Comparison of Amsler–Krumeich and Sandali Classifications for Staging Eyes with Keratoconus
Abstract
1. Introduction
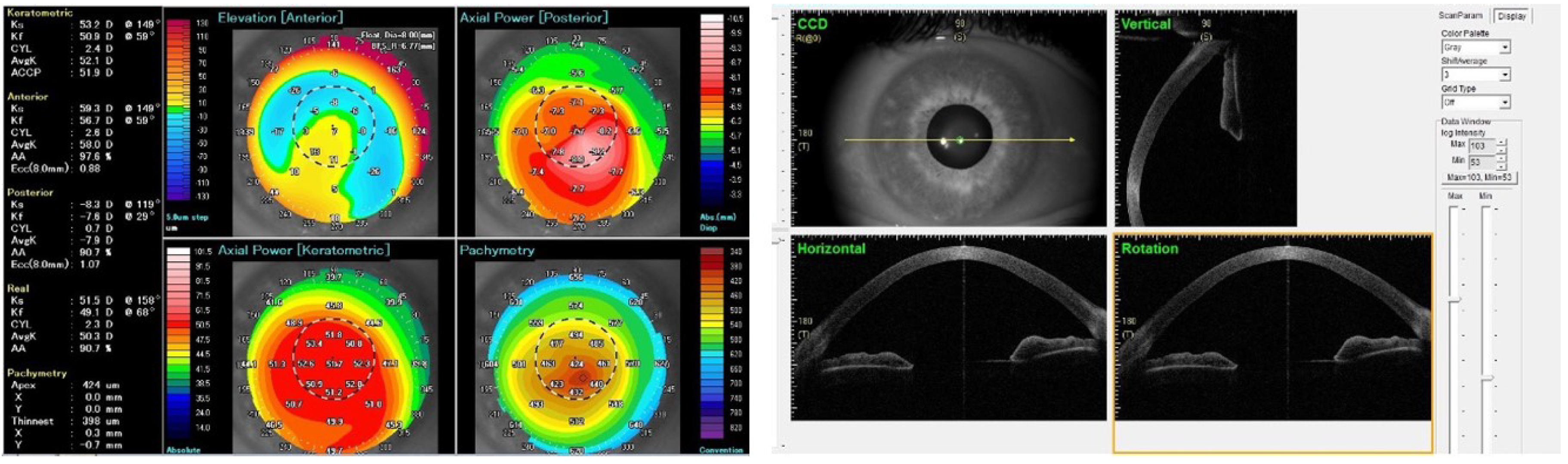
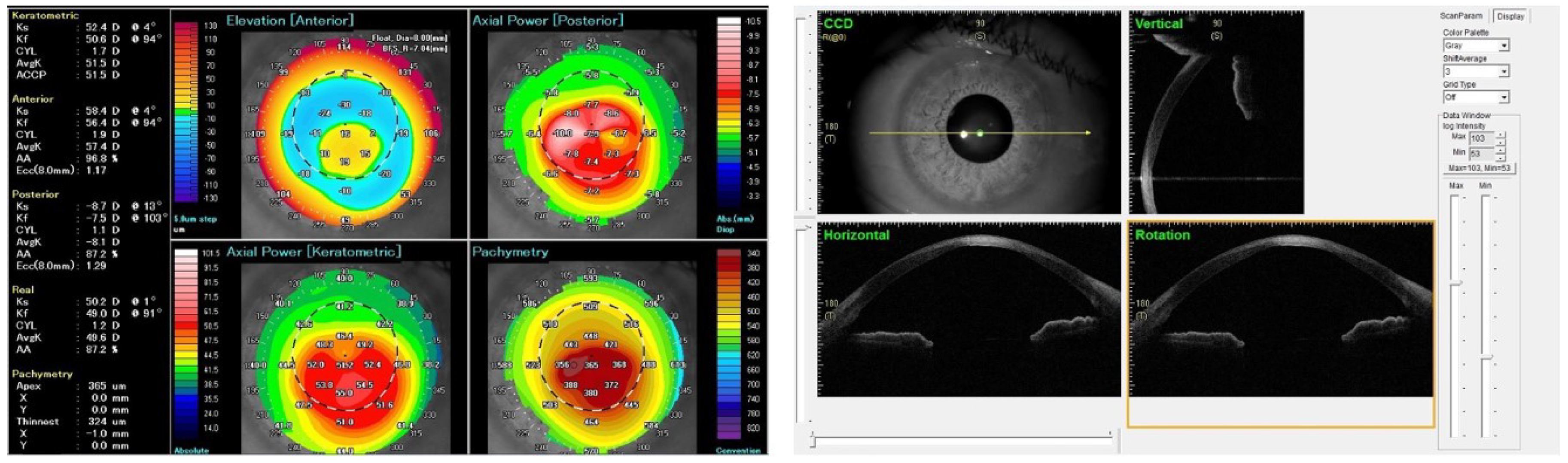
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Scorcia, V.; Giannaccare, G.; Logozzo, L.; Soda, M. Keratoconus: Advances in anterior lamellar keratoplasty techniques. Expert Rev. Ophthalmol. 2020, 15, 59–66. [Google Scholar] [CrossRef]
- Kennedy, R.H.; Bourne, W.M.; Dyer, J.A. A 48-year clinical and epidemiologic study of keratoconus. Am. J. Ophthalmol. 1986, 101, 267–273. [Google Scholar] [CrossRef]
- Amsler, M. Le kératôcne fruste au Javal. Ophtalmologica 1938, 96, 77–83. [Google Scholar] [CrossRef]
- Rabinowitz, Y.S.; Rasheed, K. KISA% index: A quantitative videokeratography algorithm embodying minimal topographic criteria for diagnosing keratoconus. J. Cataract Refract. Surg. 1999, 25, 1327–1335. [Google Scholar] [CrossRef]
- Maeda, N.; Klyce, S.D.; Smolek, M.K.; Thompson, H.W. Automated keratoconus screening with corneal topography analysis. Investig. Ophthalmol. Vis. Sci. 1994, 35, 2749–2757. [Google Scholar]
- Kamiya, K.; Ishii, R.; Shimizu, K.; Igarashi, A. Evaluation of corneal elevation, pachymetry and keratometry in keratoconic eyes with respect to the stage of Amsler-Krumeich classification. Br. J. Ophthalmol. 2014, 98, 459–463. [Google Scholar] [CrossRef] [PubMed]
- Krumeich, J.H.; Daniel, J.; Knülle, A. Live-epikeratophakia for keratoconus. J. Cataract Refract. Surg. 1998, 24, 456–463. [Google Scholar] [CrossRef]
- Christopoulos, V.; Kagemann, L.; Wollstein, G.; Ishikawa, H.; Gabriele, M.L.; Wojtkowski, M.; Srinivasan, V.; Fujimoto, J.G.; Duker, J.S.; Dhaliwal, D.K.; et al. In vivo corneal high-speed, ultra high-resolution optical coherence tomography. Arch. Ophthalmol. 2007, 125, 1027–1035. [Google Scholar] [CrossRef] [PubMed]
- Yadav, R.; Kottaiyan, R.; Ahmad, K.; Yoon, G. Epithelium and Bowman’s layer thickness and light scatter in keratoconic cornea evaluated using ultrahigh resolution optical coherence tomography. J. Biomed. Opt. 2012, 17, 116010. [Google Scholar] [CrossRef] [PubMed]
- Sandali, O.; El Sanharawi, M.; Temstet, C.; Hamiche, T.; Galan, A.; Ghouali, W.; Goemaere, I.; Basli, E.; Borderie, V.; Laroche, L. Fourier-domain optical coherence tomography imaging in keratoconus: A corneal structural classification. Ophthalmology 2013, 120, 2403–2412. [Google Scholar] [CrossRef] [PubMed]
