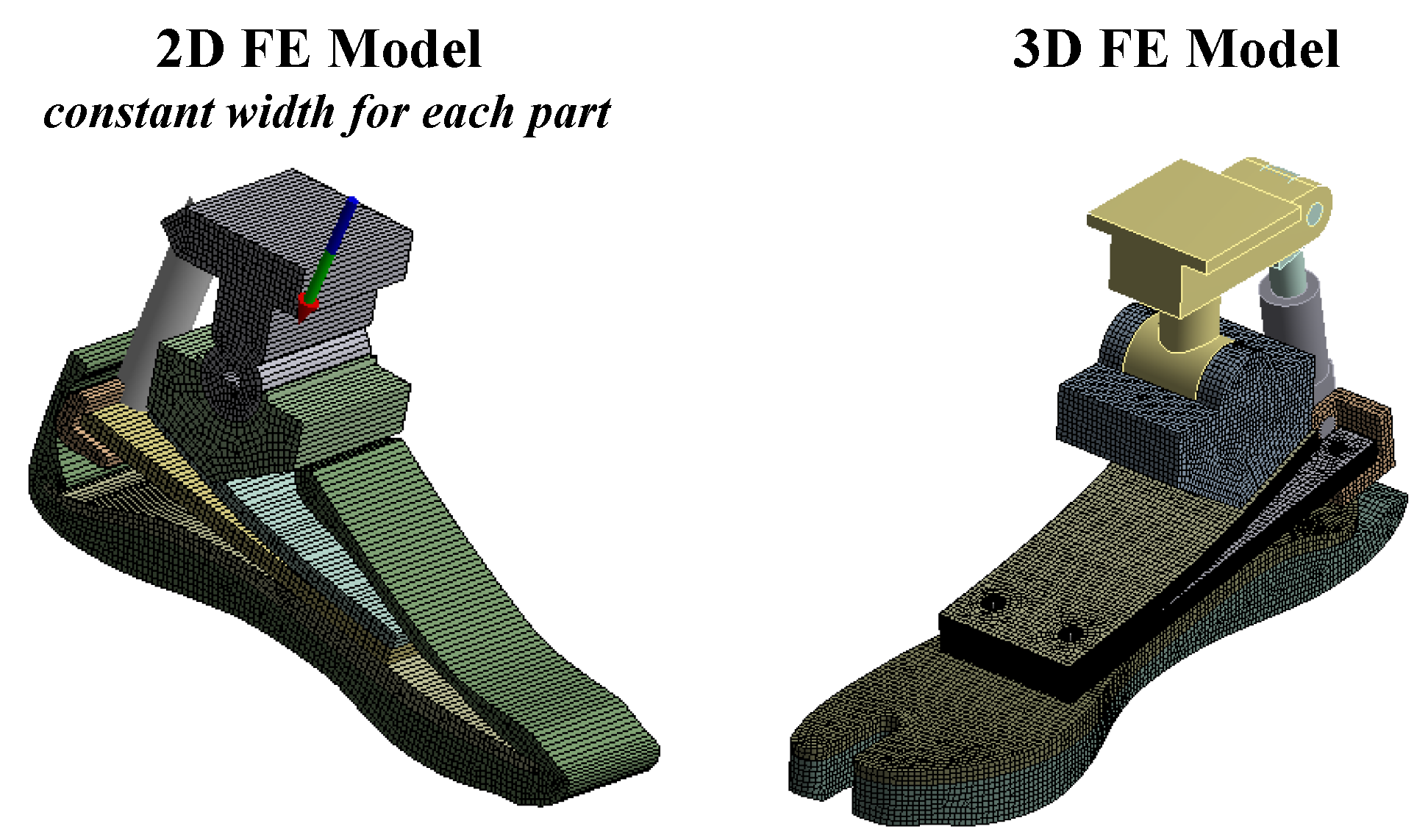
Components modeling: The 3D CAD Model was imported into ANSYS by setting
3D as the analysis type. All isotropic parts were provided as solid to ANSYS, while composite parts were surfaces—
Figure 11. All parts involved in contacts were modeled as flexible elements (platform, foot shell, lower blade, middle blade, upper blade, ankle frame and spring holder), while the parts connected with joints were modeled as rigid bodies (link and tube connector)—see
Figure 12 and
Figure 13.
Based on the results obtained from the 2D FE model in the previous step, the initial values of thicknesses and elastic properties of the composite parts were predefined and used as a reference to define the lamination sequences of layers of CFRP prepregs. Then, the types, the numbers, the orientations and the order of the layers of CFRP prepregs were changed until the targeted thickness and elastic properties (calculated with the Classical Theory of Laminates) were reached.
