Late Developed Unusual Nasal Involvement of Postoperative Maxillary Cyst Following Maxillary Sinus Augmentation: A Case Report
Abstract
:1. Introduction
2. Case Report
2.1. Past Dental Treatment
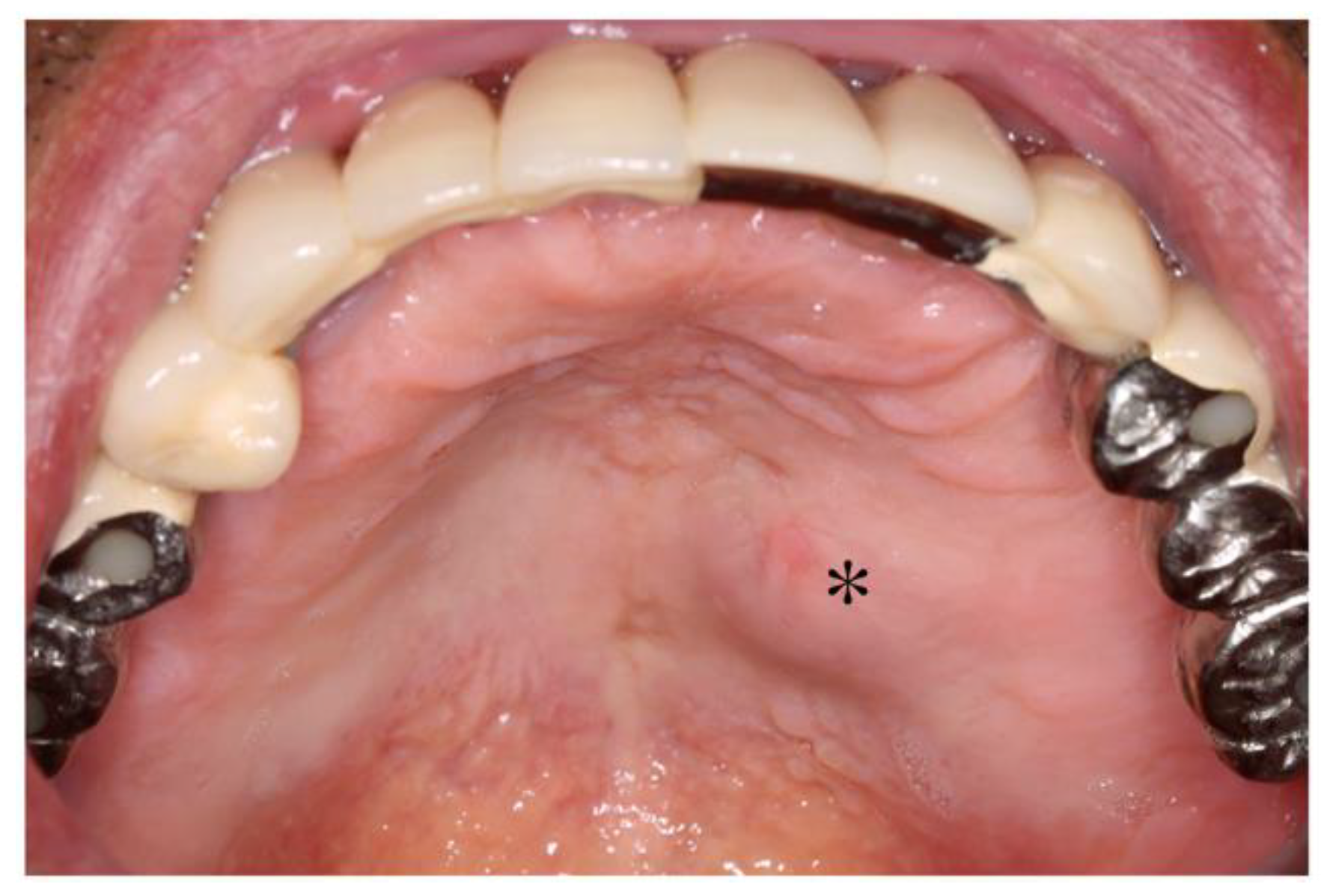
2.2. Dental Examination
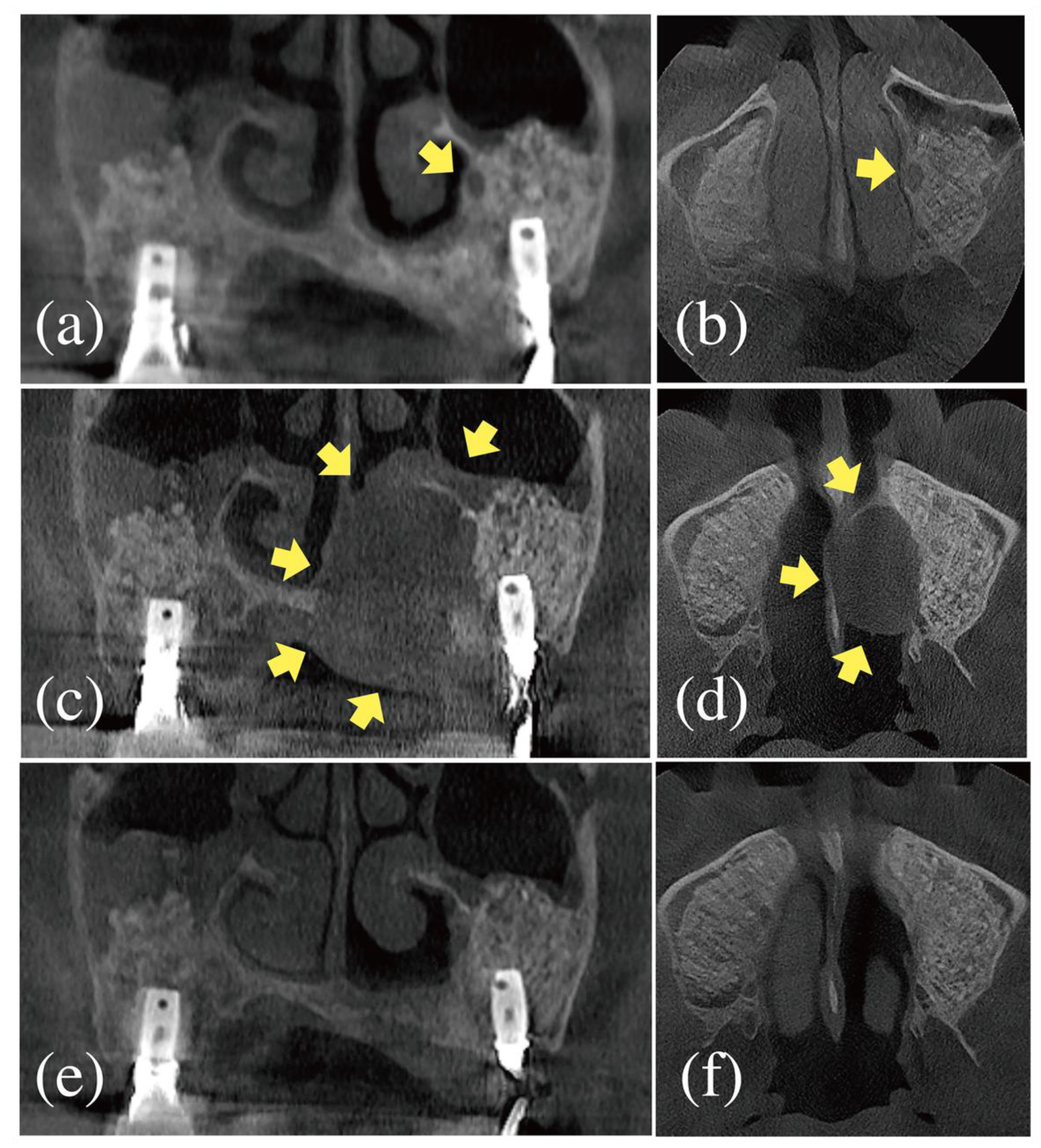
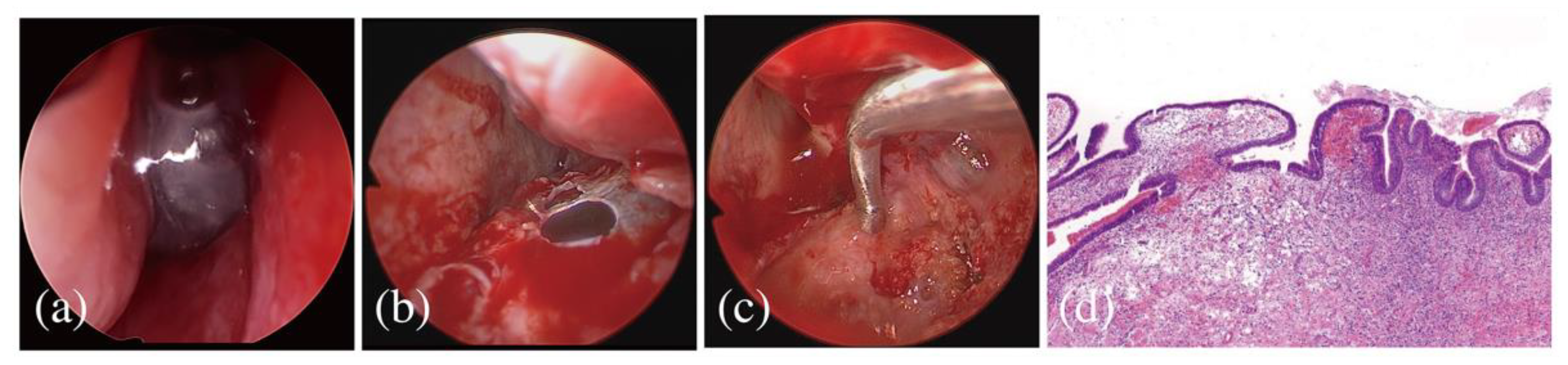
2.3. Referral to an Otolaryngological Specialist
2.4. Follow-Up
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pjetursson, B.E.; Tan, W.C.; Zwahlen, M.; Lang, N.P. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. J. Clin. Periodontol. 2008, 35, 216–240. [Google Scholar] [CrossRef] [PubMed]
- Hamdoon, Z.; Mahmood, N.; Talaat, W.; Sattar, A.A.; Naeim, K.; Qais, A.; Kheder, W.; Jerjes, W. Evaluation of different surgical approaches to remove dental implants from the maxillary sinus. Sci. Rep. 2021, 11, 1–8. [Google Scholar] [CrossRef]
- Testori, T.; Weinstein, T.; Taschieri, S.; Wallace, S.S. Risk factors in lateral window sinus elevation surgery. Periodontol. 2000 2019, 81, 91–123. [Google Scholar] [CrossRef] [PubMed]
- Kubo, I. A buccal cyst occurred after a radical operation of the maxillary sinus. JAP J. Otolaryngol. 1927, 33, 896. [Google Scholar]