- Belin, M.W.; Duncan, J.K. Keratoconus: The ABCD grading system. Klin. Monbl. Augenheilkd. 2016, 233, 701–707. [Google Scholar] [CrossRef] [PubMed]
- Busin, M.; Scorcia, V.; Leon, P.; Nahum, Y. Outcomes of Air Injection Within 2 mm Inside a Deep Trephination for Deep Anterior Lamellar Keratoplasty in Eyes With Keratoconus. Am. J. Ophthalmol. 2016, 164, 6–13. [Google Scholar] [CrossRef] [PubMed]
- Yu, A.C.; Mattioli, L.; Busin, M. Optimizing outcomes for keratoplasty in ectatic corneal disease. Curr. Opin. Ophthalmol. 2020, 31, 268–275. [Google Scholar] [CrossRef] [PubMed]
- Busin, M.; Leon, P.; Nahum, Y.; Scorcia, V. Large (9 mm) Deep Anterior Lamellar Keratoplasty with Clearance of a 6-mm Optical Zone Optimizes Outcomes of Keratoconus Surgery. Ophthalmology 2017, 124, 1072–1080. [Google Scholar] [CrossRef] [PubMed]
- Scorcia, V.; Giannaccare, G.; Lucisano, A.; Soda, M.; Scalzo, G.C.; Myerscough, J.; Pellegrini, M.; Verdoliva, F.; Piccoli, G.; Bovone, C.; et al. Predictors of Bubble Formation and Type Obtained With Pneumatic Dissection during Deep Anterior Lamellar Keratoplasty in Keratoconus. Am. J. Ophthalmol. 2020, 212, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Borderie, V.M.; Touhami, S.; Georgeon, C.; Sandali, O. Predictive Factors for Successful Type 1 Big Bubble during Deep Anterior Lamellar Keratoplasty. J. Ophthalmol. 2018, 2018, 4685406. [Google Scholar] [CrossRef] [PubMed]
- Ozmen, M.C.; Yesilirmak, N.; Aydin, B.; Ceylanoglu, K.S.; Atalay, H.T.; Akata, F. Prediction of Descemet Membrane Perforation During Deep Anterior Lamellar Keratoplasty in Patients With Keratoconus With Stromal Scar. Eye Contact Lens 2018, 44, S176–S179. [Google Scholar] [CrossRef] [PubMed]
- Gomes, J.A.; Tan, D.; Rapuano, C.J.; Belin, M.W.; Ambrósio, R., Jr.; Guell, J.L.; Malecaze, F.; Nishida, K.; Sangwan, V.S. Group of Panelists for the Global Delphi Panel of Keratoconus and Ectatic Diseases. Global con-sensus on keratoconus and ectatic diseases. Cornea 2015, 34, 359–369. [Google Scholar] [CrossRef] [PubMed]
| STAGE I: Eccentric steepening myopia/astigmatism < 5.00 D Mean keratometry value < 48.0 D | STAGE 1: Thinning of epithelial and stromal layers at the conus Corneal layers with normal aspect |
