Comparison of Trabecular Bone Mineral Density Measurement Using Hounsfield Unit and Trabecular Microstructure in Orthodontic Patients Using Cone-Beam Computed Tomography
Abstract
1. Introduction
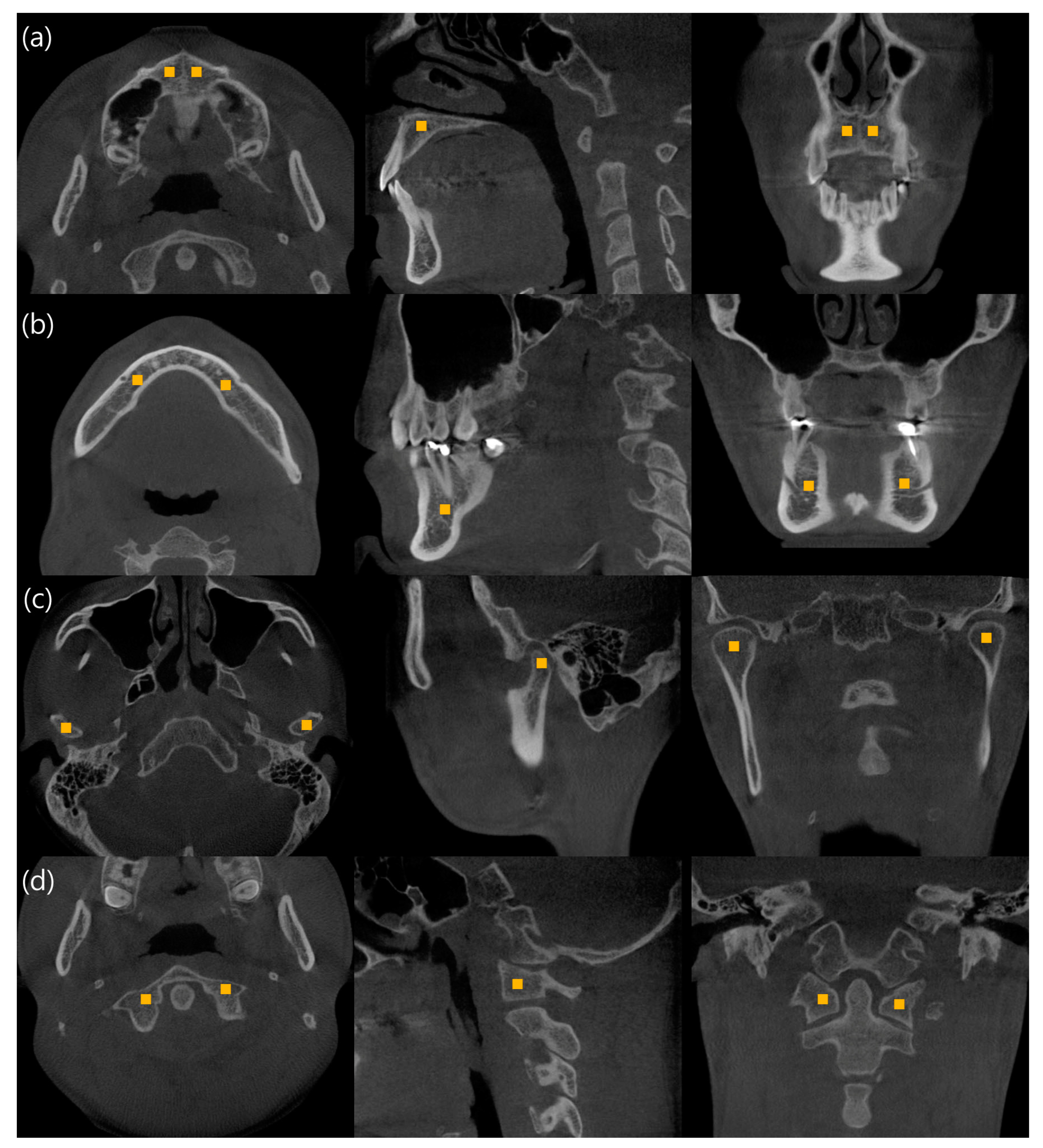
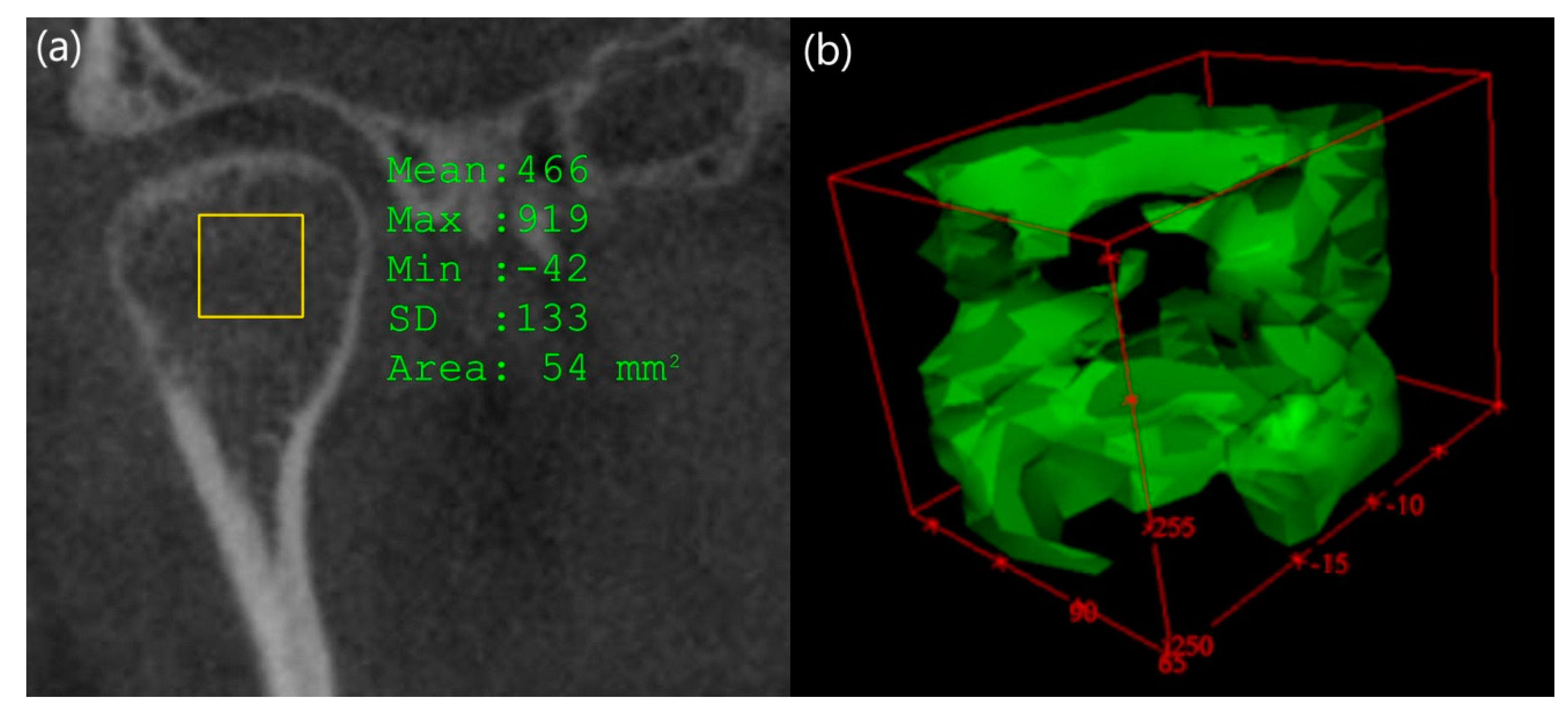
2. Materials and Methods
- (1)
- Patients without defects in the trabecular bone density measurement area.
- (2)
- Patients with no symptoms of temporomandibular disorder (TMD).
- (3)
- Patients without a history of bone diseases such as osteoporosis.
