A Proposed Protocol for Ordinary and Extraordinary Hygienic Maintenance in Different Implant Prosthetic Scenarios
Abstract
1. Introduction
2. Materials and Methods
3. Results and Discussion
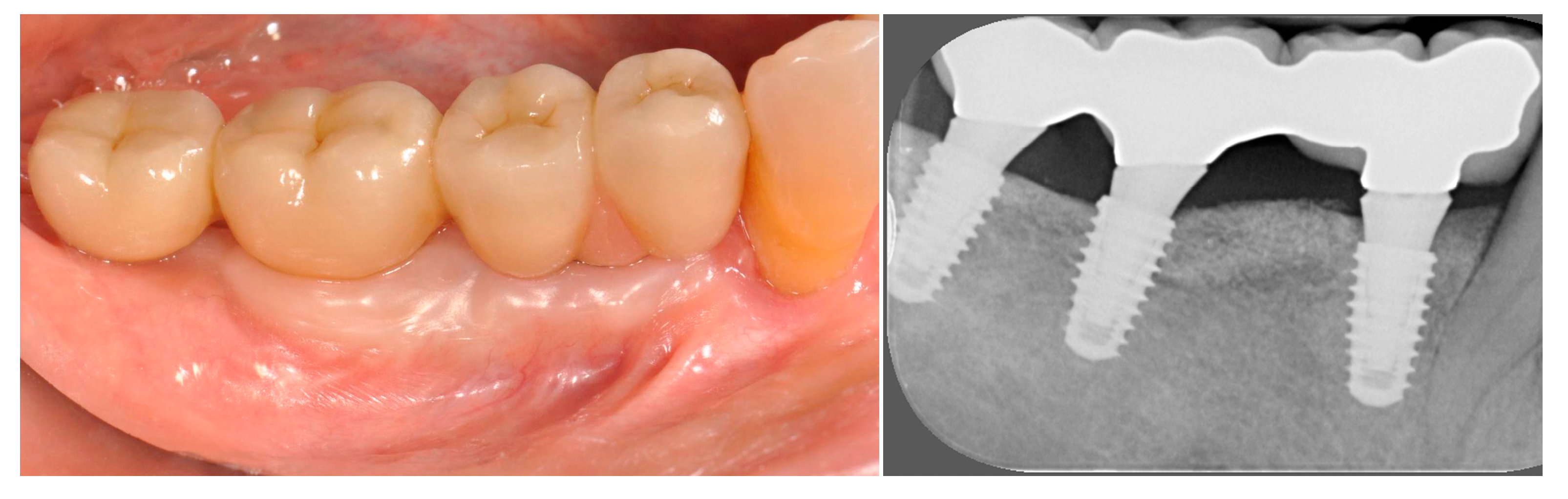
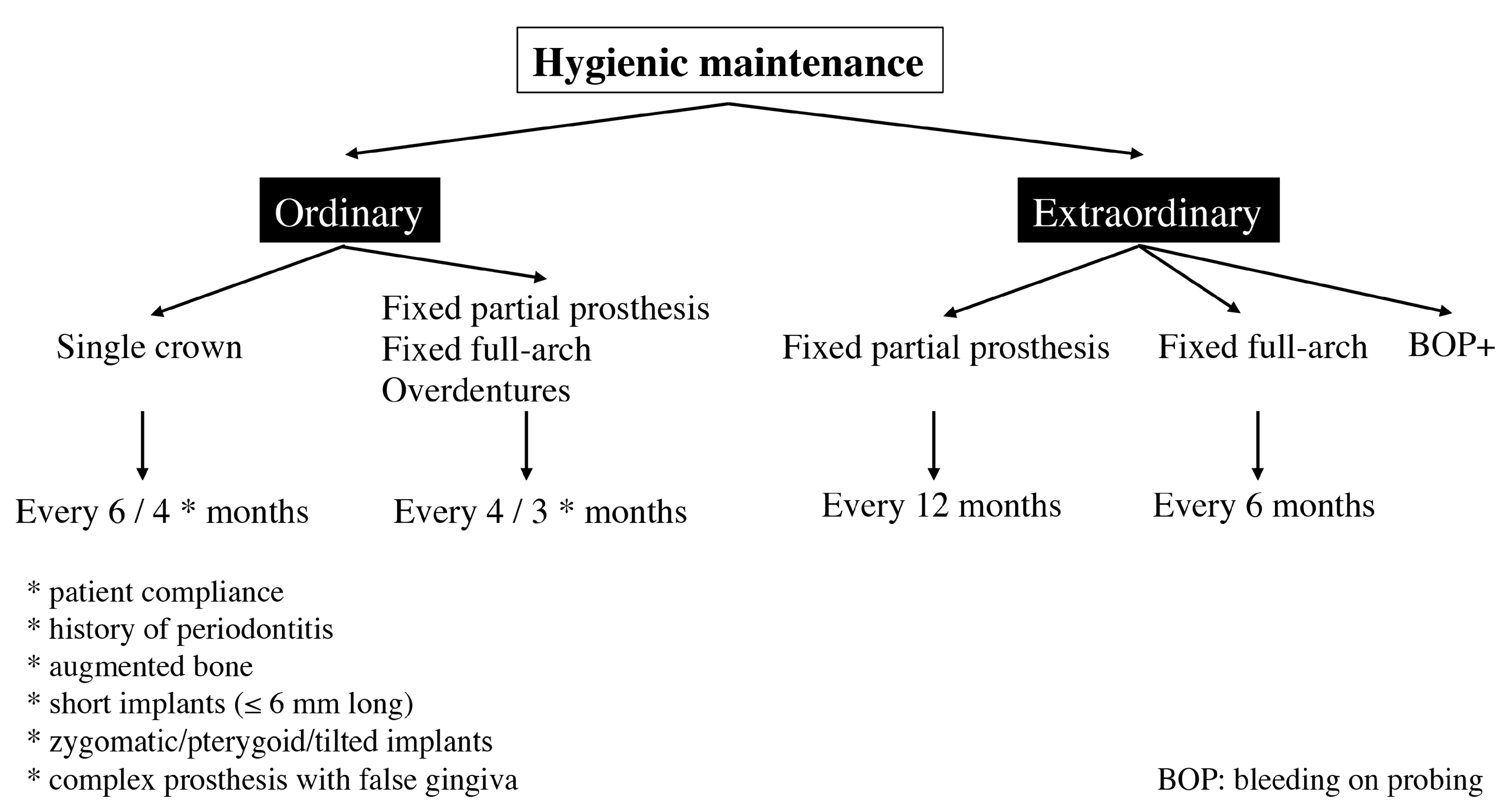
3.1. Single Crowns
3.2. Fixed Partial Prostheses
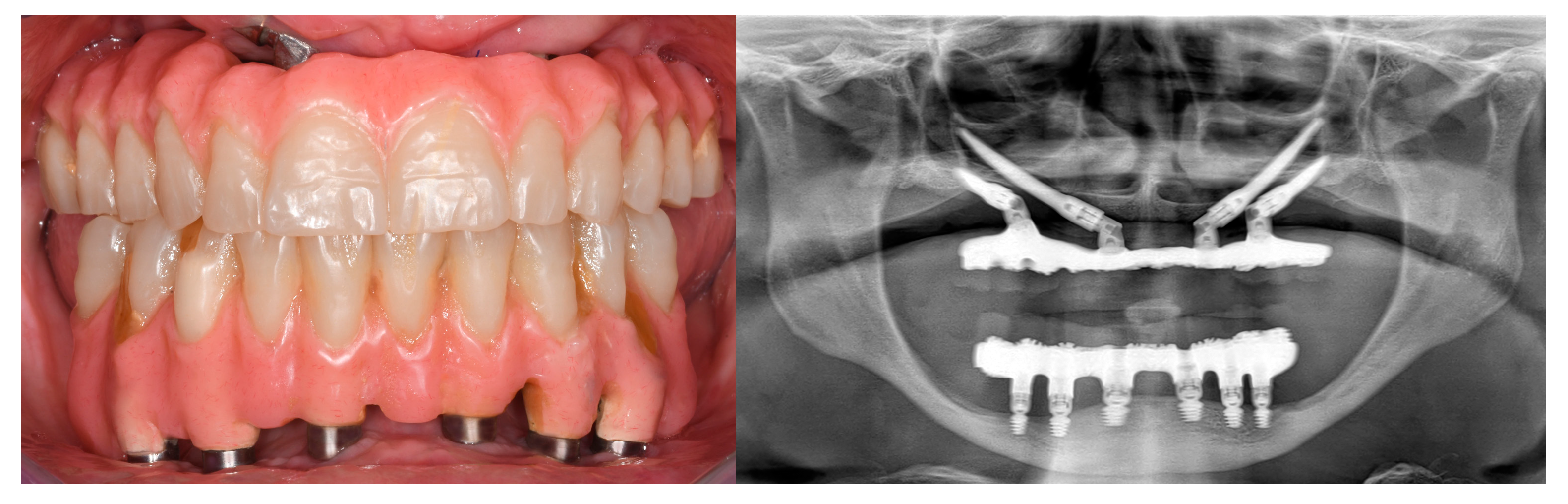
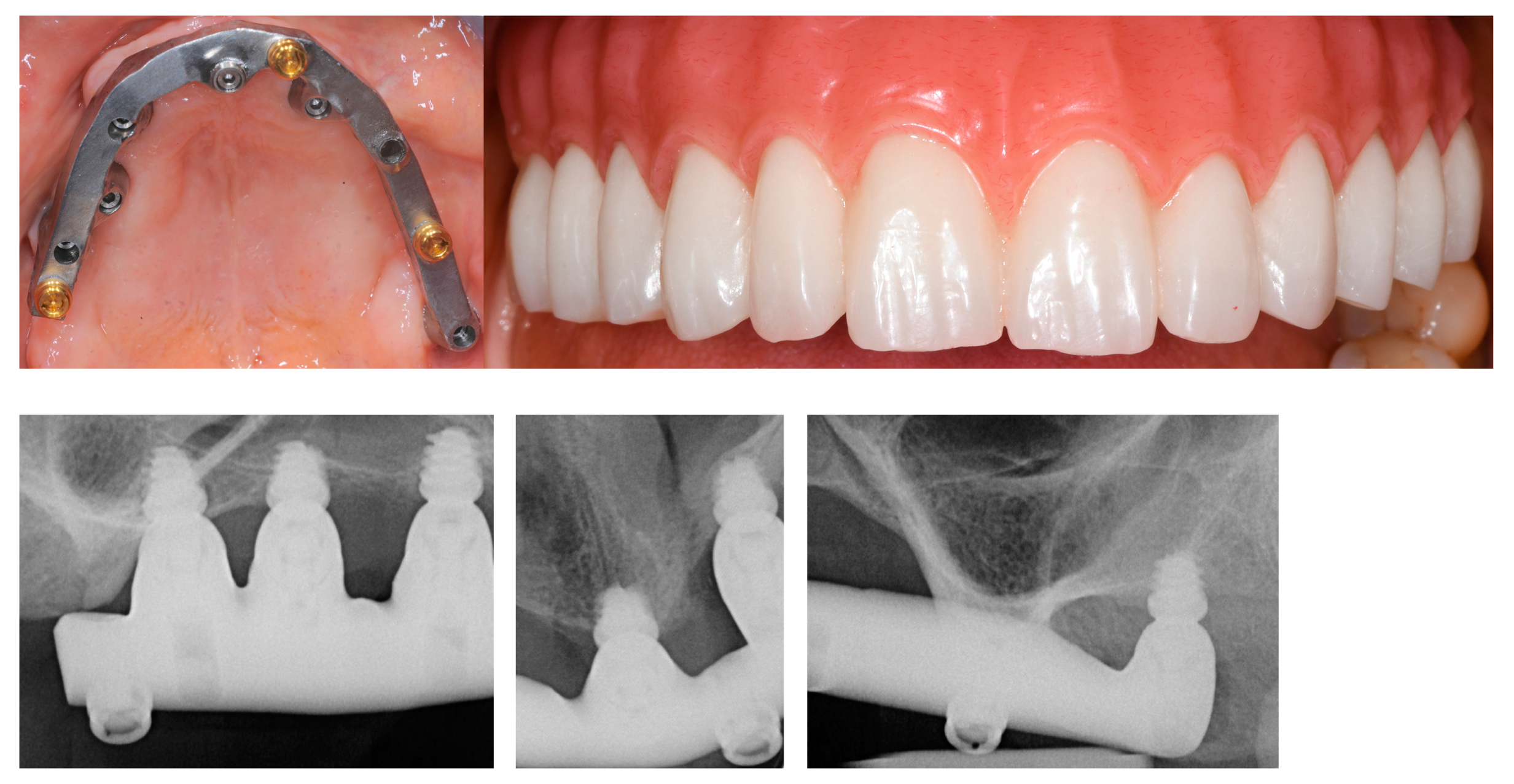
3.3. Fixed Full-Arch Prostheses
3.4. Overdentures (OVD)
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jepsen, S.; Berglundh, T.; Genco, R.; Aass, A.M.; Demirel, K.; Derks, J.; Figuero, E.; Giovannoli, J.L.; Goldstein, M.; Lambert, F.; et al. Primary prevention of peri-implantitis: Managing peri-implant mucositis. J. Clin. Periodontol. 2015, 42, S152–S157. [Google Scholar] [CrossRef] [PubMed]
- Menini, M.; Setti, P.; Pera, P.; Pera, F.; Pesce, P. Peri-implant Tissue Health and Bone Resorption in Patients with Immediately Loaded, Implant-Supported, Full-Arch Prostheses. Int. J. Prosthodont. 2018, 31, 327–333. [Google Scholar] [CrossRef]
- Crespi, R.; Capparé, P.; Crespi, G.; Lo Giudice, G.; Gastaldi, G.; Gherlone, E. Immediate Implant Placement in Sockets with Asymptomatic Apical Periodontitis. Clin. Implant. Dent. Relat. Res. 2017, 19, 20–27. [Google Scholar] [CrossRef]
- Tribst, J.P.M.; Dal Piva, A.M.O.; Lo Giudice, R.; Borges, A.L.S.; Bottino, M.A.; Epifania, E.; Ausiello, P. The Influence of Custom-Milled Framework Design for an Implant-Supported Full-Arch Fixed Dental Prosthesis: 3D-FEA Sudy. Int. J. Environ. Res. Public Health 2020, 17, 4040. [Google Scholar] [CrossRef]
- Troiano, A.; Lo Giudice, G.; De Luca, R.; Lo Giudice, F.; D’Amato, S.; Tartaro, G.; Colella, G. Salvage of Dental Implant Located in Mandibular Odontogenic Cyst. A Conservative Surgical Treatment Proposal. Dent. J. 2020, 8, 49. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, F.; Derks, J.; Monje, A.; Wang, H.L. Peri-implantitis. J. Clin. Periodontol. 2018, 45, S246–S266. [Google Scholar] [CrossRef]
