The Rate of Correctly Planned Size of Digital Templating in Two Planes—A Comparative Study of a Short-Stem Total Hip Implant with Primary Metaphyseal Fixation and a Conventional Stem
Abstract
1. Introduction
2. Materials and Methods
Statistics
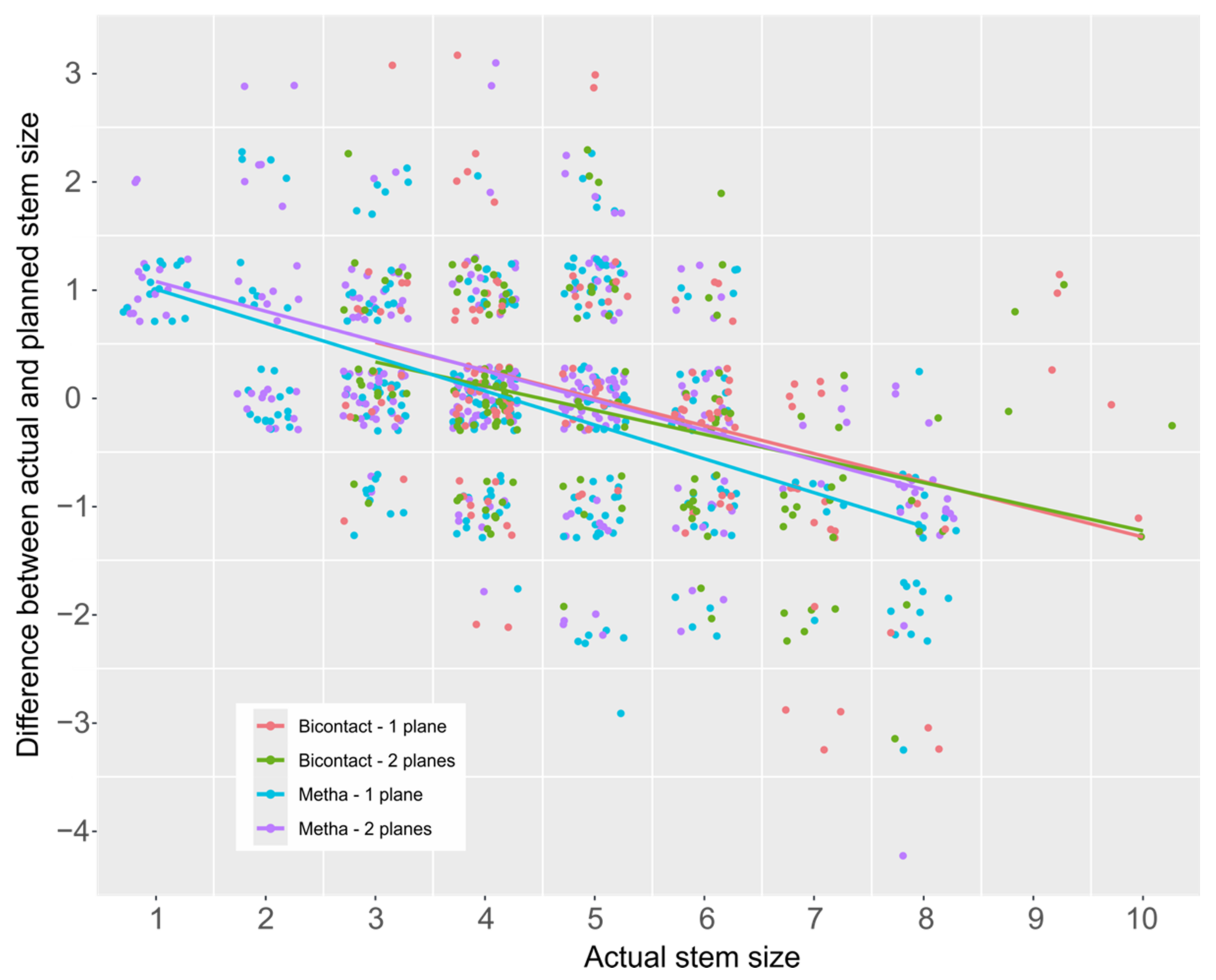
3. Results
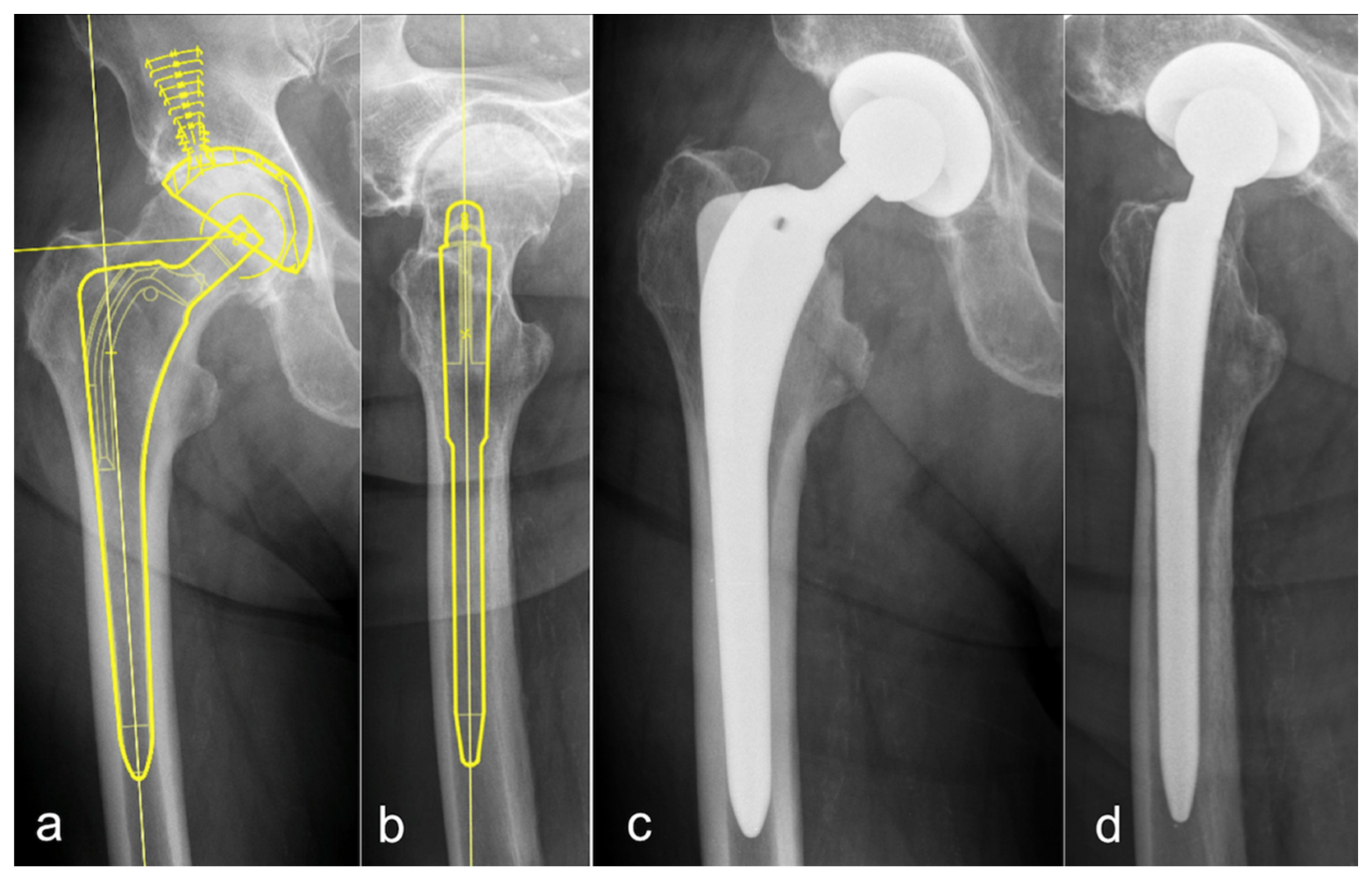
3.1. Conventional Stem Total Hip Arthroplasty (CTHA)—Conventional Templating in One Plane on the a.p. Pelvic Overview
3.2. CTHA—Templating in Two Planes—a.p. and Lateral View
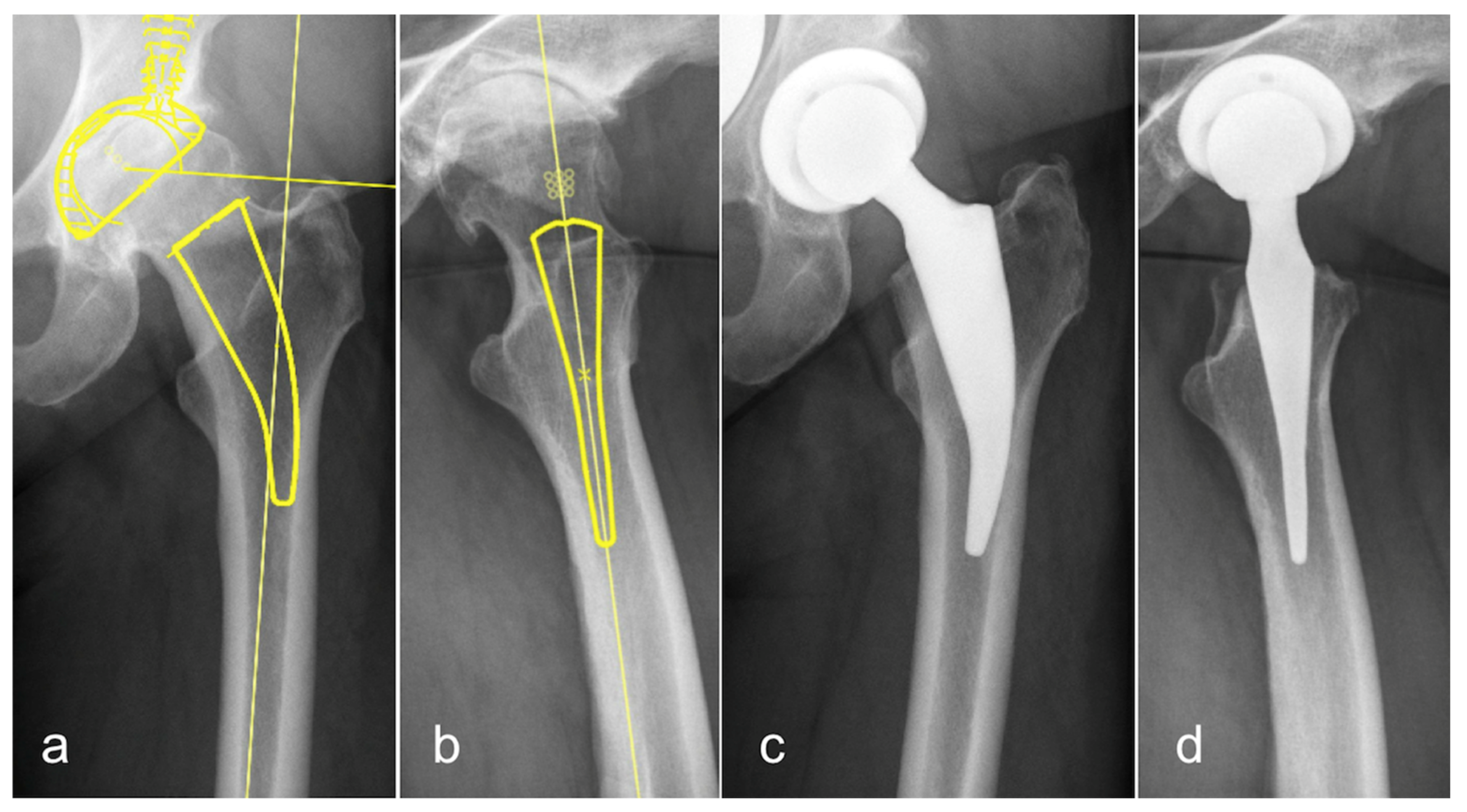
3.3. Short Stem Total Hip Arthroplasty (STHA)—Conventional Templating in One Plane on the a.p. Pelvic Overview
3.4. STHA—Templating in Two Planes—a.p. and Lateral View
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Efe, T.; El Zayat, B.F.; Heyse, T.J.; Timmesfeld, N.; Fuchs-Winkelmann, S.; Schmitt, J. Precision of preoperative digital templating in total hip arthroplasty. Acta Orthop. Belg. 2011, 77, 616–621. [Google Scholar] [PubMed]