- (4)
- CBCT images having a quality suitable for research.
3. Results
3.1. Bone Mineral Density Measurement in the Right and Left Side and in Males and Females
3.2. Comparison between the Bone Mineral Density Parameters among Regions
3.2.1. Trabecular Thickness (Tb.th)
3.2.2. Trabecular Number (Tb.n)
3.2.3. Trabecular Seperation (Tb.sp)
3.2.4. Bone Volume Fraction (BV/TV)
3.2.5. Hounsfield Unit (HU)
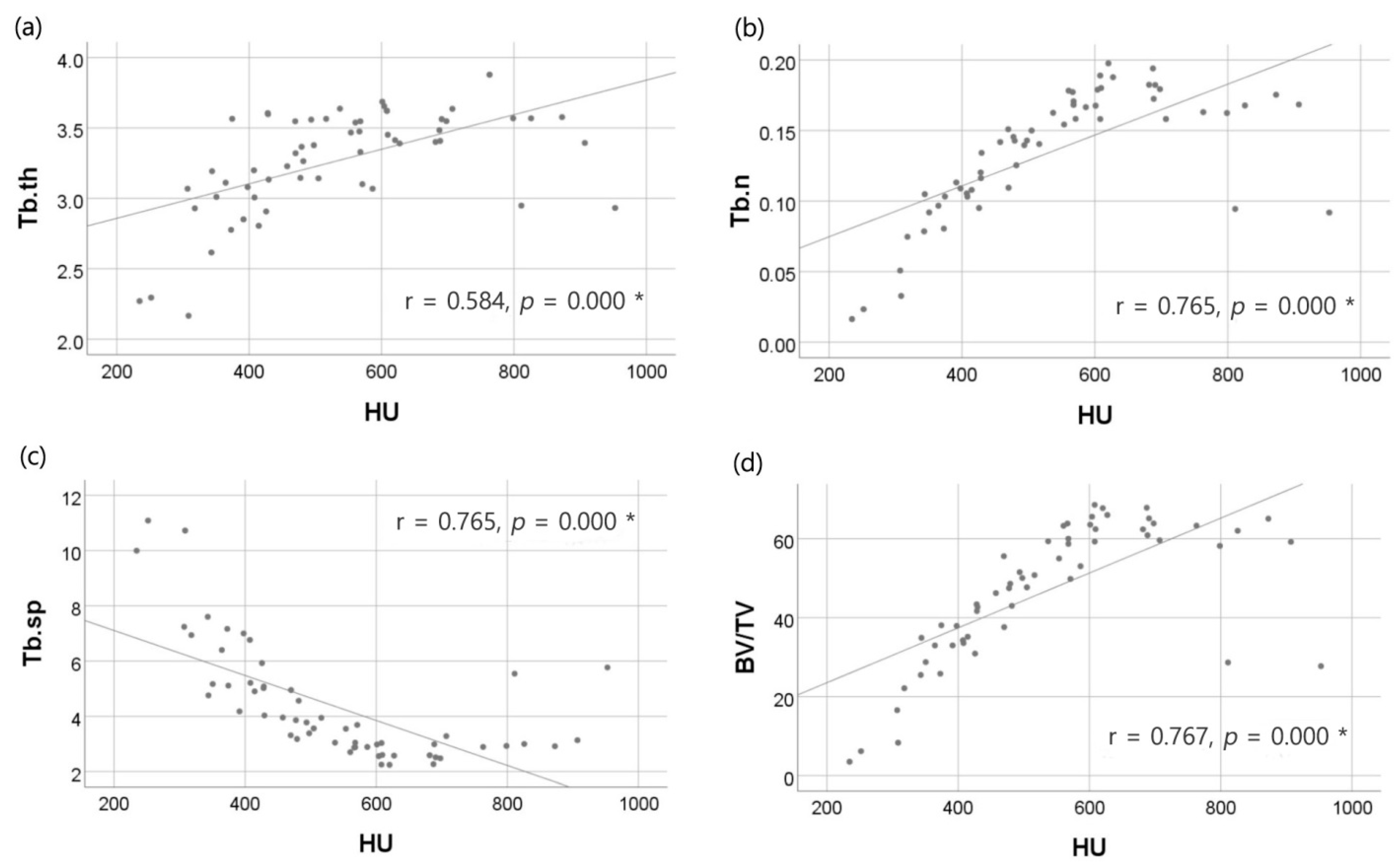
3.3. Comparison Between the Trabecular Bone Density Measurement Method Using the Hounsfield Unit and Trabecular Microstructure Parameters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- White, S.C.; Rudolph, D.J. Alterations of the trabecular pattern of the jaws in patients with osteoporosis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1999, 88, 628–635. [Google Scholar] [CrossRef]
- Roberts, W.E. Bone physiology, metabolism, and biomechanics in orthodontic practice. In Current Principles and Techniques, 4th ed.; Mosby: St. Louis, MO, USA, 2005. [Google Scholar]
- Silva, I.M.; Freitas, D.Q.; Ambrosano, G.M.; Boscolo, F.N.; Almeida, S.M. Bone density: Comparative evaluation of hounsfield units in multislice and cone-beam computed tomography. Braz. Oral Res 2012, 26, 550–556. [Google Scholar] [CrossRef] [PubMed]
- Misch, C.E.; Kircos, L.T. Diagnostic imaging and techniques. In Contemporary Implant Dentistry, 2nd ed.; Mosby: St Louis, MO, USA, 1999. [Google Scholar]
- Ibrahim, N.; Parsa, A.; Hassan, B.; van der Stelt, P.; Aartman, I.H.; Wismeijer, D. Accuracy of trabecular bone microstructural measurement at planned dental implant sites using cone-beam CT datasets. Clin. Oral Implant. Res. 2014, 25, 941–945. [Google Scholar] [CrossRef]
- Lee, M.-Y.; Park, J.-H.; Kim, S.-C.; Kang, K.-H.; Cho, J.-H.; Cho, J.-W.; Chang, N.Y.; Chae, J.M. Bone density effects on the success rate of orthodontic microimplants evaluated with cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 217–224. [Google Scholar] [CrossRef]
- Hsu, J.T.; Chen, Y.J.; Ho, J.T.; Huang, H.L.; Wang, S.P.; Cheng, F.C.; Wu, J.; Tsai, M.T. A comparison of micro-CT and dental CT in assessing cortical bone morphology and trabecular bone microarchitecture. PLoS ONE 2014, 9, e107545. [Google Scholar] [CrossRef] [PubMed]