- An, J.; Zhang, Y. Surgical ciliated cyst of the medial canthal region after the management of a midfacial fracture: A case report. J Craniofac. Surg. 2014, 25, 70–702. [Google Scholar] [CrossRef] [PubMed]
- Cano, J.; Campo, J.; Alobera, M.A.; Baca, R. Surgical ciliated cyst of the maxilla. Clinical case. Medicina Oral Patología Oral y Cirugia Bucal 2009, 14, 361–364. [Google Scholar]
- Soares, J.C.; Villalba, N.C.; Sanromán, J.F.; Ferro, M.F.; Fernández, P.L.; Betancourt, A.L.; López, A.C. Surgical Ciliated Cysts in Orthognathic Surgery. J. Craniofacial Surg. 2021, 32, e2–e5. [Google Scholar] [CrossRef]
- Leung, Y.Y.; Wong, W.Y.; Cheung, L.K. Surgical Ciliated Cysts May Mimic Radicular Cysts or Residual Cysts of Maxilla: Report of 3 Cases. J. Oral Maxillofac. Surg. 2012, 70, e264–e269. [Google Scholar] [CrossRef]
- Misch, C.M.; Resnik, R.R.; Ismail, Y.H.; Appel, B. Post-operative maxillary cyst associated with a maxillary sinus elevation procedure: A case report. J. Oral Implant. 1991, 17, 432–437. [Google Scholar]
- Kahn, A.; Matalon, S.; Salem, R.; Kats, L.; Chaushu, L.; Vered, M.; Rosen, E. Sinus Floor Augmentation—Associated Surgical Ciliated Cysts: Case Series and a Systematic Review of the Literature. Appl. Sci. 2021, 11, 1903. [Google Scholar] [CrossRef]