- Haddad, F.S.; Masri, B.A.; Garbuz, D.S.; Duncan, C.P. The prevention of periprosthetic fractures in total hip and knee arthroplasty. Orthop. Clin. N. Am. 1999, 30, 191–207. [Google Scholar] [CrossRef]
- Haddad, F.S.; Masri, B.A.; Garbuz, D.S.; Duncan, C.P. Femoral bone loss in total hip arthroplasty: Classification and preoperative planning. Instr. Course Lect. 2000, 49, 83–96. [Google Scholar] [PubMed]
- Muller, M.E. Lessons of 30 years of total hip arthroplasty. Clin. Orthop. Relat. Res. 1992, 12–21. [Google Scholar]
- Bono, J.V. Digital templating in total hip arthroplasty. J. Bone Jt. Surg. Am. 2004, 86 (Suppl. 2), 118–122. [Google Scholar] [CrossRef]
- Della Valle, A.G.; Padgett, D.E.; Salvati, E.A. Preoperative planning for primary total hip arthroplasty. J. Am. Acad. Orthop. Surg. 2005, 13, 455–462. [Google Scholar] [CrossRef]
- Fottner, A.; Steinbruck, A.; Sadoghi, P.; Mazoochian, F.; Jansson, V. Digital comparison of planned and implanted stem position in total hip replacement using a program form migration analysis. Arch. Orthop. Trauma Surg. 2011, 131, 1013–1019. [Google Scholar] [CrossRef]