- Guerra, E.N.S.; Almeida, F.T.; Bezerra, F.V.; Figueiredo, P.; Silva, M.A.G.; De Luca Canto, G.; Pacheco-Pereira, C.; Leite, A.F. Capability of CBCT to identify patients with low bone mineral density: A systematic review. Dentomaxillofac. Radiol. 2017, 46, 20160475. [Google Scholar] [CrossRef]
- Genant, H.K.; Gordon, C.; Jiang, Y.; Lang, T.F.; Link, T.M.; Majumdar, S. Advanced imaging of bone macro and micro structure. Bone 1999, 25, 149–152. [Google Scholar] [CrossRef]
- Chugh, T.; Jain, A.K.; Jaiswal, R.K.; Mehrotra, P.; Mehrotra, R. Bone density and its importance in orthodontics. J. Oral Biol. Craniofac. Res. 2013, 3, 92–97. [Google Scholar] [CrossRef]
- Zioupos, P.; Cook, R.B.; Hutchinson, J.R. Some basic relationships between density values in cancellous and cortical bone. J. Biomech. 2008, 41, 1961–1968. [Google Scholar] [CrossRef]
- Ruijven, L.J.; Giesen, E.B.W.; Mulder, L.; Farella, M.; Eijden, T.M. The effect of bone loss on rod-like and plate-like trabeculae in the cancellous bone of the mandibular condyle. Bone 2005, 36, 1078–1085. [Google Scholar]
- Odgaard, A. Three-dimensional methods for quantification for cancellous bone architecture. Bone 1997, 20, 315–328. [Google Scholar] [CrossRef]
- Moon, H.-S.; Won, Y.-Y.; Kim, K.-D.; Ruprecht, A.; Kim, H.-J.; Kook, H.-K.; Chung, M.K. The three-dimensional microstructure of the trabecular bone in the mandible. Surg. Radiol. Anat. 2004, 26, 466–473. [Google Scholar] [CrossRef] [PubMed]
- Bouxsein, M.L.; Boyd, S.K.; Christiansen, B.A.; Guldberg, R.E.; Jepsen, K.J.; Muller, R. Guidelines for assessment of bone microstructure in rodents using micro–computed tomography. J. Bone Min. Res. 2010, 25, 1468–1486. [Google Scholar] [CrossRef] [PubMed]
- Dutra, V.; Yang, J.; Devlin, H.; Susin, C. Radiomorphometric indices and their relation to gender, age, and dental status. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2005, 99, 479–484. [Google Scholar] [CrossRef] [PubMed]
- Ulm, C.W.; Kneissel, M.; Hahn, M.; Solar, P.; Matejka, M.; Donath, K. Characteristics of the cancellous bone of edentulous mandibles. Clin. Oral Implant. Res. 1997, 8, 125–130. [Google Scholar] [CrossRef]
- von Wowern, N. Bone mass of mandibles. In vitro and in vivo analyses. Dan. Med. Bull. 1986, 33, 23–44. [Google Scholar] [PubMed]