- Matarese, G.; Ramaglia, L.; Fiorillo, L.; Cervino, G.; Lauritano, F.; Isola, G. Implantology and Periodontal Disease: The Panacea to Problem Solving? Open Dent. J. 2017, 11, 460–465. [Google Scholar] [CrossRef]
- Di Gianfilippo, R.; Sirinirund, B.; Rodriguez, M.V.; Chen, Z.; Wang, H.-L. Long-Term Prognosis of Peri-Implantitis Treatment: A Systematic Review of Prospective Trials with More Than 3 Years of Follow-Up. Appl. Sci. 2020, 10, 17. [Google Scholar] [CrossRef]
- Pesce, P.; Canullo, L.; Grusovin, M.G.; de Bruyn, H.; Cosyn, J.; Pera, P. Systematic review of some prosthetic risk factors for periimplantitis. J. Prosthet. Dent. 2015, 114, 346–350. [Google Scholar] [CrossRef] [PubMed]
- Turri, A.; Rossetti, P.H.; Canullo, L.; Grusovin, M.G.; Dahlin, C. Prevalence of Peri-implantitis in Medically Compromised Patients and Smokers: A Systematic Review. Int. J. Oral Maxillofac. Implants 2016, 31, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Rakic, M.; Galindo-Moreno, P.; Monje, A.; Radovanovic, S.; Wang, H.L.; Cochran, D.; Sculean, A.; Canullo, L. How frequent does peri-implantitis occur? A systematic review and meta-analysis. Clin. Oral Investig. 2018, 22, 1805–1816. [Google Scholar] [CrossRef] [PubMed]
- Tallarico, M.; Canullo, L.; Wang, H.L.; Cochran, D.L.; Meloni, S.M. Classification Systems for Peri-implantitis: A Narrative Review with a Proposal of a New Evidence-Based Etiology Codification. Int. J. Oral Maxillofac. Implants 2018, 33, 871–879. [Google Scholar] [CrossRef]
- Berglundh, T.; Armitage, G.; Araujo, M.G.; Avila-Ortiz, G.; Blanco, J.; Camargo, P.M.; Chen, S.; Cochran, D.; Derks, J.; Figuero, E.; et al. Peri-implant diseases and conditions: Consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Clin. Periodontol. 2018, 45, S286–S291. [Google Scholar] [CrossRef]
- Caton, J.G.; Armitage, G.; Berglundh, T.; Chapple, I.L.C.; Jepsen, S.; Kornman, K.S.; Mealey, B.L.; Papapanou, P.N.; Sanz, M.; Tonetti, M.S. A new classification scheme for periodontal and peri-implant diseases and conditions - Introduction and key changes from the 1999 classification. J. Clin. Periodontol. 2018, 45, S1–S8. [Google Scholar] [CrossRef]