- Lecerf, G.; Fessy, M.H.; Philippot, R.; Massin, P.; Giraud, F.; Flecher, X.; Girard, J.; Mertl, P.; Marchetti, E.; Stindel, E. Femoral offset: Anatomical concept, definition, assessment, implications for preoperative templating and hip arthroplasty. Orthop. Traumatol. Surg. Res. 2009, 95, 210–219. [Google Scholar] [CrossRef]
- Kamada, S.; Naito, M.; Nakamura, Y.; Kiyama, T. Hip abductor muscle strength after total hip arthroplasty with short stems. Arch. Orthop. Trauma Surg. 2011, 131, 1723–1729. [Google Scholar] [CrossRef]
- Suh, K.T.; Cheon, S.J.; Kim, D.W. Comparison of preoperative templating with postoperative assessment in cementless total hip arthroplasty. Acta Orthop. Scand. 2004, 75, 40–44. [Google Scholar] [CrossRef]
- Schmidutz, F.; Steinbruck, A.; Wanke-Jellinek, L.; Pietschmann, M.; Jansson, V.; Fottner, A. The accuracy of digital templating: A comparison of short-stem total hip arthroplasty and conventional total hip arthroplasty. Int. Orthop. 2012, 36, 1767–1772. [Google Scholar] [CrossRef]
- The, B.; Verdonschot, N.; van Horn, J.R.; van Ooijen, P.M.; Diercks, R.L. Digital versus analogue preoperative planning of total hip arthroplasties: A randomized clinical trial of 210 total hip arthroplasties. J. Arthroplast. 2007, 22, 866–870. [Google Scholar] [CrossRef]
- Gamble, P.; de Beer, J.; Petruccelli, D.; Winemaker, M. The accuracy of digital templating in uncemented total hip arthroplasty. J Arthroplast. 2010, 25, 529–532. [Google Scholar] [CrossRef]
- Schiffner, E.; Latz, D.; Jungbluth, P.; Grassmann, J.P.; Tanner, S.; Karbowski, A.; Windolf, J.; Schneppendahl, J. Is computerised 3D templating more accurate than 2D templating to predict size of components in primary total hip arthroplasty? Hip Int. 2019, 29, 270–275. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020; Available online: http://www.R-project.org (accessed on 27 April 2021).