- Pavlova, M.N.; Peliakov, A.N. Age changes in the mineralization of the human femur according to quantitative microradiographic data. Arkhiv Anat. Gistol. Embriol. 1971, 61, 83–88. [Google Scholar]
- Yong, S.-J.; Lim, S.-K.; Huh, K.-B.; Park, B.-M.; Kim, N.-H. Bone mineral density of normal Korean adults. J. Korean Med. Assoc. 1988, 31, 1350–1358. [Google Scholar]
- Klemetti, E.; Vainio, P.; Kruger, H. Muscle strength and mineral densities in the mandible. Gerodontology 1994, 11, 76–79. [Google Scholar] [CrossRef]
- Perrini, P.; Gambacciani, C.; Martini, C.; Montemurro, N.; Lepori, P. Anterior cervical corpectomy for cervical spondylotic myelopathy: Reconstruction with expandable cylindrical cage versus iliac crest autograft. A retrospective study. Clin. Neurol. Neurosurg. 2015, 139, 258–263. [Google Scholar] [CrossRef]
- Montemurro, N.; Perrini, P.; Mangini, V.; Galli, M.; Papini, A. The Y-shaped trabecular bone structure in the odontoid process of the axis: A CT scan study in 54 healthy subjects and biomechanical considerations. J. Neurosurg. Spine 2019, 30, 1–8. [Google Scholar] [CrossRef] [PubMed]
- De Vos, W.; Casselman, J.; Swennen, G.R. Cone-beam computerized tomography (CBCT) imaging of the oral and maxillofacial region: A systematic review of the literature. Int J. Oral Maxillofac Surg. 2009, 38, 609–625. [Google Scholar] [CrossRef] [PubMed]
- Koc, A.; Kavut, I.; Ugur, M. Evaluation of trabecular bone microstructure of mandibular condyle in edentulous, unilateral edentulous and fully dentate patients using cone-beam computed tomography. Folia Morphol. 2020, 79, 829–834. [Google Scholar] [CrossRef] [PubMed]
| Male | Female | Total | |
|---|---|---|---|
| Number of regions measured | 272 | 192 | 464 |
| Number of patients | 34 | 24 | 58 |
| Mean age (SD) | 23.8 (6.5) | 19.5 (7.0) | 22.0 (7.0) |
| Description | Unit | |
|---|---|---|
| Tb.th | Trabecular thickness: Mean thickness of trabeculae | mm |
| Tb.n | Trabecular number: Measure of the average number of trabeculae per unit length | 1/mm |
| Tb.sp | Trabecular separation: Mean distance between trabeculae | mm |
| BV/TV | Bone volume fraction: Ratio of the segmented bone volume to the total volume of the region of interest | % |
| Region | Right | Left | Difference | p-Value | ||||