| STAGE II: Myopia/astigmatism > 5.00 D but <8.00 D Mean keratometry value < 53.0 D Absence of scarring Minimal apical corneal thickness > 400 μm | STAGE 2A: Hyperreflective anomalies at the Bowman’s layer level with epithelial thickening |
| STAGE 2B: Hyperreflective anomalies at the Bowman’s layer level with epithelial thickening plus stromal opacities | |
| STAGE III: Myopia/astigmatism > 8.00 D but <10.00 D Mean keratometry value > 53.0 D Absence of scarring Minimal apical corneal thickness < 400 μm but >300 μm | STAGE 3A: Posterior displacement of the hyperreflective structures at the Bowman’s layer level with increased epithelial thickening Stromal thinning |
| STAGE 3B: Posterior displacement of the hyperreflective structures at the Bowman’s layer level with increased epithelial thickening Stromal thinning plus the presence of stromal opacities | |
| STAGE IV: Refraction not possible Mean keratometry value > 55.0 D Central corneal scarring Minimal apical corneal thickness < 300 μm | STAGE 4: Pan stromal scar |
| STAGE 5A: Acute onset with Descemet’s membrane rupture with dilacerations of collagen lamellae, large fluid filled intrastromal cysts and epithelial edema formation | |
| STAGE 5B: Healing stage of 5A with panstromal scarring with remaining aspect of Descemet’s membrane rupture. |
| All Eyes | Stage 1 | Stage 2 | Stage 3 | Stage 4 | |
|---|---|---|---|---|---|
| (n = 252) | (n = 3) | (n = 144) | (n = 69) | (n = 36) | |
| K steep, anterior (D) | |||||
| mean ± SD | 59.22 ± 8.55 | 49.40 ± 1.27 | 54.76 ±3.66 | 61.14 ± 5.82 | 74.21 ± 8.68 |
| K flat, anterior (D) | |||||
| mean ± SD | 55.34 ± 7.45 | 47.53 ± 0.75 | 51.45 ± 2.99 | 57.03 ± 5.09 | 68.34 ± 8.03 |
| Cyl, anterior (D) mean ± SD | |||||
| 3.87 ± 2.39 | 1.80 ± 0.96 | 3.31 ± 1.77 | 4.10 ± 2.44 | 5.86 ± 3.27 | |
| K steep, posterior (D) | |||||
| mean ± SD | −8.20 ± 1.44 | −6.43 ± 0.25 | −7.42 ± 0.71 | −8.59 ± 0.93 | −10.75 ± 1.19 |
| K flat, posterior (D) | |||||
| mean ± SD | −7.52 ± 1.28 | −6.03 ± 0.32 | −6.83 ± 0.65 | −7.87 ± 0.91 | −9.69 ± 1.11 |
| Cyl, posterior (D) | |||||
| mean ± SD | 0.68 ± 0.38 | 0.40 ± 0.10 | 0.58 ± 0.27 | 0.69 ± 0.33 | 1.04 ± 0.57 |
| TCT (μm) | |||||
| mean ± SD | 406.14 ± 72.35 | 523.67 ± 11.93 | 450.94 ±27.39 | 374.83 ± 27.33 | 277.19 ± 67.35 |