- Schwarz, F.; Becker, K.; Sager, M. Efficacy of professionally administered plaque removal with or without adjunctive measures for the treatment of peri-implant mucositis: A systematic review and meta-analysis. J. Clin. Periodontol. 2015, 42, S202–S213. [Google Scholar] [CrossRef] [PubMed]
- Roccuzzo, M.; Bonino, L.; Dalmasso, P.; Aglietta, M. Long-term results of a three arms prospective cohort study on implants in periodontally compromised patients: 10-year data around sandblasted and acid-etched (SLA) surface. Clin. Oral Implants Res. 2014, 25, 1105–1112. [Google Scholar] [CrossRef]
- Tonetti, M.S.; Chapple, I.L.; Jepsen, S.; Sanz, M. Primary and secondary prevention of periodontal and peri-implant diseases: Introduction to, and objectives of the 11th European Workshop on Periodontology consensus conference. J. Clin. Periodontol. 2015, 42, S1–S4. [Google Scholar] [CrossRef]
- Guarnieri, R.; Di Nardo, D.; Di Giorgio, G.; Miccoli, G.; Testarelli, L. Longevity of Teeth and Dental Implants in Patients Treated for Chronic Periodontitis Following Periodontal Maintenance Therapy in a Private Specialist Practice: A Retrospective Study with a 10-Year Follow-up. Int. J. Periodontics Restor. Dent. 2021, 41, 89–98. [Google Scholar] [CrossRef] [PubMed]
- Roccuzzo, M.; Grasso, G.; Dalmasso, P. Keratinized mucosa around implants in partially edentulous posterior mandible: 10-year results of a prospective comparative study. Clin. Oral Implants Res. 2016, 27, 491–496. [Google Scholar] [CrossRef]
- Blasi, A.; Iorio-Siciliano, V.; Pacenza, C.; Pomingi, F.; Matarasso, S.; Rasperini, G. Biofilm removal from implants supported restoration using different instruments: A 6-month comparative multicenter clinical study. Clin. Oral Implants Res. 2016, 27, e68–e73. [Google Scholar] [CrossRef]