- Wickham, H. ggplot2: Elegant Graphics for Data Analysis; Springer: New York, NY, USA, 2009. [Google Scholar]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Lerch, M.; von der Haar-Tran, A.; Windhagen, H.; Behrens, B.A.; Wefstaedt, P.; Stukenborg-Colsman, C.M. Bone remodelling around the Metha short stem in total hip arthroplasty: A prospective dual-energy X-ray absorptiometry study. Int. Orthop. 2012, 36, 533–538. [Google Scholar] [CrossRef]
- Thorey, F.; Hoefer, C.; Abdi-Tabari, N.; Lerch, M.; Budde, S.; Windhagen, H. Clinical results of the metha short hip stem: A perspective for younger patients? Orthop. Rev. 2013, 5, e34. [Google Scholar] [CrossRef][Green Version]
- Iorio, R.; Siegel, J.; Specht, L.M.; Tilzey, J.F.; Hartman, A.; Healy, W.L. A comparison of acetate vs digital templating for preoperative planning of total hip arthroplasty: Is digital templating accurate and safe? J. Arthroplast. 2009, 24, 175–179. [Google Scholar] [CrossRef]
- Morrey, B.F.; Adams, R.A.; Kessler, M. A conservative femoral replacement for total hip arthroplasty. A prospective study. J. Bone Jt. Surg. Br. 2000, 82, 952–958. [Google Scholar] [CrossRef]
- Crooijmans, H.J.; Laumen, A.M.; van Pul, C.; van Mourik, J.B. A new digital preoperative planning method for total hip arthroplasties. Clin. Orthop. Relat. Res. 2009, 467, 909–916. [Google Scholar] [CrossRef]
- Hsu, A.R.; Kim, J.D.; Bhatia, S.; Levine, B.R. Effect of training level on accuracy of digital templating in primary total hip and knee arthroplasty. Orthopedics 2012, 35, e179–e183. [Google Scholar] [CrossRef] [PubMed]
- Wedemeyer, C.; Quitmann, H.; Xu, J.; Heep, H.; von Knoch, M.; Saxler, G. Digital templating in total hip arthroplasty with the Mayo stem. Arch. Orthop. Trauma Surg. 2008, 128, 1023–1029. [Google Scholar] [CrossRef] [PubMed]
- Jakubowitz, E.; Seeger, J.B.; Lee, C.; Heisel, C.; Kretzer, J.P.; Thomsen, M.N. Do short-stemmed-prostheses induce periprosthetic fractures earlier than standard hip stems? A biomechanical ex-vivo study of two different stem designs. Arch. Orthop. Trauma Surg. 2009, 129, 849–855. [Google Scholar] [CrossRef] [PubMed]
- Braun, A.; Sabah, A. Two-year results of a modular short hip stem prosthesis—A prospective study. Z. Orthop. Unfall 2009, 147, 700–706. [Google Scholar] [CrossRef]
- Von Lewinski, G.; Floerkemeier, T. 10-year experience with short stem total hip arthroplasty. Orthopedics 2015, 38, S51–S56. [Google Scholar] [CrossRef]
- Whiddon, D.R.; Bono, J.V.; Lang, J.E.; Smith, E.L.; Salyapongse, A.K. Accuracy of digital templating in total hip arthroplasty. Am. J. Orthop. 2011, 40, 395–398. [Google Scholar]
- Gonzalez Della Valle, A.; Comba, F.; Taveras, N.; Salvati, E.A. The utility and precision of analogue and digital preoperative planning for total hip arthroplasty. Int. Orthop. 2008, 32, 289–294. [Google Scholar] [CrossRef]
- Boese, C.K.; Wilhelm, S.; Haneder, S.; Lechler, P.; Eysel, P.; Bredow, J. Influence of calibration on digital templating of hip arthroplasty. Int. Orthop. 2019, 43, 1799–1805. [Google Scholar] [CrossRef]
- Boese, C.K.; Lechler, P.; Rose, L.; Dargel, J.; Oppermann, J.; Eysel, P.; Geiges, H.; Bredow, J. Calibration Markers for Digital Templating in Total Hip Arthroplasty. PLoS ONE 2015, 10, e0128529. [Google Scholar] [CrossRef]


| Difference in Templated Size Compared to the Truly Implanted Prosthesis | 0 | +/−1 | +/−2 | +/− > 2 | |
|---|---|---|---|---|---|
| CTHA (Templating a.p.) | Rater 1 | 52.0% | 82.0% | 90.0% | 100.0% |