- Kim, J.J.; Freire, M.; Yoon, J.-H.; Kim, H.K. Postoperative Maxillary Cyst After Maxillary Sinus Augmentation. J. Craniofacial Surg. 2013, 24, e521–e523. [Google Scholar] [CrossRef]
- Lockhart, R.; Ceccaldi, J.; Bertrand, J.C. Postoperative maxillary cyst following sinus bone graft: Report of a case. Int. J. Oral Maxillofac. Implant. 2000, 15, 583–586. [Google Scholar]
- Yamamoto, S.; Maeda, K.; Kouchi, I.; Hirai, Y.; Taniike, N.; Imai, Y.; Takenobu, T. Surgical Ciliated Cyst Following Maxillary Sinus Floor Augmentation: A Case Report. J. Oral Implant. 2017, 43, 360–364. [Google Scholar] [CrossRef]
- Caton, J.G.; Armitage, G.; Berglundh, T.; Chapple, I.L.C.; Jepsen, S.; Kornman, K.S.; Mealey, B.L.; Papapanou, P.N.; Sanz, M.; Tonetti, M.S. A new classification scheme for periodontal and peri-implant diseases and conditions - introduction and key changes from the 1999 classification. J Clin. Periodontol. 2018, 45 (Suppl. 20), S1–S8. [Google Scholar] [CrossRef] [PubMed]
- Consolo, U.; Bellini, P.; Lizio, G. Trans-nasal endoscopic marsupialization of a voluminous radicular cyst involving maxillary sinus and nasal cavity: A case report and a literature review on this surgical approach. Oral Maxillofac. Surg. Cases 2018, 4, 91–96. [Google Scholar] [CrossRef]
