Digital Health Services through Patient Empowerment: Classification, Current State and Preliminary Impact Assessment by Health Pod Systems
Abstract
:Featured Application
Abstract
1. Introduction
1.1. The Reference Scenario in Healthcare during the Current Decade
- -
- the “silverization” of society
- -
- the continuous growth of healthcare expenditure that is reaching serious and warning levels.
1.2. Lifestyle and the 5P Medicine Approach
1.3. Innovative Technologies for Prevention
- (1)
- to define a common taxonomy for these systems and their different typologies, together with a desk analysis of available solutions worldwide.
- (2)
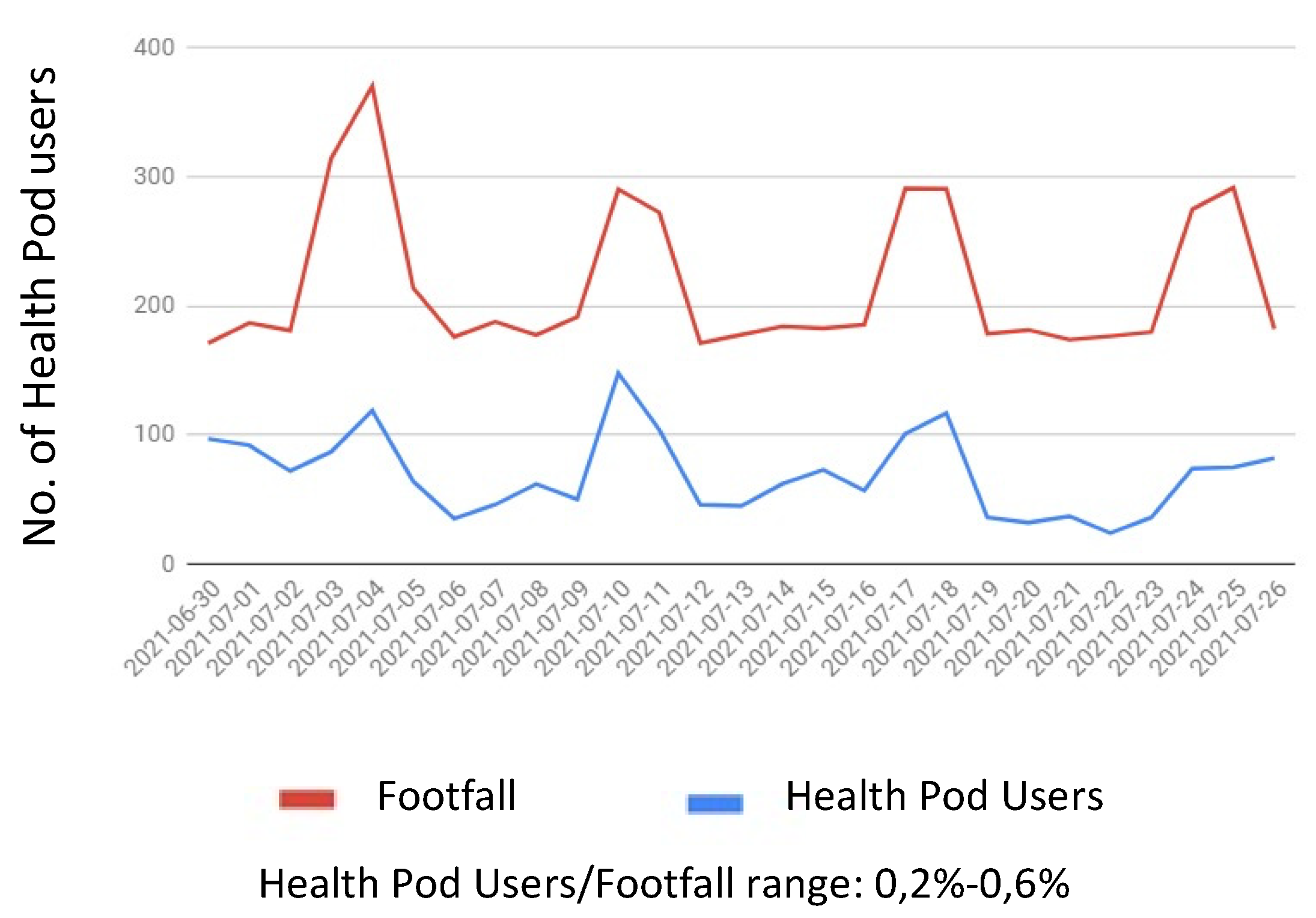
- to show preliminary data relevant to the introduction of a health care pod solution in a specific scenario of large malls as a distribution point for self-opportunistic screening;
- (3)
- to discuss the application and potential impact of such technology in preventive medicine, according to these personal and collective pictures of individual or societal health status.