|---|---|---|---|---|---|---|---|---|
| Median | IQR | Median | IQR | Median | IQR | |||
| Mx | Tb.th | 3.79 | 1.11 | 3.71 | 0.79 | 0.10 | 0.94 | 0.568 |
| Tb.n | 0.14 | 0.04 | 0.14 | 0.03 | 0.00 | 0.03 | 0.298 | |
| Tb.sp | 3.57 | 0.82 | 3.52 | 0.85 | −0.02 | 0.81 | 0.640 | |
| BV/TV | 54.52 | 10.23 | 53.10 | 11.81 | 0.49 | 9.34 | 0.502 | |
| HU | 1441.41 | 332.27 | 1505.36 | 268.68 | −74.48 | 331.90 | 0.268 | |
| Mn | Tb.th | 3.45 | 0.67 | 3.42 | 0.68 | 0.04 | 0.69 | 0.497 |
| Tb.n | 0.14 | 0.06 | 0.14 | 0.07 | 0.02 | 0.10 | 0.572 | |
| Tb.sp | 3.62 | 1.17 | 3.71 | 0.91 | −0.08 | 0.98 | 0.354 | |
| BV/TV | 49.86 | 13.25 | 48.03 | 11.85 | 1.79 | 11.21 | 0.374 | |
| HU | 1401.38 | 304.89 | 1416.11 | 283.95 | −13.08 | 290.25 | 0.248 | |
| Co | Tb.th | 3.17 | 0.51 | 3.24 | 0.43 | −0.06 | 0.58 | 0.349 |
| Tb.n | 0.14 | 0.04 | 0.13 | 0.03 | 0.01 | 0.03 | 0.130 | |
| Tb.sp | 4.46 | 3.96 | 4.55 | 3.75 | −0.31 | 4.73 | 0.811 | |
| BV/TV | 48.07 | 21.83 | 44.58 | 23.50 | −0.75 | 33.20 | 0.868 | |
| HU | 653.02 | 315.91 | 715.49 | 378.01 | −49.77 | 383.40 | 0.402 | |
| Cv | Tb.th | 3.22 | 0.60 | 3.35 | 0.47 | −0.14 | 0.65 | 0.201 |
| Tb.n | 0.13 | 0.09 | 0.14 | 0.05 | −0.01 | 0.07 | 0.366 | |
| Tb.sp | 4.50 | 3.79 | 3.96 | 2.48 | 0.79 | 2.89 | 0.659 | |
| BV/TV | 43.86 | 28.81 | 49.26 | 20.35 | −6.51 | 25.54 | 0.383 | |
| HU | 511.09 | 236.07 | 575.71 | 279.92 | −45.18 | 235.75 | 0.186 | |
| Region | Male | Female | Difference | p-Value | ||||
|---|---|---|---|---|---|---|---|---|
| Median | IQR | Median | IQR | Median | IQR | |||
| Mx | Tb.th | 3.92 | 0.90 | 3.71 | 0.59 | −0.21 | 0.31 | 0.647 |
| Tb.n | 0.14 | 0.02 | 0.15 | 0.04 | 0.01 | 0.02 | 0.776 | |
| Tb.sp | 3.51 | 0.64 | 3.50 | 0.74 | −0.01 | 0.10 | 0.825 | |
| BV/TV | 54.36 | 10.58 | 54.20 | 9.80 | −0.16 | 0.78 | 0.991 | |
| HU | 1482.81 | 269.65 | 1456.87 | 213.89 | −25.94 | 55.76 | 0.752 | |
| Mn | Tb.th | 3.42 | 0.46 | 3.50 | 0.69 | 0.08 | 0.23 | 0.412 |
| Tb.n | 0.14 | 0.04 | 0.14 | 0.06 | 0.00 | 0.02 | 0.328 | |
| Tb.sp | 3.68 | 0.94 | 3.75 | 0.87 | 0.07 | 0.07 | 0.290 | |
| BV/TV | 51.41 | 9.97 | 47.01 | 12.97 | −4.40 | 3.00 | 0.602 | |
| HU | 1441.03 | 234.83 | 1346.83 | 304.60 | −94.20 | 69.77 | 0.097 | |
| Co | Tb.th | 3.19 | 0.30 | 3.23 | 0.39 | 0.04 | 0.09 | 0.468 |
| Tb.n | 0.14 | 0.03 | 0.14 | 0.03 | 0.00 | 0.01 | 0.412 | |