- Armitage, G.C.; Xenoudi, P. Post-treatment supportive care for the natural dentition and dental implants. Periodontol. 2000 2016, 71, 164–184. [Google Scholar] [CrossRef] [PubMed]
- Geisinger, M.L.; Ogdon, D.; Kaur, M.; Valiquette, G.; Geurs, N.C.; Reddy, M.S. Toss the Floss? Evidence-Based Oral Hygiene Recommendations for the Periodontal Patient in the Age of “Flossgate”. Clin. Adv. Periodontics 2019, 9, 83–90. [Google Scholar] [CrossRef]
- Bidra, A.S.; Daubert, D.M.; Garcia, L.T.; Kosinski, T.F.; Nenn, C.A.; Olsen, J.A.; Platt, J.A.; Wingrove, S.S.; Chandler, N.D.; Curtis, D.A. Clinical Practice Guidelines for Recall and Maintenance of Patients with Tooth-Borne and Implant-Borne Dental Restorations. J. Prosthodont. 2016, 25, S32–S40. [Google Scholar] [CrossRef]
- Felice, P.; Barausse, C.; Pistilli, R.; Ippolito, D.R.; Esposito, M. Short implants versus longer implants in vertically augmented posterior mandibles: Result at 8 years after loading from a randomised controlled trial. Eur. J. Oral Implantol. 2018, 11, 385–395. [Google Scholar]
- Esposito, M.; Buti, J.; Barausse, C.; Gasparro, R.; Sammartino, G.; Felice, P. Short implants versus longer implants in vertically augmented atrophic mandibles: A systematic review of randomised controlled trials with a 5-year post-loading follow-up. Int. J. Oral Implantol. 2019, 12, 267–280. [Google Scholar]
- Esposito, M.; Zucchelli, G.; Barausse, C.; Pistilli, R.; Trullenque-Eriksson, A.; Felice, P. Four mm-long versus longer implants in augmented bone in atrophic posterior jaws: 4-month post-loading results from a multicentre randomised controlled trial. Eur. J. Oral Implantol. 2016, 9, 393–409. [Google Scholar] [PubMed]
- Esposito, M.; Barausse, C.; Pistilli, R.; Checchi, V.; Diazzi, M.; Gatto, M.R.; Felice, P. Posterior jaws rehabilitated with partial prostheses supported by 4.0 × 4.0 mm or by longer implants: Four-month post-loading data from a randomised controlled trial. Eur. J. Oral Implantol. 2015, 8, 221–230. [Google Scholar]