2. Materials and Methods
2.1. Taxonomy and Definition
2.2. Desk Analysis
3. Results
3.1. Market Analysis of Health Pod Solutions
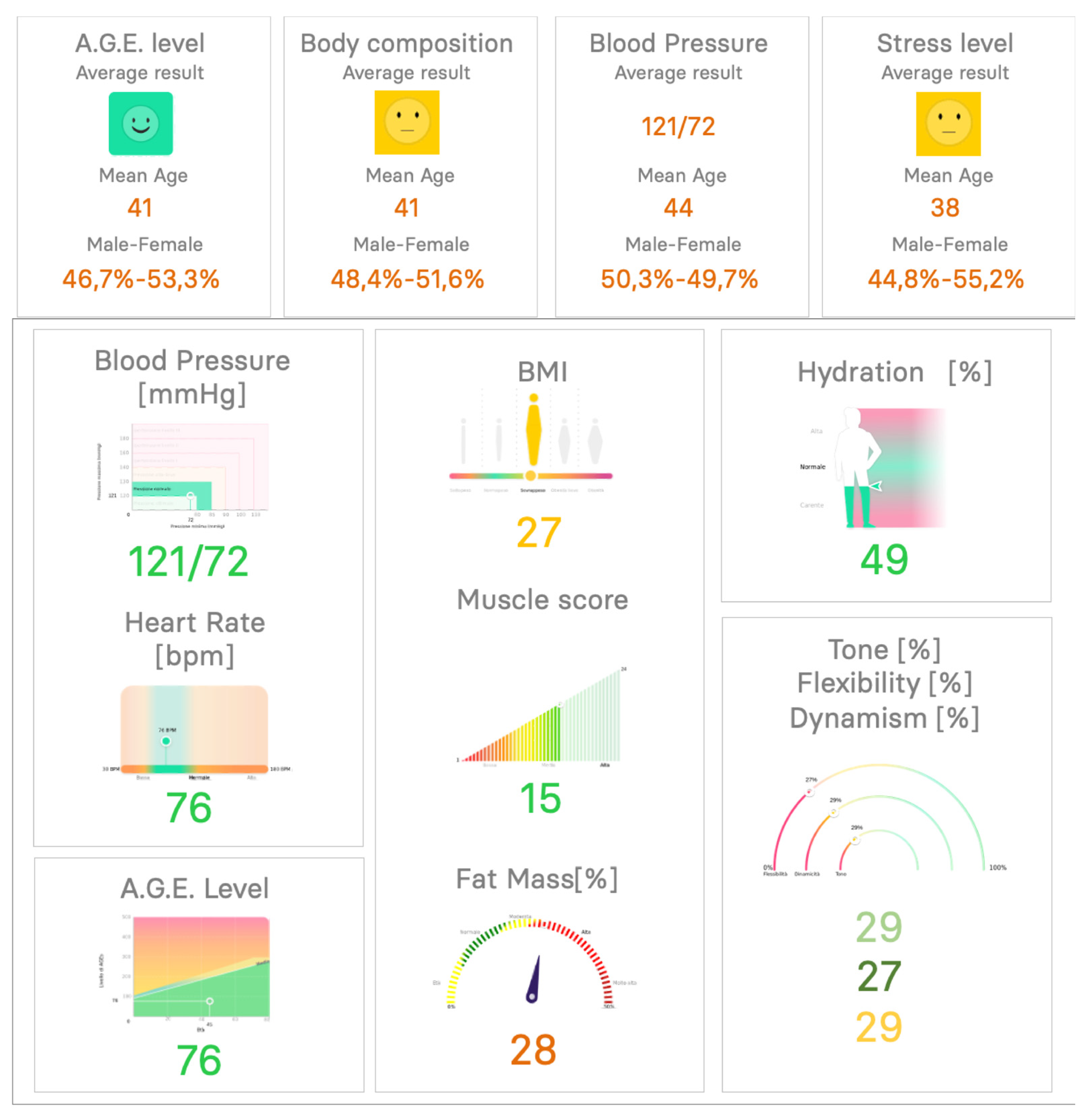
3.2. Biomedical Measurements and Services Available through Health Pods
- -
- blood pressure → cardiovascular diseases;
- -
- heart rate (HR) → cardiovascular diseases;
- -
- HR variability (HRV) → cardiovascular diseases and psycho-physical well-being;
- -
- oxygen saturation (SpO2) → chronic respiratory and cardiovascular diseases;
- -
- respiratory rate (RR) → chronic respiratory and cardiovascular diseases;
- -
- advanced glycation end products (AGEs) → diabetes mellitus and metabolic situation;
- -
- body weight (BW), body mass index (BMI), fat-free mass (FFM), fat mass (FM), total body water (TBW) → all-cause mortality risk from BMI.
- empower patients’ self-management of lifestyle and health, thus implementing the first paradigm of prevention by awareness and reducing risk factors (through the personalized coaching delivered through advanced cloud services);
- provide personalized prevention programs, promoting health environments, encouraging physical activity and healthy nutrition through a gamified approach; redefine the patient/caregiver relationship, in which care teams and subjects decide together when to visit live or virtually, reducing time and costs of the traditional healthcare delivery approach, providing immediate and geographically distributed tools for monitoring and evaluating the patients progresses;
- empower patients’ self-management of disease, helping patients to increase the level of adherence to their clinical programs and to make the healthy choice the easiest one, at the right time.
3.3. Test of Health Pod Application in a Real-World Setting
- -
- measurement of BP through an automated system;
- -
- measurement of AGEs through spectroscopy in fluorescent light;
- -
- measurement of ECG 1-lead and assessment of stress level through HRV analysis;
- -
- measurement of body weight and composition through BIA.
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php/Population_structure_and_ageing (accessed on 4 August 2021).
- Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Healthcare_expenditure_statistics (accessed on 4 August 2021).
- Available online: https://www.un.org/en/chronicle/article/lifestyle-diseases-economic-burden-health-services (accessed on 4 August 2021).
- Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 27 September 2021).
- World Health Organization. Global Status Report on Noncommunicable Diseases 2014; WHO: Geneva, Switzerland, 2014; ISBN 978 92 4 156485 4. Available online: https://apps.who.int/iris/bitstream/handle/10665/148114/9789241564854_eng.pdf;jsessionid=47154A45F723BA82CDF6B3A5D2DAEAD5?sequence=1 (accessed on 27 September 2021).