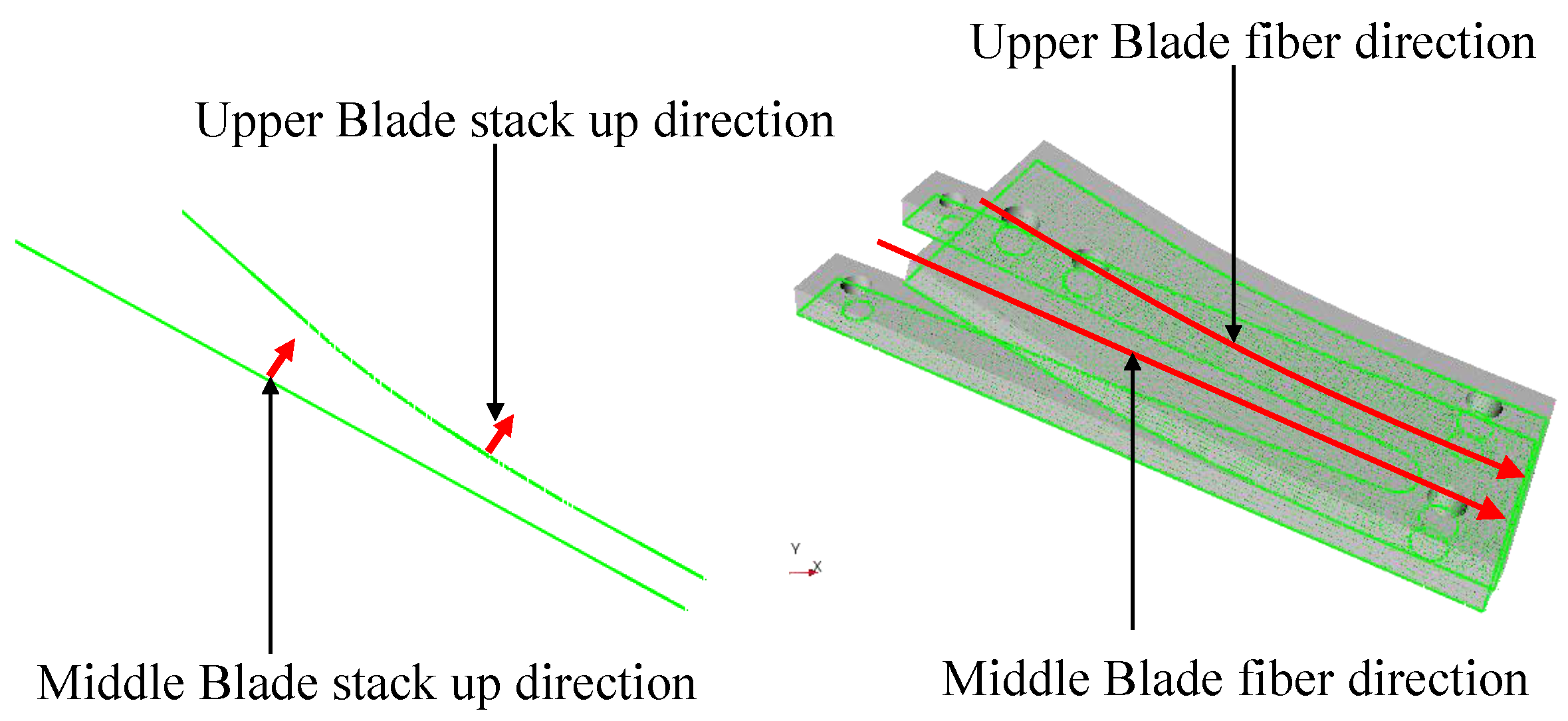
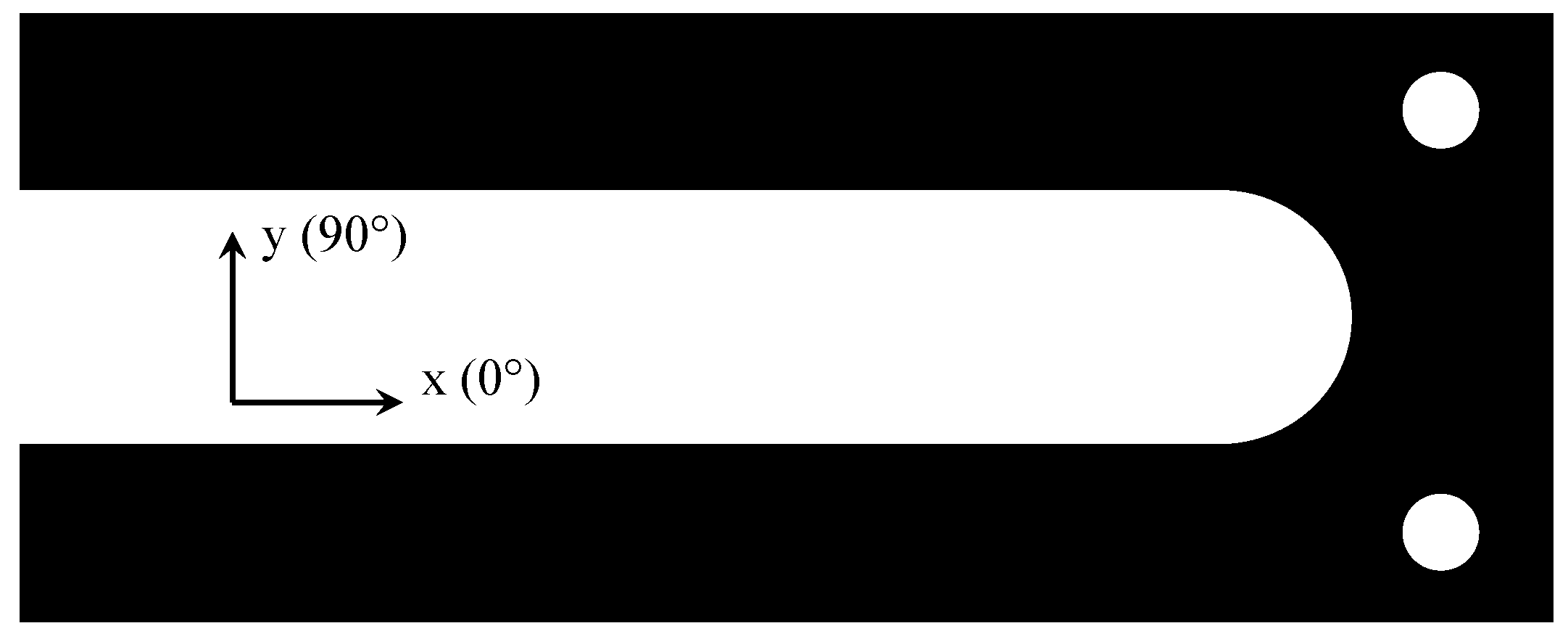
The 3D CAD model of the foot prosthesis was provided to ANSYS in
Geometry. The lamination sequences of the composite parts were modeled inside
ANSYS Composite PrePost (
ACP). The main fiber direction for each of the composite parts is depicted in
Figure 14 and it corresponds to the longitudinal direction of the foot prosthesis. Then, the composite parts were exported from
ACP to
Static Structural modeler as solid, with the final thicknesses.
Mesh modeling: The flexible components (platform, foot shell, lower blade, middle blade, upper blade, ankle blade and spring holder) were meshed. The elastic elements, including the lower blade and the foot shell, were mainly modeled with SOLID186 elements, which were 20-node elements with 3 degrees of freedom at each node and with quadratic behavior. SOLID187 elements (10-node elements with 3 degrees of freedom per node) were used for irregular areas. Ankle frame, spring holder and platform were modeled with SOLID185 elements, 8-node elements with 3 degrees of freedom at each node and linear behavior. The final 3D FE model of MyFlex-
consisted of around 1,800,000 degrees of freedom (600,000 nodes) (
Figure 12 and
Figure 13).
Contact modeling: As in the 2D FE model, for parts that bend to each other with slight sliding, the contacts were modeled as
frictional using
pure penalty formulation and 0.1 was set as the
normal stiffness factor (the factor was set to 1 for normal dominated conditions). For contacts that could be modeled as glued/bonded, the
bonded contact type was used with
augmented Lagrange formulation and 1 was set as the
normal stiffness factor. In MyFlex-
, the upper blade, the middle blade and the lower blade bend to each other with slight sliding when the foot is loaded. The contacts between the upper blade and the middle blade and between the middle blade and the lower blade were modeled as