- Davó, R.; Felice, P.; Pistilli, R.; Barausse, C.; Marti-Pages, C.; Ferrer-Fuertes, A.; Ippolito, D.R.; Esposito, M. Immediately loaded zygomatic implants vs. conventional dental implants in augmented atrophic maxillae: 1-year post-loading results from a multicentre randomised controlled trial. Eur. J. Oral Implantol. 2018, 11, 145–161. [Google Scholar] [PubMed]
- Esposito, M.; Davó, R.; Marti-Pages, C.; Ferrer-Fuertes, A.; Barausse, C.; Pistilli, R.; Ippolito, D.R.; Felice, P. Immediately loaded zygomatic implants vs. conventional dental implants in augmented atrophic maxillae: 4 months post-loading results from a multicentre randomised controlled trial. Eur. J. Oral Implantol. 2018, 11, 11–28. [Google Scholar]
- Roccuzzo, M.; De Angelis, N.; Bonino, L.; Aglietta, M. Ten-year results of a three-arm prospective cohort study on implants in periodontally compromised patients. Part 1: Implant loss and radiographic bone loss. Clin. Oral Implants Res. 2010, 21, 490–496. [Google Scholar] [CrossRef]
- Roccuzzo, M.; Bonino, F.; Aglietta, M.; Dalmasso, P. Ten-year results of a three arms prospective cohort study on implants in periodontally compromised patients. Part 2: Clinical results. Clin. Oral Implants Res. 2012, 23, 389–395. [Google Scholar] [CrossRef]
- Derks, J.; Schaller, D.; Håkansson, J.; Wennström, J.L.; Tomasi, C.; Berglundh, T. Effectiveness of Implant Therapy Analyzed in a Swedish Population: Prevalence of Peri-implantitis. J. Dent. Res. 2016, 95, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Felice, P.; Zucchelli, G.; Cannizzaro, G.; Barausse, C.; Diazzi, M.; Trullenque-Eriksson, A.; Esposito, M. Immediate, immediate-delayed (6 weeks) and delayed (4 months) post-extractive single implants: 4-month post-loading data from a randomised controlled trial. Eur. J. Oral Implantol. 2016, 9, 233–247. [Google Scholar] [PubMed]
- Esposito, M.; Zucchelli, G.; Cannizzaro, G.; Checchi, L.; Barausse, C.; Trullenque-Eriksson, A.; Felice, P. Immediate, immediate-delayed (6 weeks) and delayed (4 months) post-extractive single implants: 1-year post-loading data from a randomised controlled trial. Eur. J. Oral Implantol. 2017, 10, 11–26. [Google Scholar] [PubMed]