- Balbus, J.M.; Barouki, R.; Birnbaum, L.S.; Etzel, R.A.; Gluckman, P.D.; Grandjean, P.; Hancock, C.; Hanson, M.A.; Heindel, J.J.; Hoffman, K.; et al. Early-life prevention of non-communicable diseases. Lancet 2013, 381, 3–4. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Global Status Report on Noncommunicable Diseases 2010; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- World Health Organization. Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Chiuve, S.E.; McCullough, M.L.; Sacks, F.M.; Rimm, E.B. Healthy Lifestyle Factors in the Primary Prevention of Coronary Heart Disease Among Men. Benefits among Users and Nonusers of Lipid-Lowering and Antihypertensive Medications. Circulation 2006, 114, 160–167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anand, P.; Kunnumakara, A.B.; Sundaram, C.; Harikumar, K.B.; Tharakan, S.T.; Lai, O.S.; Sung, B.; Aggarwal, B.B. Cancer is a preventable disease that requires major lifestyle changes. Pharm Res. 2008, 25, 2097–2116. [Google Scholar] [CrossRef] [PubMed]
- Willett, W.C.; Koplan, J.P.; Nugent, R.; Dusenbury, C.; Puska, P.; Gaziano, T.A. Chapter 44—Prevention of Chronic Disease by Means of Diet and Lifestyle Changes. In Disease Control Priorities in Developing Countries, 2nd ed.; Jamison, D.T., Breman, J.G., Measham, A.R., Eds.; The International Bank for Reconstruction and Development/The World Bank: Washington, DC, USA; Oxford University Press: New York, NY, USA, 2006. Available online: https://www.ncbi.nlm.nih.gov/books/NBK11795/ (accessed on 27 September 2021).
- WHO. Global Health Risks Who Mortality and Burden of Disease Attributable to Selected Major Risks; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- World Health Organization. Ottawa Charter for Health Promotion; World Health Organization: Geneva, Switzerland, 1986. [Google Scholar]
- Flores, M.; Glusman, G.; Brogaard, K.; Price, N.D.; Hood, L. P4 medicine: How systems medicine will transform the healthcare sector and society. Per. Med. 2013, 10, 565–576. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pravettoni, G.; Triberti, S. A “P5” approach to healthcare and health technology. In P5 eHealth: An Agenda for the Health Technologies of the Future; Pravettoni, G., Triberti, S., Eds.; Springer: Cham, Switzerland, 2020. [Google Scholar] [CrossRef] [Green Version]
- Gorini, A.; Caiani, E.G.; Pravettoni, G. Chapter 7—Psycho-cognitive Factors Orienting eHealth Development and Evaluation. In P5 eHealth: An Agenda for the Health Technologies of the Future; Pravettoni, G., Triberti, S., Eds.; Springer: Cham, Switzerland, 2020. [Google Scholar] [CrossRef] [Green Version]
- Letafat-nejad, M.; Ebrahimi, P.; Maleki, M.; Aryankhesal, A. Utilization of integrated health kiosks: A systematic review. Med. J. Islamic Repub. Iran 2020, 34, 114. [Google Scholar] [CrossRef]
- Available online: https://www.cdc.gov/cpr/readiness/healthcare/closedPODtoolkit.htm#anchor_1542373553386 (accessed on 27 September 2021).
- Afzali, M.; Ahmadi, M.; Mahmoudvand, Z. Data Requiments and the Basis for Designing Helath Information Kiosks. Acta Inf. Med. 2017, 25, 198–202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kamel Boulos, M.N.; Haywood, G. Opportunistic atrial fibrillation screening and detection in “self-service health check-up stations”: A brief overview of current technology potential and possibilities. mHealth 2021, 7, 12. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://newsroom.cisco.com/press-release-content?type=webcontent&articleId=5375895 (accessed on 4 August 2021).
- Available online: https://www.higi.com (accessed on 4 August 2021).
- Available online: https://capsula.app/ (accessed on 4 August 2021).
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar] [CrossRef] [PubMed]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.T.; Corra, U.; Cosyns, B.; Deaton, C.; et al. The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice. 2016 European Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar] [CrossRef] [PubMed]
- Engelgau, M.M.; Narayan, K.M.V.; Vinicor, F. Identifying the Target Population for Primary Prevention: The Trade-Offs. Diabetes Care 2002, 25, 2098–2099. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- Chehade, M.J.; Yadav, L.; Jayatilaka, A.; Gill, T.K.; Palmer, E. Personal digital health hubs for multiple conditions. Bull. World Health Organ. 2020, 98, 569–575. [Google Scholar] [CrossRef] [PubMed]
- EU. The Economy of Wellbeing. 2021. Available online: https://data.consilium.europa.eu/doc/document/ST-13171-2019-INIT/en/pdf (accessed on 27 September 2021).