| All Eyes | Stage 1 | Stage 2 | Stage 3 | Stage 4 | Stage 5 | |
|---|---|---|---|---|---|---|
| (n = 252) | (n = 206) | (n = 16) | (n = 2) | (n = 25) | (n = 3) | |
| K steep, anterior (D) | ||||||
| mean ± SD | 59.22 ± 8.55 | 56.40 ± 5.03 | 75.14 ± 10.71 | 69.55 ± 8.83 | 69.08 ± 8.75 | 78.97 ± 2.45 |
| K flat, anterior (D) | ||||||
| mean ± SD | 55.34 ± 7.45 | 52.89 ± 4.32 | 69.71 ± 9.94 | 63.85 ± 6.71 | 63.86 ± 7.57 | 70.60 ± 2.36 |
| Cyl, anterior (D) | ||||||
| mean ± SD | 3.87 ± 2.39 | 3.51 ± 1.97 | 5.43 ± 2.47 | 5.70 ± 2.12 | 5.20 ± 3.70 | 8.47 ± 4.30 |
| K steep, posterior (D) | ||||||
| mean ± SD | −8.20 ± 1.44 | −7.71 ± 0.92 | −10.56 ± 1.45 | −10.15 ± 1.90 | −10.19 ± 1.27 | −11.20 ± 1.67 |
| K flat, posterior (D) | ||||||
| mean ± SD | −7.52 ± 1.28 | −7.10 ± 0.85 | −9.62 ± 1.20 | −9.35 ± 2.05 | −9.26 ± 1.18 | −9.47 ± 1.28 |
| Cyl, posterior (D) | ||||||
| mean ± SD | 0.68 ± 0.38 | 0.61 ± 0.29 | 0.94 ± 0.51 | 0.80 ± 0.14 | 0.90 ± 0.53 | 1.70 ± 0.98 |
| TCT (μm) | ||||||
| mean ± SD | 406.14 ± 72.35 | 429.17 ± 47.62 | 306.75 ± 67.52 | 286.00 ± 83.43 | 300.44 ± 81.76 | 315.67 ± 80.85 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giannaccare, G.; Murano, G.; Carnevali, A.; Yu, A.C.; Vaccaro, S.; Scuteri, G.; Maltese, L.; Scorcia, V. Comparison of Amsler–Krumeich and Sandali Classifications for Staging Eyes with Keratoconus. Appl. Sci. 2021, 11, 4007. https://doi.org/10.3390/app11094007
Giannaccare G, Murano G, Carnevali A, Yu AC, Vaccaro S, Scuteri G, Maltese L, Scorcia V. Comparison of Amsler–Krumeich and Sandali Classifications for Staging Eyes with Keratoconus. Applied Sciences. 2021; 11(9):4007. https://doi.org/10.3390/app11094007
Chicago/Turabian StyleGiannaccare, Giuseppe, Gianluca Murano, Adriano Carnevali, Angeli Christy Yu, Sabrina Vaccaro, Gianfranco Scuteri, Laura Maltese, and Vincenzo Scorcia. 2021. "Comparison of Amsler–Krumeich and Sandali Classifications for Staging Eyes with Keratoconus" Applied Sciences 11, no. 9: 4007. https://doi.org/10.3390/app11094007
APA StyleGiannaccare, G., Murano, G., Carnevali, A., Yu, A. C., Vaccaro, S., Scuteri, G., Maltese, L., & Scorcia, V. (2021). Comparison of Amsler–Krumeich and Sandali Classifications for Staging Eyes with Keratoconus. Applied Sciences, 11(9), 4007. https://doi.org/10.3390/app11094007