- De Angelis, N.; Felice, P.; Pellegrino, G.; Camurati, A.; Gambino, P.; Esposito, M. Guided bone regeneration with and without a bone substitute at single post-extractive implants: 1-year post-loading results from a pragmatic multicentre randomised controlled trial. Eur. J. Oral Implantol. 2011, 4, 313–325. [Google Scholar]
- Serino, G.; Ström, C. Peri-implantitis in partially edentulous patients: Association with inadequate plaque control. Clin. Oral Implants Res. 2009, 20, 169–174. [Google Scholar] [CrossRef]
- Esposito, M.; Felice, P.; Barausse, C.; Pistilli, R.; Grandi, G.; Simion, M. Immediately loaded machined versus rough surface dental implants in edentulous jaws: One-year postloading results of a pilot randomised controlled trial. Eur. J. Oral Implantol. 2015, 8, 387–396. [Google Scholar]
- Cannizzaro, G.; Felice, P.; Gherlone, E.; Barausse, C.; Ferri, V.; Leone, M.; Trullenque-Eriksson, A.; Esposito, M. Immediate loading of two (fixed-on-2) vs. four (fixed-on-4) implants placed with a flapless technique supporting mandibular cross-arch fixed prostheses: 3-year results from a pilot randomised controlled trial. Eur. J. Oral Implantol. 2017, 10, 133–145. [Google Scholar] [PubMed]
- Humphrey, S. Implant maintenance. Dent. Clin. N. Am. 2006, 50, 463–478. [Google Scholar] [CrossRef]
- Heitz-Mayfield, L.J.; Aaboe, M.; Araujo, M.; Carrión, J.B.; Cavalcanti, R.; Cionca, N.; Cochran, D.; Darby, I.; Funakoshi, E.; Gierthmuehlen, P.C.; et al. Group 4 ITI Consensus Report: Risks and biologic complications associated with implant dentistry. Clin. Oral Implants Res. 2018, 29, 351–358. [Google Scholar] [CrossRef]
- Esposito, M.; Cannizzaro, G.; Barausse, C.; Cosci, F.; Soardi, E.; Felice, P. Cosci versus Summers technique for crestal sinus lift: 3-year results from a randomised controlled trial. Eur. J. Oral Implantol. 2014, 7, 129–137. [Google Scholar]