- OECD. The Economy of Well-Being. Available online: https://data.consilium.europa.eu/doc/document/ST-10414-2019-ADD-1/en/pdf (accessed on 27 September 2021).




| General Information | Self Parameters | Teleconsultation Parameters | ||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| System | Company | Country | Medical Certification | BP | Weight | Height | BIA | Temperature | Eyesight | Single-lead ECG | SpO2 | COVID Triage | HRV | PWV | BP | Weight | Height | BIA | Temperature | Eyesight | Single-Lead ECG | ECG 12 | SpO2 | Dermatoscope | Otoscope | Hearing | Stethoscope | Blodd Analysis | DNA | Dispensary of medicine | Densitometry | Holter | HRV | Thermal camera |
| Consult Station | H4D sarl | France | CE Med IIA-FDA | X | X | X | X | X | X | X | X | X | X | X | ||||||||||||||||||||
| HIGI | Higi SH llc | USA | FDA | X | X | X | ||||||||||||||||||||||||||||
| Pursuant Health | Pursuant Health | USA | FDA | X | X | X | ||||||||||||||||||||||||||||
| CAPSULA | CAPSULA | Italy | CE Med IIA | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||||||||||||
| Health Point | Health Point SpA | Italy | X | X | X | X | X | X | X | X | X | X | X | |||||||||||||||||||||
| Bodyo | Bodyo | France | ND | X | X | X | X | X | ||||||||||||||||||||||||||
| One Minute Clinic | Ping An | China | X | X | X | |||||||||||||||||||||||||||||
| Lifestyle check point | Lifestyle check point | UK | X | X | X | X | X | X | ||||||||||||||||||||||||||
| SISU | Sisu Health group | Australia | X | X | X | X | ||||||||||||||||||||||||||||
| Spotcheck | Spotcheck | Dubai | FDA-CE | X | X | X | X | X | ||||||||||||||||||||||||||
| Tessan | Tessan | France | X | X | X | X | X | X | ||||||||||||||||||||||||||
| Vitalis | 24aLife | USA, Slovenia | X | X | X | X | X | X | ||||||||||||||||||||||||||
| Onmed | Onmed | USA | X | X | X | X | ||||||||||||||||||||||||||||
| MS Fit | Medicalsoft | Russia | X | X | X | X | X | |||||||||||||||||||||||||||
| Health ATM | Yolo Health | India | X | X | X | X | X | X | X | X | X | |||||||||||||||||||||||
| Wellbeing people | Wellbeing people | USA | X | X | X | X | ||||||||||||||||||||||||||||
| Check Duration per Typology and site | Duration Avg (mm:ss) | Duration Max (mm:ss) | Duration Min (mm:ss) |
|---|---|---|---|
| Age Check @ S1 | 00:59 | 05:26 | 00:34 |
| Body Composition Check @ S1 | 02:01 | 09:50 | 01:06 |
| HRV Check @ S1 | 02:45 | 15:40 | 01:49 |
| Vascular Check @ S1 | 01:31 | 05:48 | 00:57 |
| Age Check @ S2 | 00:57 | 03:07 | 00:29 |
| Body Composition Check @ S2 | 02:01 | 05:46 | 01:09 |
| HRV Check @ S2 | 02:40 | 12:33 | 01:52 |
| Vascular Check @ S2 | 01:29 | 05:34 | 00:55 |
| Men | Age | Blood Pressure | Body Composition | Heart Rate Variability | ||||||||||||
| Age Range | Total No. | Age Avg Value | Sample Size | BP Avg Sys | BP Avg Dia | Avg HR | Sample Size | BMI | % Fat Mass | % Hydration | % Muscle Mass | Sample Size | HRV Tone | % HRV Dynam | % Flexibility | Sample Size |