frictional contact using
pure penalty formulation. The contact between the ankle frame bottom surface and the upper blade top surface was modeled as
bonded to simplify the simulation, using
augmented Lagrange formulation. The contacts’ properties used in the present 3D model are summarized in
Table 6.
Table 6.
Contacts’ properties. See also
Figure 15. AF = ankle frame; UB = upper blade; MB = middle blade; LB = lower blade; SH = spring holder; TC = tube connector.
Table 6.
Contacts’ properties. See also
Figure 15. AF = ankle frame; UB = upper blade; MB = middle blade; LB = lower blade; SH = spring holder; TC = tube connector.
| Surface 1 | Surface 2 | Type | Formulation | Frict. Coeff. | Norm. Stiff. Fact. |
|---|
| AF top | UB bottom | bonded | augm.Lagrange | - | 1.00 |
| UB bottom | MB top | frictional | pure penalty | 0.20 | 0.01 |
| MB bottom | LB top | frictional | pure penalty | 0.20 | 0.01 |
| MB bottom | SH top | frictional | pure penalty | 0.20 | 0.01 |
Bolt modeling: In MyFlex-, the elastic elements were joined together with two preloaded M8 bolts. In addition, the middle blade and the spring holder were joined with preloaded M6 screws. The screws were modeled as preloaded spring joints (ANSYS; COMBIN14) and with specific axial stiffness and pretensions that corresponded to M8 (front bolts) and M6 (spring holder bolts). The extremities of the springs were applied, as remote attachments, on the portions of the upper-blade top surface and on the bottom of the lower-blade surface to simulate the washers’ section.
Loads and constraints: The FEA was carried out in a nonlinear static structural analysis by enabling the
large deflection option. The
vertical displacement was imposed on the platform, free to move along the x-direction and fixed along y (transverse)-direction (see
Figure 10 and
Figure 13). The platform compressed the ESR foot and the reaction force was measured where the fixed support constraint was set.