| 2 | 39.1 | 89.1 | 91.3 | 100.0 | |
| 3 | 42.0 | 94.0 | 100.0 | 100.0 | |
| Mean ± Standard Deviation | 44.4 ± 6.8 | 88.4 ± 6.0 | 93.8 ± 5.4 | 100.0 ± 0 | |
| CTHA (Templating 2 Planes) | Rater 1 | 64.0% | 96.0% | 100.0% | 100.0% |
| 2 | 26.1 | 78.2 | 97.8 | 100.0 | |
| 3 | 30.0 | 94.0 | 100.0 | 100.0 | |
| Mean ± Standard Deviation | 40.0 ± 20.8 | 89.4 ± 9.8 | 99.3 ± 1.3 | 100.0 ± 0 | |
| STHA (Templating a.p.) | Rater 1 | 45.0% | 83.0% | 99.0% | 100.0% |
| 2 | 16.7 | 78.9 | 100.0 | 100.0 | |
| 3 | 47.0 | 97.0 | 100.0 | 100.0 | |
| Mean ± Standard Deviation | 36.2 ± 16.9 | 86.3 ± 9.5 | 99.7 ± 0.6 | 100.0 ± 0 | |
| STHA (Templating 2 Planes) | Rater 1 | 60.0% | 93.0% | 100.0% | 100.0% |
| 2 | 18.9 | 76.7 | 94.5 | 100.0 | |
| 3 | 71.0 | 100.0 | 100.0 | 100.0 | |
| Mean ± Standard Deviation | 50.0 ± 27.5 | 89.9 ± 12.0 | 98.2 ± 3.2 | 100.0 ± 0 | |
| Stem Size | CTHA | STHA |
|---|---|---|
| a.p. planning | 0.774 | 0.736 |
| a.p. + lateral planning | 0.838 | 0.757 |
| Difference to Implanted Size | CTHA | STHA |
| a.p. planning | 0.586 | 0.483 |
| a.p. + lateral planning | 0.623 | 0.422 |
| Stem Size | CTHA | STHA |
|---|---|---|
| a.p. planning | 0.911 | 0.893 |
| a.p. + lateral planning | 0.94 | 0.903 |
| Difference to Implanted Size | CTHA | STHA |
| a.p. planning | 0.81 | 0.737 |
| a.p. + lateral planning | 0.832 | 0.687 |
| Stem Size | CTHA | STHA |
|---|---|---|
| a.p. planning | 0.411 | 0.228 |
| a.p. + lateral planning | 0.27 | 0.3 |
| Difference to Implanted Size | CTHA | STHA |
| a.p. planning | 0.33 | 0.149 |
| a.p. + lateral planning | 0.178 | 0.16 |
| CTHA | STHA | |||
|---|---|---|---|---|
| r | p | r | p | |
| a.p. planning | 0.029 | 0.266 | 0.023 | 0.131 |
| a.p. + lateral planning | 0.035 | 0.196 | 0.054 | 0.008 |
| Stem Size | CTHA | STHA | ||
|---|---|---|---|---|
| r | p | r | p | |
| a.p. planning | 0.74 | 0.001 | 0.80 | 0.001 |
| a.p. + lateral planning | 0.79 | 0.001 | 0.84 | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buschatzky, J.K.; Schwarze, M.; Wirries, N.; von Lewinski, G.; Windhagen, H.; Floerkemeier, T.; Budde, S. The Rate of Correctly Planned Size of Digital Templating in Two Planes—A Comparative Study of a Short-Stem Total Hip Implant with Primary Metaphyseal Fixation and a Conventional Stem. Appl. Sci. 2021, 11, 3965. https://doi.org/10.3390/app11093965
Buschatzky JK, Schwarze M, Wirries N, von Lewinski G, Windhagen H, Floerkemeier T, Budde S. The Rate of Correctly Planned Size of Digital Templating in Two Planes—A Comparative Study of a Short-Stem Total Hip Implant with Primary Metaphyseal Fixation and a Conventional Stem. Applied Sciences. 2021; 11(9):3965. https://doi.org/10.3390/app11093965
Chicago/Turabian StyleBuschatzky, Johanna K., Michael Schwarze, Nils Wirries, Gabriela von Lewinski, Henning Windhagen, Thilo Floerkemeier, and Stefan Budde. 2021. "The Rate of Correctly Planned Size of Digital Templating in Two Planes—A Comparative Study of a Short-Stem Total Hip Implant with Primary Metaphyseal Fixation and a Conventional Stem" Applied Sciences 11, no. 9: 3965. https://doi.org/10.3390/app11093965
APA StyleBuschatzky, J. K., Schwarze, M., Wirries, N., von Lewinski, G., Windhagen, H., Floerkemeier, T., & Budde, S. (2021). The Rate of Correctly Planned Size of Digital Templating in Two Planes—A Comparative Study of a Short-Stem Total Hip Implant with Primary Metaphyseal Fixation and a Conventional Stem. Applied Sciences, 11(9), 3965. https://doi.org/10.3390/app11093965