| 65+ | 758 | 234.3 | 158 | 125.7 | 67.2 | 69.4 | 313 | 27.2 | 25.2% | 54.9% | 71.1% | 158 | 52.4% | 29.6% | 16.5% | 127 |
| 55–64 | 922 | 202.4 | 214 | 126.0 | 77.4 | 74.6 | 253 | 28.1 | 24.7% | 54.4% | 71.5% | 229 | 37.5% | 28.6% | 21.8% | 224 |
| 40–54 | 1814 | 175.2 | 410 | 123.9 | 76.7 | 74.0 | 500 | 27.8 | 23.8% | 54.8% | 72.4% | 455 | 35.8% | 32.4% | 27.4% | 442 |
| 25–39 | 1417 | 143.9 | 318 | 119.9 | 70.2 | 74.8 | 329 | 26.7 | 22.4% | 55.8% | 73.7% | 376 | 34.2% | 41.6% | 40.1% | 391 |
| 18–24 | 875 | 138.6 | 165 | 107.3 | 63.4 | 78.7 | 177 | 23.2 | 28.3% | 49.5% | 68.0% | 263 | 19.6% | 33.6% | 34.6% | 267 |
| TOTAL | 5786 | TOTAL | 1265 | TOTAL | 1572 | TOTAL | 1481 | TOTAL | 1451 | |||||||
| Females | Age | Blood Pressure | Body Composition | Heart Rate Variability | ||||||||||||
| Age Range | Total No. | Age Avg Value | Sample Size | BP Avg Sys | BP Avg Dia | Avg HR | Sample Size | BMI | % Fat Mass | % Hydration | % Muscle Mass | Sample Size | HRV Tone | % HRV Dynam | % Flexibility | Sample Size |
| 65+ | 548 | 199.2 | 128 | 128.6 | 65.5 | 72.4 | 179 | 25.3 | 29.4% | 48.1% | 67.0% | 117 | 47.6% | 33.5% | 17.9% | 123 |
| 55–64 | 917 | 189.2 | 215 | 120.1 | 69.1 | 74.9 | 258 | 25.8 | 30.4% | 47.4% | 66.0% | 208 | 36.0% | 30.9% | 23.8% | 233 |
| 40–54 | 1912 | 176.4 | 442 | 113.7 | 67.8 | 75.9 | 485 | 25.6 | 30.1% | 48.0% | 66.4% | 467 | 32.5% | 35.1% | 28.5% | 508 |
| 25–39 | 1593 | 151.1 | 351 | 110.3 | 65.6 | 78.2 | 361 | 24.7 | 29.1% | 48.9% | 67.3% | 423 | 24.5% | 38.6% | 38.4% | 456 |
| 18–24 | 875 | 138.6 | 165 | 107.3 | 63.4 | 78.7 | 177 | 23.2 | 28.3% | 49.5% | 68.0% | 263 | 19.6% | 33.6% | 34.6% | 267 |
| TOTAL | 5786 | TOTAL | 1301 | TOTAL | 1460 | TOTAL | 1478 | TOTAL | 1587 | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Andreoni, G.; Caiani, E.G.; Castaldini, N. Digital Health Services through Patient Empowerment: Classification, Current State and Preliminary Impact Assessment by Health Pod Systems. Appl. Sci. 2022, 12, 359. https://doi.org/10.3390/app12010359
Andreoni G, Caiani EG, Castaldini N. Digital Health Services through Patient Empowerment: Classification, Current State and Preliminary Impact Assessment by Health Pod Systems. Applied Sciences. 2022; 12(1):359. https://doi.org/10.3390/app12010359
Chicago/Turabian StyleAndreoni, Giuseppe, Enrico Gianluca Caiani, and Nicola Castaldini. 2022. "Digital Health Services through Patient Empowerment: Classification, Current State and Preliminary Impact Assessment by Health Pod Systems" Applied Sciences 12, no. 1: 359. https://doi.org/10.3390/app12010359
APA StyleAndreoni, G., Caiani, E. G., & Castaldini, N. (2022). Digital Health Services through Patient Empowerment: Classification, Current State and Preliminary Impact Assessment by Health Pod Systems. Applied Sciences, 12(1), 359. https://doi.org/10.3390/app12010359