- Felice, P.; Pistilli, R.; Zucchelli, G.; Simion, M.; Karaban, M.; Bonifazi, L.; Barausse, C. Decision Criteria Proposed for the Treatment of Vertical Bone Atrophies in the Posterior Mandible. Int. J. Periodontics Restor. Dent. 2021, 41, 71–77. [Google Scholar] [CrossRef]
- Checchi, V.; Felice, P.; Zucchelli, G.; Barausse, C.; Piattelli, M.; Pistilli, R.; Grandi, G.; Esposito, M. Wide diameter immediate post-extractive implants vs. delayed placement of normal-diameter implants in preserved sockets in the molar region: 1-year post-loading outcome of a randomised controlled trial. Eur. J. Oral Implantol. 2017, 10, 263–278. [Google Scholar] [PubMed]
- Felice, P.; Barausse, C.; Barone, A.; Zucchelli, G.; Piattelli, M.; Pistilli, R.; Ippolito, D.R.; Simion, M. Interpositional Augmentation Technique in the Treatment of Posterior Mandibular Atrophies: A Retrospective Study Comparing 129 Autogenous and Heterologous Bone Blocks with 2 to 7 Years Follow-Up. Int. J. Periodontics Restor. Dent. 2017, 37, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Carcuac, O.; Abrahamsson, I.; Derks, J.; Petzold, M.; Berglundh, T. Spontaneous progression of experimental peri-implantitis in augmented and pristine bone: A pre-clinical in vivo study. Clin. Oral Implants Res. 2020, 31, 192–200. [Google Scholar] [CrossRef]
- Felice, P.; Pistilli, R.; Barausse, C.; Piattelli, M.; Buti, J.; Esposito, M. Posterior atrophic jaws rehabilitated with prostheses supported by 6-mm-long 4-mm-wide implants or by longer implants in augmented bone. Five-year post-loading results from a within-person randomised controlled trial. Int. J. Oral Implantol. 2019, 12, 57–72. [Google Scholar]
- Esposito, M.; Barausse, C.; Pistilli, R.; Piattelli, M.; Di Simone, S.; Ippolito, D.R.; Felice, P. Posterior atrophic jaws rehabilitated with prostheses supported by 5 × 5 mm implants with a nanostructured calcium-incorporated titanium surface or by longer implants in augmented bone. Five-year results from a randomised controlled trial. Int. J. Oral Implantol. 2019, 12, 39–54. [Google Scholar]