- Kim, T.H.; Kim, J.S.; Heo, S.J. Postoperative maxillary mucocele with orbital wall defect treated by transnasal endoscopic marsupialization with a penrose drain insertion: A case report. Medicine 2019, 98, e15674. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, W.-B.; Lim, H.-C. Late Developed Unusual Nasal Involvement of Postoperative Maxillary Cyst Following Maxillary Sinus Augmentation: A Case Report. Appl. Sci. 2021, 11, 10730. https://doi.org/10.3390/app112210730
Park W-B, Lim H-C. Late Developed Unusual Nasal Involvement of Postoperative Maxillary Cyst Following Maxillary Sinus Augmentation: A Case Report. Applied Sciences. 2021; 11(22):10730. https://doi.org/10.3390/app112210730
Chicago/Turabian StylePark, Won-Bae, and Hyun-Chang Lim. 2021. "Late Developed Unusual Nasal Involvement of Postoperative Maxillary Cyst Following Maxillary Sinus Augmentation: A Case Report" Applied Sciences 11, no. 22: 10730. https://doi.org/10.3390/app112210730
APA StylePark, W.-B., & Lim, H.-C. (2021). Late Developed Unusual Nasal Involvement of Postoperative Maxillary Cyst Following Maxillary Sinus Augmentation: A Case Report. Applied Sciences, 11(22), 10730. https://doi.org/10.3390/app112210730