| Tb.sp | 4.38 | 2.26 | 4.31 | 3.53 | −0.07 | 1.27 | 0.962 | |
| BV/TV | 45.61 | 13.95 | 49.63 | 20.43 | 4.02 | 6.48 | 0.122 | |
| HU | 656.03 | 253.57 | 739.79 | 343.88 | 83.76 | 90.31 | 0.067 | |
| Cv | Tb.th | 3.23 | 0.48 | 3.37 | 0.43 | 0.14 | 0.05 | 0.190 |
| Tb.n | 0.13 | 0.07 | 0.14 | 0.05 | 0.01 | 0.02 | 0.728 | |
| Tb.sp | 4.48 | 3.23 | 4.10 | 1.86 | −0.38 | 1.37 | 0.776 | |
| BV/TV | 45.92 | 24.52 | 52.51 | 19.55 | 6.59 | 4.97 | 0.507 | |
| HU | 522.27 | 232.53 | 549.13 | 255.92 | 26.86 | 23.39 | 0.764 | |
| Mx | Mn | Co | Cv | p-Value | |
|---|---|---|---|---|---|
| Median(IQR) | Median(IQR) | Median(IQR) | Median(IQR) | ||
| Tb.th | 3.84(0.85) a | 3.49(0.53) b | 3.21(0.36) c | 3.25(0.50) bc | 0.025 |
| Tb.n | 0.14(0.034) a | 0.14(0.05) ab | 0.13(0.03) b | 0.14(0.05) ab | 0.032 |
| Tb.sp | 3.51(0.73) c | 3.74(1.05) bc | 4.51(3.21) a | 4.27(2.79) ab | 0.015 |
| BV/TV | 53.42(9.78) a | 50.29(12.35) b | 47.50(16.72) bc | 46.58(24.06) c | 0.008 |
| HU | 1458.69(227.17) a | 1414.19(265.78) b | 697.14(264.81) c | 540.51(226.40) d | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, T.-H.; Lee, D.-Y.; Jung, S.-K. Comparison of Trabecular Bone Mineral Density Measurement Using Hounsfield Unit and Trabecular Microstructure in Orthodontic Patients Using Cone-Beam Computed Tomography. Appl. Sci. 2021, 11, 1028. https://doi.org/10.3390/app11031028
Kim T-H, Lee D-Y, Jung S-K. Comparison of Trabecular Bone Mineral Density Measurement Using Hounsfield Unit and Trabecular Microstructure in Orthodontic Patients Using Cone-Beam Computed Tomography. Applied Sciences. 2021; 11(3):1028. https://doi.org/10.3390/app11031028
Chicago/Turabian StyleKim, Tae-Hyun, Dong-Yul Lee, and Seok-Ki Jung. 2021. "Comparison of Trabecular Bone Mineral Density Measurement Using Hounsfield Unit and Trabecular Microstructure in Orthodontic Patients Using Cone-Beam Computed Tomography" Applied Sciences 11, no. 3: 1028. https://doi.org/10.3390/app11031028
APA StyleKim, T.-H., Lee, D.-Y., & Jung, S.-K. (2021). Comparison of Trabecular Bone Mineral Density Measurement Using Hounsfield Unit and Trabecular Microstructure in Orthodontic Patients Using Cone-Beam Computed Tomography. Applied Sciences, 11(3), 1028. https://doi.org/10.3390/app11031028