- Felice, P.; Barausse, C.; Pistilli, R.; Ippolito, D.R.; Esposito, M. Five-year results from a randomised controlled trial comparing prostheses supported by 5-mm long implants or by longer implants in augmented bone in posterior atrophic edentulous jaws. Int. J. Oral Implantol. 2019, 12, 25–37. [Google Scholar]


| Types of Implant Prosthetic Rehabilitations | ORDINARY Hygiene (Months) | EXTRAORDINARY Hygiene (Months) |
|---|---|---|
| Single crown | 6/4 * | BOP+ |
| Fixed partial prosthesis | 4/3 * | 12/BOP+ |
| Fixed full-arch | 4/3 * | 6/BOP+ |
| Overdentures | 4/3 * | BOP+ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Felice, P.; Bertacci, A.; Bonifazi, L.; Karaban, M.; Canullo, L.; Pistilli, R.; Sammartino, P.; Gasparro, R.; Barausse, C. A Proposed Protocol for Ordinary and Extraordinary Hygienic Maintenance in Different Implant Prosthetic Scenarios. Appl. Sci. 2021, 11, 2957. https://doi.org/10.3390/app11072957
Felice P, Bertacci A, Bonifazi L, Karaban M, Canullo L, Pistilli R, Sammartino P, Gasparro R, Barausse C. A Proposed Protocol for Ordinary and Extraordinary Hygienic Maintenance in Different Implant Prosthetic Scenarios. Applied Sciences. 2021; 11(7):2957. https://doi.org/10.3390/app11072957
Chicago/Turabian StyleFelice, Pietro, Angelica Bertacci, Lorenzo Bonifazi, Maryia Karaban, Luigi Canullo, Roberto Pistilli, Pasquale Sammartino, Roberta Gasparro, and Carlo Barausse. 2021. "A Proposed Protocol for Ordinary and Extraordinary Hygienic Maintenance in Different Implant Prosthetic Scenarios" Applied Sciences 11, no. 7: 2957. https://doi.org/10.3390/app11072957
APA StyleFelice, P., Bertacci, A., Bonifazi, L., Karaban, M., Canullo, L., Pistilli, R., Sammartino, P., Gasparro, R., & Barausse, C. (2021). A Proposed Protocol for Ordinary and Extraordinary Hygienic Maintenance in Different Implant Prosthetic Scenarios. Applied Sciences, 11(7), 2957. https://doi.org/10.3390/app11072957









